Evaluation of Dental Root Development Regarding Maxillary Canine Eruption Status after Secondary Alveolar Bone Grafting in Patients with Cleft Lip and Palate
Abstract
1. Introduction
2. Materials and Methods
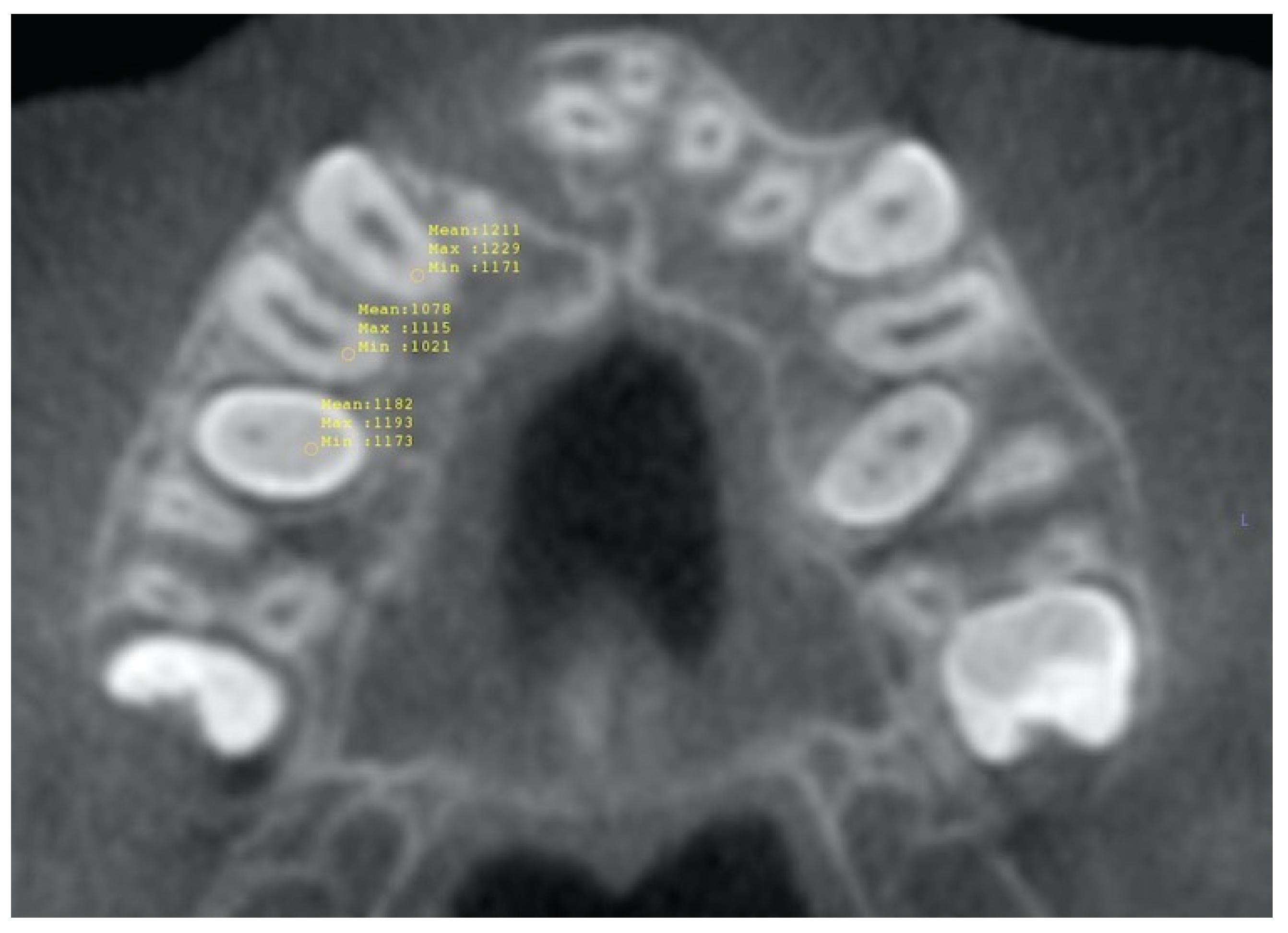
2.1. Volumetric Analysis
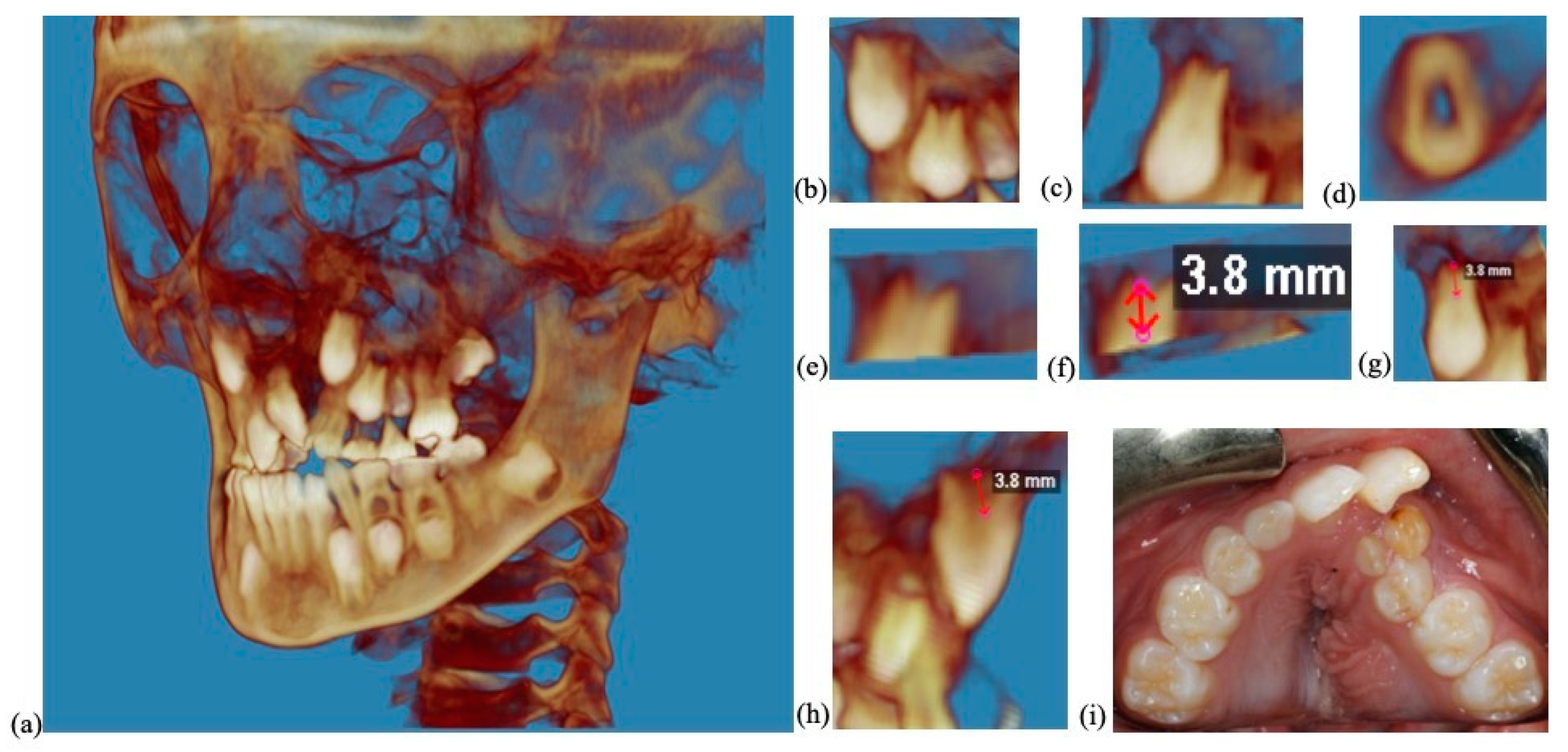
2.2. Root Length Analysis
2.3. Statistical Analysis
2.4. Sample Size
3. Results
3.1. Volumetric Analysis
3.2. Root Length Analysis
3.2.1. Independent t Tests for Root Length
3.2.2. Paired t Tests for Reciprocal of Mean Root Length Ratios
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Oberoi, S.; Gill, P.; Chigurupati, R.; Hoffman, W.Y.; Hatcher, D.C.; Vargervik, K. Three-dimensional assessment of the eruption path of the canine in individuals with bone-grafted alveolar clefts using cone beam computed tomography. Cleft Palate Craniofac. J. 2010, 47, 507–512. [Google Scholar] [CrossRef]
- Salari, N.; Darvishi, N.; Heydari, M.; Bokaee, S.; Darvishi, F.; Mohammadi, M. Global prevalence of cleft palate, cleft lip and cleft palate and lip: A comprehensive systematic review and meta-analysis. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 110–120. [Google Scholar] [CrossRef]
- Paradowska-Stolarz, A.; Mikulewicz, M.; Dus-Ilnicka, I. Current Concepts and Challenges in the Treatment of Cleft Lip and Palate Patients-A Comprehensive Review. J. Pers. Med. 2022, 12, 2089. [Google Scholar] [CrossRef] [PubMed]
- Fahradyan, A.; Tsuha, M.; Wolfswinkel, E.M.; Mitchell, K.-A.; Hammoudeh, J.A.; Magee, W. Optimal Timing of Secondary Alveolar Bone Grafting: A Literature Review. J. Oral Maxillofac. Surg. 2019, 77, 843–849. [Google Scholar] [CrossRef]
- Weissler, E.H.; Paine, K.M.; Ahmed, M.K.; Taub, P.J. Alveolar Bone Grafting and Cleft Lip and Palate: A Review. Plast. Reconstr. Surg. 2016, 138, 1287–1295. [Google Scholar] [CrossRef] [PubMed]
- Elhaddaoui, R.; Bahije, L.; Zaoui, F.; Rerhrhaye, W. Timing of alveolar bone graft and sequences of canine eruption in cases of cleft lip and palate: A systematic review. Orthod Fr. 2017, 88, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Kaura, A.S.; Srinivasa, D.R.; Kasten, S.J. Optimal Timing of Alveolar Cleft Bone Grafting for Maxillary Clefts in the Cleft Palate Population. J. Craniofac. Surg. 2018, 29, 1551–1557. [Google Scholar] [CrossRef] [PubMed]
- Boyne, P.J.; Sands, N.R. Secondary bone grafting of residual alveolar and palatal clefts. J. Oral Surg. 1972, 30, 87–92. [Google Scholar]
- Baldini, N.; De Sanctis, M.; Ferrari, M. Deproteinized bovine bone in periodontal and implant surgery. Dent. Mater. 2011, 27, 61–70. [Google Scholar] [CrossRef]
- Petretta, M.; Gambardella, A.; Boi, M.; Berni, M.; Cavallo, C.; Marchiori, G.; Maltarello, M.C.; Bellucci, D.; Fini, M.; Baldini, N.; et al. Composite Scaffolds for Bone Tissue Regeneration Based on PCL and Mg-Containing Bioactive Glasses. Biology 2021, 10, 398. [Google Scholar] [CrossRef]
- Chisci, G.; Hatia, A.; Chisci, E.; Chisci, D.; Gennaro, P.; Gabriele, G. Socket Preservation after Tooth Extraction: Particulate Autologous Bone vs. Deproteinized Bovine Bone. Bioengineering 2023, 10, 421. [Google Scholar] [CrossRef]
- Carbullido, M.K.; Dean, R.A.; Kamel, G.N.; Davis, G.L.; Hornacek, M.; Segal, R.M.; Ewing, E.; Lance, S.H.; Gosman, A.A. Long-Term Treatment Outcomes of Primary Alveolar Bone Grafts for Alveolar Clefts: A Qualitative Systematic Review. Cleft Palate Craniofac. J. 2022, 59, 86–97. [Google Scholar] [CrossRef]
- Seifeldin, S.A. Is alveolar cleft reconstruction still controversial? (Review of literature). Saudi Dent. J. 2016, 28, 3–11. [Google Scholar] [CrossRef]
- Helms, J.A.; Speidel, T.M.; Denis, K.L. Effect of timing on long-term clinical success of alveolar cleft bone grafts. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Turvey, T.A.; Vig, K.; Moriarty, J.; Hoke, J. Delayed bone grafting in the cleft maxilla and palate: A retrospective multidisciplinary analysis. Am. J. Orthod. 1984, 86, 244–256. [Google Scholar] [CrossRef] [PubMed]
- Boyne, P.J.; Sands, N.R. Combined orthodontic-surgical management of residual palato-alveolar cleft defects. Am. J. Orthod. 1976, 70, 20–37. [Google Scholar] [CrossRef]
- Vig, K.W. Alveolar bone grafts: The surgical/orthodontic management of the cleft maxilla. Ann. Acad. Med. Singap. 1999, 28, 721–727. [Google Scholar] [PubMed]
- Bergland, O.; Semb, G.; Abyholm, F.E. Elimination of the residual alveolar cleft by secondary bone grafting and subsequent orthodontic treatment. Cleft Palate J. 1986, 23, 175–205. [Google Scholar]
- Kim, J.; Jeong, W. Secondary bone grafting for alveolar clefts: Surgical timing, graft materials, and evaluation methods. Arch. Craniofac. Surg. 2022, 23, 53–58. [Google Scholar] [CrossRef]
- Dissaux, C.; Ruffenach, L.; Bruant-Rodier, C.; George, D.; Bodin, F.; Rémond, Y. Cleft Alveolar Bone Graft Materials: Literature Review. Cleft Palate Craniofac. J. 2022, 59, 336–346. [Google Scholar] [CrossRef]
- Kortebein, M.J.; Nelson, C.L.; Sadove, A.M. Retrospective analysis of 135 secondary alveolar cleft grafts using iliac or calvarial bone. J. Oral Maxillofac. Surg. 1991, 49, 493–498. [Google Scholar] [CrossRef]
- Desai, S.K.; Adirajaiah, S.; Desai, A.K.; Kumar, N. Observing the Eruption of Canine after Secondary Alveolar Bone Grafting. J. Oral Maxillofac. Surg. 2021, 79, 2562–2573. [Google Scholar] [CrossRef] [PubMed]
- Ranta, R. A review of tooth formation in children with cleft lip/palate. Am. J. Orthod Dentofacial. Orthop. 1986, 90, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Van Dyck, J.; Pérula, M.C.D.L.; Willems, G.; Verdonck, A. Dental development in cleft lip and palate patients: A systematic review. Forensic Sci. Int. 2019, 300, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Black, G.V. Anatomy of the Human Teeth; The S.S. White Dental Manufacturing Co.: Philadelphia, PA, USA, 1902; p. 17. [Google Scholar]
- Dwivedi, A.K.; Mallawaarachchi, I.; Alvarado, L.A. Analysis of small sample size studies using nonparametric bootstrap test with pooled resampling method. Stat. Med. 2017, 36, 2187–2205. [Google Scholar] [CrossRef]
- Padwa, B.L.; Tio, P.; Garkhail, P.; Nuzzi, L.C. Cone Beam Computed Tomographic Analysis Demonstrates a 94% Radiographic Success Rate in 783 Alveolar Bone Grafts. J. Oral Maxillofac. Surg. 2022, 80, 633–640. [Google Scholar] [CrossRef]
- du Prel, J.B.; Hommel, G.; Röhrig, B.; Blettner, M. Confidence interval or p-value?: Part 4 of a series on evaluation of scientific publications. Dtsch. Arztebl. Int. 2009, 106, 335–339. [Google Scholar] [CrossRef]
- Di Angelo, L.; Di Stefano, P.; Bernardi, S.; Continenza, M. A new computational method for automatic dental measurement: The case of maxillary central incisor. Comput. Biol. Med. 2016, 70, 202–209. [Google Scholar] [CrossRef]
- Haberthur, D.; Hlushchuk, R.; Wolf, T.G. Automated segmentation and description of the internal morphology of human permanent teeth by means of micro-CT. BMC Oral Health 2021, 21, 185. [Google Scholar] [CrossRef]
- Kuralt, M.; Cmok Kučič, A.; Gašperšič, R.; Grošelj, J.; Knez, M.; Fidler, A. Gingival shape analysis using surface curvature estimation of the intraoral scans. BMC Oral Health 2022, 22, 283. [Google Scholar]
| Erupting Canine | Non-Erupting Canine | p Value | |||
|---|---|---|---|---|---|
| Mean (%) | Standard Deviation (%) | Mean (%) | Standard Deviation (%) | ||
| Canine | 19.65 | 15.32 | 16.78 | 12.58 | NS |
| 1st Premolar | 21.64 | 23.09 | 12.34 | 8.98 | NS |
| 2nd Premolar | 21.68 | 26.82 | 17.17 | 12.83 | NS |
| Erupting Canine | Non-Erupting Canine | p Value | |||
|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | ||
| Canine | 0.18 | 4.76 | 0.18 | 1.89 | NS |
| 1st Premolar | 0.19 | 5.50 | 0.19 | 5.22 | NS |
| 2nd Premolar | 0.12 | 8.41 | 0.11 | 8.87 | NS |
| Erupting Canine | Non-Erupting Canine | p Value | |||
|---|---|---|---|---|---|
| Mean | Standard Deviation | Mean | Standard Deviation | ||
| Canine | 0.43 * | 0.77 | 0.35 * | 0.86 | 0.025 |
| 1st Premolar | 0.49 | 1.18 | 0.42 | 0.79 | NS |
| 2nd Premolar | 0.33 | 1.43 | 0.29 | 1.72 | NS |
| Erupting | Non-Erupting | |||||||
|---|---|---|---|---|---|---|---|---|
| Correlation | p Value Paired t Test | p Value Bootstrap Paired t Test | Power | Correlation | p Value Paired t Test | p Value Bootstrap Paired t Test | Power | |
| Canine | 0.53 | <0.001 * | 0.014 * | 99% | 0.48 | <0.001 * | <0.001 * | 100% |
| 1st Premolar | 0.76 | <0.001 * | 0.005 * | 99% | 0.35 | <0.001 * | <0.001 * | 100% |
| 2nd Premolar | 0.51 | <0.001 * | 0.033 * | 95% | 0.33 | 0.002 * | 0.071 | 93% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferguson, M.A.; Akyalcin, S.; Campos, H.; Gliksten, A.; Hargett, K.; Yang, S.; MacLaine, J. Evaluation of Dental Root Development Regarding Maxillary Canine Eruption Status after Secondary Alveolar Bone Grafting in Patients with Cleft Lip and Palate. Diagnostics 2023, 13, 1642. https://doi.org/10.3390/diagnostics13091642
Ferguson MA, Akyalcin S, Campos H, Gliksten A, Hargett K, Yang S, MacLaine J. Evaluation of Dental Root Development Regarding Maxillary Canine Eruption Status after Secondary Alveolar Bone Grafting in Patients with Cleft Lip and Palate. Diagnostics. 2023; 13(9):1642. https://doi.org/10.3390/diagnostics13091642
Chicago/Turabian StyleFerguson, Melissa A., Sercan Akyalcin, Hugo Campos, Abigail Gliksten, Kadriye Hargett, Stephanie Yang, and James MacLaine. 2023. "Evaluation of Dental Root Development Regarding Maxillary Canine Eruption Status after Secondary Alveolar Bone Grafting in Patients with Cleft Lip and Palate" Diagnostics 13, no. 9: 1642. https://doi.org/10.3390/diagnostics13091642
APA StyleFerguson, M. A., Akyalcin, S., Campos, H., Gliksten, A., Hargett, K., Yang, S., & MacLaine, J. (2023). Evaluation of Dental Root Development Regarding Maxillary Canine Eruption Status after Secondary Alveolar Bone Grafting in Patients with Cleft Lip and Palate. Diagnostics, 13(9), 1642. https://doi.org/10.3390/diagnostics13091642





