The Diagnostic and Prognostic Role of Biomarkers in Chronic Rhinosinusitis
Abstract
1. Introduction to Chronic Rhinosinusitis (CRS)
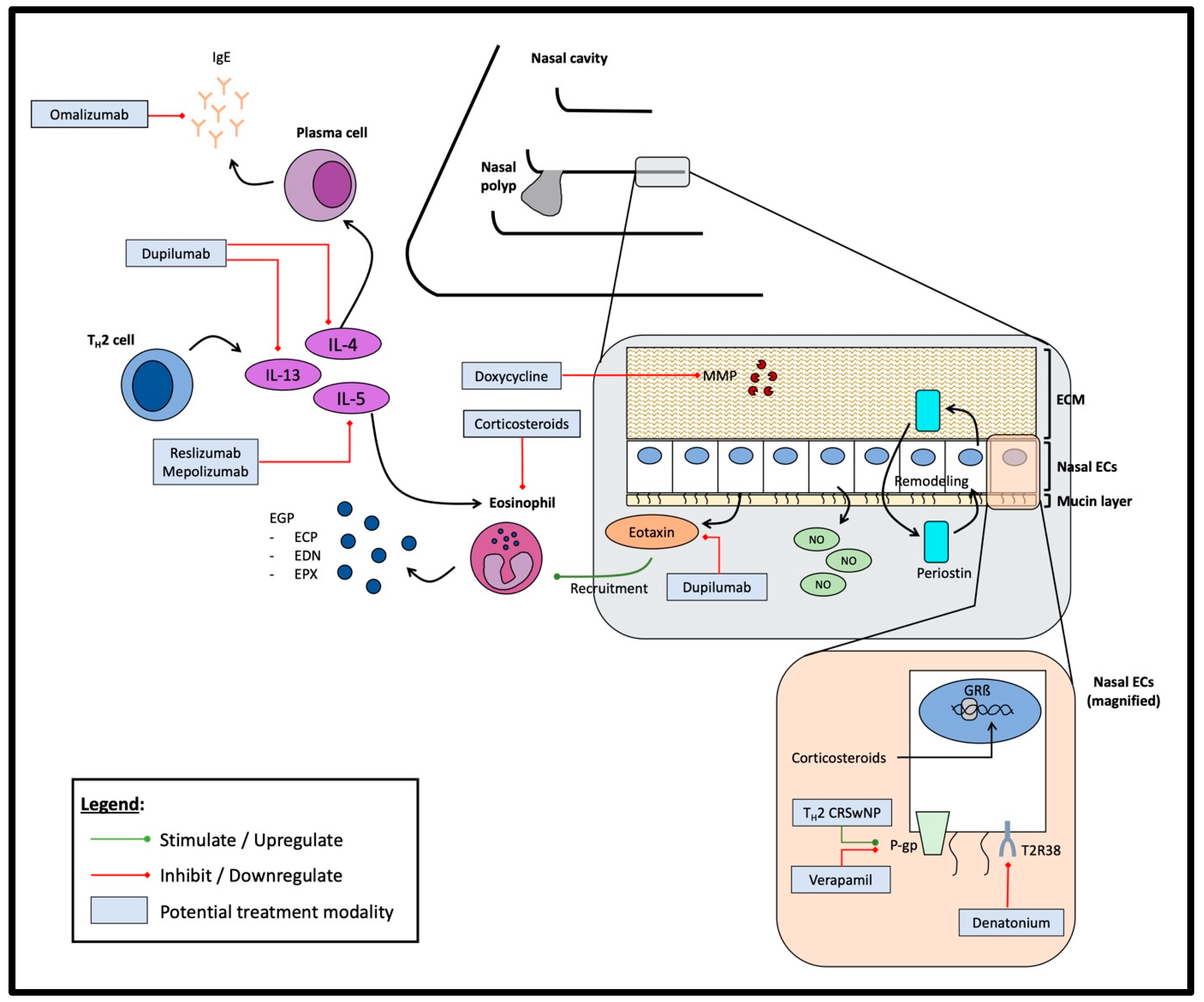
2. Biomarkers in CRS
3. Potential Biomarkers in the Diagnosis and Prognosis of CRS
3.1. Eosinophil Count
3.2. Immunoglobulin E (IgE)
3.2.1. Serum IgE
3.2.2. Tissue IgE
3.2.3. Nasal Secretions IgE
3.3. Eosinophil Granule Proteins
3.3.1. Eosinophilic Cationic Protein (ECP)
3.3.2. Eosinophil-Derived Neurotoxin (EDN)
3.3.3. Eosinophil Peroxidase (EPX)
3.4. Periostin
3.5. Interleukins
3.5.1. Type 2 Interleukins (IL-4, IL-5, IL-13)
3.5.2. Other Interleukins
3.6. Eotaxin-3
3.7. Nasal Nitric Oxide
3.8. Matrix Metalloproteinases (MMPs)
3.9. P-glycoprotein
3.10. Glucocorticoid Receptor β (GRβ)
3.11. Mucins
3.12. Taste Receptors
4. Future Needs
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I.; et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 2020, 58 (Suppl. S29), 1–464. [Google Scholar] [CrossRef]
- Rudmik, L. Economics of chronic rhinosinusitis. Curr. Allergy Asthma Rep. 2017, 17, 20. [Google Scholar] [CrossRef]
- Kato, A.; Peters, A.T.; Stevens, W.W.; Schleimer, R.P.; Tan, B.K.; Kern, R.C. Endotypes of chronic rhinosinusitis: Relationships to disease phenotypes, pathogenesis, clinical findings, and treatment approaches. Allergy 2022, 77, 812–826. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Van Zele, T.; Perez-Novo, C.; Van Bruaene, N.; Holtappels, G.; DeRuyck, N.; Van Cauwenberge, P.; Bachert, C. Different types of T-effector cells orchestrate mucosal inflammation in chronic sinus disease. J. Allergy Clin. Immunol. 2008, 122, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Rothenberg, M.E.; Hogan, S.P. The eosinophil. Annu. Rev. Immunol. 2006, 24, 147–174. [Google Scholar] [CrossRef]
- Zhu, J. T helper 2 (Th2) cell differentiation, type 2 innate lymphoid cell (ILC2) development and regulation of interleukin-4 (IL-4) and IL-13 production. Cytokine 2015, 75, 14–24. [Google Scholar] [CrossRef]
- Anyfantakis, D. A Young Male With Anorexia, Abdominal Complaints and Marked Blood Eosinophilia. Cureus 2020, 12, e12314. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, S.H.; Lim, J.Y.; Kim, D.; Jeong, I.S.; Lee, D.K.; Jang, Y.J. Association between the sinus microbiota with eosinophilic inflammation and prognosis in chronic rhinosinusitis with nasal polyps. Exp. Mol. Med. 2020, 52, 978–987. [Google Scholar] [CrossRef] [PubMed]
- Cao, P.P.; Li, H.B.; Wang, B.F.; Wang, S.B.; You, X.J.; Cui, Y.H.; Wang, D.Y.; Desrosiers, M.; Liu, Z. Distinct immunopathologic characteristics of various types of chronic rhinosinusitis in adult Chinese. J. Allergy Clin. Immunol. 2009, 124, 478–484. [Google Scholar] [CrossRef]
- Kim, J.W.; Hong, S.L.; Kim, Y.K.; Lee, C.H.; Min, Y.G.; Rhee, C.S. Histological and immunological features of non-eosinophilic nasal polyps. Otolaryngol.–Head Neck Surg. 2007, 137, 925–930. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, Y.; Ishitoya, J.; Komatsu, M.; Shiono, O.; Hirama, M.; Yamashita, Y.; Kaneko, T.; Morita, S.; Tsukuda, M. New clinical diagnostic criteria for eosinophilic chronic rhinosinusitis. Auris Nasus Larynx 2011, 38, 583–588. [Google Scholar] [CrossRef]
- Zuo, K.; Guo, J.; Chen, F.; Xu, R.; Xu, G.; Shi, J.; Li, H. Clinical characteristics and surrogate markers of eosinophilic chronic rhinosinusitis in Southern China. Eur. Arch. Oto-Rhino-Laryngol. 2014, 271, 2461–2468. [Google Scholar] [CrossRef] [PubMed]
- Roufosse, F.; Weller, P.F. Practical approach to the patient with hypereosinophilia. J. Allergy Clin. Immunol. 2010, 126, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Cao, P.P.; Liang, G.T.; Cui, Y.H.; Liu, Z. Diagnostic significance of blood eosinophil count in eosinophilic chronic rhinosinusitis with nasal polyps in Chinese adults. Laryngoscope 2012, 122, 498–503. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.; Li, W.; Grayson, J.W.; Alvarado, R.; Rimmer, J.; Sewell, W.A.; Harvey, R.J. Systemic medication requirement in post-surgical patients with eosinophilic chronic rhinosinusitis. Rhinology 2021, 59, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Honma, A.; Takagi, D.; Nakamaru, Y.; Homma, A.; Suzuki, M.; Fukuda, S. Reduction of blood eosinophil counts in eosinophilic chronic rhinosinusitis after surgery. J. Laryngol. Otol. 2016, 130, 1147–1152. [Google Scholar] [CrossRef]
- Snidvongs, K.; Lam, M.; Sacks, R.; Earls, P.; Kalish, L.; Phillips, P.S.; Pratt, E.; Harvey, R.J. Structured histopathology profiling of chronic rhinosinusitis in routine practice. Int. Forum Allergy Rhinology. 2012, 2, 376–385. [Google Scholar] [CrossRef]
- Wen, W.; Liu, W.; Zhang, L.; Bai, J.; Fan, Y.; Xia, W.; Luo, Q.; Zheng, J.; Wang, H.; Li, Z.; et al. Increased neutrophilia in nasal polyps reduces the response to oral corticosteroid therapy. J. Allergy Clin. Immunol. 2012, 129, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Ishitoya, J.; Sakuma, Y.; Tsukuda, M. Eosinophilic chronic rhinosinusitis in Japan. Allergol. Int. 2010, 59, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Zhang, L.; Gevaert, P. Current and future treatment options for adult chronic rhinosinusitis: Focus on nasal polyposis. J. Allergy Clin. Immunol. 2015, 136, 1431–1440. [Google Scholar] [CrossRef] [PubMed]
- Hulse, K.E.; Stevens, W.W.; Tan, B.K.; Schleimer, R.P. Pathogenesis of nasal polyposis. Clin. Exp. Allergy 2015, 45, 328–346. [Google Scholar] [CrossRef]
- Kountakis, S.E.; Arango, P.; Bradley, D.; Wade, Z.K.; Borish, L. Molecular and cellular staging for the severity of chronic rhinosinusitis. Laryngoscope 2004, 114, 1895–1905. [Google Scholar] [CrossRef]
- Soler, Z.M.; Sauer, D.; Mace, J.; Smith, T.L. Impact of mucosal eosinophilia and nasal polyposis on quality-of-life outcomes after sinus surgery. Otolaryngol.-Head Neck Surg. 2010, 142, 64–71. [Google Scholar] [CrossRef]
- Lou, H.; Meng, Y.; Piao, Y.; Wang, C.; Zhang, L.; Bachert, C. Predictive significance of tissue eosinophilia for nasal polyp recurrence in the Chinese population. Am. J. Rhinol. Allergy 2015, 29, 350–356. [Google Scholar] [CrossRef]
- Tokunaga, T.; Sakashita, M.; Haruna, T.; Asaka, D.; Takeno, S.; Ikeda, H.; Nakayama, T.; Seki, N.; Ito, S.; Murata, J.; et al. Novel scoring system and algorithm for classifying chronic rhinosinusitis: The JESREC Study. Allergy 2015, 70, 995–1003. [Google Scholar] [CrossRef]
- McHugh, T.; Snidvongs, K.; Xie, M.; Banglawala, S.; Sommer, D. High tissue eosinophilia as a marker to predict recurrence for eosinophilic chronic rhinosinusitis: A systematic review and meta-analysis. Int. Forum Allergy Rhinol. 2018, 8, 1421–1429. [Google Scholar] [CrossRef]
- Wei, B.; Liu, F.; Zhang, J.; Liu, Y.; Du, J.; Liu, S.; Zhang, N.; Bachert, C.; Meng, J. Multivariate analysis of inflammatory endotypes in recurrent nasal polyposis in a Chinese population. Rhinology 2018, 56, 216–226. [Google Scholar] [CrossRef]
- Ho, J.; Hamizan, A.W.; Alvarado, R.; Rimmer, J.; Sewell, W.A.; Harvey, R.J. Systemic predictors of eosinophilic chronic rhinosinusitis. Am. J. Rhinol. Allergy 2018, 32, 252–257. [Google Scholar] [CrossRef]
- Mori, E.; Matsuwaki, Y.; Mitsuyama, C.; Okushi, T.; Nakajima, T.; Moriyama, H. Risk factors for olfactory dysfunction in chronic rhinosinusitis. Auris Nasus Larynx 2013, 40, 465–469. [Google Scholar] [CrossRef]
- Gevaert, P.; Calus, L.; Van Zele, T.; Blomme, K.; De Ruyck, N.; Bauters, W.; Hellings, P.; Brusselle, G.; De Bacquer, D.; Van Cauwenberge, P.; et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. J. Allergy Clin. Immunol. 2013, 131, 110–116. [Google Scholar] [CrossRef]
- Baba, S.; Kondo, K.; Toma-Hirano, M.; Kanaya, K.; Suzukawa, K.; Ushio, M.; Suzukawa, M.; Ohta, K.; Yamasoba, T. Local increase in IgE and class switch recombination to IgE in nasal polyps in chronic rhinosinusitis. Clin. Exp. Allergy 2014, 44, 701–712. [Google Scholar] [CrossRef]
- Gevaert, P.; Calus, L.; van Bruaene, N.; Van Zele, T.; Bachert, C. Allergic sensitization, high local IL-5 and IgE predict surgical outcome 12 years after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. J. Allergy Clin. Immunol. 2015, 135, AB238. [Google Scholar] [CrossRef]
- De Schryver, E.; Devuyst, L.; Derycke, L.; Dullaers, M.; Van Zele, T.; Bachert, C.; Gevaert, P. Local immunoglobulin E in the nasal mucosa: Clinical implications. Allergy Asthma Immunol. Res. 2015, 7, 321–331. [Google Scholar] [CrossRef]
- Bachert, C.; Gevaert, P.; Holtappels, G.; Johansson, S.G.; Van Cauwenberge, P. Total and specific IgE in nasal polyps is related to local eosinophilic inflammation. J. Allergy Clin. Immunol. 2001, 107, 607–614. [Google Scholar] [CrossRef]
- Bachert, C.; Zhang, N.; Holtappels, G.; De Lobel, L.; Van Cauwenberge, P.; Liu, S.; Lin, P.; Bousquet, J.; Van Steen, K. Presence of IL-5 protein and IgE antibodies to staphylococcal enterotoxins in nasal polyps is associated with comorbid asthma. J. Allergy Clin. Immunol. 2010, 126, 962–968. [Google Scholar] [CrossRef]
- Liu, J.K. The history of monoclonal antibody development—Progress, remaining challenges and future innovations. Ann. Med. Surg. 2014, 3, 113–116. [Google Scholar] [CrossRef]
- Samaranayake, H.; Wirth, T.; Schenkwein, D.; Räty, J.K.; Ylä-Herttuala, S. Challenges in monoclonal antibody-based therapies. Ann. Med. 2009, 41, 322–331. [Google Scholar] [CrossRef]
- Riechelmann, H.; Deutschle, T.; Rozsasi, A.; Keck, T.; Polzehl, D.; Bürner, H. Nasal biomarker profiles in acute and chronic rhinosinusitis. Clin. Exp. Allergy 2005, 35, 1186–1191. [Google Scholar] [CrossRef]
- Bachert, C.; Cho, S.; Laidlaw, T.; Swanson, B.; Harel, S.; Mannent, L.; Amin, N.; Jagerschmidt, A. Dupilumab reduces blood, urine, and nasal biomarkers of type 2 inflammation in patients with chronic rhinosinusitis with nasal polyps in the phase 3 SINUS-52 trial. J. Allergy Clin. Immunol. 2020, 145, AB185. [Google Scholar] [CrossRef]
- Venge, P.; Byström, J. Molecules in focus eosinophil cationic protein (ECP). Int. J. Biochem. Cell Biol. 1998, 30, 433–437. [Google Scholar] [CrossRef]
- Koh, G.C.; Shek, L.P.; Goh, D.Y.; Van Bever, H.; Koh, D.S. Eosinophil cationic protein: Is it useful in asthma? A systematic review. Respir. Med. 2007, 101, 696–705. [Google Scholar] [CrossRef] [PubMed]
- Czech, W.; Krutmann, J.; Schöpf, E.; Kapp, A. Serum eosinophil cationic protein (ECP) is a sensitive measure for disease activity in atopic dermatitis. Br. J. Dermatol. 1992, 126, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Rich, R.R.; Fleisher, T.A.; Shearer, W.T.; Schroeder, H.W., Jr.; Frew, A.J.; Weyand, C.M. Clinical Immunology E-Book: Principles and Practice; Elsevier Health Sciences: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Van Zele, T.; Claeys, S.; Gevaert, P.; Van Maele, G.E.; Holtappels, G.; Van Cauwenberge, P.; Bachert, C. Differentiation of chronic sinus diseases by measurement of inflammatory mediators. Allergy 2006, 61, 1280–1289. [Google Scholar] [CrossRef]
- Tsuda, T.; Maeda, Y.; Nishide, M.; Koyama, S.; Hayama, Y.; Nojima, S.; Takamatsu, H.; Okuzaki, D.; Kinehara, Y.; Kato, Y.; et al. Eosinophil-derived neurotoxin enhances airway remodeling in eosinophilic chronic rhinosinusitis and correlates with disease severity. Int. Immunol. 2019, 31, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.S.; Won, H.R.; Park, C.Y.; Hong, J.H.; Lee, J.H.; Lee, K.E.; Cho, H.S.; Kim, H.J. Analyzing serum eosinophil cationic protein in the clinical assessment of chronic rhinosinusitis. Am. J. Rhinol. Allergy 2013, 27, e75–e80. [Google Scholar] [CrossRef] [PubMed]
- Hamidova, D.; Smolnikova, E.; Mokronosova, M. Eosinophil cationic protein in nasal secretion, serum and polyps tissue in patients with chronic rhinosinusitis. Allergy 2011, 66, 245. [Google Scholar]
- Lee, Y.; Lee, J.H.; Yang, E.M.; Kwon, E.; Jung, C.G.; Kim, S.C.; Choi, Y.; Cho, Y.S.; Kim, C.K.; Park, H.S. Serum levels of eosinophil-derived neurotoxin: A biomarker for asthma severity in adult asthmatics. Allergy Asthma Immunol. Res. 2019, 11, 394–405. [Google Scholar] [CrossRef]
- Lee, J.J.; Rosenberg, H.F. (Eds.) Eosinophils in Health and Disease; Academic Press: Cambridge, MA, USA, 2012. [Google Scholar]
- Barnes, P.J. Reactive oxygen species and airway inflammation. Free. Radic. Biol. Med. 1990, 9, 235–243. [Google Scholar] [CrossRef]
- Wang, Z.; DiDonato, J.A.; Buffa, J.; Comhair, S.A.; Aronica, M.A.; Dweik, R.A.; Lee, N.A.; Lee, J.J.; Thomassen, M.J.; Kavuru, M.; et al. Eosinophil peroxidase catalyzed protein carbamylation participates in asthma. J. Biol. Chem. 2016, 291, 22118–22135. [Google Scholar] [CrossRef]
- Lal, D.; Wright, B.L.; Shim, K.P.; Zarka, M.A.; Lee, J.J.; Chang, Y.H.; Ochkur, S.; Divekar, R.; Doyle, A.; Jacobsen, E.; et al. Eosinophil peroxidase, GATA3, and T-bet as tissue biomarkers in chronic rhinosinusitis. J. Allergy Clin. Immunol. 2019, 143, 2284–2287. [Google Scholar] [CrossRef]
- Workman, A.D.; Kohanski, M.A.; Cohen, N.A. Biomarkers in chronic rhinosinusitis with nasal polyps. Immunol. Allergy Clin. 2018, 38, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Xie, S.; Yang, C.; Zhang, J.; Wu, X.; Sun, H. Biomarkers in the evaluation and management of chronic rhinosinusitis with nasal polyposis. Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 3559–3566. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wang, X.; Zhang, N.; Wang, H.; Li, Y.; Fan, E.; Zhang, L.; Zhang, L.; Bachert, C. Association of periostin expression with eosinophilic inflammation in nasal polyps. J. Allergy Clin. Immunol. 2015, 136, 1700–1703. [Google Scholar] [CrossRef] [PubMed]
- Jonstam, K.; Westman, M.; Holtappels, G.; Holweg, C.T.; Bachert, C. Serum periostin, IgE, and SE-IgE can be used as biomarkers to identify moderate to severe chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2017, 140, 1705–1708. [Google Scholar] [CrossRef] [PubMed]
- Ohta, N.; Ishida, A.; Kurakami, K.; Suzuki, Y.; Kakehata, S.; Ono, J.; Ikeda, H.; Okubo, K.; Izuhara, K. Expressions and roles of periostin in otolaryngological diseases. Allergol. Int. 2014, 63, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Zhang, W.; Chen, D.; Zhou, H.; Chen, L. Diagnostic significance of serum periostin in eosinophilic chronic sinusitis with nasal polyps. Acta Oto-Laryngol. 2018, 138, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Ninomiya, T.; Noguchi, E.; Haruna, T.; Hasegawa, M.; Yoshida, T.; Yamashita, Y.; Okano, M.; Yoshida, N.; Haruna, S.; Sakuma, Y.; et al. Periostin as a novel biomarker for postoperative recurrence of chronic rhinosinitis with nasal polyps. Sci. Rep. 2018, 8, 11450. [Google Scholar] [CrossRef]
- Zhang, W.; Hubin, G.; Endam, L.M.; Al-Mot, S.; Filali-Mouhim, A.; Desrosiers, M. Expression of the extracellular matrix gene periostin is increased in chronic rhinosinusitis and decreases following successful endoscopic sinus surgery. Int. Forum Allergy Rhinol. 2012, 2, 471–476. [Google Scholar] [CrossRef]
- Kim, D.W.; Kulka, M.; Jo, A.; Eun, K.M.; Arizmendi, N.; Tancowny, B.P.; Hong, S.N.; Lee, J.P.; Jin, H.R.; Lockey, R.F.; et al. Cross-talk between human mast cells and epithelial cells by IgE-mediated periostin production in eosinophilic nasal polyps. J. Allergy Clin. Immunol. 2017, 139, 1692–1695. [Google Scholar] [CrossRef]
- Tomaru, A.; Kobayashi, T.; Hinneh, J.A.; Baffour Tonto, P.; D’Alessandro-Gabazza, C.N.; Fujimoto, H.; Fujiwara, K.; Takahashi, Y.; Ohnishi, M.; Yasuma, T.; et al. Oligonucleotide-targeting periostin ameliorates pulmonary fibrosis. Gene Ther. 2017, 24, 706–716. [Google Scholar] [CrossRef]
- Takeno, S.; Taruya, T.; Ueda, T.; Noda, N.; Hirakawa, K. Increased exhaled nitric oxide and its oxidation metabolism in eosinophilic chronic rhinosinusitis. Auris Nasus Larynx 2013, 40, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Kubota, K.; Takeno, S.; Taruya, T.; Sasaki, A.; Ishino, T.; Hirakawa, K. IL-5 and IL-6 are increased in the frontal recess of eosinophilic chronic rhinosinusitis patients. J. Otolaryngol.-Head Neck Surg. 2017, 46, 36. [Google Scholar] [CrossRef] [PubMed]
- Tomassen, P.; Vandeplas, G.; Van Zele, T.; Cardell, L.O.; Arebro, J.; Olze, H.; Förster-Ruhrmann, U.; Kowalski, M.L.; Olszewska-Ziąber, A.; Holtappels, G.; et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J. Allergy Clin. Immunol. 2016, 137, 1449–1456. [Google Scholar] [CrossRef]
- Van Zele, T.; Holtappels, G.; Gevaert, P.; Bachert, C. Differences in initial immunoprofiles between recurrent and nonrecurrent chronic rhinosinusitis with nasal polyps. Am. J. Rhinol. Allergy 2014, 28, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Schlosser, R.J.; Mulligan, J.K.; Hyer, J.M.; Karnezis, T.T.; Gudis, D.A.; Soler, Z.M. Mucous cytokine levels in chronic rhinosinusitis-associated olfactory loss. JAMA Otolaryngol.–Head Neck Surg. 2016, 142, 731–737. [Google Scholar] [CrossRef] [PubMed]
- Gevaert, P.; Bachert, C.; Holtappels, G.; Novo, C.P.; Van Der Heyden, J.; Fransen, L.; Depraetere, S.; Walter, H.; Van Cauwenberge, P.; Tavernier, J. Enhanced soluble interleukin-5 receptor alpha expression in nasal polyposis. Allergy 2003, 58, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Hamilos, D.L.; Leung, D.Y.; Huston, D.P.; Kamil, A.; Wood, R.; Hamid, Q. GM-CSF, IL-5 and RANTES immunoreactivity and mRNA expression in chronic hyperplastic sinusitis with nasal polyposis (NP). Clin. Exp. Allergy 1998, 28, 1145–1152. [Google Scholar] [CrossRef]
- Gevaert, P.; Lang-Loidolt, D.; Lackner, A.; Stammberger, H.; Staudinger, H.; Van Zele, T.; Holtappels, G.; Tavernier, J.; Van Cauwenberge, P.; Bachert, C. Nasal IL-5 levels determine the response to anti–IL-5 treatment in patients with nasal polyps. J. Allergy Clin. Immunol. 2006, 118, 1133–1141. [Google Scholar] [CrossRef]
- Gevaert, P.; Van Bruaene, N.; Cattaert, T.; Van Steen, K.; Van Zele, T.; Acke, F.; De Ruyck, N.; Blomme, K.; Sousa, A.R.; Marshall, R.P.; et al. Mepolizumab, a humanized anti–IL-5 mAb, as a treatment option for severe nasal polyposis. J. Allergy Clin. Immunol. 2011, 128, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Sousa, A.R.; Lund, V.J.; Scadding, G.K.; Gevaert, P.; Nasser, S.; Durham, S.R.; Cornet, M.E.; Kariyawasam, H.H.; Gilbert, J.; et al. Reduced need for surgery in severe nasal polyposis with mepolizumab: Randomized trial. J. Allergy Clin. Immunol. 2017, 140, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Naclerio, R.M.; Baroody, F.M.; Pinto, J.M. Nasal polyps and biomarkers. J. Allergy Clin. Immunol. Pract. 2017, 5, 1589–1590. [Google Scholar] [CrossRef] [PubMed]
- Voehringer, D.; Reese, T.A.; Huang, X.; Shinkai, K.; Locksley, R.M. Type 2 immunity is controlled by IL-4/IL-13 expression in hematopoietic non-eosinophil cells of the innate immune system. J. Exp. Med. 2006, 203, 1435–1446. [Google Scholar] [CrossRef]
- Turner, J.H.; Li, P.; Chandra, R.K. Mucus T helper 2 biomarkers predict chronic rhinosinusitis disease severity and prior surgical intervention. Int. Forum Allergy Rhinol. 2018, 8, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Mannent, L.; Naclerio, R.M.; Mullol, J.; Ferguson, B.J.; Gevaert, P.; Hellings, P.; Jiao, L.; Wang, L.; Evans, R.R.; et al. Effect of subcutaneous dupilumab on nasal polyp burden in patients with chronic sinusitis and nasal polyposis: A randomized clinical trial. JAMA 2016, 315, 469–479. [Google Scholar] [CrossRef]
- Lackner, A.; Raggam, R.B.; Stammberger, H.; Beham, A.; Braun, H.; Kleinhappl, B.; Buzina, W.; Kittinger, C.; Reinisch, S.; Berghold, A.; et al. The role of interleukin-16 in eosinophilic chronic rhinosinusitis. Eur. Arch. Oto-Rhino-Laryngol. 2007, 264, 887–893. [Google Scholar] [CrossRef] [PubMed]
- Lam, M.; Hull, L.; Imrie, A.; Snidvongs, K.; Chin, D.; Pratt, E.; Kalish, L.; Sacks, R.; Earls, P.; Sewell, W.; et al. Interleukin-25 and interleukin-33 as mediators of eosinophilic inflammation in chronic rhinosinusitis. Am. J. Rhinol. Allergy 2015, 29, 175–181. [Google Scholar] [CrossRef]
- Lam, M.; Hull, L.; McLachlan, R.; Snidvongs, K.; Chin, D.; Pratt, E.; Kalish, L.; Sacks, R.; Earls, P.; Sewell, W.; et al. Clinical severity and epithelial endotypes in chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2013, 3, 121–128. [Google Scholar] [CrossRef]
- Chen, F.; Hong, H.; Sun, Y.; Hu, X.; Zhang, J.; Xu, G.; Zhao, W.; Li, H.; Shi, J. Nasal interleukin 25 as a novel biomarker for patients with chronic rhinosinusitis with nasal polyps and airway hypersensitiveness: A pilot study. Ann. Allergy Asthma Immunol. 2017, 119, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.W.; Kim, D.K.; Park, M.H.; Eun, K.M.; Lee, M.; So, D.; Kong, I.G.; Mo, J.H.; Yang, M.S.; Jin, H.R.; et al. IL-25 as a novel therapeutic target in nasal polyps of patients with chronic rhinosinusitis. J. Allergy Clin. Immunol. 2015, 135, 1476–1485. [Google Scholar] [CrossRef] [PubMed]
- Ozturan, A.; Eyigor, H.; Eyigor, M.; Osma, U.; Yilmaz, M.D.; Selcuk, O.T.; Renda, L.; Gultekin, M. The role of IL-25 and IL-33 in chronic rhinosinusitis with or without nasal polyps. Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 283–288. [Google Scholar] [CrossRef]
- Reh, D.D.; Wang, Y.; Ramanathan, M.; Lane, A.P. Treatment-recalcitrant chronic rhinosinusitis with polyps is associated with altered epithelial cell expression of interleukin-33. Am. J. Rhinol. Allergy 2010, 24, 105–109. [Google Scholar] [CrossRef]
- Kim, D.K.; Jin, H.R.; Eun, K.M.; Mo, J.H.; Cho, S.H.; Oh, S.; Cho, D.; Kim, D.W. The role of interleukin-33 in chronic rhinosinusitis. Thorax 2017, 72, 635–645. [Google Scholar] [CrossRef] [PubMed]
- Zarling, J.M.; Shoyab, M.; Marquardt, H.; Hanson, M.B.; Lioubin, M.N.; Todaro, G.J. Oncostatin M: A growth regulator produced by differentiated histiocytic lymphoma cells. Proc. Natl. Acad. Sci. USA 1986, 83, 9739–9743. [Google Scholar] [CrossRef]
- Pothoven, K.L.; Norton, J.E.; Hulse, K.E.; Suh, L.A.; Carter, R.G.; Rocci, E.; Harris, K.E.; Shintani-Smith, S.; Conley, D.B.; Chandra, R.K.; et al. Oncostatin M promotes mucosal epithelial barrier dysfunction, and its expression is increased in patients with eosinophilic mucosal disease. J. Allergy Clin. Immunol. 2015, 136, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.; Earls, P.; Harvey, R.J. Systemic biomarkers of eosinophilic chronic rhinosinusitis. Curr. Opin. Allergy Clin. Immunol. 2020, 20, 23–29. [Google Scholar] [CrossRef]
- Ikeda, K.; Shiozawa, A.; Ono, N.; Kusunoki, T.; Hirotsu, M.; Homma, H.; Saitoh, T.; Murata, J. Subclassification of chronic rhinosinusitis with nasal polyp based on eosinophil and neutrophil. Laryngoscope 2013, 123, E1–E9. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Miyabe, Y.; Ueki, S.; Fujieda, S.; Tokunaga, T.; Sakashita, M.; Kato, Y.; Ninomiya, T.; Kawasaki, Y.; Suzuki, S.; et al. Eotaxin-3 as a plasma biomarker for mucosal eosinophil infiltration in chronic rhinosinusitis. Front. Immunol. 2019, 10, 74. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Gao, X.; Zhu, Z.; Hu, X.; Zhou, H.; Liu, J. The roles of nasal nitric oxide in diagnosis and endotypes of chronic rhinosinusitis with nasal polyps. J. Otolaryngol.-Head Neck Surg. 2020, 49, 68. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Zheng, S.; Dweik, R.A.; Erzurum, S.C. Role of epithelial nitric oxide in airway viral infection. Free. Radic. Biol. Med. 2006, 41, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Delclaux, C.; Malinvaud, D.; Chevalier-Bidaud, B.; Callens, E.; Mahut, B.A.; Bonfils, P. Nitric oxide evaluation in upper and lower respiratory tracts in nasal polyposis. Clin. Exp. Allergy 2008, 38, 1140–1147. [Google Scholar] [CrossRef]
- Colantonio, D.; Brouillette, L.; Parikh, A.; Scadding, G.K. Paradoxical low nasal nitric oxide in nasal polyposis. Clin. Exp. Allergy 2002, 32, 698–701. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zheng, M.; He, F.; Wang, X.; Zhang, L. Role of exhaled nasal nitric oxide in distinguishing between chronic rhinosinusitis with and without nasal polyps. Am. J. Rhinol. Allergy 2017, 31, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Bommarito, L.; Guida, G.; Heffler, E.; Badiu, I.; Nebiolo, F.; Usai, A.; De Stefani, A.; Rolla, G. Nasal nitric oxide concentration in suspected chronic rhinosinusitis. Ann. Allergy Asthma Immunol. 2008, 101, 358–362. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.H.; Yoo, H.S.; Lee, S.H.; Kim, K.R.; Yoon, H.J.; Kim, S.H. Nasal and exhaled nitric oxide in chronic rhinosinusitis with polyps. Am. J. Rhinol. Allergy 2014, 28, e11–e16. [Google Scholar] [CrossRef]
- Lee, J.M.; McKnight, C.L.; Aves, T.; Yip, J.; Grewal, A.S.; Gupta, S. Nasal nitric oxide as a marker of sinus mucosal health in patients with nasal polyposis. Int. Forum Allergy Rhinol. 2015, 5, 894–899. [Google Scholar] [CrossRef] [PubMed]
- Vaidyanathan, S.; Williamson, P.; Anderson, K.; Lipworth, B. Effect of systemic steroids on humming nasal nitric oxide in chronic rhinosinusitis with nasal polyposis. Ann. Allergy Asthma Immunol. 2010, 105, 412–417. [Google Scholar] [CrossRef] [PubMed]
- Deroee, A.F.; Naraghi, M.; Sontou, A.F.; Ebrahimkhani, M.R.; Dehpour, A.R. Nitric oxide metabolites as biomarkers for follow-up after chronic rhinosinusitis surgery. Am. J. Rhinol. Allergy 2009, 23, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Visse, R.; Nagase, H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: Structure, function, and biochemistry. Circ. Res. 2003, 92, 827–839. [Google Scholar] [CrossRef]
- Li, X.; Meng, J.; Qiao, X.; Liu, Y.; Liu, F.; Zhang, N.; Zhang, J.; Holtappels, G.; Luo, B.; Zhou, P.; et al. Expression of TGF, matrix metalloproteinases, and tissue inhibitors in Chinese chronic rhinosinusitis. J. Allergy Clin. Immunol. 2010, 125, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- Malinsky, R.R.; Valera, F.C.; Cavallari, F.E.; Küpper, D.S.; Milaneze, C.; Silva, J.S.; Tamashiro, E.; Anselmo-Lima, W.T. Matrix metalloproteinases and their impact on sinusal extension in chronic rhinosinusitis with nasal polyps. Eur. Arch. Oto-Rhino-Laryngol. 2013, 270, 1345–1348. [Google Scholar] [CrossRef]
- Yeo, N.K.; Eom, D.W.; Oh, M.Y.; Lim, H.W.; Song, Y.J. Expression of matrix metalloproteinase 2 and 9 and tissue inhibitor of metalloproteinase 1 in nonrecurrent vs recurrent nasal polyps. Ann. Allergy Asthma Immunol. 2013, 111, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.F.; Chien, C.Y.; Chiang, F.Y.; Chai, C.Y.; Tai, C.F. Corelationship between matrix metalloproteinase 2 and 9 expression and severity of chronic rhinosinusitis with nasal polyposis. Am. J. Rhinol. Allergy 2012, 26, e1–e4. [Google Scholar] [CrossRef]
- Watelet, J.B.; Claeys, C.; Cauwenberge, P.V.; Bachert, C. Predictive and monitoring value of matrix metalloproteinase-9 for healing quality after sinus surgery. Wound Repair Regen. 2004, 12, 412–418. [Google Scholar] [CrossRef]
- Watelet, J.B.; Demetter, P.; Claeys, C.; Van Cauwenberge, P.; Cuvelier, C.; Bachert, C. Neutrophil-derived metalloproteinase-9 predicts healing quality after sinus surgery. Laryngoscope 2005, 115, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Van Zele, T.; Gevaert, P.; Holtappels, G.; Beule, A.; Wormald, P.J.; Mayr, S.; Hens, G.; Hellings, P.; Ebbens, F.A.; Fokkens, W.; et al. Oral steroids and doxycycline: Two different approaches to treat nasal polyps. J. Allergy Clin. Immunol. 2010, 125, 1069–1076. [Google Scholar] [CrossRef]
- Huvenne, W.; Zhang, N.; Tijsma, E.; Hissong, B.; Huurdeman, J.; Holtappels, G.; Claeys, S.; Van Cauwenberge, P.; Nelis, H.; Coenye, T.; et al. Pilot study using doxycycline-releasing stents to ameliorate postoperative healing quality after sinus surgery. Wound Repair Regen. 2008, 16, 757–767. [Google Scholar] [CrossRef]
- Pinto Bezerra Soter, A.C.; Bezerra, T.F.; Pezato, R.; Teles Abdo, T.R.; Pilan, R.M.; Pinna, F.D.; Gevaert, P.; Van Zele, T.; Bachert, C.; Voegels, R.L. Prospective open-label evaluation of long-term low-dose doxycycline for difficult-to-treat chronic rhinosinusitis with nasal polyps. Rhinology 2017, 55, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Bleier, B.S. Regional expression of epithelial MDR1/P-glycoprotein in chronic rhinosinusitis with and without nasal polyposis. Int. Forum Allergy Rhinol. 2012, 2, 122–125. [Google Scholar] [CrossRef]
- Feldman, R.E.; Lam, A.C.; Sadow, P.M.; Bleier, B.S. P-glycoprotein is a marker of tissue eosinophilia and radiographic inflammation in chronic rhinosinusitis without nasal polyps. Int. Forum Allergy Rhinol. 2013, 3, 684–687. [Google Scholar] [CrossRef] [PubMed]
- Nocera, A.L.; Meurer, A.T.; Miyake, M.M.; Sadow, P.M.; Han, X.; Bleier, B.S. Secreted P-glycoprotein is a noninvasive biomarker of chronic rhinosinusitis. Laryngoscope 2017, 127, E1–E4. [Google Scholar] [CrossRef]
- Miyake, M.M.; Nocera, A.; Levesque, P.; Guo, R.; Finn, C.A.; Goldfarb, J.; Gray, S.; Holbrook, E.; Busaba, N.; Dolci, J.E.; et al. Double-blind placebo-controlled randomized clinical trial of verapamil for chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2017, 140, 271–273. [Google Scholar] [CrossRef]
- Pujols, L.; Mullol, J.; Picado, C. Importance of glucocorticoid receptors in upper and lower airways. Front. Biosci.-Landmark 2010, 15, 789–800. [Google Scholar] [CrossRef] [PubMed]
- Hamilos, D.L.; Leung, D.Y.; Muro, S.; Kahn, A.M.; Hamilos, S.S.; Thawley, S.E.; Hamid, Q.A. GRβ expression in nasal polyp inflammatory cells and its relationship to the anti-inflammatory effects of intranasal fluticasone. J. Allergy Clin. Immunol. 2001, 108, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Valera, F.C.; Queiroz, R.; Scrideli, C.; Tone, L.G.; Anselmo-Lima, W.T. Evaluating budesonide efficacy in nasal polyposis and predicting the resistance to treatment. Clin. Exp. Allergy 2009, 39, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Diaz, L.K.; Wiley, E.L.; Morrow, M. Expression of epithelial mucins Muc1, Muc2, and Muc3 in ductal carcinoma in situ of the breast. Breast J. 2001, 7, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Wesseling, J.; van der Valk, S.W.; Hilkens, J. A mechanism for inhibition of E-cadherin-mediated cell-cell adhesion by the membrane-associated mucin episialin/MUC1. Mol. Biol. Cell 1996, 7, 565–577. [Google Scholar] [CrossRef]
- Milara, J.; Peiró, T.; Armengot, M.; Frias, S.; Morell, A.; Serrano, A.; Cortijo, J. Mucin 1 downregulation associates with corticosteroid resistance in chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2015, 135, 470–476. [Google Scholar] [CrossRef]
- Milara, J.; Morell, A.; Ballester, B.; Armengot, M.; Morcillo, E.; Cortijo, J. MUC4 impairs the anti-inflammatory effects of corticosteroids in patients with chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 2017, 139, 855–862. [Google Scholar] [CrossRef]
- Adappa, N.D.; Zhang, Z.; Palmer, J.N.; Kennedy, D.W.; Doghramji, L.; Lysenko, A.; Reed, D.R.; Scott, T.; Zhao, N.W.; Owens, D.; et al. The bitter taste receptor T2R38 is an independent risk factor for chronic rhinosinusitis requiring sinus surgery. Int. Forum Allergy Rhinol. 2014, 4, 3–7. [Google Scholar] [CrossRef]
- Adappa, N.D.; Truesdale, C.M.; Workman, A.D.; Doghramji, L.; Mansfield, C.; Kennedy, D.W.; Palmer, J.N.; Cowart, B.J.; Cohen, N.A. Correlation of T2R38 taste phenotype and in vitro biofilm formation from nonpolypoid chronic rhinosinusitis patients. Int. Forum Allergy Rhinol. 2016, 6, 783–791. [Google Scholar] [CrossRef]
- Workman, A.D.; Brooks, S.G.; Kohanski, M.A.; Blasetti, M.T.; Cowart, B.J.; Mansfield, C.; Kennedy, D.W.; Palmer, J.N.; Adappa, N.D.; Reed, D.R.; et al. Bitter and sweet taste tests are reflective of disease status in chronic rhinosinusitis. J. Allergy Clin. Immunol. Pract. 2018, 6, 1078–1080. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Reitsma, S.; Wang, D.Y.; Fokkens, W.J. Updates in biologic therapy for chronic rhinosinusitis with nasal polyps and NSAID-exacerbated respiratory disease. Allergy 2022, 77, 3593–3605. [Google Scholar] [CrossRef] [PubMed]
| Diagnosis | Prognosis | Treatment | |
|---|---|---|---|
| Eosinophil count | |||
| Blood | EosCRSwNP [11], EosCRS [12] | EosCRS [15], CRS [16] | |
| Tissue | CRS [22,23] | CRSwNP [18,20,21,22,24], CRS [22,23,25], EosCRSwNP [26] | |
| Immunoglobulin E (IgE) | |||
| Serum | CRS [27], EosCRS [29] | CRSwNP [30] † | |
| Tissue | EosCRS [31] | CRSwNP [32,33,34,35] | CRSwNP [30] † |
| Nasal secretions | CRSwNP [38] | CRSwNP [39] † | |
| Eosinophil granule proteins (EGPs) | |||
| |||
| Serum | CRSwNP [44], EosCRS [45] | CRS [46] | |
| Nasal secretions | CRS [47] | ||
| |||
| Serum | EosCRS [45] | ||
| |||
| Tissue | CRS [52] | ||
| Periostin | |||
| Serum | CRSwNP [55,56,57], EosCRSwNP [58] | EosCRS [55,59], CRSwNP [56] | |
| Tissue | CRS [60], EosCRSwNP [61], CRSwNP [55] | ||
| Interleukins (ILs) | |||
| |||
| Tissue | EosCRS [31,63,64], CRS [65] | CRSwNP [32,35,66], EosCRS [64] | |
| Nasal secretions | CRS [67] | CRSwNP [70,71] †, CRS [65] † | |
| |||
| Nasal secretions | CRS [75], CRSwNP [75] | ||
| |||
| NA | CRSwNP [76] † | ||
| |||
| Tissue | EosCRS [77] | ||
| |||
| Tissue | CRSwNP [78] | CRSwNP [78,79] | CRSwNP * [81] † |
| |||
| Tissue | CRSwNP [82,84] | CRSwNP [83,84] | CRSwNP * [84] † |
| |||
| Tissue | CRSwNP [86] | ||
| Eotaxin | |||
| Plasma | EosCRS [89] | CRSwNP [39] † | |
| Tissue | CRSwNP [34], EosCRS [88] | ||
| Nitric oxide (NO) | |||
| Nasal exhalation | CRSwNP [92,93,96], CRSsNP [94], CRS [95] | CRSwNP [92,93,95,96,97] | CRS [93,97,98,99] |
| Matrix metalloproteinase (MMP) | |||
| Tissue | CRSwNP [101,102,103,104] | CRS [105] | |
| Nasal secretions | CRS [106] | CRSwNP [107], CRS [108] | |
| P-glycoprotein (P-gp) | |||
| Tissue | CRSwNP [110,111] | ||
| Nasal secretions | CRSwNP [112], CRS [112] | CRSwNP [113] | |
| Glucocorticoid receptor ß (GRß) | |||
| Tissue | CRSwNP [114,116] | ||
| Mucin | |||
| Tissue | CRSwNP [119,120] | ||
| Taste receptors | |||
| NA | CRS [121,122] | CRSsNP [123] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seah, J.J.; Thong, M.; Wang, D.Y. The Diagnostic and Prognostic Role of Biomarkers in Chronic Rhinosinusitis. Diagnostics 2023, 13, 715. https://doi.org/10.3390/diagnostics13040715
Seah JJ, Thong M, Wang DY. The Diagnostic and Prognostic Role of Biomarkers in Chronic Rhinosinusitis. Diagnostics. 2023; 13(4):715. https://doi.org/10.3390/diagnostics13040715
Chicago/Turabian StyleSeah, Jun Jie, Mark Thong, and De Yun Wang. 2023. "The Diagnostic and Prognostic Role of Biomarkers in Chronic Rhinosinusitis" Diagnostics 13, no. 4: 715. https://doi.org/10.3390/diagnostics13040715
APA StyleSeah, J. J., Thong, M., & Wang, D. Y. (2023). The Diagnostic and Prognostic Role of Biomarkers in Chronic Rhinosinusitis. Diagnostics, 13(4), 715. https://doi.org/10.3390/diagnostics13040715






