Diagnostic Value of Neutrophil CD64 in Sepsis Patients in the Intensive Care Unit: A Cross-Sectional Study
Abstract
1. Introduction
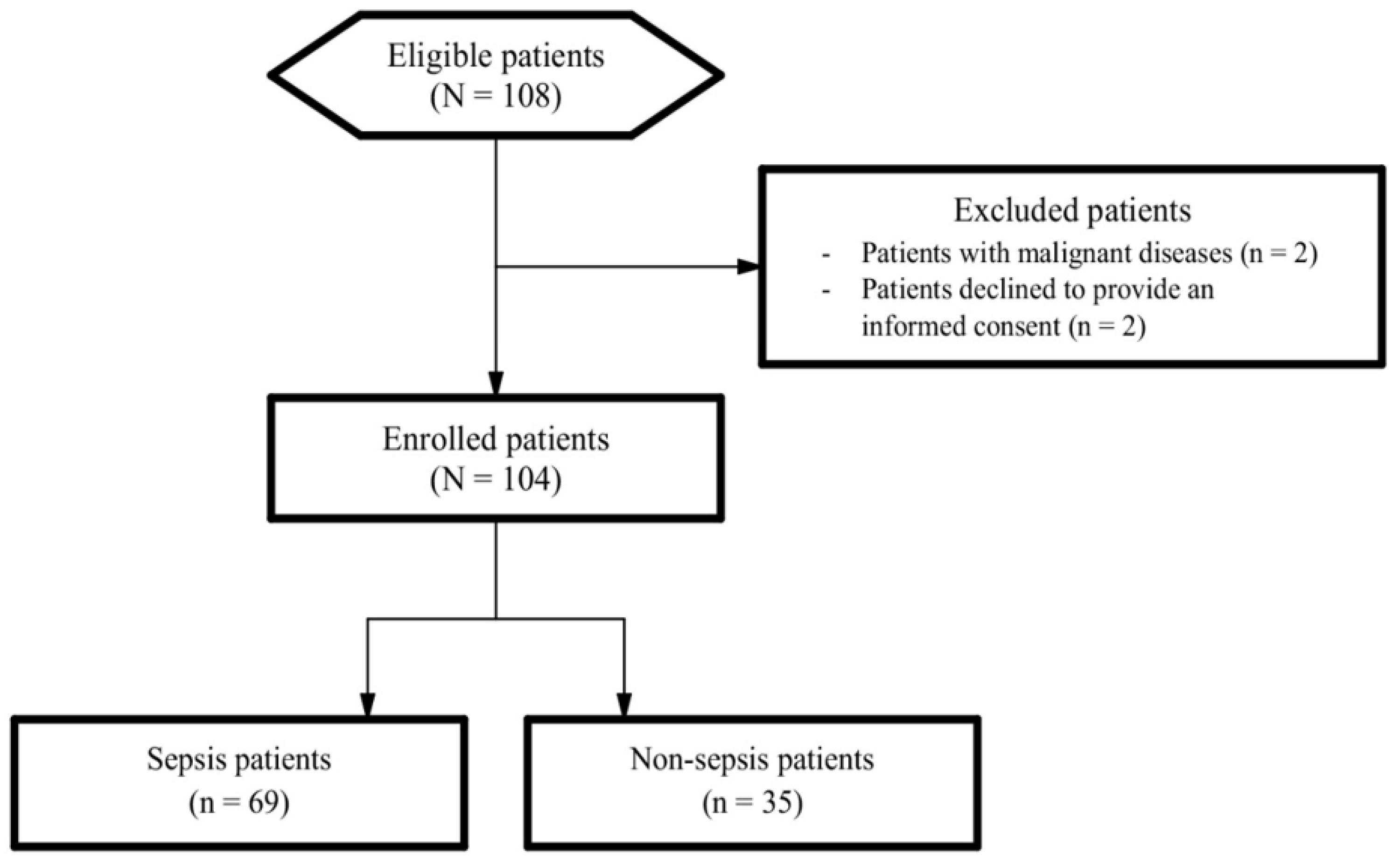
2. Materials and Methods
2.1. Study Context and Design
2.2. Measurement of nCD64 Levels
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics of Study Participants
3.2. The Predictive Values of nCD64, PCT, and WBC and Combinations of These Parameters
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martin, G.S.; Mannino, D.M.; Eaton, S.; Moss, M. The epidemiology of sepsis in the United States from 1979 through 2000. N. Engl. J. Med. 2003, 348, 1546–1554. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Bauer, M.; Gerlach, H.; Vogelmann, T.; Preissing, F.; Stiefel, J.; Adam, D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019—Results from a systematic review and meta-analysis. Crit. Care 2020, 24, 239. [Google Scholar] [CrossRef] [PubMed]
- Li, A.; Ling, L.; Qin, H.; Arabi, Y.; Myatra, S.; Egi, M.; Kim, J.H.; Nor, M.B.M.; Son, D.N.; Fang, W.-F.; et al. Epidemiology, Management, and Outcomes of Sepsis in Intensive Care Units Among Countries of Differing National Wealth Across Asia. Am. J. Respir. Crit. Care Med. 2022, 206, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- Kassyap, C.K.; Abraham, S.V.; Krishnan, S.V.; Palatty, B.U.; Rajeev, P.C. Factors Affecting Early Treatment Goals of Sepsis Patients Presenting to the Emergency Department. Indian J. Crit. Care Med. 2018, 22, 797–800. [Google Scholar]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit. Care Med. 2021, 49, e1063–e1143. [Google Scholar] [CrossRef]
- Bauman, K.A.; Han, M.K. Chapter 27-Gender Differences in Susceptibility, Outcomes, and Pathophysiology of Sepsis. In Principles of Gender-Specific Medicine, 2nd ed.; Legato, M.J., Ed.; Academic Press: San Diego, CA, USA, 2010; pp. 291–301. [Google Scholar]
- Sweeney, T.E.; Liesenfeld, O.; May, L. Diagnosis of bacterial sepsis: Why are tests for bacteremia not sufficient? Expert Rev. Mol. Diagn. 2019, 19, 959–962. [Google Scholar] [CrossRef]
- Barichello, T.; Generoso, J.S.; Singer, M.; Dal-Pizzol, F. Biomarkers for sepsis: More than just fever and leukocytosis—A narrative review. Crit. Care 2022, 26, 14. [Google Scholar] [CrossRef]
- Aziz, N.; Detels, R.; Quint, J.J.; Li, Q.; Gjertson, D.; Butch, A.W. Stability of cytokines, chemokines and soluble activation markers in unprocessed blood stored under different conditions. Cytokine 2016, 84, 17–24. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Lelubre, C. Sepsis Biomarkers. In Handbook of Sepsis; Springer: Berlin/Heidelberg, Germany, 2018; pp. 81–94. [Google Scholar]
- Marik, P.E. Don’t miss the diagnosis of sepsis! Crit. Care 2014, 18, 529. [Google Scholar] [CrossRef]
- Benz, F.; Roy, S.; Trautwein, C.; Roderburg, C.; Luedde, T. Circulating MicroRNAs as Biomarkers for Sepsis. Int. J. Mol. Sci. 2016, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Zhang, Y.; Lin, S.; Li, Y.; Hua, Y.; Zhou, K. Diagnostic significance of microRNAs in sepsis. PLoS ONE 2023, 18, e0279726. [Google Scholar] [CrossRef] [PubMed]
- Maiese, A.; Scatena, A.; Costantino, A.; Chiti, E.; Occhipinti, C.; La Russa, R.; Di Paolo, M.; Turillazzi, E.; Frati, P.; Fineschi, V. Expression of MicroRNAs in Sepsis-Related Organ Dysfunction: A Systematic Review. Int. J. Mol. Sci. 2022, 23, 9354. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, J.J. Neutrophil CD64 as a sepsis biomarker. Biochem. Med. 2011, 21, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, Z.-Y.; Zeng, L.; Zhang, A.-Q.; Pan, W.; Gu, W.; Jiang, J.-X. Neutrophil CD64 expression as a diagnostic marker for sepsis in adult patients: A meta-analysis. Crit Care. 2015, 19, 245–254. [Google Scholar] [CrossRef]
- Yeh, C.-F.; Wu, C.-C.; Liu, S.-H.; Chen, K.-F. Comparison of the accuracy of neutrophil CD64, procalcitonin, and C-reactive protein for sepsis identification: A systematic review and meta-analysis. Ann. Intensive Care 2019, 9, 5. [Google Scholar] [CrossRef]
- General Information of Cho Ray Hospital [in Vietnamese]. Available online: http://choray.vn/ (accessed on 1 March 2023).
- Negida, A.; Fahim, N.K.; Negida, Y. Sample Size Calculation Guide-Part 4: How to Calculate the Sample Size for a Diagnostic Test Accuracy Study based on Sensitivity, Specificity, and the Area under the ROC Curve. Adv. J. Emerg. Med. 2019, 3, e33. [Google Scholar]
- Sakr, Y.; Jaschinski, U.; Wittebole, X.; Szakmany, T.; Lipman, J.; Ñamendys-Silva, S.A.; Martin-Loeches, I.; Leone, M.; Lupu, M.-N.; Vincent, J.-L.; et al. Sepsis in Intensive Care Unit Patients: Worldwide Data From the Intensive Care over Nations Audit. Open Forum Infect. Dis. 2018, 5, ofy313. [Google Scholar] [CrossRef]
- Dimoula, A.; Pradier, O.; Kassengera, Z.; Dalcomune, D.; Turkan, H.; Vincent, J.-L. Serial determinations of neutrophil CD64 expression for the diagnosis and monitoring of sepsis in critically ill patients. Clin. Infect. Dis. 2013, 58, 820–829. [Google Scholar] [CrossRef]
- Lakhani, J.; Lakhani, R.; Desai, M.; Tripathi, S. SOFA vs APACHE II as ICU scoring system for sepsis: A dilemma. J. Integr. Health Sci. 2015, 3, 3–7. [Google Scholar] [CrossRef]
- Naqvi, I.H.; Mahmood, K.; Ziaullaha, S.; Kashif, S.M.; Sharif, A. Better prognostic marker in ICU-APACHE II, SOFA or SAP II! Pak. J. Med. Sci. 2016, 32, 1146–1151. [Google Scholar] [CrossRef] [PubMed]
- PE Phycoerythrin Fluorescence Quantitation Kit 2022. Available online: https://www.bdbiosciences.com/en-us/products/reagents/flow-cytometry-reagents/clinical-discovery-research/controls-and-supporting-reagents-ruo-gmp/pe-phycoerythrin-fluorescence-quantitation-kit.340495 (accessed on 1 March 2023).
- Mitsumoto-Kaseida, F.; Murata, M.; Ura, K.; Takayama, K.; Hiramine, S.; Shimizu, M.; Toyoda, K.; Ogawa, E.; Furusyo, N. The Expression Level of Neutrophil CD64 Is a Useful Marker of Systemic Inflammation Associated with HIV Infection. AIDS Res. Hum. Retrovir. 2017, 33, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Sanju, S.; Jain, P.; Priya, V.V.; Varma, P.K.; Mony, U. Quantitation of mHLA-DR and nCD64 by Flow Cytometry to Study Dysregulated Host Response: The Use of QuantiBRITE™ PE Beads and Its Stability. Appl. Biochem. Biotechnol. 2022, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pandey, K.; Malviya, D.; Awasthi, N.P.; Nath, S.S.; Harjai, M. Comparison of neutrophil CD64 and monocytic HLA-DR with existing biomarkers for the diagnosis and prognosis of sepsis. Anaesthesiol. Intensive Ther. 2021, 53, 304–311. [Google Scholar] [CrossRef] [PubMed]
- Pham Thao, T.N. Examining the Clinical Prognosis Levels of Cytokines in Patients with Sepsis. Ph.D. Thesis, Faculty of Medicine, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam, 2011. (In Vietnamese). [Google Scholar]
- Ye, Z.; Zou, H.; Liu, S.; Mei, C.; Chang, X.; Hu, Z.; Yang, H.; Wu, Y. Diagnostic performance of neutrophil CD64 index in patients with sepsis in the intensive care unit. J. Int. Med. Res. 2019, 47, 4304–4311. [Google Scholar] [CrossRef]
- Xu, C.; Li, S.; Wang, Y.; Zhang, M.; Zhou, M.; Medicine, C.C. Biomarkers in intensive care unit infections, friend or foe? J. Emerg. Crit. Care Med. 2019, 3, 27. [Google Scholar] [CrossRef]
- Yin, W.P.; Li, J.B.; Zheng, X.F.; An, L.; Shao, H.; Li, C.S. Effect of neutrophil CD64 for diagnosing sepsis in emergency department. World J. Emerg. Med. 2020, 11, 79–86. [Google Scholar] [CrossRef]
- Jämsä, J.; Ala-Kokko, T.; Huotari, V.; Ohtonen, P.; Savolainen, E.R.; Syrjälä, H. Neutrophil CD64, C-reactive protein, and procalcitonin in the identification of sepsis in the ICU-Post-test probabilities. J. Crit. Care 2018, 43, 139–142. [Google Scholar] [CrossRef]
- Burgos, J.; Los-Arcos, I.; de la Sierra, D.Á.; Falcó, V.; Aguiló, A.; Sánchez, I.; Almirante, B.; Gallo, M.M. Determination of neutrophil CD64 expression as a prognostic biomarker in patients with community-acquired pneumonia. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 1411–1416. [Google Scholar] [CrossRef]
- Cardelli, P.; Ferraironi, M.; Amodeo, R.; Tabacco, F.; De Blasi, R.; Nicoletti, M.; Sessa, R.; Petrucca, A.; Costante, A.; Cipriani, P. Evaluation of neutrophil CD64 expression and procalcitonin as useful markers in early diagnosis of sepsis. Int. J. Immunopathol. Pharmacol. 2008, 21, 43–49. [Google Scholar] [CrossRef]
- Righi, S.; Santambrogio, L.; Monsagrati, A.; Saliu, M.; Locati, L.; Radrizzani, D. Clinical Evaluation of Neutrophil CD64 as a Diagnostic Marker of Infection in a Polyvalent Intensive Care Unit. Infect. Dis. Clin. Pract. 2014, 22, 32–37. [Google Scholar] [CrossRef]
- Cui, W.; Xu, Y.; Fang, H.; Tong, W.; Zhu, L.; Jin, D.; Liu, H. Assessment of continuous neutrophil CD64 index measurement for diagnosing sepsis and predicting outcome in a Chinese pediatric intensive care unit: A prospective study. Transl. Pediatr. 2021, 10, 1668–1676. [Google Scholar] [CrossRef] [PubMed]
- Bauer, P.R.; Kashyap, R.; League, S.C.; Park, J.G.; Block, D.R.; Baumann, N.A.; Algeciras-Schimnich, A.; Jenkins, S.M.; Smith, C.Y.; Gajic, O.; et al. Diagnostic accuracy and clinical relevance of an inflammatory biomarker panel for sepsis in adult critically ill patients. Diagn. Microbiol. Infect. Dis. 2016, 84, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Cong, S.; Ma, T.; Di, X.; Tian, C.; Zhao, M.; Wang, K. Diagnostic value of neutrophil CD64, procalcitonin, and interleukin-6 in sepsis: A meta-analysis. BMC Infect. Dis. 2021, 21, 384. [Google Scholar] [CrossRef]
- Pewsner, D.; Battaglia, M.; Minder, C.; Marx, A.; Bucher, H.C.; Egger, M. Ruling a diagnosis in or out with “SpPIn” and “SnNOut”: A note of caution. BMJ 2004, 329, 209–213. [Google Scholar] [CrossRef]
- Wong, H.R.; Lindsell, C.J.; Pettilä, V.; Meyer, N.J.; Thair, S.A.; Karlsson, S.; Russell, J.A.; Fjell, C.D.; Boyd, J.H.; Ruokonen, E.; et al. A multibiomarker-based outcome risk stratification model for adult septic shock. Crit. Care Med. 2014, 42, 781–789. [Google Scholar] [CrossRef]
- Gibot, S.; Béné, M.C.; Noel, R.; Massin, F.; Guy, J.; Cravoisy, A.; Barraud, D.; Bittencourt, M.D.C.; Quenot, J.-P.; Bollaert, P.-E.; et al. Combination Biomarkers to Diagnose Sepsis in the Critically Ill Patient. Am. J. Respir. Crit. Care Med. 2012, 186, 65–71. [Google Scholar] [CrossRef]
- Zarkesh, M.; Sedaghat, F.; Heidarzadeh, A.; Tabrizi, M.; Bolooki-Moghadam, K.; Ghesmati, S. Diagnostic value of IL-6, CRP, WBC, and absolute neutrophil count to predict serious bacterial infection in febrile infants. Acta Med. Iran. 2015, 53, 408–411. [Google Scholar]
- Pradhan, S.; Ghimire, A.; Bhattarai, B.; Khanal, B.; Pokharel, K.; Lamsal, M.; Koirala, S. The role of C-reactive protein as a diagnostic predictor of sepsis in a multidisciplinary Intensive Care Unit of a tertiary care center in Nepal. Indian J. Crit. Care Med. 2016, 20, 417–420. [Google Scholar] [CrossRef]
- Gros, A.; Roussel, M.; Sauvadet, E.; Gacouin, A.; Marqué, S.; Chimot, L.; Lavoué, S.; Camus, C.; Fest, T.; Tulzo, Y.L. The sensitivity of neutrophil CD64 expression as a biomarker of bacterial infection is low in critically ill patients. Intensive Care Med. 2012, 38, 445–452. [Google Scholar] [CrossRef]
| Characteristics | Non-Sepsis Group | Sepsis Group | Total Population | p |
|---|---|---|---|---|
| n = 35 | n = 69 | n = 104 | OR (95%CI) | |
| Age (years) | 40.6 ± 15.8 | 61.3 ± 16.3 | 54.3 ± 18.9 | <0.001 t |
| Male | 27 (77.1) | 33 (47.8) | 60 (57.7) | 0.008 c 0.27 (0.11–0.68) |
| BMI (kg/m2) | 23.0 ± 2.8 | 23.2 ± 3.42 | 23.2 ± 3.21 | 0.778 t |
| APACHE II (score) | 15.0 [8.0; 18.0] | 21.0 [17.0; 25.0] | 19.0 [15.0; 23.0] | <0.001 u |
| SOFA (score) | 4.97 ± 2.65 | 9.22 ± 3.97 | 7.79 ± 4.10 | <0.001 t |
| Serum lactate (mmol/L) | 2.15 [1.58; 3.72] | 2.40 [1.4; 4.13] | 2.20 [1.48; 4.12] | <0.926 u |
| Deaths | 7 (20.0) | 30 (43.5) | 37 (35.6) | 0.02 c 3.08 (1.18–8.00) |
| Ventilator days (days) | 3.00 [0.00; 11.0] | 7.00 [4.00; 10.5] | 6.00 [3.0; 10.75] | 0.007 u |
| ICU length of stay (days) | 4.00 [2.50; 12.0] | 7.00 [4.00; 11.0] | 7.00 [4.00; 12.0] | 0.054 u |
| Hospital length of stay (days) | 10.0 [7.00; 18.0] | 14.0 [8.50; 22.0] | 13.00 [8.25; 20.0] | 0.11 u |
| Characteristics | Non-Sepsis Group n = 35 | Sepsis Group n = 69 | p * |
|---|---|---|---|
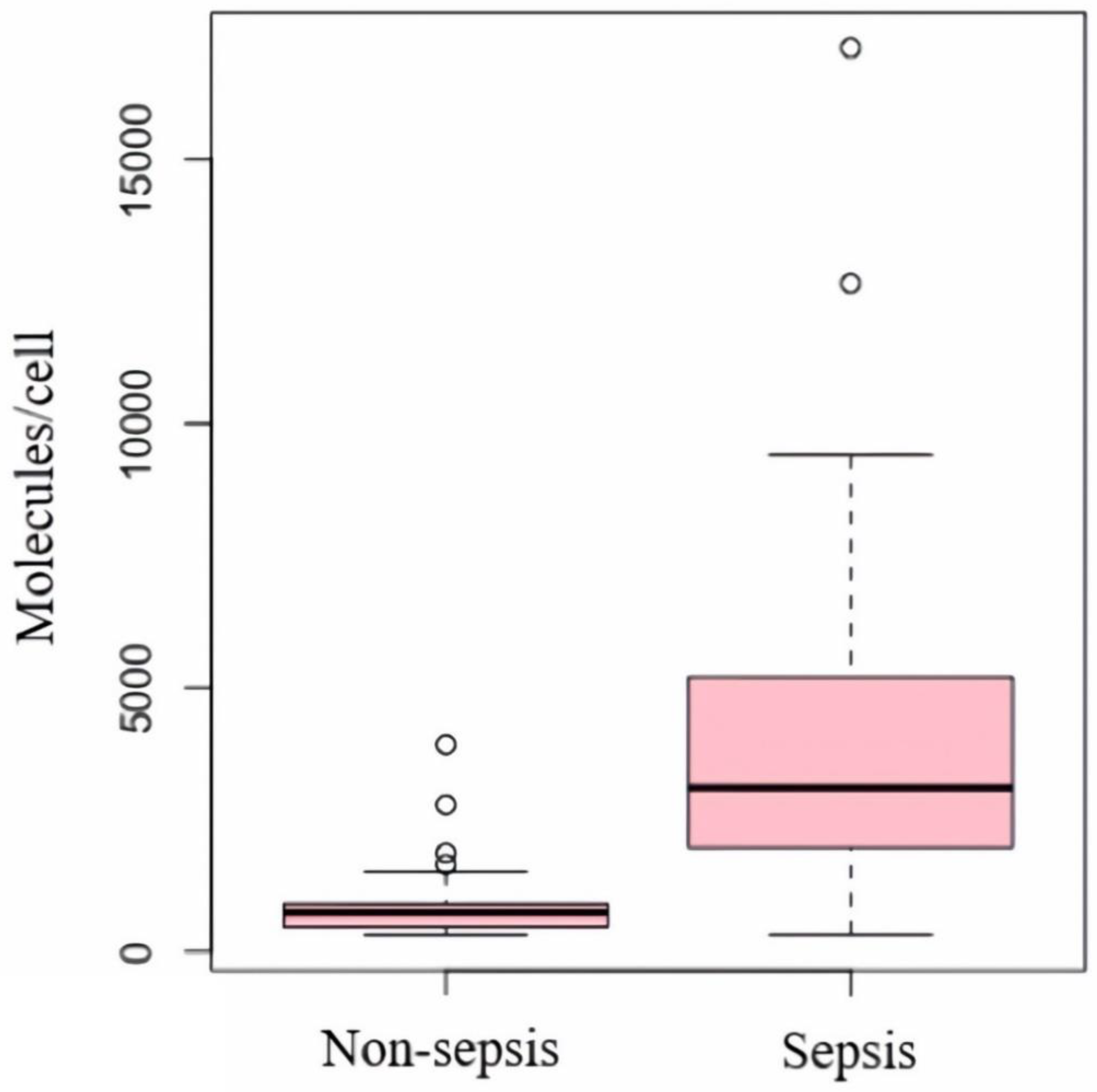
| nCD64 (molecules/cell) | 745 [458; 906] | 3106 [1970; 5200] | <0.001 |
| PCT (ng/mL) | 1.10 [0.30; 4.63] | 43.4 [4.97; 70.30] | <0.001 |
| WBC (G/L) | 17.3 [13.1; 20.4] | 13.9 [10.2; 18.5] | 0.023 |
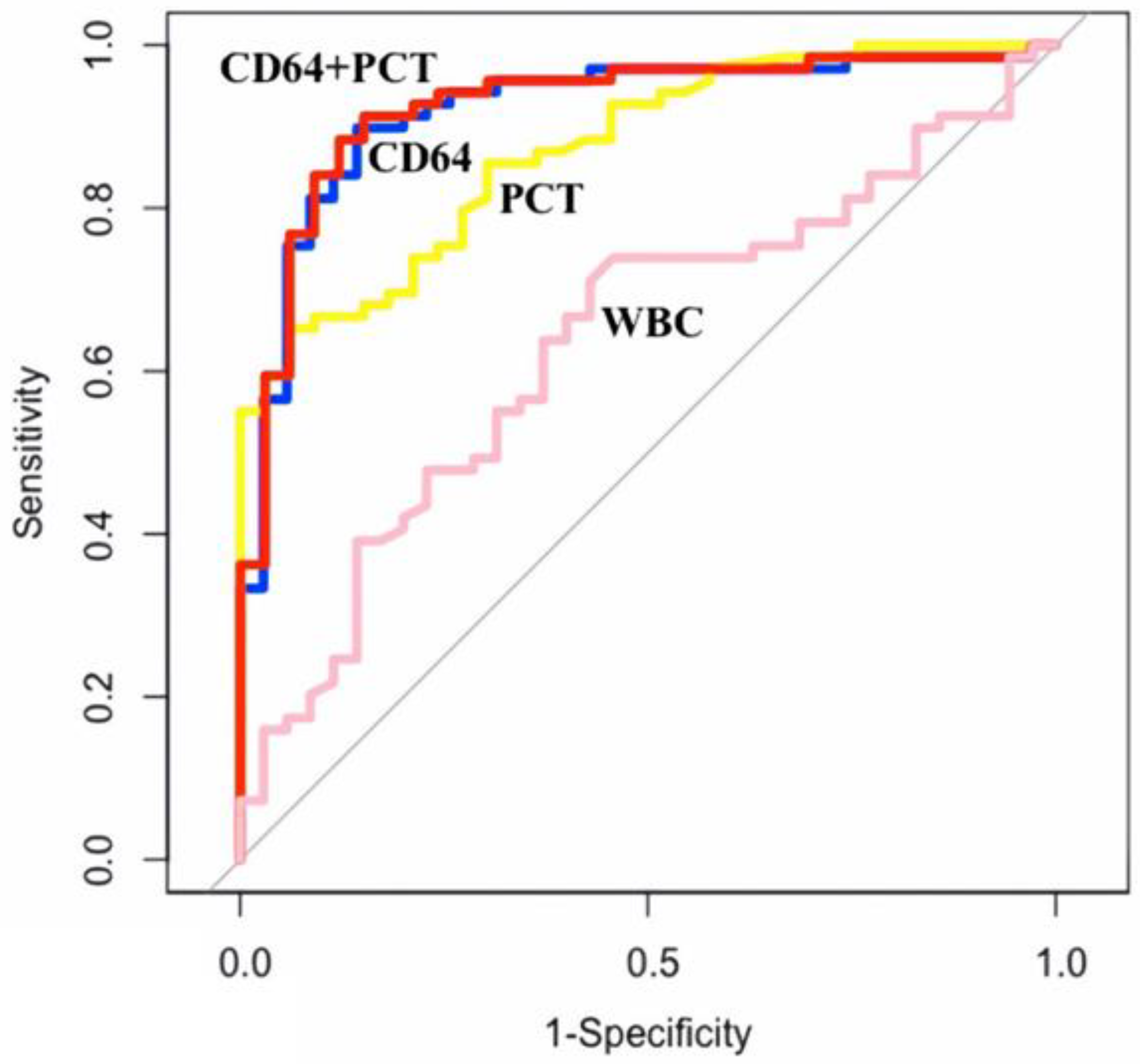
| Biomarkers | AUC | 95%CI | Cut-off | Sens | Spec | PPV | NPV |
|---|---|---|---|---|---|---|---|
| nCD64 (molecules/cell) | 0.920 | 0.863–0.978 | 1311 | 89.9% | 85.7% | 92.5% | 81.1% |
| PCT (ng/mL) | 0.872 | 0.806–0.938 | 13.385 | 65.2% | 93.9% | 95.7% | 56.4% |
| WBC (G/L) | 0.637 | 0.526–0.748 | 17.19 | 73.9% | 54.3% | 76.1% | 51.4% |
| nCD64 + PCT | 0.924 | 0.868–0.981 | - | 88.4% | 87.9% | 93.8% | 78.4% |
| nCD64 + WBC | 0.906 | 0.845–0.967 | - | 78.3% | 97% | 98.2% | 68.1% |
| nCD64 + WBC + PCT | 0.919 | 0.863–0.975 | - | 79.7% | 97% | 98.2% | 69.6% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pham, H.M.; Nguyen, D.L.M.; Duong, M.C.; Tran, L.T.; Pham, T.T.N. Diagnostic Value of Neutrophil CD64 in Sepsis Patients in the Intensive Care Unit: A Cross-Sectional Study. Diagnostics 2023, 13, 1427. https://doi.org/10.3390/diagnostics13081427
Pham HM, Nguyen DLM, Duong MC, Tran LT, Pham TTN. Diagnostic Value of Neutrophil CD64 in Sepsis Patients in the Intensive Care Unit: A Cross-Sectional Study. Diagnostics. 2023; 13(8):1427. https://doi.org/10.3390/diagnostics13081427
Chicago/Turabian StylePham, Huy Minh, Duy Ly Minh Nguyen, Minh Cuong Duong, Linh Thanh Tran, and Thao Thi Ngoc Pham. 2023. "Diagnostic Value of Neutrophil CD64 in Sepsis Patients in the Intensive Care Unit: A Cross-Sectional Study" Diagnostics 13, no. 8: 1427. https://doi.org/10.3390/diagnostics13081427
APA StylePham, H. M., Nguyen, D. L. M., Duong, M. C., Tran, L. T., & Pham, T. T. N. (2023). Diagnostic Value of Neutrophil CD64 in Sepsis Patients in the Intensive Care Unit: A Cross-Sectional Study. Diagnostics, 13(8), 1427. https://doi.org/10.3390/diagnostics13081427







