The Role of Telemedicine in Prehospital Traumatic Hand Injury Evaluation
Abstract
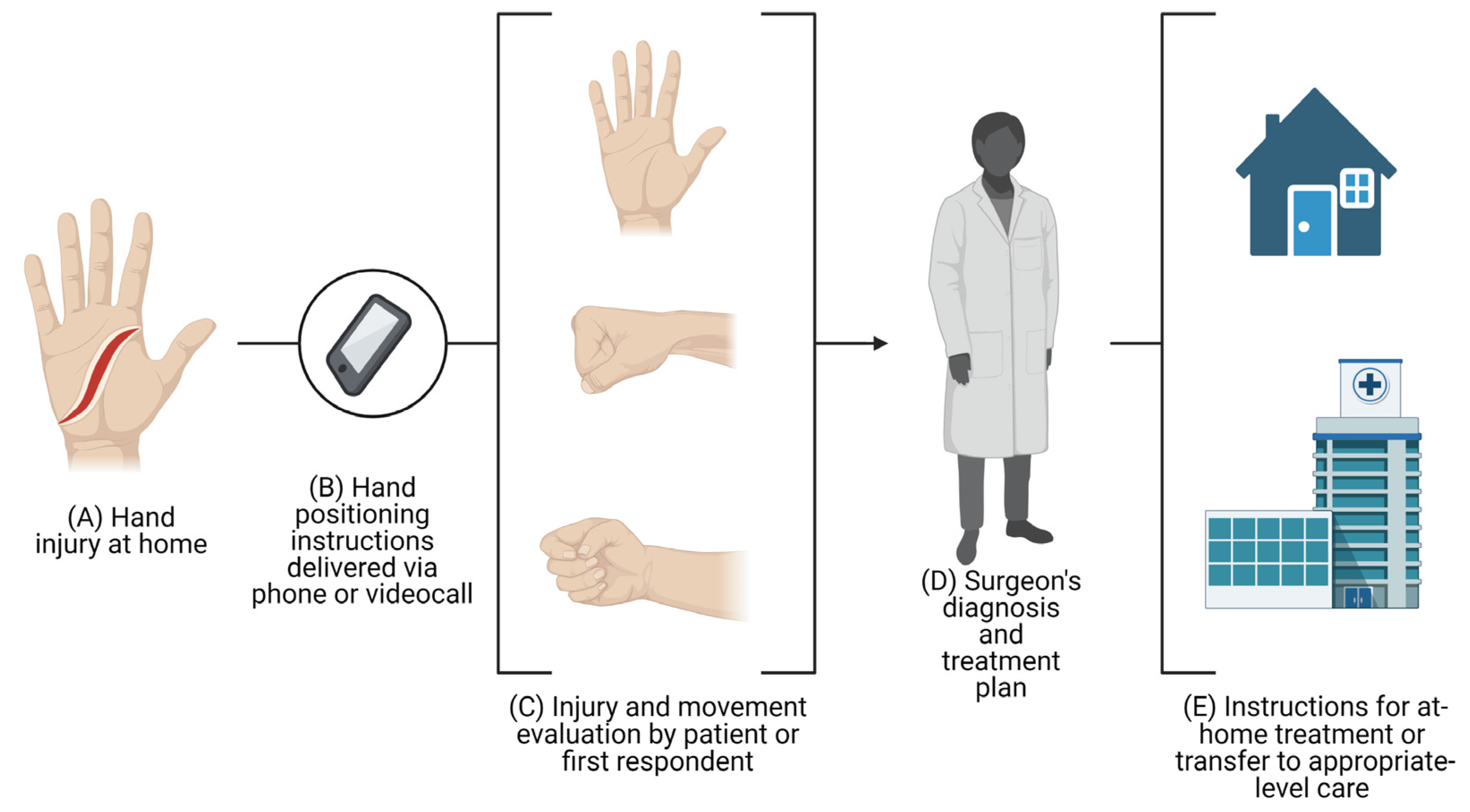
1. Introduction
2. Study Outcomes
2.1. Treatment Outcomes
2.2. Triage Outcomes
2.3. Diagnosis Outcomes
2.4. Cost Analysis Outcomes
2.5. Time Outcomes
3. Impact of Telemedicine for Remote Evaluation of Hand Injuries during the Current COVID-19 Pandemic
4. Legal Implications of Telemedicine in Traumatic Hand Injuries
5. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bureau of Labor Statistics. Number of Nonfatal Occupational Injuries and Illnesses Involving Days away from Work by Occupation and Selected Parts of Body Affected by Injury or Illness, Private Industry; Bureau of Labor Statistics: Washington, DC, USA, 2018. [Google Scholar]
- Ootes, D.; Lambers, K.T.; Ring, D.C. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand 2012, 7, 18–22. [Google Scholar] [CrossRef]
- Bauer, A.S.; Blazar, P.E.; Earp, B.E.; Louie, D.L.; Pallin, D.J. Characteristics of emergency department transfers for hand surgery consultation. Hand 2013, 8, 12–16. [Google Scholar] [CrossRef]
- Drolet, B.C.; Tandon, V.J.; Ha, A.Y.; Guo, Y.; Phillips, B.Z.; Akelman, E.; Schmidt, S.T. Unnecessary Emergency Transfers for Evaluation by a Plastic Surgeon: A Burden to Patients and the Health Care System. Plast. Reconstr. Surg. 2016, 137, 1927–1933. [Google Scholar] [CrossRef] [PubMed]
- Trzeciak, S.; Rivers, E.P. Emergency department overcrowding in the United States: An emerging threat to patient safety and public health. Emerg. Med. J. 2003, 20, 402–405. [Google Scholar] [CrossRef]
- Lauque, D.; Khalemsky, A.; Boudi, Z.; Östlundh, L.; Xu, C.; Alsabri, M.; Onyeji, C.; Cellini, J.; Intas, G.; Soni, K.D.; et al. Length-of-Stay in the Emergency Department and In-Hospital Mortality: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 12, 32. [Google Scholar] [CrossRef]
- Hsu, C.M.; Liang, L.L.; Chang, Y.T.; Juang, W.C. Emergency department overcrowding: Quality improvement in a Taiwan Medical Center. J. Formos. Med. Assoc. 2019, 118, 186–193. [Google Scholar] [CrossRef]
- Aungst, L.A. Can telemedicine improve triage and patient satisfaction in urgent care settings? J. Am. Assoc. Nurse Pract. 2019, 31, 162–166. [Google Scholar] [CrossRef] [PubMed]
- Rademacher, N.J.; Cole, G.; Psoter, K.J.; Kelen, G.; Fan, J.W.Z.; Gordon, D.; Razzak, J. Use of Telemedicine to Screen Patients in the Emergency Department: Matched Cohort Study Evaluating Efficiency and Patient Safety of Telemedicine. JMIR Med. Inform. 2019, 7, e11233. [Google Scholar] [CrossRef] [PubMed]
- Alfaleh, A.; Alkattan, A.; Alageel, A.; Salah, M.; Almutairi, M.; Sagor, K.; Alabdulkareem, K. The role of telemedicine services in changing users’ intentions for presenting to the emergency departments in Saudi Arabia. Digit. Health 2022, 8, 20552076221091358. [Google Scholar] [CrossRef]
- World Health Organization. Telehealth. Available online: https://www.who.int/gho/goe/telehealth/en/ (accessed on 6 June 2020).
- Ohannessian, R.; Duong, T.A.; Odone, A. Global Telemedicine Implementation and Integration within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill. 2020, 6, e18810. [Google Scholar] [CrossRef]
- Bart, N.K.; Emmanuel, S.; Friits-Lamora, R.; Larkins, E.; Kotlyar, E.; Muthiah, K.; Jabbour, A.; Hayward, C.; Jansz, P.C.; Keogh, A.M.; et al. Rapid triage and transition to telehealth for heart transplant patients in the COVID-19 pandemic setting. J. Telemed. Telecare 2023, 1357633x231151714. [Google Scholar] [CrossRef] [PubMed]
- Venkatesan, A.; Iyengar, K.; Loh, W.Y. Strategies in reconfiguration of hand injuries management during COVID-19 pandemic. J. Clin. Orthop. Trauma 2020, 11, 697–699. [Google Scholar] [CrossRef] [PubMed]
- Reissis, D.; Georgiou, A.; Nikkhah, D.; O’Toole, G.U.K. Response to the COVID-19 Pandemic: Managing Plastic Surgery Patients Safely. Plast. Reconstr. Surg. 2020, 146, 250e–251e. [Google Scholar] [CrossRef] [PubMed]
- Langabeer, J.R., 2nd; Gonzalez, M.; Alqusairi, D.; Champagne-Langabeer, T.; Jackson, A.; Mikhail, J.; Persse, D. Telehealth-Enabled Emergency Medical Services Program Reduces Ambulance Transport to Urban Emergency Departments. West. J. Emerg. Med. 2016, 17, 713–720. [Google Scholar] [CrossRef]
- Schröder, H.; Beckers, S.K.; Ogrodzki, K.; Borgs, C.; Ziemann, S.; Follmann, A.; Rossaint, R.; Felzen, M. Tele-EMS physicians improve life-threatening conditions during prehospital emergency missions. Sci. Rep. 2021, 11, 14366. [Google Scholar] [CrossRef]
- Jaeger, L.R.; McCartin, M.P.; Haamid, A.; Weber, J.M.; Tataris, K.L. TeleEMS: An EMS Telemedicine Pilot Program Barriers to Implementation. Prehosp. Emerg. Care 2023, 1–6. [Google Scholar] [CrossRef]
- Fleming, A.; Whitty, K. Implementation of a Standardized Protocol for Telehealth Provider in Triage to Improve Efficiency and ED Throughput: A Quality Improvement Project. Adv. Emerg. Nurs. J. 2022, 44, 312–321. [Google Scholar] [CrossRef]
- Khoo, S.S.; Guruseelan, N.; Gunasagaran, J.; Shamsul, S.A.; Razak, I.; Ahmad, T.S. Reliability of WhatsApp images of plain radiographs to diagnose fractures of the hand and wrist. J. Hand Surg. Eur. Vol. 2023, 17531934231151202. [Google Scholar] [CrossRef]
- Lesher, A.; McDuffie, L.; Smith, T.; Foster, A.; Ruggiero, K.; Barroso, J.; Gavrilova, Y. Optimizing an Outpatient mHealth Intervention for Children with Burns: A Convergent Mixed-Methods Study. J. Burn Care Res. 2023, irad020. [Google Scholar] [CrossRef] [PubMed]
- Buntic, R.F.; Siko, P.P.; Buncke, G.M.; Ruebeck, D.; Kind, G.M.; Buncke, H.J. Using the Internet for rapid exchange of photographs and X-ray images to evaluate potential extremity replantation candidates. J. Trauma 1997, 43, 342–344. [Google Scholar] [CrossRef]
- Hsieh, C.H.; Tsai, H.H.; Yin, J.W.; Chen, C.Y.; Yang, J.C.; Jeng, S.F. Teleconsultation with the mobile camera-phone in digital soft-tissue injury: A feasibility study. Plast. Reconstr. Surg. 2004, 114, 1776–1782. [Google Scholar] [CrossRef]
- Lam, T.K.; Preketes, A.; Gates, R. Mobile phone photo messaging assisted communication in the assessment of hand trauma. ANZ J. Surg. 2004, 74, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.H.; Jeng, S.F.; Chen, C.Y.; Yin, J.W.; Yang, J.C.S.; Tsai, H.H.; Yeh, M.C. Teleconsultation with the mobile camera-phone in remote evaluation of replantation potential. J. Trauma-Inj. Infect. Crit. Care 2005, 58, 1208–1212. [Google Scholar] [CrossRef] [PubMed]
- Diver, A.J.; Lewis, H.; Gordon, D.J. Telemedicine and trauma referrals—A plastic surgery pilot project. Ulst. Med. J. 2009, 78, 113–114. [Google Scholar]
- Althubaiti, G.; Buntic, R.; Brooks, D. The utility of multimedia in the diagnosis and management of acute and subacute problems in hand surgery. Ann. Plast. Surg. 2012, 68, 389–390. [Google Scholar] [CrossRef] [PubMed]
- Waterman, B.R.; Laughlin, M.D.; Belmont, P.J., Jr.; Schoenfeld, A.J.; Pallis, M.P.; Belmont, P.J., Jr. Enhanced casualty care from a Global Military Orthopaedic Teleconsultation Program. Injury 2014, 45, 1736–1740. [Google Scholar] [CrossRef]
- Hara, T.; Nishizuka, T.; Yamamoto, M.; Iwatsuki, K.; Natsume, T.; Hirata, H. Teletriage for patients with traumatic finger injury directing emergency medical transportation services to appropriate hospitals: A pilot project in Nagoya City, Japan. Injury 2015, 46, 1349–1353. [Google Scholar] [CrossRef] [PubMed]
- Dehours, E.; Tourneret, M.-L.; Roux, P.; Tabarly, J. Benefits of photograph transmission for trauma management in isolated areas: Cases from the French tele-medical assistance service. Int. Marit. Health 2016, 67, 83–87. [Google Scholar] [CrossRef]
- Paik, A.M.; Granick, M.S.; Scott, S. Plastic surgery telehealth consultation expedites Emergency Department treatment. J. Telemed. Telecare 2017, 23, 321–327. [Google Scholar] [CrossRef]
- Tripod, M.; Tait, M.; Bracey, J.; Sexton, K.; Beck, W.; Wyrick, T.O. The Use of Telemedicine Decreases Unnecessary Hand Trauma Transfers. Hand 2020, 15, 422–427. [Google Scholar] [CrossRef]
- Bracey, J.W.; Tait, M.A.; Hollenberg, S.B.; Wyrick, T.O. A Novel Telemedicine System for Care of Statewide Hand Trauma. Hand 2019, 2, 253–257. [Google Scholar] [CrossRef] [PubMed]
- Westley, S.; Mistry, R.; Dheansa, B. Accuracy of virtual assessment in hand trauma. JPRAS Open 2022, 31, 92–98. [Google Scholar] [CrossRef]
- Bracey, J.; Morell, S.; Tait, M.; Frazier, G.T.; Wyrick, T.O. Assessment of Telemedicine and Phone Consultation Effects on Rate of Hand Transfers to Trauma Centers and Specialty Services Referrals. Hand 2021, 15589447211044783. [Google Scholar] [CrossRef]
- Mohr, N.M.; Young, T.; Harland, K.K.; Skow, B.; Wittrock, A.; Bell, A.; Ward, M.M. Emergency Department Telemedicine Shortens Rural Time-To-Provider and Emergency Department Transfer Times. Telemed. J. e-Health 2018, 24, 582–593. [Google Scholar] [CrossRef] [PubMed]
- Mohr, N.M.; Vakkalanka, J.P.; Harland, K.K.; Bell, A.; Skow, B.; Shane, D.M.; Ward, M.M. Telemedicine Use Decreases Rural Emergency Department Length of Stay for Transferred North Dakota Trauma Patients. Telemed. J. e-Health 2018, 24, 194–202. [Google Scholar] [CrossRef]
- Tsou, C.; Robinson, S.; Boyd, J.; Jamieson, A.; Blakeman, R.; Yeung, J.; McDonnell, J.; Waters, S.; Bosich, K.; Hendrie, D. Effectiveness of Telehealth in Rural and Remote Emergency Departments: Systematic Review. J. Med. Internet Res. 2021, 23, e30632. [Google Scholar] [CrossRef] [PubMed]
- Gidora, H.; Borycki, E.M.; Kushniruk, A.W. Effects of Telenursing Triage and Advice on Healthcare Costs and Resource Use. Stud. Health Technol. Inform. 2019, 257, 133–139. [Google Scholar] [PubMed]
- Reiss, A.B.; De Leon, J.; Dapkins, I.P.; Shahin, G.; Peltier, M.R.; Goldberg, E.R. A Telemedicine Approach to COVID-19 Assessment and Triage. Medicina 2020, 56, 461. [Google Scholar] [CrossRef]
- Blom, L.; Boissin, C.; Allorto, N.; Wallis, L.; Hasselberg, M.; Laflamme, L. Accuracy of acute burns diagnosis made using smartphones and tablets: A questionnaire-based study among medical experts. BMC Emerg. Med. 2017, 17, 39. [Google Scholar] [CrossRef]
- Boissin, C.; Blom, L.; Wallis, L.; Laflamme, L. Image-based teleconsultation using smartphones or tablets: Qualitative assessment of medical experts. Emerg. Med. J. 2017, 34, 95–99. [Google Scholar] [CrossRef]
- Fonseca, A.S.; Goldenberg, D.C.; Stocchero, G.F.; Luiz, A.V.; Gemperli, R. Validation of Videoconference with Smartphones in Telemedicine Facial Trauma Care: Analysis of Concordance to On-Site Evaluation. Ann. Plast. Surg. 2016, 77, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Said, M.; Ngo, V.; Hwang, J.; Hom, D.B. Navigating telemedicine for facial trauma during the COVID-19 pandemic. Laryngoscope Investig. Otolaryngol. 2020, 5, 649–656. [Google Scholar] [CrossRef]
- De la Torre-Díez, I.; López-Coronado, M.; Vaca, C.; Aguado, J.S.; de Castro, C. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: A systematic review. Telemed. J. e-Health 2015, 21, 81–85. [Google Scholar] [CrossRef]
- Eze, N.D.; Mateus, C.; Cravo Oliveira Hashiguchi, T. Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS ONE 2020, 15, e0237585. [Google Scholar] [CrossRef]
- Snoswell, C.L.; Taylor, M.L.; Comans, T.A.; Smith, A.C.; Gray, L.C.; Caffery, L.J. Determining if Telehealth Can Reduce Health System Costs: Scoping Review. J. Med. Internet Res. 2020, 22, e17298. [Google Scholar] [CrossRef] [PubMed]
- San Diego ED leverages telemedicine in a bid to ease crowding, long wait times. ED Manag. 2013, 25, 93–95.
- Guss, B.; Mishkin, D.; Sharma, R. Using Telemedicine to Address Crowding in the ED. ED Manag. 2016, 28, 127–131. [Google Scholar]
- Saleh, S.; Faulkner, H.; Golledge, K.; Graham, D.J.; Lawson, R.D.; Symes, M.J.; Sivakumar, B.S. The Impact of COVID-19 on Hand Trauma. Hand 2021, 15589447211028918. [Google Scholar] [CrossRef] [PubMed]
- Pidgeon, T.E.; Parthiban, S.; Malone, P.; Foster, M.; Chester, D.L. Injury patterns of patients with upper limb and hand trauma sustained during the COVID-19 pandemic lockdown in the UK: A retrospective cohort study. Hand Surg. Rehabil. 2021, 40, 235–240. [Google Scholar] [CrossRef]
- Saha, S.; Dash, S.; Ansari, M.T.; Bichupuriya, A.D.; Gupta, A.K.; Singhal, M. Optimising Hand Surgery during COVID-19 Pandemic. J. Hand Surg. Asian Pac. Vol. 2021, 26, 84–91. [Google Scholar] [CrossRef]
- Cordova, L.Z.; Savage, N.; Ram, R.; Ellis, L.; Tobin, V.; Rozen, W.M.; Seifman, M.A. Effects of COVID-19 lockdown measures on emergency plastic and reconstructive surgery presentations. ANZ J. Surg. 2021, 91, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Fortané, T.; Bouyer, M.; Le Hanneur, M.; Belvisi, B.; Courtiol, G.; Chevalier, K.; Dainotto, C.; Loret, M.; Kling, A.; Bentejac, A.; et al. Epidemiology of hand traumas during the COVID-19 confinement period. Injury 2021, 52, 679–685. [Google Scholar] [CrossRef]
- Poggetti, A.; Del Chiaro, A.; Nucci, A.M.; Suardi, C.; Pfanner, S. How hand and wrist trauma has changed during COVID-19 emergency in Italy: Incidence and distribution of acute injuries. What to learn? J. Clin. Orthop. Trauma 2021, 12, 22–26. [Google Scholar] [CrossRef]
- Leti Acciaro, A.; Montanari, S.; Venturelli, M.; Starnoni, M.; Adani, R. Retrospective study in clinical governance and financing system impacts of the COVID-19 pandemic in the hand surgery and microsurgery HUB center. Musculoskelet. Surg. 2021, 106, 291–296. [Google Scholar] [CrossRef]
- Svorai Band, S.; Gannot, G.; Oron, A. Failure to Approach the Emergency Room Following a Hand Laceration Due to Fear during the COVID-19 Pandemic. Isr. Med. Assoc. J. 2021, 23, 88. [Google Scholar]
- De Meijer, P.P.; Karlsson, J.; LaPrade, R.F.; Verhaar, J.A.; Wijdicks, C.A. A guideline to medical photography: A perspective on digital photography in an orthopaedic setting. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 2606–2611. [Google Scholar] [CrossRef] [PubMed]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Karan, A. To control the COVID-19 outbreak, young, healthy patients should avoid the emergency department. BMJ 2020, 368, m1040. [Google Scholar] [CrossRef]
- Gilbert, A.W.; Billany, J.C.T.; Adam, R.; Martin, L.; Tobin, R.; Bagdai, S.; Galvin, N.; Farr, I.; Allain, A.; Davies, L.; et al. Rapid implementation of virtual clinics due to COVID-19: Report and early evaluation of a quality improvement initiative. BMJ Open Qual. 2020, 9, e000985. [Google Scholar] [CrossRef]
- Popova, D.; Young, K.; Hobday, D.; Welman, T.; Pahal, G.S. Hand Trauma Virtual Clinics Prove Effective during the COVID-19 Pandemic. Hand 2021, 15589447211017210. [Google Scholar] [CrossRef]
- Kahan, E.H.; Shin, J.D.; Jansen, M.E.; Parker, R.H.; Parikh, R. Malpractice Cases Arising from Telephone Based Telemedicine Triage in Ophthalmology. In Seminars in Ophthalmology; Taylor & Francis: Abingdon, UK, 2022; pp. 1–12. [Google Scholar] [CrossRef]
- Ernesäter, A.; Winblad, U.; Engström, M.; Holmström, I.K. Malpractice claims regarding calls to Swedish telephone advice nursing: What went wrong and why? J. Telemed. Telecare 2012, 18, 379–383. [Google Scholar] [CrossRef] [PubMed]
- Ernesäter, A.; Engström, M.; Winblad, U.; Holmström, I.K. A comparison of calls subjected to a malpractice claim versus ‘normal calls’ within the Swedish healthcare direct: A case-control study. BMJ Open 2014, 4, e005961. [Google Scholar] [CrossRef]
- Di Paolo, M.; Guidi, B.; Picano, E.; Caramella, D. Emergency radiology without the radiologist: The forensic perspective. Radiol. Med. 2009, 114, 475–483. [Google Scholar] [CrossRef]
- Schmitt, B.D. Telephone triage liability: Protecting your patients and your practice from harm. Adv. Pediatr. 2008, 55, 29–42. [Google Scholar] [CrossRef]
- Wheeler, S.Q.; Greenberg, M.E.; Mahlmeister, L.; Wolfe, N. Safety of clinical and non-clinical decision makers in telephone triage: A narrative review. J. Telemed. Telecare 2015, 21, 305–322. [Google Scholar] [CrossRef] [PubMed]
- Rathbone, A.L.; Prescott, J. The Use of Mobile Apps and SMS Messaging as Physical and Mental Health Interventions: Systematic Review. J. Med. Internet Res. 2017, 19, e295. [Google Scholar] [CrossRef]
- McKay, F.H.; Cheng, C.; Wright, A.; Shill, J.; Stephens, H.; Uccellini, M. Evaluating mobile phone applications for health behaviour change: A systematic review. J. Telemed. Telecare 2018, 24, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Al-Arkee, S.; Mason, J.; Lane, D.A.; Fabritz, L.; Chua, W.; Haque, M.S.; Jalal, Z. Mobile Apps to Improve Medication Adherence in Cardiovascular Disease: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e24190. [Google Scholar] [CrossRef]
- Pan, S.; Rong, L.Q. Mobile Applications in Clinical and Perioperative Care for Anesthesia: Narrative Review. J. Med. Internet Res. 2021, 23, e25115. [Google Scholar] [CrossRef] [PubMed]
- Montano, I.H.; de la Torre Díez, I.; López-Izquierdo, R.; Villamor, M.A.C.; Martín-Rodríguez, F. Mobile Triage Applications: A Systematic Review in Literature and Play Store. J. Med. Syst. 2021, 45, 86. [Google Scholar] [CrossRef]
- Boltin, N.; Valdes, D.; Culley, J.M.; Valafar, H. Mobile Decision Support Tool for Emergency Departments and Mass Casualty Incidents (EDIT): Initial Study. JMIR Mhealth Uhealth 2018, 6, e10727. [Google Scholar] [CrossRef] [PubMed]
- Savatmongkorngul, S.; Yuksen, C.; Suwattanasilp, C.; Sawanyawisuth, K.; Sittichanbuncha, Y. Is a mobile emergency severity index (ESI) triage better than the paper ESI? Intern. Emerg. Med. 2017, 12, 1273–1277. [Google Scholar] [CrossRef] [PubMed]
- Emergency Severity Index (ESI): A Triage Tool for Emergency Departments. Available online: https://www.ahrq.gov/patient-safety/settings/emergency-dept/esi.html (accessed on 22 February 2023).
- Freshwater, E.S.; Crouch, R. Technology for trauma: Testing the validity of a smartphone app for pre-hospital clinicians. Int. Emerg. Nurs. 2015, 23, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, D.; McKenna, M.; Duncan, E.A.S.; Laird, C.; Lyon, R.; Corfield, A. Critcomms: A national cross-sectional questionnaire based study to investigate prehospital handover practices between ambulance clinicians and specialist prehospital teams in Scotland. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 45. [Google Scholar] [CrossRef]
- Sutham, K.; Khuwuthyakorn, P.; Thinnukool, O. Thailand medical mobile application for patients triage base on criteria based dispatch protocol. BMC Med. Inform. Decis. Mak. 2020, 20, 66. [Google Scholar] [CrossRef]
- Nimmolrat, A.; Sutham, K.; Thinnukool, O. Patient triage system for supporting the operation of dispatch centres and rescue teams. BMC Med. Inform. Decis. Mak. 2021, 21, 68. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, R.G.; Silva, G.S.; Lima, F.O.; Yeh, Y.C.; Fleming, C.; Branco, D.; Yancey, A.H.; Ratcliff, J.J.; Wages, R.K.; Doss, E.; et al. The FAST-ED App: A Smartphone Platform for the Field Triage of Patients with Stroke. Stroke 2017, 48, 1278–1284. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, A.; Brasseur, E.; Ghuysen, A.; D’Orio, V. New method to regulate unscheduled urgent care: The ODISSEE interactive self-triage platform. Rev. Med. Liege 2020, 75, 159–163. [Google Scholar]
- Gilbert, A.; Diep, A.N.; Boufraioua, M.; Pétré, B.; Donneau, A.F.; Ghuysen, A. Patients’ self-triage for unscheduled urgent care: A preliminary study on the accuracy and factors affecting the performance of a Belgian self-triage platform. BMC Health Serv. Res. 2022, 22, 1199. [Google Scholar] [CrossRef]
| Author, Year, and Country | Study Design | Device | Photography or Video | Number of Patients Included in the Study | Summary of Methods | Outcomes |
|---|---|---|---|---|---|---|
| Buntic R.F. et al. [22], 1997, USA | Case report | Digital camera | Photography | 1 patient | A photography of the injury and its radiography were emailed to consultant physicians | Successful reimplantation of the mutilated thumb |
| Hsieh C.H. et al. [23], 2004, Taiwan | Observational descriptive | Cell phone camera | Photography | 45 patients (81 digits) | A photograph of the injury and a short trauma history were sent to the consultant surgeon, who triaged the patients into three groups. The patients were also triaged by three junior plastic surgery residents at a later time | 15% of the cases resulted in treatment disagreement between final treatment and teleconsultation. A total of 20% of cases resulted in triaging disagreement. Remote diagnosis had a sensitivity of 79% and specificity of 71%, while remote recognition of bone exposure had a sensitivity of 76% and a specificity of 75% |
| Lam T.K. et al. [24], 2004, Australia | Observational descriptive | Cell phone camera | Photography | 27 patients | Photos of the lesion(s) were taken by the resident in the ED and cases were discussed with the consultant surgeon, who established treatment before seeing the pictures | Treatment changed after photo inspection in four cases |
| Hsieh C.H. et al. [25], 2005, Taiwan | Observational descriptive | Cell phone camera | Photography | 35 patients (60 digits) | A photography of the amputated portion and stump were sent to the consultant surgeon along with patient information and its radiograph. The images were evaluated by three other remote plastic surgeons. | The three remote surgeons correctly identified amputation location and status in 90% and 87% of cases, respectively, identified distal skin ecchymosis along the digital artery with 79% sensitivity and 90% specificity, and identified digital replantation potential with 90% sensitivity and 83% specificity |
| Diver A.J. et al. [26], 2008, United Kingdom | Observational descriptive | Digital camera | Photography | 20 patients (17 with hand injuries) | A surgery resident assessed the patient and took pictures of the lesion, which were then taken to the attending surgeon along with the patient history to provide a preliminary management decision. After this, the attending surgeon examined the patients in person and final management was prescribed | High (95%) agreement by the attending surgeon with photography and description and high (95%) agreement between preliminary and final treatment. Five of the twenty patients (25%) could have been managed without attending the ED |
| Althubahati G. et al. [27], 2011, USA | Case series | Cell phone camera | Video | 4 patients (1 patient with hand injury) | Consultations of patients with a requested urgent transfer were supplemented with videos of specific points in physical examination taken by the hand surgery fellow. Based on the described clinical picture and the video, the hand surgeon decided whether to accept or decline the transfer | Out of the four included cases that required transfer based on initial diagnosis, only one (25%) was considered for transfer after video evaluation by the attending surgeon |
| Waterman B.R. et al. [28], 2014, USA | Observational descriptive | Not specified | Photography | 597 consults (197 hand injuries) | Using the AKO e-mail system, the on-site clinical team showed photos and a description of the case to an orthopedic surgeon, who decided on whether to evacuate the patient for tertiary care or treat him or her on-site | Teleconsultation prevented medical evacuation of 11 hand injury cases (out of 30 cases for which evacuation was initially requested) |
| Hara T. et al. [29], 2015, Japan | Observational descriptive | Cell phone camera | Photography | 474 patients | The EMTs took photos of the injured fingers (following the hand surgeon’s instructions), which were sent to the investigators to assess the necessity for specialized treatment and redirect the ambulance to the most appropriate hospital | Acceptance to a hospital after three or fewer requests significantly increased (p = 0.039) after implementation of the Interactive Teletriage (from 79.2% to 86.4%) |
| Dehours E. et al. [30], 2016, France | Case series | Not specified | Photography | 5 patients (1 finger injury) | A photo of an injured finger was taken by a civilian with limited training to the French Tele-Medical Assistance Service, who declined patient evacuation and advised for on-site treatment of the wound | Out of the five cases, there was only one evacuation |
| Paik A.M. et al. [31], 2017, USA | Observational descriptive | Tablet | Photography | 42 patients (31 patients had hand injuries) | Patients with acute hand and facial wounds took pictures of their lesions, which were shown to a PSE, who then provided educational materials for the ED physician to make treatment and triage decisions. At the same time, patients were triaged, and a surgeon was consulted on-site, answering in person or by phone | Agreement rate between consultant and PSE was 90.5%. The mean response time for consultants was 48.3 min, while for PSE, it was 8.9 min, showing a statistically significant time reduction (p < 0.001) |
| Tripod M. et al. [32], 2018, USA | Cross-sectional | Tablet | Video and/or photography | 202 patients (with isolated hand injuries) | The UAMS institutional trauma registry was queried for isolated hand injuries for the 2012–2015 period and subsequently divided into pre-AHTTP and post-AHTTP for transfer and costs assessments | In the pre-AHTTP group, 47.8% of patients were discharged home, while 52.2% were admitted or underwent surgery. In the post-AHTTP group, 31.8% patients were discharged home, while 68.2% were admitted or underwent surgery, resulting in a significant difference (p = 0.02). The direct cost of transportation for patients was also significantly lower in the post-AHTTP group (38.5% pre- vs. 21.4% post-, p < 0.0001) |
| Bracey J.W. et al. [33], 2019, USA | Cross-sectional | Tablet | Video and/or photography | 331 patients, of which 298 had a telemedicine consultation (65% of these had videoconsultation) | The authors reviewed data on hand trauma from the first year of the AHTTP (2014) and compared it to the year prior (2013). Data collection focused on number of hand consultations, need for transfer, and time to disposition | After implementation of the AHTTP, transfers decreased from 73% in de pre-system period to 45% (p < 0.001). Time to disposition increased by 31 min on average (p < 0.001) |
| Westley S., Mistry R., and Dheansa B. [34], 2021, United Kingdom | Cross-sectional | Phone | Video or telephone using supporting photographs | 126 patients evaluated in the virtual clinic; 99 patients evaluated in the face-to-face clinic | Trainees were asked to predict what treatment was required for patients in face-to-face visits (prior to COVID-19 lockdown) or virtual clinic | 87% of patients evaluated virtually had an accurate assessment and all injured structures were correctly predicted, no patient had an unnecessary procedure—No significant difference in accuracy between video or telephone assessments (p = 0.88); 78% of patients in the face-to-face clinic had an accurate assessment, with no unnecessary procedures; no significant difference in overall accuracy between both clinics (p = 0.27) |
| Bracey J. et al. [35], 2021, USA | Cross-sectional | Tablet | Video and/or photography | 331 patients, of which 298 had a telemedicine consultation (65% of these had videoconsultation) | The authors reviewed data on hand trauma from January 1 to December 31, 2014 (first year of the program). Data focused on type of telemedicine consultation, need for transfer, and type of transfer recommended (general orthopedic vs. hand surgeon) | Out of 298 telemedicine consultations, 195 (65%) used video and 103 (35%) used phone only (both groups had access to imaging studies); of the patients using video, 91 (47%) were transferred and 60 (58%) were managed locally; of the patients using phone only, 43 (42%) were transferred and 60 (58%) were managed locally; using video did not significantly affect the decision to transfer (p = 0.42) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Avila, F.R.; Carter, R.E.; McLeod, C.J.; Bruce, C.J.; Guliyeva, G.; Torres-Guzman, R.A.; Maita, K.C.; Ho, O.A.; TerKonda, S.P.; Forte, A.J. The Role of Telemedicine in Prehospital Traumatic Hand Injury Evaluation. Diagnostics 2023, 13, 1165. https://doi.org/10.3390/diagnostics13061165
Avila FR, Carter RE, McLeod CJ, Bruce CJ, Guliyeva G, Torres-Guzman RA, Maita KC, Ho OA, TerKonda SP, Forte AJ. The Role of Telemedicine in Prehospital Traumatic Hand Injury Evaluation. Diagnostics. 2023; 13(6):1165. https://doi.org/10.3390/diagnostics13061165
Chicago/Turabian StyleAvila, Francisco R., Rickey E. Carter, Christopher J. McLeod, Charles J. Bruce, Gunel Guliyeva, Ricardo A. Torres-Guzman, Karla C. Maita, Olivia A. Ho, Sarvam P. TerKonda, and Antonio J. Forte. 2023. "The Role of Telemedicine in Prehospital Traumatic Hand Injury Evaluation" Diagnostics 13, no. 6: 1165. https://doi.org/10.3390/diagnostics13061165
APA StyleAvila, F. R., Carter, R. E., McLeod, C. J., Bruce, C. J., Guliyeva, G., Torres-Guzman, R. A., Maita, K. C., Ho, O. A., TerKonda, S. P., & Forte, A. J. (2023). The Role of Telemedicine in Prehospital Traumatic Hand Injury Evaluation. Diagnostics, 13(6), 1165. https://doi.org/10.3390/diagnostics13061165






