Correlation between TMJ Space Alteration and Disc Displacement: A Retrospective CBCT and MRI Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
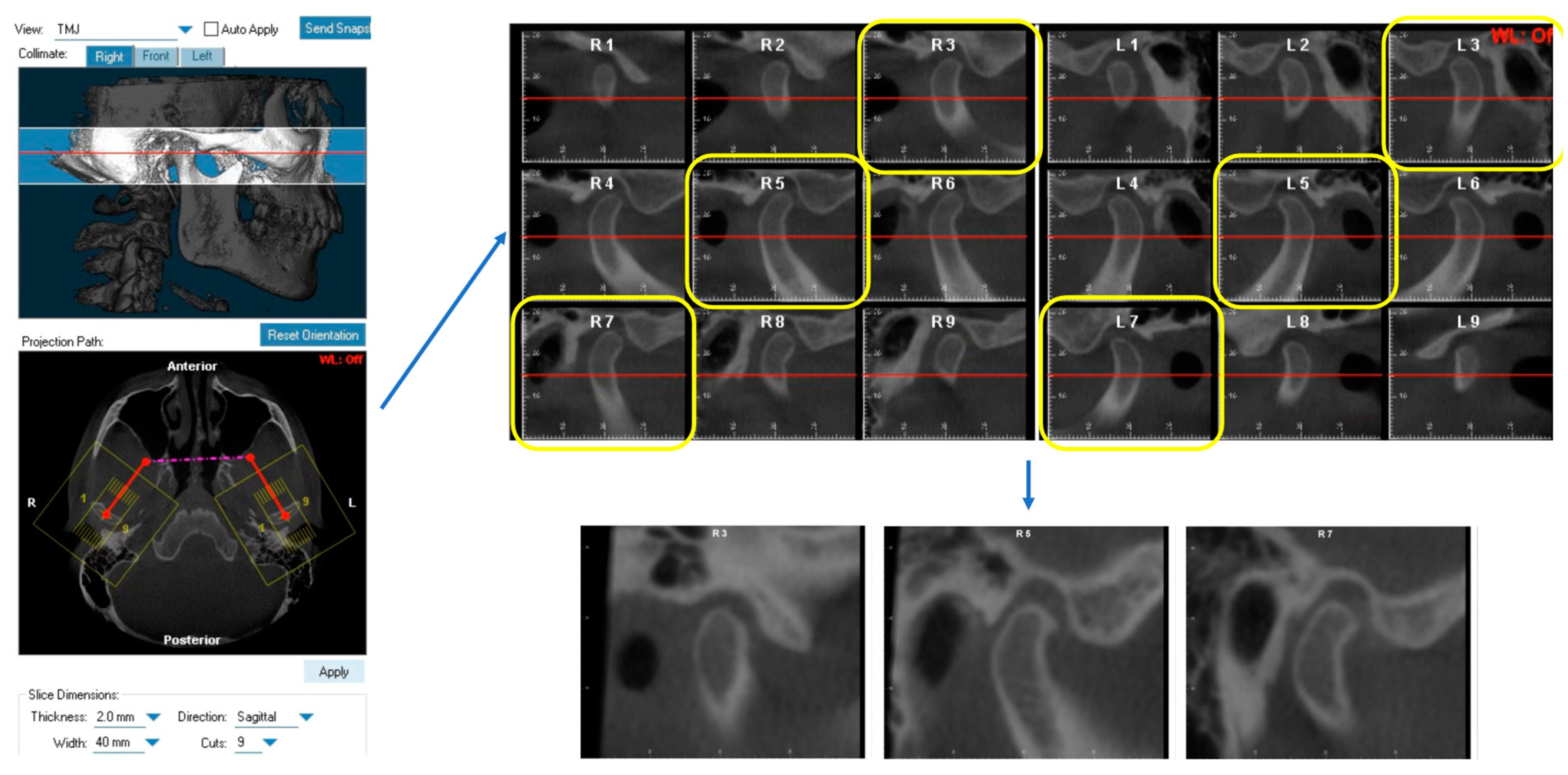
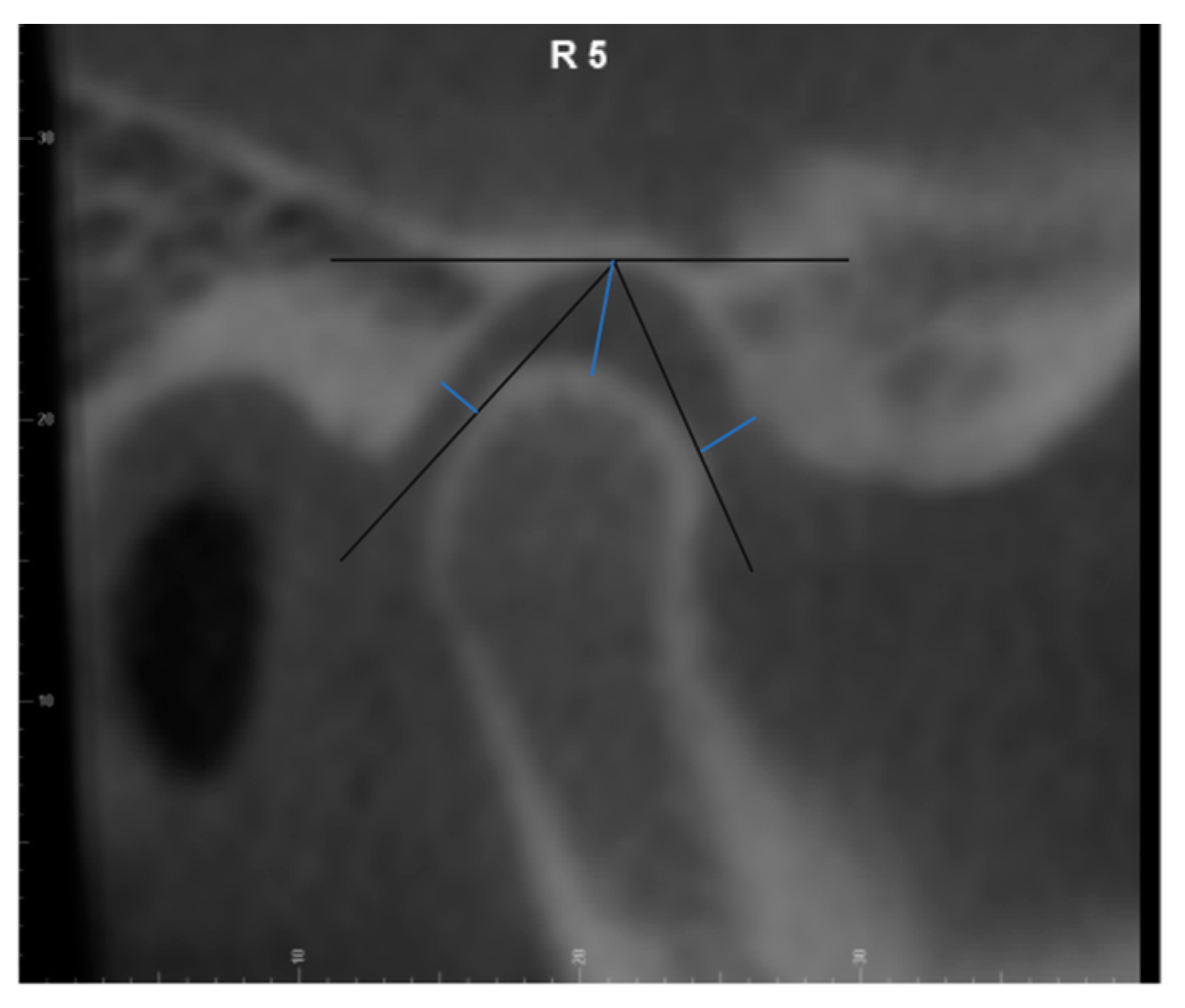
2.2. CBCT Measurements
2.3. MRI Evaluation
2.4. Statistics
3. Results
3.1. Sample Population
3.2. Disc Position Information
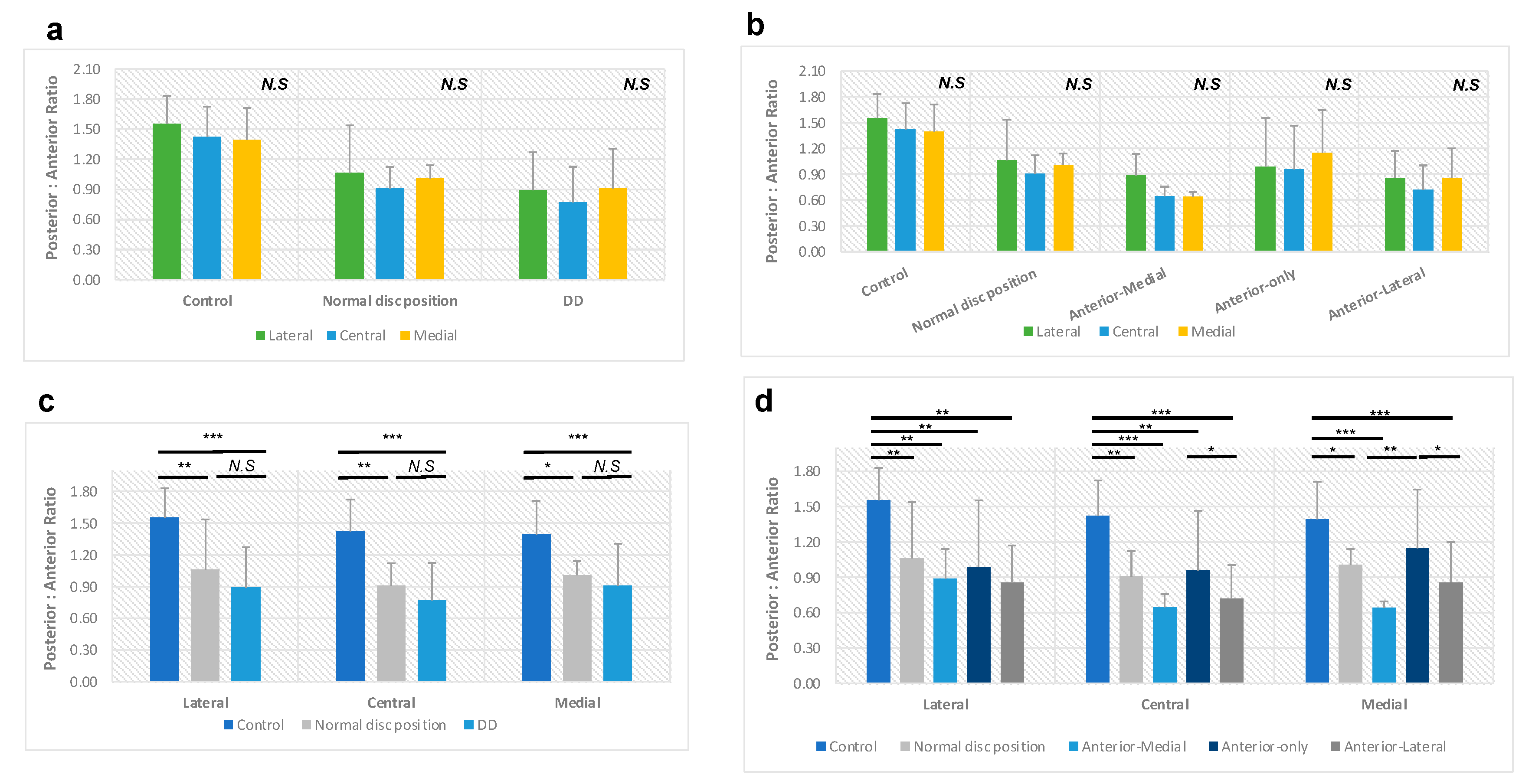
3.3. Posterior-to-Anterior Joint Space Ratio (P-A Ratio)
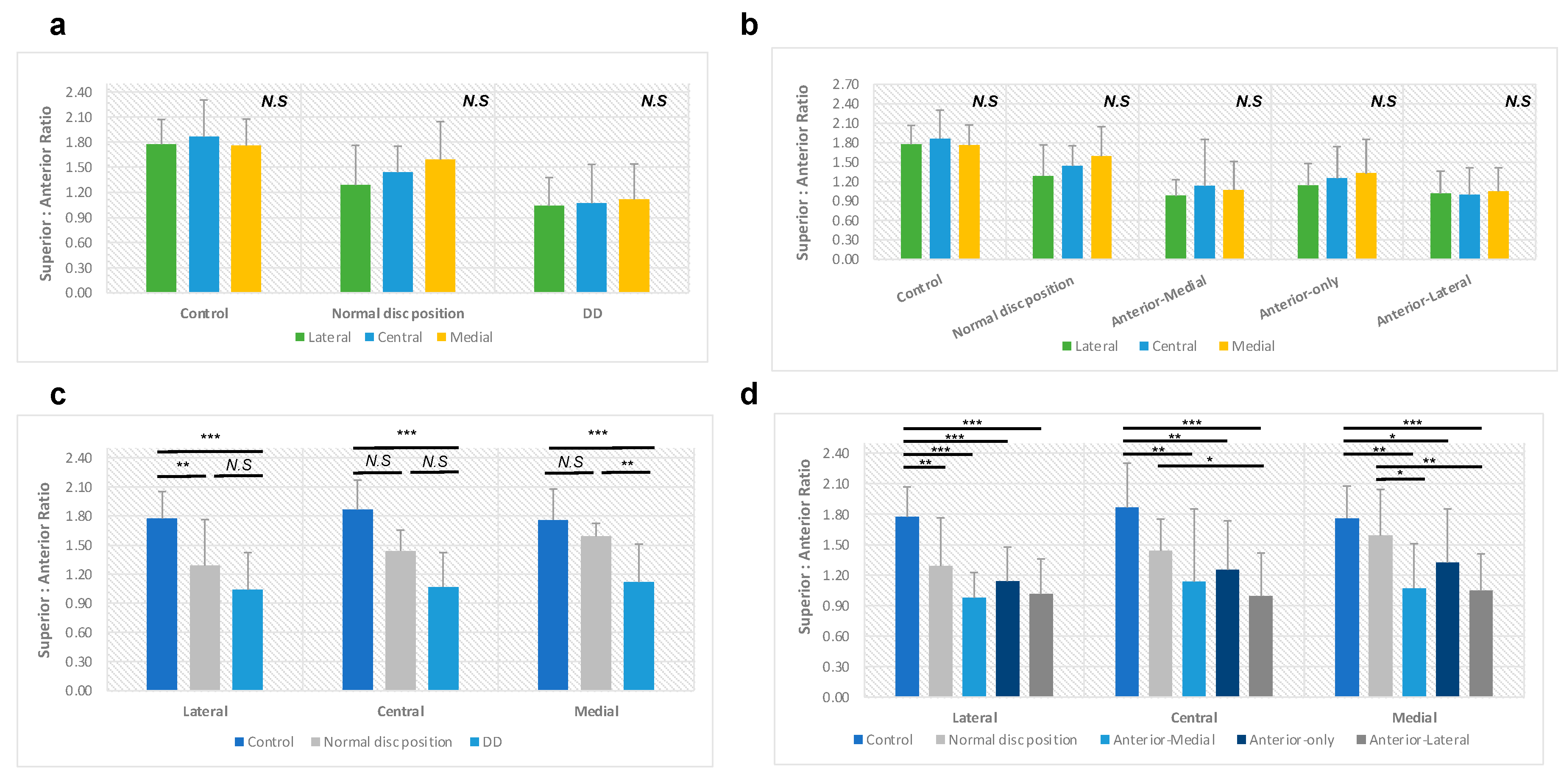
3.4. Superior-to-Anterior Joint Space Ratio (S-A Ratio)
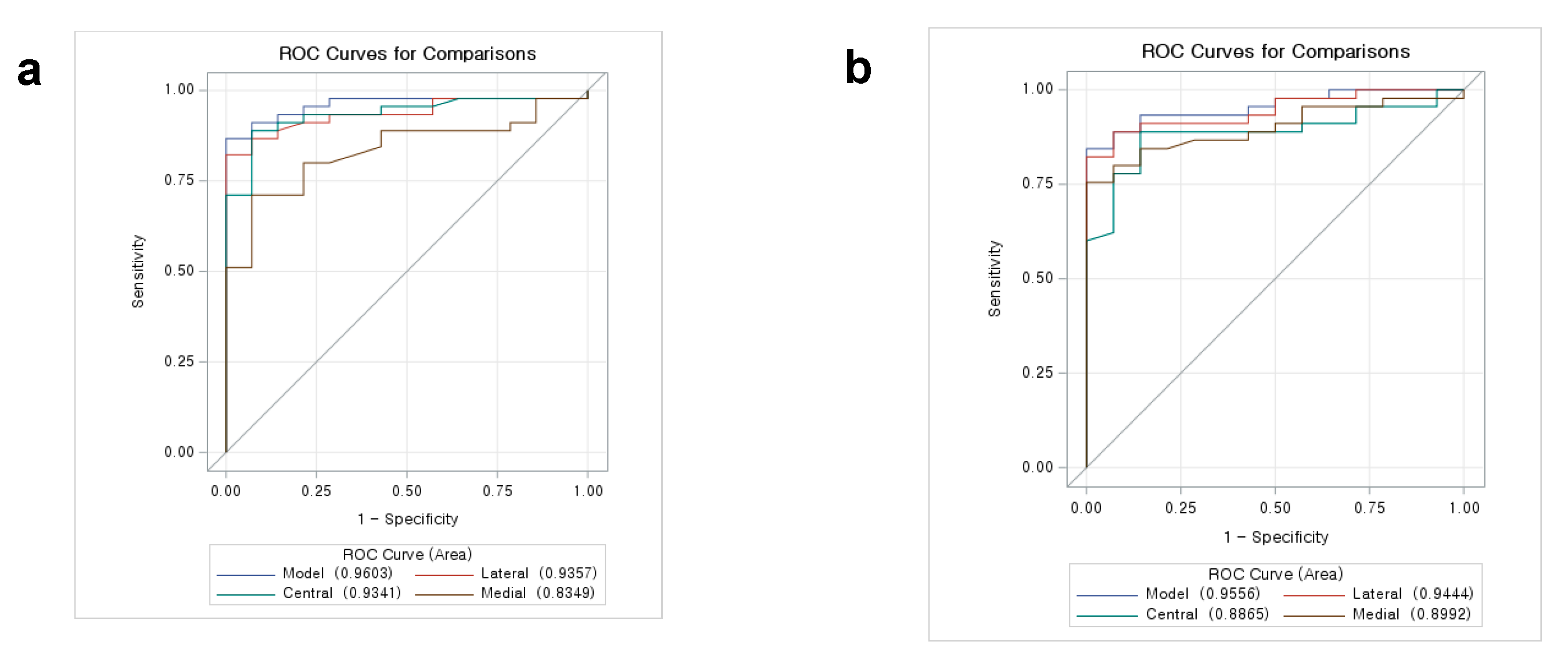
3.5. Receiver Operating Characteristic (ROC) Curve Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 8th ed.; Mosby: Maryland Heights, MO, USA, 2019. [Google Scholar]
- Singh, B.; Kumar, N.R.; Balan, A.; Nishan, M.; Haris, P.S.; Jinisha, M.; Denny, C.D. Evaluation of Normal Morphology of Mandibular Condyle: A Radiographic Survey. J. Clin. Imaging Sci. 2020, 10, 51. [Google Scholar] [CrossRef] [PubMed]
- Kimos, P.; Nebbe, B.; Heo, G.; Packota, G.; Major, P.W. Changes in temporomandibular joint sagittal disc position over time in adolescents: A longitudinal retrospective study. Am. J. Orthod. Dentofacial Orthop. 2009, 136, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Laskin, D.M. Temporomandibular disorders: A term past its time? J. Am. Dent. Assoc. 2008, 139, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, R.F.; Tallents, R.H.; Katzberg, R.W.; Murphy, W.C.; Moss, M.E.; Magalhaes, A.C.; Tavano, O. The prevalence of disc displacement in symptomatic and asymptomatic volunteers aged 6 to 25 years. J. Orofac. Pain. 1997, 11, 37–47. [Google Scholar] [PubMed]
- Wolford, L.M. Can orthodontic relapse be blamed on the temporomandibular joint? J. Orthod. Sci. 2014, 3, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Bryndahl, F.; Eriksson, L.; Legrell, P.E.; Isberg, A. Bilateral TMJ disk displacement induces mandibular retrognathia. J. Dent. Res. 2006, 85, 1118–1123. [Google Scholar] [CrossRef]
- Hu, Y.K.; Abdelrehem, A.; Yang, C.; Cai, X.Y.; Xie, Q.Y.; Sah, M.K. Changes in temporomandibular joint spaces after arthroscopic disc repositioning: A self-control study. Sci. Rep. 2017, 7, 45513. [Google Scholar] [CrossRef]
- Scrivani, S.J.; Keith, D.A.; Kaban, L.B. Temporomandibular disorders. N. Engl. J. Med. 2008, 359, 2693–2705. [Google Scholar] [CrossRef]
- Hashimoto, K.; Kawashima, S.; Kameoka, S.; Akiyama, Y.; Honjoya, T.; Ejima, K.; Sawada, K. Comparison of image validity between cone beam computed tomography for dental use and multidetector row helical computed tomography. Dentomaxillofac Radiol. 2007, 36, 465–471. [Google Scholar] [CrossRef]
- Tomas, X.; Pomes, J.; Berenguer, J.; Quinto, L.; Nicolau, C.; Mercader, J.M.; Castro, V. MR imaging of temporomandibular joint dysfunction: A pictorial review. Radiographics 2006, 26, 765–781. [Google Scholar] [CrossRef]
- Gateno, J.; Anderson, P.B.; Xia, J.J.; Horng, J.C.; Teichgraeber, J.F.; Liebschner, M.A. A comparative assessment of mandibular condylar position in patients with anterior disc displacement of the temporomandibular joint. J. Oral. Maxillofac. Surg. 2004, 62, 39–43. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, K.; Kawamura, A. Assessment of optimal condylar position with limited cone-beam computed tomography. Am. J. Orthod. Dentofacial Orthop. 2009, 135, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, K.; Kawamura, A. Disc displacement and changes in condylar position. Dentomaxillofac. Radiol. 2013, 42, 84227642. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Groupdagger. J. Oral. Facial Pain. Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Christie, K.F.; Boucher, N.; Chung, C.H. Effects of bonded rapid palatal expansion on the transverse dimensions of the maxilla: A cone-beam computed tomography study. Am. J. Orthod. Dentofac. Orthop. 2010, 137, S79–S85. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Hong, I.K.; An, J.S. Anterior joint space narrowing in patients with temporomandibular disorder. J. Orofac. Orthop. 2019, 80, 116–127. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, R.; Ikeda, K. Directional characteristics of incipient temporomandibular joint disc displacements: A magnetic resonance imaging study. Am. J. Orthod. Dentofacial Orthop. 2016, 149, 39–45. [Google Scholar] [CrossRef]
- Ikeda, K. A reference line on temporomandibular joint MRI. J. Prosthodont. 2013, 22, 603–607. [Google Scholar] [CrossRef]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef]
- Yin, J.; Mutiso, F.; Tian, L. Joint hypothesis testing of the area under the receiver operating characteristic curve and the Youden index. Pharm. Stat. 2021, 20, 657–674. [Google Scholar] [CrossRef]
- Karkazi, F.; Ozdemir, F. Temporomandibular Disorders: Fundamental Questions and Answers. Turk. J. Orthod. 2020, 33, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Flores-Mir, C.; Nebbe, B.; Heo, G.; Major, P.W. Longitudinal study of temporomandibular joint disc status and craniofacial growth. Am. J. Orthod. Dentofacial Orthop. 2006, 130, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Peroz, I.; Seidel, A.; Griethe, M.; Lemke, A.J. MRI of the TMJ: Morphometric comparison of asymptomatic volunteers and symptomatic patients. Quintessence Int. 2011, 42, 659–667. [Google Scholar] [PubMed]
- Brand, J.W.; Nielson, K.J.; Tallents, R.H.; Nanda, R.S.; Currier, G.F.; Owen, W.L. Lateral cephalometric analysis of skeletal patterns in patients with and without internal derangement of the temporomandibular joint. Am. J. Orthod. Dentofacial Orthop. 1995, 107, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Nebbe, B.; Major, P.W.; Prasad, N.G.; Grace, M.; Kamelchuk, L.S. TMJ internal derangement and adolescent craniofacial morphology: A pilot study. Angle Orthod. 1997, 67, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Nebbe, B.; Major, P.W.; Prasad, N.G. Adolescent female craniofacial morphology associated with advanced bilateral TMJ disc displacement. Eur. J. Orthod. 1998, 20, 701–712. [Google Scholar] [CrossRef]
- Nebbe, B.; Major, P.W.; Prasad, N. Female adolescent facial pattern associated with TMJ disk displacement and reduction in disk length: Part I. Am. J. Orthod. Dentofacial Orthop. 1999, 116, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Nebbe, B.; Major, P.W.; Prasad, N.G. Male adolescent facial pattern associated with TMJ disk displacement and reduction in disk length: Part II. Am. J. Orthod. Dentofacial Orthop. 1999, 116, 301–307. [Google Scholar] [CrossRef]
- Yang, I.H.; Moon, B.S.; Lee, S.P.; Ahn, S.J. Skeletal differences in patients with temporomandibular joint disc displacement according to sagittal jaw relationship. J. Oral. Maxillofac. Surg. 2012, 70, e349–e360. [Google Scholar] [CrossRef]
- Nebbe, B.; Major, P.W. Prevalence of TMJ disc displacement in a pre-orthodontic adolescent sample. Angle Orthod. 2000, 70, 454–463. [Google Scholar] [CrossRef]
- Ikeda, K.; Kawamura, A.; Ikeda, R. Prevalence of disc displacement of various severities among young preorthodontic population: A magnetic resonance imaging study. J. Prosthodont. 2014, 23, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Barghan, S.; Tetradis, S.; Mallya, S. Application of cone beam computed tomography for assessment of the temporomandibular joints. Aust. Dent. J. 2012, 57 (Suppl. S1), 109–118. [Google Scholar] [CrossRef] [PubMed]
- Talmaceanu, D.; Lenghel, L.M.; Bolog, N.; Hedesiu, M.; Buduru, S.; Rotar, H.; Baciut, M.; Baciut, G. Imaging modalities for temporomandibular joint disorders: An update. Clujul Med. 2018, 91, 280–287. [Google Scholar] [CrossRef] [PubMed]
| Myalgia | Local Myalgia | Myofascial Pain | Myofascial Pain with Referral | Arthralgia | Headache Attributed to TMD | Disc Displacement (DD) with Reduction | DD with Reduction with Intermittent Locking | DD without Reduction with Limited Opening | DD without Reduction without Limited Opening | Degenerative Joint Disease | Subluxation | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | 0 | 1 | 10 | 0 | 0 | 6 | 0 | 0 | 0 | 1 | 1 | 0 |
| Experimental | 0 | 6 | 27 | 2 | 0 | 6 | 8 | 15 | 5 | 3 | 12 | 0 |
| N | Percentage | N | Percentage | |||
|---|---|---|---|---|---|---|
| Control group | 14 | 21.2% | ||||
| Experimental group | Normal disc position (N) | 7 | 10.6% | |||
| Disc Displacement (DD) | 45 | 68.2% | Anterior-Medial | 4 | 8.9% | |
| Anterior-only | 11 | 24.4% | ||||
| Anterior-Lateral | 30 | 66.7% | ||||
| Total | 66 | 100.0% |
| Posterior: Anterior Ratio | Lateral | Central | Medial | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | S.D. | p | Mean | S.D. | p | Mean | S.D. | p | Mean | S.D. | p | ||
| Control group | 1.55 | 0.28 | <0.001 abcd | 1.42 | 0.30 | <0.001 abcde | 1.39 | 0.32 | <0.001 abdef | 1.46 | 0.21 | <0.001 abcdef | |
| Experimental group | Normal disc position | 1.06 | 0.48 | 0.91 | 0.21 | 1.01 | 0.13 | 0.99 | 0.23 | ||||
| Disc displacement | 0.89 | 0.38 | 0.77 | 0.35 | 0.91 | 0.39 | 0.86 | 0.30 | |||||
| Anterior-Medial | 0.89 | 0.25 | 0.64 | 0.11 | 0.64 | 0.06 | 0.72 | 0.08 | |||||
| Anterior-only | 0.99 | 0.56 | 0.95 | 0.51 | 1.15 | 0.50 | 1.03 | 0.44 | |||||
| Anterior-Lateral | 0.85 | 0.32 | 0.72 | 0.29 | 0.86 | 0.34 | 0.81 | 0.24 | |||||
| Superior: Anterior Ratio | Lateral | Central | Medial | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | S.D. | p | Mean | S.D. | p | Mean | S.D. | p | Mean | S.D. | p | ||
| Control group | 1.77 | 0.29 | <0.001 abcd | 1.87 | 0.44 | <0.001 bcdf | 1.76 | 0.31 | <0.001 bcdef | 1.80 | 0.27 | <0.001 abcdf | |
| Experimental group | Normal disc position | 1.29 | 0.47 | 1.44 | 0.31 | 1.59 | 0.45 | 1.44 | 0.33 | ||||
| Disc displacement | 1.04 | 0.33 | 1.07 | 0.47 | 1.12 | 0.42 | 1.08 | 0.35 | |||||
| Anterior-Medial | 0.98 | 0.25 | 1.13 | 0.72 | 1.07 | 0.44 | 1.06 | 0.46 | |||||
| Anterior-only | 1.14 | 0.34 | 1.25 | 0.48 | 1.32 | 0.53 | 1.24 | 0.35 | |||||
| Anterior-Lateral | 1.01 | 0.34 | 0.99 | 0.42 | 1.05 | 0.36 | 1.02 | 0.34 | |||||
| Cut-Off Point | Sensitivity | Specificity | Youden’s Index | AUC | 95% CI | |
|---|---|---|---|---|---|---|
| Lateral poles | 1.678 | 0.911 | 0.929 | 0.840 | 0.94 | 0.87–1.00 |
| 1.641 | 0.889 | 0.929 | 0.817 | |||
| 1.527 | 0.867 | 0.929 | 0.795 | |||
| 1.408 | 0.778 | 1.000 | 0.778 | |||
| 1.488 | 0.844 | 0.929 | 0.773 | |||
| 1.692 | 0.911 | 0.857 | 0.768 | |||
| 1.386 | 0.756 | 1.000 | 0.756 | |||
| 1.430 | 0.822 | 0.929 | 0.751 | |||
| 1.381 | 0.733 | 1.000 | 0.733 | |||
| 1.428 | 0.800 | 0.929 | 0.729 | |||
| 1.348 | 0.711 | 1.000 | 0.711 | |||
| 1.409 | 0.778 | 0.929 | 0.706 | |||
| Central poles | 1.339 | 0.867 | 0.929 | 0.795 | 0.93 | 0.86–1.00 |
| 1.467 | 0.933 | 0.857 | 0.790 | |||
| 1.224 | 0.844 | 0.929 | 0.773 | |||
| 1.452 | 0.911 | 0.857 | 0.768 | |||
| 1.216 | 0.822 | 0.929 | 0.751 | |||
| 1.434 | 0.889 | 0.857 | 0.746 | |||
| 1.572 | 0.956 | 0.786 | 0.741 | |||
| 1.209 | 0.800 | 0.929 | 0.729 | |||
| 1.374 | 0.867 | 0.857 | 0.724 | |||
| 1.476 | 0.933 | 0.756 | 0.719 | |||
| 1.186 | 0.778 | 0.929 | 0.706 |
| Cut-Off Point | Sensitivity | Specificity | Youden’s Index | AUC | 95% CI | |
|---|---|---|---|---|---|---|
| Lateral poles | 1.733 | 0.911 | 0.929 | 0.840 | 0.94 | 0.88–1.00 |
| 1.666 | 0.889 | 0.929 | 0.817 | |||
| 1.592 | 0.867 | 0.929 | 0.795 | |||
| 1.565 | 0.844 | 0.929 | 0.773 | |||
| 1.769 | 0.911 | 0.857 | 0.768 | |||
| 1.398 | 0.756 | 1.000 | 0.756 | |||
| 1.528 | 0.822 | 0.929 | 0.751 | |||
| 1.394 | 0.733 | 1.000 | 0.733 | |||
| 1.521 | 0.800 | 0.929 | 0.729 | |||
| 1.375 | 0.711 | 1.000 | 0.711 | |||
| 1.520 | 0.778 | 0.929 | 0.706 | |||
| Medial poles | 1.916 | 0.822 | 0.929 | 0.751 | 0.91 | 0.84–0.99 |
| 2.028 | 0.889 | 0.857 | 0.746 | |||
| 1.835 | 0.800 | 0.929 | 0.729 | |||
| 2.028 | 0.867 | 0.857 | 0.724 | |||
| 1.829 | 0.778 | 0.929 | 0.706 | |||
| 1.961 | 0.844 | 0.857 | 0.702 |
| Cut-Off Point | Sensitivity | Specificity | Youden’s Index | AUC | 95% CI | |
|---|---|---|---|---|---|---|
| Total | 1.294 | 0.844 | 1.000 | 0.844 | 0.96 | 0.90–1.00 |
| P-A | 1.235 | 0.822 | 1.000 | 0.822 | ||
| 1.357 | 0.889 | 0.929 | 0.817 | |||
| 1.508 | 0.956 | 0.857 | 0.813 | |||
| 1.182 | 0.800 | 1.000 | 0.800 | |||
| 1.316 | 0.867 | 0.929 | 0.795 | |||
| 1.436 | 0.933 | 0.857 | 0.790 | |||
| 1.180 | 0.778 | 1.000 | 0.778 | |||
| 1.305 | 0.844 | 0.929 | 0.773 | |||
| 1.427 | 0.911 | 0.857 | 0.768 | |||
| 1.167 | 0.756 | 1.000 | 0.756 | |||
| 1.382 | 0.889 | 0.857 | 0.746 | |||
| 1.512 | 0.956 | 0.786 | 0.741 | |||
| 1.144 | 0.733 | 1.000 | 0.733 | |||
| 1.129 | 0.711 | 1.000 | 0.711 | |||
| Total | 1.492 | 0.800 | 1.000 | 0.800 | 0.93 | 0.86–0.99 |
| S-A | 1.769 | 0.867 | 0.929 | 0.795 | ||
| 1.461 | 0.778 | 1.000 | 0.778 | |||
| 1.707 | 0.844 | 0.929 | 0.773 | |||
| 1.899 | 0.911 | 0.857 | 0.768 | |||
| 1.367 | 0.756 | 1.000 | 0.756 | |||
| 1.653 | 0.822 | 0.929 | 0.751 | |||
| 1.832 | 0.889 | 0.857 | 0.746 | |||
| 1.361 | 0.733 | 1.000 | 0.733 | |||
| 1.571 | 0.800 | 0.929 | 0.729 | |||
| 1.814 | 0.867 | 0.857 | 0.724 | |||
| 1.353 | 0.711 | 1.000 | 0.711 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, W.; Jeon, H.H.; Kim, S.; Dayo, A.; Mupparapu, M.; Boucher, N.S. Correlation between TMJ Space Alteration and Disc Displacement: A Retrospective CBCT and MRI Study. Diagnostics 2024, 14, 44. https://doi.org/10.3390/diagnostics14010044
Yu W, Jeon HH, Kim S, Dayo A, Mupparapu M, Boucher NS. Correlation between TMJ Space Alteration and Disc Displacement: A Retrospective CBCT and MRI Study. Diagnostics. 2024; 14(1):44. https://doi.org/10.3390/diagnostics14010044
Chicago/Turabian StyleYu, Wenjing, Hyeran Helen Jeon, Soriul Kim, Adeyinka Dayo, Muralidhar Mupparapu, and Normand S. Boucher. 2024. "Correlation between TMJ Space Alteration and Disc Displacement: A Retrospective CBCT and MRI Study" Diagnostics 14, no. 1: 44. https://doi.org/10.3390/diagnostics14010044
APA StyleYu, W., Jeon, H. H., Kim, S., Dayo, A., Mupparapu, M., & Boucher, N. S. (2024). Correlation between TMJ Space Alteration and Disc Displacement: A Retrospective CBCT and MRI Study. Diagnostics, 14(1), 44. https://doi.org/10.3390/diagnostics14010044






