Post-Coronary Artery Bypass Grafting Outcomes of Patients with/without Type-2 Diabetes Mellitus and Chronic Kidney Disease Treated with SGLT2 Inhibitor Dapagliflozin: A Single-Center Experience Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Overview of Study Coordinates and Phases
2.2. Inclusion and Exclusion Criteria
2.3. Treatment and Rehabilitation
2.4. Patient Data Collected and Definitions
- General patient characteristics and past medical history;
- Clinical, paraclinical, echocardiographic, and laboratory findings in phase I and then again in phase II.
- Heart failure upon admission based on left ventricular ejection fraction values: heart failure with reduced ejection fraction (severely reduced if EF ≤ 30%, moderately reduced if EF is between 31% and 40%, mildly reduced if EF is between 41% and 49%), and heart failure with preserved ejection fraction if EF ≥ 50% [18];
- Type-2 diabetes mellitus or prediabetes as had been diagnosed prior to the study (part of the patient’s medical history data), or prediabetes diagnosed incidentally based on glycated hemoglobin levels between 5.7% and 6.4% at the time of the surgery.
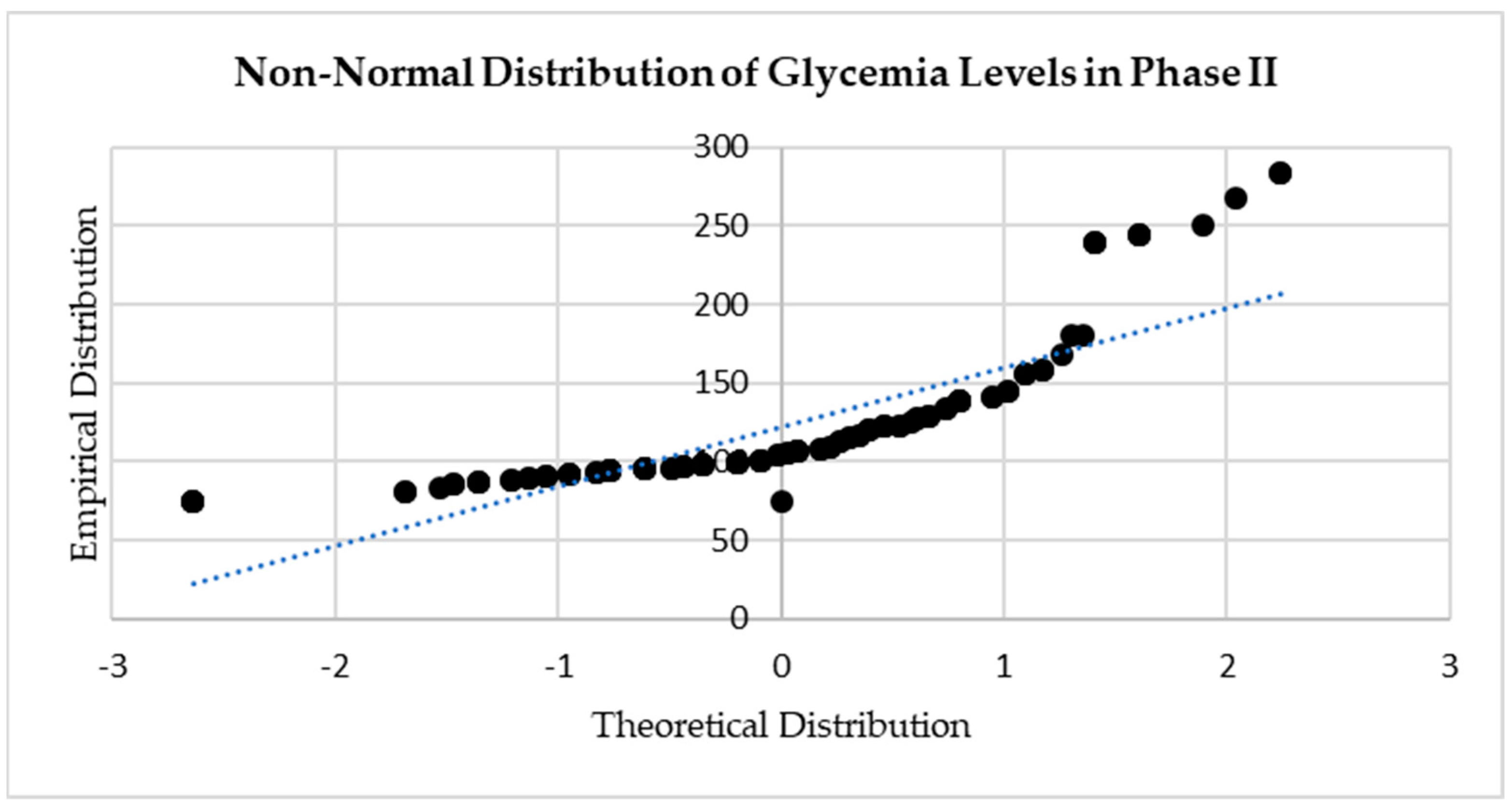
2.5. Organization of Database and Statistical Analysis
- Patients with established type-2 diabetes mellitus (T2DM):
- With chronic kidney disease as well (T2DM+CKD);
- Without chronic kidney disease (T2DM−CKD).
- Patients with established or incidental prediabetes (PreD):
- With chronic kidney disease as well (PreD+CKD);
- Without chronic kidney disease (PreD−CKD).
3. Results
3.1. General Patient Characteristics and Relevant Past Medical History
3.2. Echocardiographic and Laboratory Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Neumann, F.-J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.-P.; Falk, V.; Head, S.J.; et al. ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Farkouh, M.E.; Yanagawa, B.; Fitchett, D.H.; Ahsan, M.R.; Ruel, M.; Sud, S.; Gupta, M.; Singh, S.; Gupta, N.; et al. Comparison of coronary artery bypass surgery and percutaneous coronary intervention in patients with diabetes: A meta-analysis of randomised controlled trials. Lancet Diabetes Endocrinol. 2013, 1, 317–328. [Google Scholar] [CrossRef] [PubMed]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Biomath, D.; Devins, T.; Johansen, O.E.; et al. EMPA-REG OUTCOME Investigators. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research. Guidance for Industry. Diabetes Mellitus—Evaluating Cardiovascular Risk in New Antidiabetic Therapies to Treat Type 2 Diabetes. Available online: https://www.fda.gov/media/71297/download (accessed on 15 October 2023).
- American Diabetes Association. Pharmacologic approaches to glycemic treatment. Sec. 8. In Standards of Medical Care in Diabetes. Diabetes Care 2017, 40 (Suppl. 1), 64–74. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Mazer, C.D.; Fitchett, D.; Inzucchi, S.E.; Pfarr, E.; George, J.T.; Zinman, B. Empagliflozin reduces cardiovascular events, mortality and renal events in participants with type 2 diabetes after coronary artery bypass graft surgery: Subanalysis of the EMPA-REG OUTCOME® randomised trial. Diabetologia 2018, 61, 1712–1723. [Google Scholar] [CrossRef] [PubMed]
- Eikelboom, R.; Amir, T.; Gupta, S.; Whitlock, R.P. Optimal medical therapy after coronary artery bypass grafting: A primer for surgeons. Curr. Opin. Cardiol. 2021, 36, 609–615. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Raz, I.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; Silverman, M.G.; Zelniker, T.A.; Kuder, J.F.; Murphy, S.A.; et al. DECLARE–TIMI 58 Investigators. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2019, 380, 347–357. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; DeMets, D.L.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Langkilde, A.M.; Martinez, F.A.; Bengtsson, O.; Ponikowski, P.; Sabatine, M.S.; et al. DAPA-HF Committees and Investigators. A trial to evaluate the effect of the sodium-glucose co-transporter 2 inhibitor dapagliflozin on morbidity and mortality in patients with heart failure and reduced left ventricular ejection fraction (DAPA-HF). Eur. J. Heart Fail. 2019, 21, 665–675. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. DAPA-HF Trial Committees and Investigators.. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef]
- Petrie, M.C.; Verma, S.; Docherty, K.F.; Inzucchi, S.E.; Anand, I.; Belohlávek, J.; Böhm, M.; Chiang, C.-E.; Chopra, V.K.; de Boer, R.A.; et al. Effect of Dapagliflozin on Worsening Heart Failure and Cardiovascular Death in Patients with Heart Failure with and Without Diabetes. JAMA 2020, 323, 1353–1368. [Google Scholar] [CrossRef]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. EMPEROR-Reduced Trial Investigators. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef] [PubMed]
- Braunwald, E. Diabetes, heart failure, and renal dysfunction: The vicious circles. Prog. Cardiovasc. Dis. 2019, 62, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Zelniker, T.A.; Wiviott, S.D.; Raz, I.; Im, K.; Goodrich, E.; Bonaca, M.P.; Mosenzon, O.; Kato, E.; Cahn, A.; Furtado, R.H.M.; et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: A systematic review and meta-analysis of cardiovascular outcome trials. Lancet 2019, 393, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Zelniker, T.A.; Braunwald, E. Clinical Benefit of Cardiorenal Effects of Sodium-Glucose Cotransporter 2 Inhibitors: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 435–447. [Google Scholar] [CrossRef] [PubMed]
- Perkovic, V.; Jardine, M.J.; Neal, B.; Bompoint, S.; Heerspink, H.J.L.; Charytan, D.M.; Edwards, R.; Agarwal, R.; Bakris, G.; Bull, S.; et al. CREDENCE Trial Investigators. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N. Engl. J. Med. 2019, 380, 2295–2306. [Google Scholar] [CrossRef]
- Zelniker, T.A.; Raz, I.; Mosenzon, O.; Dwyer, J.P.; Heerspink, H.H.; Cahn, A.; Goodrich, E.L.; Im, K.; Bhatt, D.L.; Leiter, L.A.; et al. Effect of Dapagliflozin on Cardiovascular Outcomes According to Baseline Kidney Function and Albuminuria Status in Patients With Type 2 Diabetes: A Prespecified Secondary Analysis of a Randomized Clinical Trial. JAMA Cardiol. 2021, 6, 801–810. [Google Scholar] [CrossRef]
- Al Namat, R.; Al Namat, D.; Ciocoiu, M.; Hînganu, M.V.; Șorodoc, L.; Șorodoc, V.; Foia, L.G.; Florea, L.; Vlad, C.; Tănasă, A.; et al. H-FABP Levels and Psycho-Emotional Improvement of CABG Patients during Cardiac Rehabilitation. J. Cardiovasc. Dev. Dis. 2022, 9, 242. [Google Scholar] [CrossRef]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of Cardiovascular Disease in Type 2 Diabetes: A Systematic Literature Review of Scientific Evidence from across the World in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef]
- Butnariu, L.I.; Florea, L.; Badescu, M.C.; Țarcă, E.; Costache, I.-I.; Gorduza, E.V. Etiologic Puzzle of Coronary Artery Disease: How Important Is Genetic Component? Life 2022, 12, 865. [Google Scholar] [CrossRef]
- Sardu, C.; D’onofrio, N.; Torella, M.; Portoghese, M.; Loreni, F.; Mureddu, S.; Signoriello, G.; Scisciola, L.; Barbieri, M.; Rizzo, M.R.; et al. Pericoronary Fat Inflammation and Major Adverse Cardiac Events (MACE) in Prediabetic Patients with Acute Myocardial Infarction: Effects of Metformin. Cardiovasc. Diabetol. 2019, 18, 126. [Google Scholar] [CrossRef]
- Marfella, R.; Sardu, C.; Balestrieri, M.L.; Siniscalchi, M.; Minicucci, F.; Signoriello, G.; Calabrò, P.; Mauro, C.; Pieretti, G.; Coppola, A.; et al. Effects of Incretin Treatment on Cardiovascular Outcomes in Diabetic STEMI-Patients with Culprit Obstructive and Multivessel Non Obstructive-Coronary-Stenosis. Diabetol. Metab. Syndr. 2018, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Moisa, S.M.; Trandafir, L.M.; Brinza, C.; Miron, I.C.; Tarca, E.; Butnariu, L.I.; Burlacu, A. Current Antithrombotic Therapy Strategies in Children with a Focus on Off-Label Direct Oral Anticoagulants-A Narrative Review. Children 2022, 9, 1093. [Google Scholar] [CrossRef]
- Wan, S.; LeClerc, J.-L.; Vincent, J.-L. Inflammatory Response to Cardiopulmonary Bypass: Mechanisms Involved and Possible Therapeutic Strategies. Chest 1997, 112, 676–692. [Google Scholar] [CrossRef] [PubMed]
- Anastasiadis, K.; Murkin, J.; Antonitsis, P.; Bauer, A.; Ranucci, M.; Gygax, E.; Schaarschmidt, J.; Fromes, Y.; Philipp, A.; Eberle, B.; et al. Use of Minimal Invasive Extracorporeal Circulation in Cardiac Surgery: Principles, Definitions and Potential Benefits. A Position Paper from the Minimal Invasive Extra-corporeal Technologies International Society (MiECTiS). Interact Cardiovasc. Thorac. Surg. 2016, 22, 647–662. [Google Scholar] [CrossRef]
- Winkler, B.; Heinisch, P.P.; Zuk, G.; Zuk, K.; Gahl, B.; Jenni, H.-J.; Kadner, A.; Huber, C.; Carrel, T. Minimally Invasive Extracorporeal Circulation: Excellent Outcome and Life Expectancy after Coronary Artery Bypass Grafting Surgery. Swiss Med. Wkly. 2017, 147, w14474. [Google Scholar] [CrossRef][Green Version]
- Toyama, T.; Neuen, B.L.; Jun, M.; Ohkuma, T.; Neal, B.; Jardine, M.J.; Heerspink, H.L.; Wong, M.G.; Ninomiya, T.; Wada, T.; et al. Effect of SGLT2 inhibitors on cardiovascular, renal and safety outcomes in patients with type 2 diabetes mellitus and chronic kidney disease: A systematic review and meta-analysis. Diabetes Obes. Metab. 2019, 21, 1237–1250. [Google Scholar] [CrossRef] [PubMed]
- Bakaeen, F. CABG: A continuing evolution. Cleve. Clin. J. Med. 2017, 84, 15–19. [Google Scholar] [CrossRef]
- Olgoye, A.M.; Samadi, A.; Jamalian, S.A. Effects of a home-based exercise intervention on cardiac biomarkers, liver enzymes, and cardiometabolic outcomes in CABG and PCI patients. J. Res. Med. Sci. 2021, 26, 5. [Google Scholar]
- Wilson, S.; Mone, P.; Kansakar, U.; Jankauskas, S.S.; Donkor, K.; Adebayo, A.; Varzideh, F.; Eacobacci, M.; Gambardella, J.; Lombardi, A.; et al. Diabetes and restenosis. Cardiovasc. Diabetol. 2022, 21, 23. [Google Scholar] [CrossRef]
- Liu, D.; Cui, X.; Luo, X.; Sun, Z.; Xu, B.; Qiao, S.; Yuan, J. Long-term outcomes of percutaneous coronary intervention in grafts and native vessels in coronary artery bypass grafting patients with diabetes mellitus. J. Thorac. Dis. 2019, 11, 4798–4806. [Google Scholar] [CrossRef]
- Kologrivova, I.; Shtatolkina, M.; Suslova, T.; Ryabov, V. Cells of the Immune System in Cardiac Remodeling: Main Players in Resolution of Inflammation and Repair After Myocardial Infarction. Front. Immunol. 2021, 12, 664457. [Google Scholar] [CrossRef] [PubMed]
- Volpe, M.; Pedicino, D. SGLT2 inhibitors DELIVER benefits in heart failure independently of ejection fraction and diabetes: End of the line or need for new studies? Eur. Heart J. 2022, 43, 4614–4615. [Google Scholar] [CrossRef] [PubMed]

| General Data | Overall (N = 120) | T2DM (N = 65) | T2DM+CKD (N = 18) | T2DM−CKD (N = 47) | PreD (N = 55) | PreD+CKD (N = 17) | PreD−CKD (N = 38) |
|---|---|---|---|---|---|---|---|
| Mean age (years) | 65.93 | 67.25 | 70.22 | 66.11 | 64.36 | 65.47 | 63.87 |
| Median age (years) | 67 | 67 | 70 | 65 | 67 | 66 | 67.5 |
| Age range (years) | 41–85 | 58–85 | 58–80 | 46–85 | 55–77 | 55–75 | 41–77 |
| Male sex | 91 (75.83%) | 53 (81.54%) | 16 (88.89%) | 37 (78.72%) | 38 (69.09%) | 15 (88.24%) | 23 (60.53%) |
| Urban | 106 (88.33%) | 55 (84.62%) | 17 (94.44%) | 38 (80.85%) | 51 (92.73%) | 16 (94.12%) | 35 (92.11%) |
| Smokers | 73 (60.83%) | 44 (67.69%) | 12 (66.67%) | 32 (68.09%) | 29 (52.73%) | 11 (64.71%) | 18 (47.37%) |
| BMI (kg/m2) | 30.12 | 30 | 30.78 | 29.70 | 28.73 | 30.12 | 28.11 |
| Hypertension | 111 (92.5%) | 65 (100%) | 18 (100%) | 47 (100%) | 46 (83.64%) | 15 (88.24%) | 31 (81.58%) |
| No history | 9 (7.5%) | - | - | - | 9 (16.36%) | 2 (11.76%) | 7 (18.42%) |
| Stage 1 | 7 (5.83%) | 2 (3.08%) | - | 2 (4.26%) | 5 (9.09%) | 2 (11.76%) | 3 (7.89%) |
| Stage 2 | 22 (18.33%) | 14 (21.54%) | 2 (11.11%) | 12 (25.53%) | 8 (14.55%) | 2 (11.76%) | 6 (15.79%) |
| Stage 3 | 82 (68.33%) | 49 (75.38%) | 16 (88.89%) | 33 (70.21%) | 33 (60.00%) | 11 (64.71%) | 22 (57.89%) |
| Heart failure | 87 (72.5%) | 49 (75.38%) | 12 (66.67%) | 37 (78.72%) | 38 (69.09%) | 15 (88.24%) | 23 (60.53%) |
| No history | 33 (27.5%) | 16 (24.62%) | 6 (33.33%) | 10 (21.28%) | 17 (30.91%) | 2 (11.76%) | 15 (39.47%) |
| Class I | 6 (5%) | 2 (3.08%) | 1 (5.56%) | 1 (2.13%) | 4 (7.27%) | 1 (5.88%) | 3 (7.89%) |
| Class II | 33 (27.5%) | 20 (30.77%) | 3 (16.67%) | 17 (36.17%) | 13 (23.64%) | 6 (35.29%) | 7 (18.42%) |
| Class III | 48 (40%) | 27 (41.54%) | 8 (44.44%) | 19 (40.43%) | 21 (38.18%) | 8 (47.06%) | 13 (34.21%) |
| Peripheral artery disease | 32 (26.67%) | 24 (36.92%) | 10 (55.56%) | 14 (29.79%) | 8 (14.55%) | 4 (23.53%) | 4 (10.53%) |
| Chronic kidney disease | 35 (29.17%) | 18 (27.69%) | 18 (100%) | - | 17 (30.91%) | 17 (100%) | - |
| Stage 1 | 28 (23.33%) | 15 (23.08%) | 15 (83.33%) | - | 13 (23.64%) | 13 (76.47%) | - |
| Stage 2 | 3 (2.5%) | 3 (4.62%) | 3 (16.67%) | - | - | - | - |
| Stage 3 | 4 (3.33%) | - | - | - | 4 (7.27%) | 4 (23.53%) | - |
| Stage 4 | - | - | - | - | - | - | - |
| Stroke | 6 (5%) | - | - | 2 (4.26%) | 4 (7.27%) | - | 4 (10.53%) |
| Studied Variable | Overall (N = 120) | p Value | T2DM (N = 65) | p Value | T2DM+ CKD (N = 18) | p Value | T2DM−CKD (N = 47) | p Value | PreD (N = 55) | p Value | PreD+ CKD (N = 17) | p Value | PreD− CKD (N = 38) | p Value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cardiac status | ||||||||||||||
| EF I | 43.5 | 0.000 | 44.77 | 0.000 | 44.22 | 0.000 | 44.98 | 0.000 | 41.93 | 0.000 | 47.59 | 0.000 | 39.39 | 0.000 |
| EF II | 51.9 | 51.75 | 51.39 | 51.89 | 52.07 | 53.65 | 51.37 | |||||||
| Δ EF | ↑ 8.43 | ↑ 6.98 | ↑ 7.17 | ↑ 6.92 (c) | ↑ 10.14 (b) | ↑ 6.06 (c)(c) | ↑ 11.98 (c)(b)(b) | |||||||
| FS I | 26.08 | 0.074 | 26.22 | 0.722 | 25.44 | 0.143 | 26.51 | 0.967 | 25.93 | 0.025 | 28.29 | 0.475 | 24.87 | 0.020 |
| FS II | 27.57 | 26.62 | 26.72 | 26.57 | 28.69 | 30.24 | 28.00 | |||||||
| Δ FS | ↑ 1.48 | ↑ 0.40 | ↑ 1.28 | ↑ 0.06 (c) | ↑ 2.76 (c) | ↑ 1.94 (c)(b) | ↑ 3.13 (c)(b)(c) | |||||||
| LVMi I | 143.31 | 0.000 | 150.29 | 0.000 | 167.94 | 0.000 | 143.53 | 0.000 | 135.05 | 0.000 | 119.94 | 0.000 | 141.82 | 0.000 |
| LVMi II | 119.98 | 128.74 | 142.83 | 123.34 | 109.64 | 97.76 | 114.95 | |||||||
| Δ LVMi | ↓ 23.33 | ↓ 21.55 | ↓ 25.11 | ↓ 20.19 (c) | ↓ 25.414 (c) | ↓ 22.18 (c)(c) | ↓ 26.87 (c)(b)(c) | |||||||
| Myocardial cytolytic enzymes | ||||||||||||||
| H-FABP I | 68.40 | 0.000 | 59.29 | 0.000 | 53.09 | 0.000 | 61.67 | 0.000 | 79.16 | 0.000 | 85.15 | 0.000 | 76.48 | 0.000 |
| H-FABP II | 4.82 | 4.81 | 4.74 | 4.83 | 4.83 | 5.52 | 4.53 | |||||||
| Δ H-FABP | ↓ 63.58 | ↓ 54.48 | ↓ 48.35 | ↓ 56.83 (b) | ↓ 74.33 (b) | ↓ 79.63 (b)(b) | ↓ 71.95 (b)(b)(c) | |||||||
| hs-cTn I | 361,375 | 0.000 | 357,076.9 | 0.003 | 321,722.2 | 0.000 | 370,617 | 0.173 | 366,454.5 | 0.012 | 378,882.4 | 0.047 | 360,894.74 | 0.102 |
| hs-cTn II | 316,916.7 | 316,630.8 | 239,222.2 | 346,276.6 | 317,254.5 | 305,588.2 | 322,473.68 | |||||||
| Δ Troponin | ↓ 44,458 | ↓ 40,446 | ↓ 82,500 | ↓ 24,340 (b) | ↓ 49,200 (c) | ↓ 73,294 (c)(a) | ↓ 3842 (a)(c)(a) | |||||||
| Studied Variable | Overall (N = 120) | p Value | T2DM (N = 65) | p Value | T2DM+ CKD (N = 18) | p Value | T2DM− CKD (N = 47) | p Value | PreD (N = 55) | p Value | PreD+ CKD (N = 17) | p Value | PreD− CKD (N = 38) | p Value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diabetes biomarkers | ||||||||||||||
| HbA1c I | 6.54 | 0.000 | 7.06 | 0.000 | 7.011 | 0.000 | 7.08 | 0.000 | 5.92 | 0.000 | 5.66 | 0.014 | 6.03 | 0.000 |
| HbA1c II | 5.55 | 6.06 | 6.083 | 6.048 | 4.95 | 4.98 | 4.94 | |||||||
| Δ HbA1c | ↓ 0.99 | ↓ 1.0 | ↓ 0.93 | ↓ 1.03 (c) | ↓ 0.97 (c) | ↓ 0.68 (c)(c) | ↓ 1.10 (c)(c)(b) | |||||||
| Glycemia I | 138.53 | 0.000 | 164.75 | 0.000 | 165.89 | 0.089 | 164.32 | 0.000 | 107.55 | 0.000 | 104.12 | 0.616 | 109.08 | 0.000 |
| Glycemia II | 120.63 | 141.77 | 157.78 | 135.64 | 95.65 | 102.24 | 92.71 | |||||||
| Δ Glycemia | ↓ 17.90 | ↓ 22.99 | ↓ 8.11 | ↓ 28.68 (c) | ↓ 11.89 (b) | ↓ 1.88 (a)(a) | ↓ 16.37 (b)(b)(a) | |||||||
| Kidney function | ||||||||||||||
| MDRD-GFR I | 65.50 | 0.000 | 65.20 | 0.000 | 68.15 | 0.000 | 64.07 | 0.001 | 65.85 | 0.000 | 64.75 | 0.000 | 66.35 | 0.003 |
| MDRD-GFR II | 77.01 | 75.54 | 87.07 | 71.12 | 78.76 | 79.64 | 78.36 | |||||||
| Δ MDRD-GFR | ↑ 11.51 | ↑ 10.34 | ↑ 18.93 | ↑ 7.05 (b) | ↑ 12.91 (c) | ↑ 14.89 (c)(b) | ↑ 12.01 (c)(c)(c) | |||||||
| Urea I | 45.42 | 0.000 | 42.91 | 0.191 | 51.72 | 0.403 | 39.53 | 0.327 | 48.38 | 0.000 | 45.41 | 0.000 | 49.71 | 0.001 |
| Urea II | 41.45 | 41.23 | 49.17 | 38.19 | 41.71 | 39.24 | 42.82 | |||||||
| Δ Urea | ↓ 3.97 | ↓ 1.68 | ↓ 2.56 | ↓ 1.34 (c) | ↓ 6.67 (b) | ↓ 6.18 (a)(a) | ↓ 6.90 (b)(b)(c) | |||||||
| Creatinine I | 1.28 | 0.000 | 1.26 | 0.000 | 1.24 | 0.001 | 1.28 | 0.001 | 1.30 | 0.002 | 1.53 | 0.042 | 1.20 | 0.012 |
| Creatinine II | 1.09 | 1.10 | 0.97 | 1.15 | 1.06 | 1.10 | 1.04 | |||||||
| Δ Creatinine | ↓ 0.20 | ↓ 0.16 | ↓ 0.26 | ↓ 0.12 (c) | ↓ 0.24 (c) | ↓ 0.42 (c)(c) | ↓ 0.15 (c)(c)(c) | |||||||
| Inflammatory status | ||||||||||||||
| Fibrinogen I | 636.96 | 0.000 | 624.78 | 0.000 | 570.89 | 0.000 | 645.43 | 0.000 | 651.35 | 0.000 | 549.29 | 0.000 | 697.00 | 0.000 |
| Fibrinogen II | 441.62 | 460.23 | 478.50 | 453.23 | 419.62 | 368.94 | 442.29 | |||||||
| Δ Fibrinogen | ↓ 195.34 | ↓ 164.55 | ↓ 92.39 | ↓ 192.19 (b) | ↓ 231.73 (b) | ↓ 180.35 (a)(c) | ↓ 254.7 (a)(b)(b) | |||||||
| CRP I | 3.74 | 0.000 | 3.64 | 0.000 | 3.37 | 0.000 | 3.75 | 0.000 | 3.84 | 0.011 | 3.57 | 0.000 | 3.96 | 0.151 |
| CRP II | 1.62 | 1.07 | 1.19 | 1.03 | 2.26 | 1.22 | 2.72 | |||||||
| Δ CRP | ↓ 2.12 | ↓ 2.57 | ↓ 2.18 | ↓ 2.72 (c) | ↓ 1.58 (c) | ↓ 2.35 (c)(c) | ↓ 1.24 (b)(b)(b) | |||||||
| Lipid profile | ||||||||||||||
| Total chol I | 181.54 | 0.000 | 185.89 | 0.000 | 178.44 | 0.001 | 188.74 | 0.000 | 176.40 | 0.445 | 186.59 | 0.003 | 171.84 | 0.896 |
| Total chol II | 168.10 | 165.34 | 152.06 | 170.43 | 171.36 | 167.65 | 173.03 | |||||||
| Δ Total chol | ↓ 13.42 | ↓ 20.55 | ↓ 26.39 | ↓ 18.32 (c) | ↓ 5.04 (b) | ↓ 18.94 (b)(c) | ↑ 1.18 (a)(a)(a) | |||||||
| LDL-chol I | 144.26 | 0.000 | 138.83 | 0.000 | 140.67 | 0.002 | 138.13 | 0.000 | 150.67 | 0.000 | 134.35 | 0.000 | 157.97 | 0.000 |
| LDL-chol II | 122.02 | 115.00 | 119.06 | 113.45 | 130.33 | 117.24 | 136.18 | |||||||
| Δ LDL-chol | ↓ 22.23 | ↓ 23.83 | ↓ 21.61 | ↓ 24.68 (c) | ↓ 20.35 (c) | ↓ 17.12 (b)(b) | ↓ 21.79 (c)(c)(b) | |||||||
| HDL-chol I | 40.19 | 0.000 | 42.26 | 0.000 | 37.78 | 0.000 | 43.98 | 0.000 | 37.75 | 0.000 | 35.71 | 0.008 | 38.66 | 0.000 |
| HDL-chol II | 50.33 | 53.22 | 51.66 | 53.83 | 46.91 | 45.46 | 47.55 | |||||||
| Δ HDL-chol | ↑ 10.14 | ↑ 10.96 | ↑ 13.88 | ↑ 9.85 (c) | ↑ 9.16 (c) | ↑ 9.75 (b)(c) | ↑ 8.90 (b)(c)(c) | |||||||
| TGs I | 147.95 | 0.000 | 154.29 | 0.006 | 138.56 | 0.563 | 160.32 | 0.006 | 140.45 | 0.023 | 134.24 | 0.077 | 143.24 | 0.109 |
| TGs II | 132.64 | 137.38 | 133.11 | 139.01 | 127.03 | 118.18 | 130.99 | |||||||
| Δ TGs | ↓ 15.32 | ↓ 16.92 | ↓ 5.44 | ↓ 21.31 (c) | ↓ 13.42 (c) | ↓ 16.06 (b)(b) | ↓ 12.42 (b)(b)(c) | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Namat, R.; Duceac, L.D.; Chelaru, L.; Dabija, M.G.; Guțu, C.; Marcu, C.; Popa, M.V.; Popa, F.; Bogdan Goroftei, E.R.; Țarcă, E. Post-Coronary Artery Bypass Grafting Outcomes of Patients with/without Type-2 Diabetes Mellitus and Chronic Kidney Disease Treated with SGLT2 Inhibitor Dapagliflozin: A Single-Center Experience Analysis. Diagnostics 2024, 14, 16. https://doi.org/10.3390/diagnostics14010016
Al Namat R, Duceac LD, Chelaru L, Dabija MG, Guțu C, Marcu C, Popa MV, Popa F, Bogdan Goroftei ER, Țarcă E. Post-Coronary Artery Bypass Grafting Outcomes of Patients with/without Type-2 Diabetes Mellitus and Chronic Kidney Disease Treated with SGLT2 Inhibitor Dapagliflozin: A Single-Center Experience Analysis. Diagnostics. 2024; 14(1):16. https://doi.org/10.3390/diagnostics14010016
Chicago/Turabian StyleAl Namat, Razan, Letiția Doina Duceac, Liliana Chelaru, Marius Gabriel Dabija, Cristian Guțu, Constantin Marcu, Maria Valentina Popa, Florina Popa, Elena Roxana Bogdan Goroftei, and Elena Țarcă. 2024. "Post-Coronary Artery Bypass Grafting Outcomes of Patients with/without Type-2 Diabetes Mellitus and Chronic Kidney Disease Treated with SGLT2 Inhibitor Dapagliflozin: A Single-Center Experience Analysis" Diagnostics 14, no. 1: 16. https://doi.org/10.3390/diagnostics14010016
APA StyleAl Namat, R., Duceac, L. D., Chelaru, L., Dabija, M. G., Guțu, C., Marcu, C., Popa, M. V., Popa, F., Bogdan Goroftei, E. R., & Țarcă, E. (2024). Post-Coronary Artery Bypass Grafting Outcomes of Patients with/without Type-2 Diabetes Mellitus and Chronic Kidney Disease Treated with SGLT2 Inhibitor Dapagliflozin: A Single-Center Experience Analysis. Diagnostics, 14(1), 16. https://doi.org/10.3390/diagnostics14010016






