Abstract
Shoulder pain is a common issue often linked to conditions such as subacromial impingement or rotator cuff lesions. The role of the acromion in these symptoms remains a subject of debate. This study aims to establish standardized values for commonly used acromion dimensions based on whole-body MRI scans of a large and healthy population and to investigate potential correlations between acromion shape and influencing factors such as sex, age, BMI, dominant hand, and shoulder pain. The study used whole-body MRI scans from the Study of Health in Pomerania, a German population-based study. Acromion index, acromion tilt, and acromion slope were measured. Interrater variability was tested with two independent, trained viewers on 100 MRI sequences before actual measurements started. Descriptive statistics and logistic regression were used to evaluate the results. We could define reference values based on a shoulder-healthy population for each acromion parameter within the 2.5 to 97.5 percentile. No significant differences were found in acromion slope, tilt, and index between male and female participants. No significant correlations were observed between acromion morphology and anthropometric parameters such as height, weight, or BMI. No significant differences were observed in acromion parameters between dominant and non-dominant hands or stated pain intensity. This study provides valuable reference values for acromion-related parameters, offering insight into the anatomy of a healthy shoulder. The findings indicate no significant differences in acromion morphology based on sex, weight, BMI, or dominant hand. Further research is necessary to ascertain the clinical implications of these reference values. The establishment of standardized reference values opens new possibilities for enhancing clinical decision making regarding surgical interventions, such as acromioplasty.
1. Introduction
Shoulder pain is a prevalent issue affecting many patients [1], often attributed to conditions such as subacromial impingement or rotator cuff lesions [2,3]. The role of the acromion in the development of these symptoms in atraumatic cases remains a subject of conflicting debate [4,5,6,7]. Moreover, the lack of a standardized method to describe acromion shape further complicates this discussion.
One of the earliest and most commonly used classifications was proposed by Bigliani et al. in 1986 [8]. They identified three types of acromial morphology in outlet-view radiographs: flat (type I), curved (type II), and hooked (type III) acromion. The hooked type was later associated with a higher likelihood of developing shoulder symptoms [9,10]. However, contrasting findings from other authors have questioned the correlation between the acromion type according to Bigliani and shoulder pathologies [9]. Some did not detect any correlation between the acromion type according to Bigliani and shoulder pathologies [11]. Moreover, the types appear to be independent of age or sex [9,12,13].
A major limitation of the Bigliani classification is its poor interrater reliability, leading to the development of alternative measurements to describe acromion morphology [14]. These include the acromial slope [8,15], acromial tilt [15], acromion index [16], and the lateral acromion angle [17].
Despite their improved reliability, these measurements lack well-defined reference values for each parameter, making it challenging to establish a standard acromion appearance. Reference values are essential for clinical assessment to determine if a patient’s symptoms may be attributed to acromion shape, influencing decisions regarding surgical interventions like acromioplasty [7,18,19].
While the mentioned acromion measurements are based on X-ray assessments, magnetic resonance imaging (MRI) is considered the gold standard in shoulder pain diagnostics [20]. Thus, the objective of this study is to establish standardized values for commonly used acromion dimensions based on whole-body MRI scans of a large and healthy population. Additionally, we aim to investigate potential correlations between acromion shape and influencing factors such as sex, age, BMI, dominant hand, and shoulder pain. By addressing these research objectives, we aim to contribute valuable insights to the understanding of acromion anatomy and its implications for shoulder pathologies.
2. Materials and Methods
2.1. SHIP Design
The study of Health in Pomerania is a German population-based study performed in the counties of Northern and Eastern Pomerania and the German cities Stralsund and Greifswald to describe the health status of the Pomeranian society [21,22]. There were two independent cohorts of Pomeranian citizens examined aged from 20 to 79 years. In 1997, 6265 citizens were randomly chosen from the official resident registry office and invited via three letters, phone calls, and one personal contact. Migrated and deceased persons were excluded. The first cohort comprised 4308 participants (response 68.8%) from 1997 to 2001 who underwent an interview as well as several non-invasive examinations. The standardized interview included pain-related questions, e.g., if the participants suffer from neck or shoulder pain.
Two follow-up examinations were executed from 2002–2006 (SHIP-1, n = 3300) and 2008–2012 (SHIP-2, n = 2333). In 2008, there was another independent cohort accomplished (SHIP-TREND, n = 4420, response 50%) with a wider spectrum of examinations [21,22]. Overall, 3371 of 6753 experimentees from SHIP-2 and SHIP-TREND went through a whole-body MRI examination (Magnetom Avanto, 1.5 Tesla, Siemens Healthcare, Erlangen, Germany), which were used for the current study. The whole-body MRI was performed as a TIRM fat-suppressed imaging with a voxel size of 2.1 × 1.6 × 5 mm. The patients were lying in the MRI in a supine position; head first, on the table, the arms were positioned laterally lying at their sides. Reasons for dropout were, for example, claustrophobia, metal implants, or personal reasons. MRI scans were evaluated by two independent radiologists with the help of a standardized examination sheet. SHIP was the first population-based study using whole-body MRI examinations. The complete MR procedure and imaging protocol including further technical data have already been published [23].
2.2. Image Analysis and Measurement
In total, there were 3371 whole-body MRI sequences to be measured. Horos (Horos Project Community, GNU Lesser General Public License, v. 3.3.5) was used as an image viewer in addition to a plug-in which was prepared especially for these measurements. It converted single points in the MRI sequences into three-dimensional distances and angles. In detail, these are the three parameters: acromion index, acromion tilt, and acromion slope. A single observer analyzed the MRI sequences blinded to any subjects’ health data.
2.3. Acromion Index (Figure 1)
The index is the relation of the distances between the articular surface of the glenoid to the lateral edge of the humeral head, on the one hand, and the lateral edge of the acromion on the other hand. Measuring took place by an adjusted form of the method by Nyffeler et. al. [16], but in a horizontal plane.
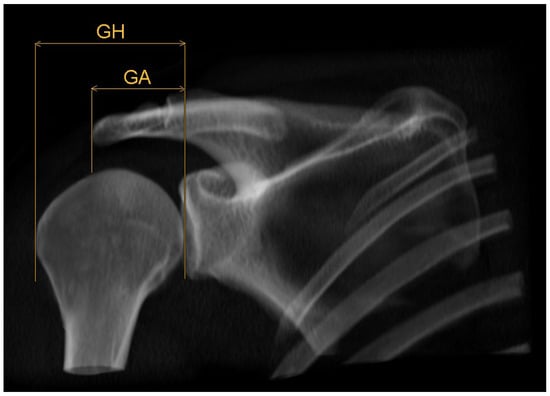
Figure 1.
Schematic 3D reconstruction of the glenohumeral joint in anterior–posterior view, illustrating the measurement technique for the acromion index AI = GA/GH. GA indicates the distance between glenoid surface and lateral edge of the acromion, GH the distance between glenoid surface and lateral edge of the humeral head.
First, pinpoints are set to mark the lower (G1, Figure 2) and the upper (G2, Figure 3) end of the glenoid, each in the middle of it. A line connecting these two points, created by the plug-in, representing the axis of the glenoid. Another point H (Figure 4) marks the lateral edge of the humeral head.
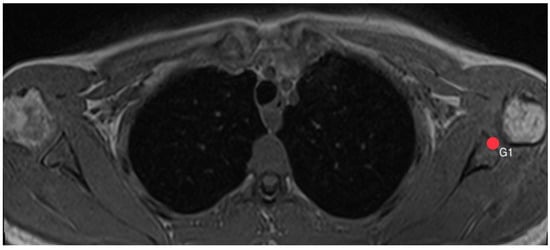
Figure 2.
How to measure acromion index: Axial MRI of the thorax depicting the shoulder joint in T1 weighting (3D-GRE VIBE sequence), with a slice thickness of 3 mm. Point G1 indicates the lower end of the glenoid.
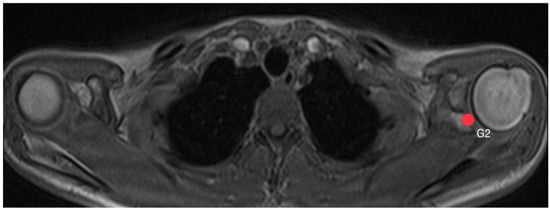
Figure 3.
How to measure acromion index: Axial MRI of the thorax depicting the shoulder joint in T1 weighting (3D-GRE VIBE sequence), with a slice thickness of 3 mm. Point G2 indicates the upper end of the glenoid.
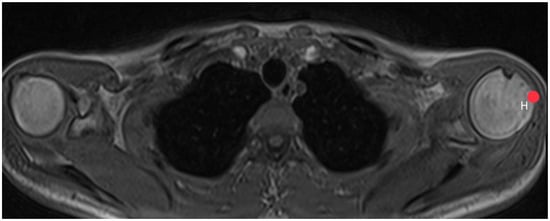
Figure 4.
How to measure acromion index: Axial MRI of the thorax depicting the shoulder joint in T1 weighting (3D-GRE VIBE sequence), with a slice thickness of 3 mm. Point H indicates the lateral edge of the humeral head.
The plug-in calculates the distance GH between the glenoid surface at the same height as point H is marked. Afterwards, another point A (Figure 5) shows the lateral edge of the acromion, from which distance GA is calculated by the plug-in in the same way. The acromion index is the relation between both distances, so AI = GA/GH.
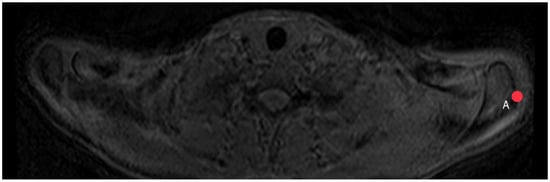
Figure 5.
How to measure acromion index: Axial MRI of the thorax depicting the shoulder joint in T1 weighting (3D-GRE VIBE sequence), with a slice thickness of 3 mm. Point A indicates the lateral edge of the acromion.
2.4. Acromion Tilt (Figure 6)
The acromion tilt shows the tilt angle of the acromion in relation to the coracoid process in the sagittal plane. Measuring was based on the method by Kitay et. al. [15], but in the horizontal plane. Two points mark the ventral (A1, Figure 7) and the dorsal (A2, Figure 8) end of the acromion’s bottom. A line connecting these points builds line A.
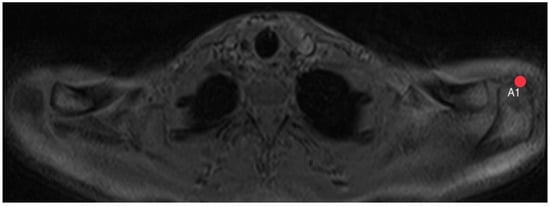
Figure 7.
How to measure acromion tilt: Axial MRI of the thorax depicting the shoulder joint in T1 weighting (3D-GRE VIBE sequence), with a slice thickness of 3 mm. Point A1 indicates the ventral end of the acromion’s bottom.
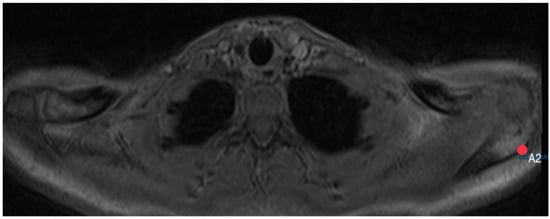
Figure 8.
How to measure acromion tilt: Axial MRI of the thorax depicting the shoulder joint in T1 weighting (3D-GRE VIBE sequence), with a slice thickness of 3 mm. Point A2 indicates the dorsal end of the acromion’s bottom.
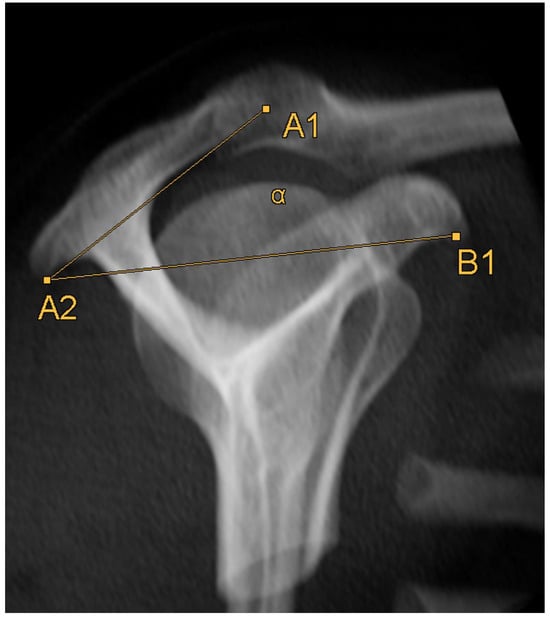
Figure 6.
Schematic 3D reconstruction of the glenohumeral joint in anterior–posterior view, illustrating the measurement technique for the acromion tilt (α). A1 indicates the ventral end of the acromion’s bottom, A2 the dorsal end of the acromion’s bottom, B1 the lower end of the coracoid process.
Afterwards, a point B1 (Figure 9) is set on the lower end of the coracoid process. A line connecting point B1 with point A2 builds line B. The plug-in calculates the angle between lines A and B, which shows the acromial tilt.
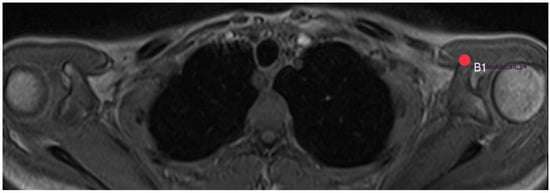
Figure 9.
How to measure acromion tilt: Axial MRI of the thorax depicting the shoulder joint in T1 weighting (3D-GRE VIBE sequence), with a slice thickness of 3 mm. Point B1 indicates the lower end of the coracoid process.
2.5. Acromion Slope (Figure 10)
The acromion slope measures the curvature of the acromion in the sagittal plane. Measuring was based on the method by Bigliani et al. [8] and Kitay et al. [15], but once more in the horizontal plane. One line connects the ventral end of the acromion (A1, Figure 7) with the middle of the acromion’s bottom (M, Figure 11). Another line connects the dorsal end (A2, Figure 8) with the middle of the acromion’s bottom (M). The plug-in takes points A1 and A2 from the acromion tilt and calculates the angle between those two lines.
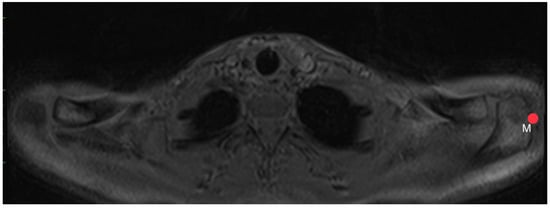
Figure 11.
How to measure acromion slope: Axial MRI of the thorax depicting the shoulder joint in T1 weighting (3D-GRE VIBE sequence), with a slice thickness of 3 mm. Point M indicates the middle of the acromion’s bottom.
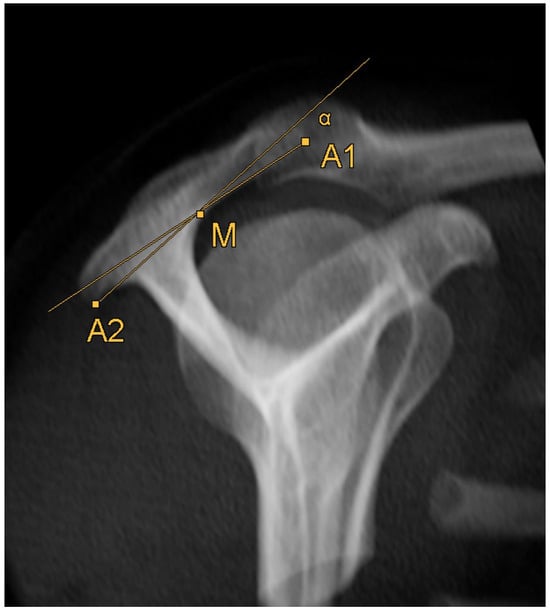
Figure 10.
Schematic 3D reconstruction of the glenohumeral joint in anterior–posterior view, illustrating the measurement technique for the acromion slope (α). A1 indicates the ventral end of the acromion’s bottom, A2 the dorsal end of the acromion’s bottom, M the middle of the acromion’s bottom.
2.6. Statistical Analysis
Interrater variability was tested on 100 MRI sequences before actual measurements started. Two independent, trained viewers used the plug-in to validate the method. Bland and Altman plots as well as intraclass correlation coefficients were used to evaluate intra- and interreader variabilities (Table 1 and Figure 12).

Table 1.
Interrater variability values. Number of measurements (n), intraclass correlation coefficients (ICC), mean bias (absolute, in % to 360° and their standard deviations (SDs)).
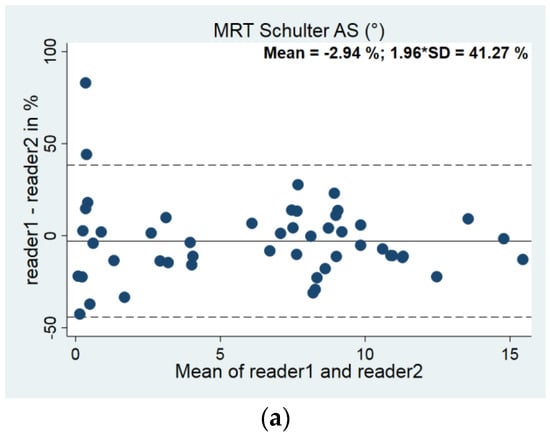
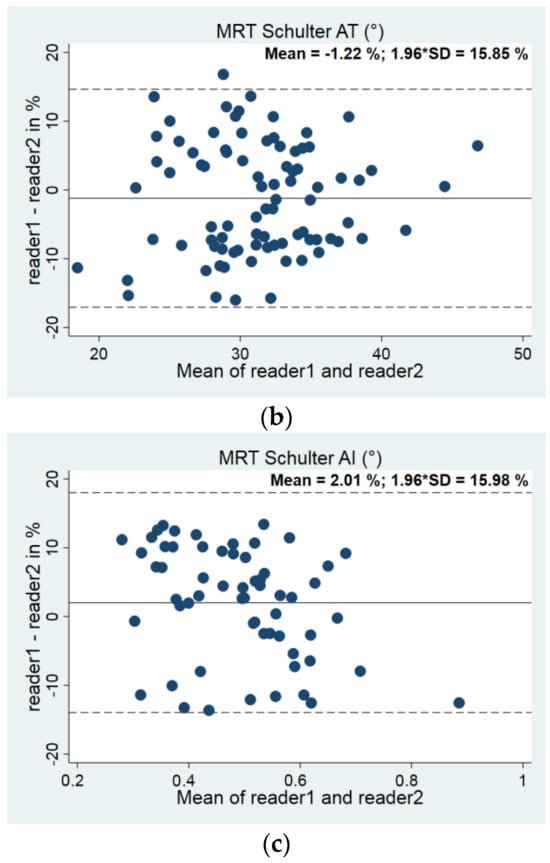
Figure 12.
(a–c). Bland–Altman plots for interrater variability: (a) Acromion slope (AS, n = 60), (b) Acromion tilt (AT, n = 85), (c) Acromion index (n = 60).
Descriptive statistics like mean values, standard deviations (SDs), ranges, and percentiles were used to evaluate the results. Logistic regression adjusted for age and sex was used to investigate the correlation between acromion parameters and the prevalence of pathological changes like edema, peripheral attachments, and pain. Pearson’s correlation coefficient was used to determine the correlation between the right and left side as well as possible interactions between the parameters.
Stratified by sex, upper and lower reference limits were calculated by quantile regressions for the 2.5th and the 97.5th percentile in the same way the influence of age, weight, and height was studied. We excluded patients who showed an edema, joint effusion, or bony peripheral attachments and those who declared a pain intensity bigger than 3 on a scale from 0 to 10 or a fracture in the close anatomical region of the shoulder (15.18%) for the group of reference values.
A p-value less than 0.05 was considered statistically significant. We assumed small impact for a Pearson’s correlation coefficient ≥ 0,1, moderate impact for beta ≥ 0.3, and big impact for beta ≥ 0.5 [24]. Statistical analysis was performed using common statistical software: Stata 17.0 (Stata Corporation, College Station, TX, USA).
3. Results
From the initial 3371 whole-body MRI sequences, only 1034 sequences showed clear visualization of the acromioclavicular joint (Figure 13). Thirty-eight sequences were excluded due to blurring. In the MRI scans of the remaining 996 participants, we were able to analyze the acromion 915 times on the right side and 642 times on the left side.
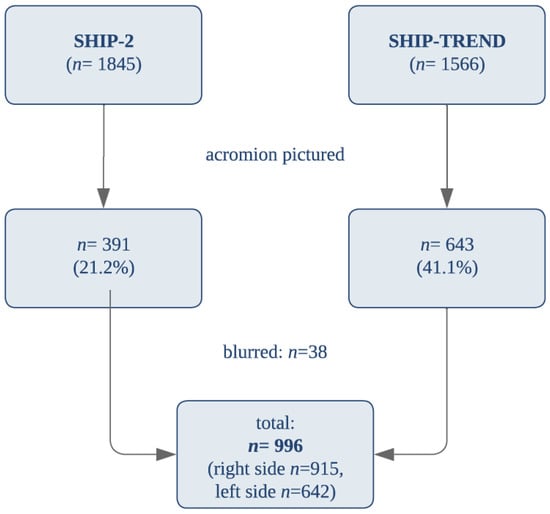
Figure 13.
Amount and Composition of Measured MRIs.
3.1. Correlation Analysis
3.1.1. Comparison between Left and Right Side
A significant correlation coefficient of 0.53 was found between the acromion tilt measurements on the left and right sides, indicating at least a moderate association. The acromion index exhibited a lesser moderate correlation (coefficient of 0.34), while the acromion slope showed no significant correlation (coefficient of 0.19) between both sides (Table 2).

Table 2.
Correlation between right and left side. Median, 25th and 75th percentile, and Pearson´s correlation coefficient for each parameter.
3.1.2. Comparison between Genders
No significant differences were found in acromion slope, tilt, and index between male and female participants (Table 3).

Table 3.
Differences between genders. Median, 25th and 75th percentile, and p-values for the difference between both genders. A p-value lower than 0.05 was considered statistically significant (r = right side, l = left side).
3.1.3. Correlation with Anthropometric Parameters
No significant correlations were observed between acromion morphology and anthropometric parameters such as height, weight, or BMI (Table 4).

Table 4.
Correlation between anthropometric parameters and each acromion parameter. A p-value lower than 0.05 was considered statistically significant (r = right side, l = left side).
3.1.4. Hand Dominance and Pain Intensity
Concerning the dominance of one hand, 90.53% of participants were right-handed, 4.62% left-handed, and 4.85% ambidextrous. No significant differences were observed in acromion parameters between dominant and non-dominant hands (Table 5).

Table 5.
Differences between right- and left-handed participants. Coefficients for each parameter considering the declared dominant hand of the participants. A p-value lower than 0.05 was considered statistically significant (r = right side, l = left side).
No significant differences were observed in acromion parameters between participants with pain intensity greater than 3 on a scale from 0 to 10 (15.18% of all participants) and those with an intensity of 3 or lower (Table 6).

Table 6.
Differences between participants with pain intensity <3 and >3. Coefficients for each parameter considering the declared pain on a visual analog scale from 1 to 10. A p-value lower than 0.05 was considered statistically significant (r = right side, l = left side).
3.1.5. Reference Values
We defined our exclusion criteria to estimate the standard values for a healthy population. Reference values for an average acromion in a healthy shoulder were calculated within the 2.5th to 97.5th percentile for all participants, as there were no significant differences between men and women (Table 7).

Table 7.
Reference values for each anatomical parameter [with corresponding 95% confidence interval] respecting our excluding criteria (see above) (r = right side, l = left side).
4. Discussion
In this study, we have presented reference values for acromion-related parameters, which, to the best of our knowledge, are reported for the first time. Despite MRI not being the gold standard for examining bony structures, our results show good comparability with previous studies using CT or X-ray imaging, particularly regarding acromion tilt [19,25]. For instance, Balke et al. using a.p. and outlet-view X-ray reported acromion slope values of 21–25°, acromion tilt values of 29–34°, and an acromion index range of 0.67–0.75 [10]. Nyffeler et al. described an acromion index of 0.64 in a.p. X-rays [16], while Chaimongkhol et al. discovered an acromion tilt of 28° through manual measurements [13].
MRI proves to be a valid alternative diagnostic tool for assessing acromial issues, as demonstrated by Chalmers et al. without any radiation exposure [19]. Additionally, our measurements seem transferable to other diagnostic imaging methods. However, radiography is often more readily available and faster, making it a reasonable addition in the diagnostics of acromial pathologies, such as subacromial impingement syndrome. Differences in acromion slope and index parameters between MRI and X-ray diagnostics might be attributed to varying interobserver reliability in interpreting the imaging and differences in the imaging planes used as well as the different positioning of the scapula during radiography since MRI was conducted in a supine position, in contrast to X-ray imaging in an erect position. The advantage of MRI lies in its more consistent image quality due to the possibility of reconstruction techniques, potentially resulting in higher accuracy of reference values compared to X-ray diagnostics.
An interesting finding is the lack of correlation of the acromion parameters with one another, suggesting that it is not feasible to classify acromion shapes into distinct “types” based on acromion tilt, slope, and index. We could not reproduce the historical classification according to Bigliani et al. using a shoulder outlet-view radiograph, which may have yielded different findings [8]. It has been previously reported that the Bigliani classification has poor interobserver reliability, leading to its decreasing significance [14]. While our study did not directly investigate pathological conditions, and thus did not utilize the Bigliani classification for data analysis, we recognize that the morphological characteristics we measured may have implications for understanding shoulder pathologies. Although there are limitations of the Bigliani classification, notably its poor interrater reliability, we suggest that future research could explore the relationship between our measurements and the Bigliani types to potentially elucidate any associations with clinical outcomes. However, due to the non-pathological nature of our study design, a direct comparison or application of the Bigliani classification within our current work remains beyond its scope. While our focus was on providing reference values for acromion-related parameters, we recognize the historical significance of the Bigliani classification and its association with shoulder pathologies.
Our reference values are completely independent of individual characteristics such as sex, age, anthropometric data, or dominant hand, making their clinical use straightforward. This raises the hypothesis that behavioral therapy strategies may have limited success in acromial pathologies. There is a certain correlation between the anatomy of the left and right side, at least in terms of the acromion tilt. This could be justified by the assumption that human anatomy is roughly symmetrical. As a potential hypothesis, deviations could be due, for example, to varying degrees of strain during the growth phase. Interestingly, despite focusing on sex differences in subacromial impingement, our findings demonstrate no difference in acromion anatomy, matching the results of Nyffeler et al. or Colegate-Stone et al. [9,16]. In contrast, multiple investigations found a difference between genders in glenoid anatomy [26,27]. We also could not reproduce the findings from Chaimongkhol et al. showing a higher frequency of hooked type acromion in males [13]. Then again, the anatomy of the humeral head seems to show no difference between men and women [28]. This raises the question of why men suffer from this pathology more often than women [29,30], which could be a subject of further investigation, possibly indicating a gender bias or differences in diagnosis. It is crucial to note the regional limitation of our data, which primarily encompasses a German population. Generalizing our findings to diverse populations, including those in Asia or America, should be approached with caution and may require further studies in these regions.
To predict the precise clinical benefit of our reference values, further studies are necessary. The primary aim of this study was to create reference values to aid in deciding whether a patient could benefit from surgical interventions like acromioplasty. We did not find any correlation between pain intensity and single anatomical parameters, which is not surprising given the healthy characteristics of our cohort. Performing similar examinations in a cohort of symptomatic patients and comparing them to our reference values could provide valuable insights. Nonetheless, although subacromial impingement is the most common cause of shoulder pain [31], further potential causes should not be ignored [32,33] but have been minimized by mainly excluding arthritic changes through our methodology. Nevertheless, Chalmers et al. did not find any correlation between acromion morphology in MRI and the likelihood of developing rotator cuff tears, discouraging surgery like lateral acromioplasty [19].
Despite the robustness of our study, certain methodological considerations should be acknowledged. The whole-body MRI captured the acromion in only a few cases, which may be attributed to the risk of a systematic error in excluding participants with a large height or issues with standardization during MRI. That could be reinforced by the fact that the position of the patient in the MRI is different than in X-ray. This is therefore a difference from X-rays of the shoulder joint, which may result in a different scapula alignment and consequently deviations. Although the MRI images have been controlled to ensure correct scapular orientation and minimize potential impacts on measurements, a different scapula orientation could have led to variations. Moreover, the larger layer thickness (5 mm) of the whole-body MRI compared to the standard shoulder MRI thickness (lower than 3 mm) and the poor resolution of the shoulder area are methodological challenges. Additionally, measuring small angles in transversal planes proved difficult with our plug-in, potentially leading to inaccuracies which are shown best in the larger deviation of the interrater variability of acromion slope measurements. Future studies should consider using coronary or sagittal planes for more precise and practical measurements. Nevertheless, the high-quality data from our large collective allowed us to describe the anatomy of the acromion in detail, a feat not previously achieved to this extent, and methodical issues have been approached by interobserver and intraobserver reliability analysis.
This study provides valuable reference values for acromion-related parameters, offering insight into the anatomy of a healthy shoulder. Further investigations are necessary to explore the clinical implications of these reference values and their applicability in patients with acromial pathologies. The findings also raise questions about potential gender biases and the utility of behavioral therapy strategies in managing acromial conditions. Our work contributes to the growing body of knowledge on shoulder anatomy and provides a foundation for future research in this field.
5. Conclusions
In conclusion, our comprehensive anatomical analysis of the acromion has yielded valuable reference values for commonly used parameters such as acromion slope, tilt, and the acromion index. These reference values are based on a large and healthy population, providing a solid foundation for clinical use and research in the field of acromial pathologies.
Notably, our findings indicate no significant differences in acromion morphology based on sex, weight, BMI, or dominant hand. This suggests that the reference values are applicable across diverse patient populations, independent of individual characteristics.
While our study sheds light on the normal anatomy of the acromion, further research is necessary to ascertain the clinical implications of these reference values. Prospective investigations are warranted to explore potential associations between acromion morphology and the development of rotator cuff injuries. Additionally, studies comparing symptomatic patients to our reference values could provide valuable insights into the diagnostic and therapeutic utility of these measurements.
The establishment of standardized reference values opens new possibilities for enhancing clinical decision making regarding surgical interventions, such as acromioplasty. By comparing individual patient measurements to these reference values, healthcare providers can make more informed treatment decisions tailored to each patient’s unique anatomy. While MRI proved to be a valid alternative diagnostic tool for assessing acromial issues without any radiation exposure, CT remains the gold standard for examining bony structures and might be used additionally [19].
In summary, our study contributes to the growing body of knowledge on acromial anatomy and provides an essential resource for clinicians and researchers alike. As our understanding of acromial pathologies continues to evolve, these reference values will prove indispensable in advancing patient care and optimizing treatment strategies.
Author Contributions
Conceptualization, R.B.; Data curation, T.I.; Formal analysis, T.I.; Investigation, A.P. and T.L.; Methodology, A.P., T.L. and R.L.; Project administration, A.E. and M.S.B.; Resources, R.B.; Software, R.L.; Supervision, L.H., G.I.W., A.E. and M.S.B.; Writing—original draft, A.P.; Writing—review and editing, M.S.B. All authors have read and agreed to the published version of the manuscript.
Funding
The SHIP study is part of the Community Medicine Research Net of the University of Greifswald, Germany, which was funded by the Federal Ministry of Education and Research (grant no. 03ZIK012), the Ministry of Cultural Affairs, as well as the Social Ministry of the Federal State of Mecklenburg-West Pomerania. MR imaging was supported by the Federal State of Mecklenburg-Vorpommern, the Federal Ministry of Education and Research, and a joint grant from Siemens Healthcare, Erlangen, Germany. No further funding was disclosed by the authors.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the University Medicine Greifswald ethics committee (BB 39/08, 19 June 2008).
Informed Consent Statement
Written informed consent, including consent for publication, was obtained from the patients.
Data Availability Statement
The data presented in this study are available within the manuscript.
Acknowledgments
We thank the participants for providing their data.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Urwin, M.; Symmons, D.; Allison, T.; Bramah, T. Estimating the Burden of Musculoskeletal Disorders in the Community: The Comparative Prevalence of Symptoms at Different Anatomical Sites, and the Relation to Social Deprivation. Ann. Rheum. Dis. 1998, 57, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Garving, C.; Jakob, S.; Bauer, I.; Nadjar, R.; Brunner, U.H. Impingement Syndrome of the Shoulder. Dtsch. Arztebl. Int. 2017, 114, 765–776. [Google Scholar] [CrossRef] [PubMed]
- Ostör, A.J.K.; Richards, C.A.; Prevost, A.T.; Speed, C.A.; Hazleman, B.L. Diagnosis and Relation to General Health of Shoulder Disorders Presenting to Primary Care. Rheumatology 2005, 44, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Bigliani, L.U.; Levine, W.N. Subacromial Impingement Syndrome. J. Bone Jt. Surg. Am. 1997, 79, 1854–1868. [Google Scholar] [CrossRef]
- Tangtrakulwanich, B.; Kapkird, A. Analyses of Possible Risk Factors for Subacromial Impingement Syndrome. World J. Orthop. 2012, 3, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Moor, B.K.; Bouaicha, S.; Rothenfluh, D.A.; Sukthankar, A.; Gerber, C. Is There an Association between the Individual Anatomy of the Scapula and the Development of Rotator Cuff Tears or Osteoarthritis of the Glenohumeral Joint?: A Radiological Study of the Critical Shoulder Angle. Bone Jt. J. 2013, 95–B, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Katthagen, J.C.; Marchetti, D.C.; Tahal, D.S.; Turnbull, T.L.; Millett, P.J. The Effects of Arthroscopic Lateral Acromioplasty on the Critical Shoulder Angle and the Anterolateral Deltoid Origin: An Anatomic Cadaveric Study. Arthroscopy 2016, 32, 569–575. [Google Scholar] [CrossRef]
- Bigliani, L.U.; Morrison, D.S.; April, E.W. The Morphology of the Acromion and Its Relationship to Rotator Cuff Tears. Orthop. Trans. 1986, 10, 228. [Google Scholar]
- Colegate-Stone, T.J.; Tavakkolizadeh, A.; Sinha, J. An Analysis of Acromioclavicular Joint Morphology as a Factor for Shoulder Impingement Syndrome. Shoulder Elb. 2014, 6, 165–170. [Google Scholar] [CrossRef]
- Balke, M.; Schmidt, C.; Dedy, N.; Banerjee, M.; Boillon, B.; Liem, D. Correlation of Acromial Morphology with Impingement Syndrome and Rotator Cuff Tears. Acta Orthop. 2013, 84, 178–183. [Google Scholar] [CrossRef]
- Ludewig, P.M.; Reynolds, J.F. The Association of Scapular Kinematics and Glenohumeral Joint Pathologies. J. Orthop. Sports Phys. Ther. 2009, 39, 90–104. [Google Scholar] [CrossRef] [PubMed]
- Colegate-Stone, T.; Allom, R.; Singh, R.; Elias, D.A.; Standring, S.; Sinha, J. Classification of the Morphology of the Acromioclavicular Joint Using Cadaveric and Radiological Analysis. J. Bone Jt. Surg. Br. 2010, 92, 743–746. [Google Scholar] [CrossRef] [PubMed]
- Chaimongkhol, T.; Benjachaya, S.; Mahakkanukrauh, P. Acromial Morphology and Morphometry Associated with Subacromial Impingement Syndrome. Anat. Cell Biol. 2020, 53, 435–443. [Google Scholar] [CrossRef] [PubMed]
- McLean, A.; Taylor, F. Classifications in Brief: Bigliani Classification of Acromial Morphology. Clin. Orthop. Relat. Res. 2019, 477, 1958–1961. [Google Scholar] [CrossRef] [PubMed]
- Kitay, G.S.; Iannotti, J.P.; Williams, G.R.; Haygood, T.; Kneeland, B.J.; Berlin, J. Roentgenographic Assessment of Acromial Morphologic Condition in Rotator Cuff Impingement Syndrome. J. Shoulder Elb. Surg. 1995, 4, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Nyffeler, R.W.; Werner, C.M.; Sukthankar, A.; Schmid, M.R.; Gerber, C. Association of a Large Lateral Extension of the Acromion with Rotator Cuff Tears. J. Bone Jt. Surg. 2006, 88, 800–805. [Google Scholar] [CrossRef]
- Banas, M.P.; Miller, R.J.; Totterman, S. Relationship between the Lateral Acromion Angle and Rotator Cuff Disease. J. Shoulder Elb. Surg. 1995, 4, 454–461. [Google Scholar] [CrossRef]
- Ellman, H. Arthroscopic Subacromial Decompression: Analysis of One- to Three-Year Results. Arthroscopy 1987, 3, 173–181. [Google Scholar] [CrossRef]
- Chalmers, P.N.; Beck, L.; Miller, M.; Kawakami, J.; Dukas, A.G.; Burks, R.T.; Greis, P.E.; Tashjian, R.Z. Acromial Morphology Is Not Associated with Rotator Cuff Tearing or Repair Healing. J. Shoulder Elb. Surg. 2020, 29, 2229–2239. [Google Scholar] [CrossRef]
- Galvin, J.W.; Parada, S.A.; Li, X.; Eichinger, J.K. Critical Findings on Magnetic Resonance Arthrograms in Posterior Shoulder Instability Compared With an Age-Matched Controlled Cohort. Am. J. Sports Med. 2016, 44, 3222–3229. [Google Scholar] [CrossRef]
- Völzke, H.; Schössow, J.; Schmidt, C.O.; Jürgens, C.; Richter, A.; Werner, A.; Werner, N.; Radke, D.; Teumer, A.; Ittermann, T.; et al. Cohort Profile Update: The Study of Health in Pomerania (SHIP). Int. J. Epidemiol. 2011, 51, e372–e383. [Google Scholar] [CrossRef] [PubMed]
- Kasch, R.; Scheele, J.; Hancock, M.; Hofer, A.; Maher, C.; Bülow, R. Prevalence of Benign Osseous Lesions of the Spine and Association with Spinal Pain in the General Population in Whole Body MRI. PLoS ONE 2018, 13, e0193343. [Google Scholar] [CrossRef] [PubMed]
- Hegenscheid, K.; Kühn, J.P.; Völzke, H.; Biffar, R.; Hosten, N.; Puls, R. Whole-Body Magnetic Resonance Imaging of Healthy Volunteers: Pilot Study Results from the Population-Based SHIP Study. Rofo 2009, 181, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Akoglu, H. User’s Guide to Correlation Coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Parada, S.A.; Shaw, K.A.; Antosh, I.J.; Eichinger, J.K.; Li, X.; Curry, E.J.; Provencher, M.T. Magnetic Resonance Imaging Correlates With Computed Tomography for Glenoid Version Calculation Despite Lack of Visibility of Medial Scapula. Arthroscopy 2020, 36, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Matsen, F.A.; Whitson, A.; Hsu, J.E.; Stankovic, N.K.; Neradilek, M.B.; Somerson, J.S. Prearthroplasty Glenohumeral Pathoanatomy and Its Relationship to Patient’s Sex, Age, Diagnosis, and Self-Assessed Shoulder Comfort and Function. J. Shoulder Elb. Surg. 2019, 28, 2290–2300. [Google Scholar] [CrossRef] [PubMed]
- Matsuki, K.; Sugaya, H.; Hoshika, S.; Ueda, Y.; Takahashi, N.; Tokai, M.; Banks, S.A. Three-Dimensional Measurement of Glenoid Dimensions and Orientations. J. Orthop. Sci. 2019, 24, 624–630. [Google Scholar] [CrossRef]
- Tackett, J.J.; Ablove, R.H. Magnetic Resonance Imaging Study of Glenohumeral Relationships between Genders. J. Shoulder Elb. Surg. 2011, 20, 1335–1339. [Google Scholar] [CrossRef]
- Hill, L.; Collins, M.; Posthumus, M. Risk Factors for Shoulder Pain and Injury in Swimmers: A Critical Systematic Review. Phys. Sports Med. 2015, 43, 412–420. [Google Scholar] [CrossRef]
- Hoppe, M.W.; Brochhagen, J.; Tischer, T.; Beitzel, K.; Seil, R.; Grim, C. Risk Factors and Prevention Strategies for Shoulder Injuries in Overhead Sports: An Updated Systematic Review. J. Exp. Orthop. 2022, 9, 78. [Google Scholar] [CrossRef]
- Greenberg, D.L. Evaluation and Treatment of Shoulder Pain. Med. Clin. N. Am. 2014, 98, 487–504. [Google Scholar] [CrossRef] [PubMed]
- Linaker, C.H.; Walker-Bone, K. Shoulder Disorders and Occupation. Best Pract. Res. Clin. Rheumatol. 2015, 29, 405–423. [Google Scholar] [CrossRef] [PubMed]
- Lollino, N.; Brunocilla, P.R.; Poglio, F.; Vannini, E.; Lollino, S.; Lancia, M. Non-Orthopaedic Causes of Shoulder Pain: What the Shoulder Expert Must Remember. Musculoskelet. Surg. 2012, 96, 63–68. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).