Brain Tumor at Diagnosis: From Cognition and Behavior to Quality of Life
Abstract
1. Introduction
2. Materials and Methods
3. Symptoms at Diagnosis
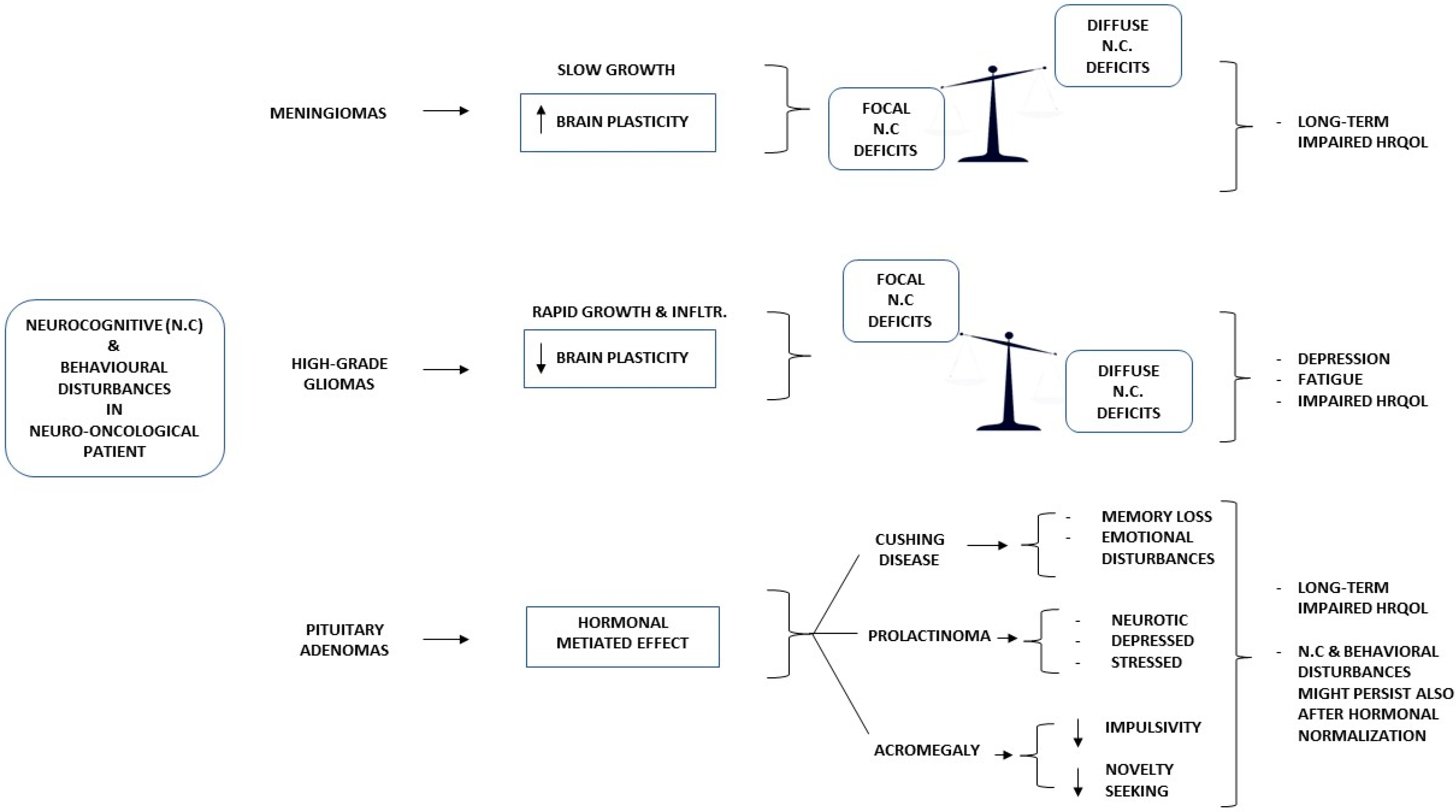
4. Meningioma
5. Glioma
6. Pituitary Adenoma
7. Communication of Diagnosis
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.M.; Parney, I.F.; Huang, W.; Anderson, F.A., Jr.; Asher, A.L.; Bernstein, M.; Lillehei, K.O.; Brem, H.; Berger, M.S.; Laws, E.R. Glioma Outcomes Project Investigators. Patterns of care for adults with newly diagnosed malignant glioma. JAMA 2005, 293, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Lageman, S.K.; Cerhan, J.H.; Locke, D.E.; Anderson, S.K.; Wu, W.; Brown, P.D. Comparing neuropsychological tasks to optimize brief cognitive batteries for brain tumor clinical trials. J. Neurooncol. 2010, 96, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Schiavolin, S.; Raggi, A.; Scaratti, C.; Toppo, C.; Silvaggi, F.; Sattin, D.; Broggi, M.; Ferroli, P.; Leonardi, M. Outcome prediction in brain tumor surgery: A literature review on the influence of nonmedical factors. Neurosurg. Rev. 2021, 44, 807–819. [Google Scholar] [CrossRef] [PubMed]
- Bunevicius, A.; Deltuva, V.P.; Tamasauskas, A. Association of pre-operative depressive and anxiety symptoms with five-year survival of glioma and meningioma patients: A prospective cohort study. Oncotarget 2017, 8, 57543–57551. [Google Scholar] [CrossRef]
- Thong, M.S.Y.; van Noorden, C.J.F.; Steindorf, K.; Arndt, V. Cancer-Related Fatigue: Causes and Current Treatment Options. Curr. Treat Options Oncol. 2020, 21, 17. [Google Scholar] [CrossRef]
- van der Linden, S.D.; Gehring, K.; Rutten, G.M.; Kop, W.J.; Sitskoorn, M.M. Prevalence and correlates of fatigue in patients with meningioma before and after surgery. Neurooncol. Pract. 2020, 7, 77–85. [Google Scholar] [CrossRef]
- Cheng, J.X.; Liu, B.L.; Zhang, X.; Lin, W.; Zhang, Y.Q.; Liu, W.P.; Zhang, J.N.; Lin, H.; Wang, R.; Yin, H. Health-related quality of life in glioma patients in China. BMC Cancer 2010, 10, 305. [Google Scholar] [CrossRef]
- Armstrong, T.S.; Vera-Bolanos, E.; Acquaye, A.A.; Gilbert, M.R.; Ladha, H.; Mendoza, T. The symptom burden of primary brain tumors: Evidence for a core set of tumor- and treatment-related symptoms. Neuro Oncol. 2016, 18, 252–260. [Google Scholar] [CrossRef]
- Rockhill, J.; Mrugala, M.; Chamberlain, M.C. Intracranial meningiomas: An overview of diagnosis and treatment. Neurosurg. Focus. 2007, 23, E1. [Google Scholar] [CrossRef]
- Whittle, I.R.; Smith, C.; Navoo, P.; Collie, D. Meningiomas. Lancet 2004, 363, 1535–1543. [Google Scholar] [CrossRef] [PubMed]
- Tucha, O.; Smely, C.; Preier, M.; Becker, G.; Paul, G.M.; Lange, K.W. Preoperative and postoperative cognitive functioning in patients with frontal meningiomas. J. Neurosurg. 2003, 98, 21–31. [Google Scholar] [CrossRef]
- Meskal, I.; Gehring, K.; van der Linden, S.D.; Rutten, G.J.; Sitskoorn, M.M. Cognitive improvement in meningioma patients after surgery: Clinical relevance of computerized testing. J. Neurooncol. 2015, 121, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Yoshii, Y.; Tominaga, D.; Sugimoto, K.; Tsuchida, Y.; Hyodo, A.; Yonaha, H.; Kushi, S. Cognitive function of patients with brain tumor in pre- and postoperative stage. Surg. Neurol. 2008, 69, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Van Nieuwenhuizen, D.; Ambachtsheer, N.; Heimans, J.J.; Reijneveld, J.C.; Peerdeman, S.M.; Klein, M. Neurocognitive functioning and health-related quality of life in patients with radiologically suspected meningiomas. J. Neurooncol. 2013, 113, 433–440. [Google Scholar] [CrossRef]
- Abel, T.J.; Manzel, K.; Bruss, J.; Belfi, A.M.; Howard, M.A., 3rd; Tranel, D. The cognitive and behavioral effects of meningioma lesions involving the ventromedial prefrontal cortex. J. Neurosurg. 2016, 124, 1568–1577. [Google Scholar] [CrossRef]
- Pranckeviciene, A.; Deltuva, V.P.; Tamasauskas, A.; Bunevicius, A. Association between psychological distress, subjective cognitive complaints and objective neuropsychological functioning in brain tumor patients. Clin. Neurol. Neurosurg. 2017, 163, 18–23. [Google Scholar] [CrossRef]
- Van Lonkhuizen, P.J.C.; Rijnen, S.J.M.; van der Linden, S.D.; Rutten, G.M.; Gehring, K.; Sitskoorn, M.M. Subjective cognitive functioning in patients with a meningioma: Its course and association with objective cognitive functioning and psychological symptoms. Psychooncology 2019, 28, 1654–1662. [Google Scholar] [CrossRef]
- Merckelbach, H.; Muris, P.; Nijman, H.; de Jong, P. Self-reported cognitive failures and neurotic symptomatology. Pers. Individ. Differ. 1996, 20, 715–724. [Google Scholar] [CrossRef]
- Zamanipoor Najafabadi, A.H.; Peeters, M.C.M.; Dirven, L.; Lobatto, D.J.; Groen, J.L.; Broekman, M.L.D.; Peerdeman, S.M.; Peul, W.C.; Taphoorn, M.J.B.; van Furth, W.R. Impaired health-related quality of life in meningioma patients-a systematic review. Neuro Oncol. 2017, 19, 897–907. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Feeny, D.H.; Patrick, D.L. Measuring health-related quality of life. Ann. Intern. Med. 1993, 118, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Zhang, H.; Wu, J.; Yu, Z.; Chen, X.; Rekik, I.; Wang, Q.; Lu, J.; Shen, D. Overall survival time prediction for high-grade glioma patients based on large-scale brain functional networks. Brain Imaging Behav. 2019, 13, 1333–1351. [Google Scholar] [CrossRef] [PubMed]
- Acevedo-Vergara, K.; Perez-Florez, M.; Ramirez, A.; Torres-Bayona, S.; Dau, A.; Salva, S.; Maloof, D.; Garcia, C.; Luque, M.; Guillen-Burgos, H.F. Cognitive deficits in adult patients with high-grade glioma: A systematic review. Clin. Neurol Neurosurg. 2022, 219, 107296. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Tao, L.; Qian, Z.; Wu, J.; Liu, H.; Yu, Y.; Song, J.; Wang, S.; Sun, J. Altered brain anatomical networks and disturbed connection density in brain tumor patients revealed by diffusion tensor tractography. Int. J. Comput. Assist. Radiol. Surg. 2016, 11, 2007–2019. [Google Scholar] [CrossRef] [PubMed]
- Marin, D.; Madotto, E.; Fabbro, F.; Skrap, M.; Tomasino, B. Design fluency and neuroan-atomical correlates in 54 neurosurgical patients with lesions to the right hemi-sphere. J. Neurooncol. 2017, 135, 141–150. [Google Scholar] [CrossRef]
- Habets, E.J.J.; Hendriks, E.J.; Taphoorn, M.J.B.; Douw, L.; Zwinderman, A.H.; Vandertop, W.P.; Barkhof, F.; De Witt Hamer, P.C.; Klein, M. Association between tumor location and neurocognitive functioning using tumor localization maps. J. Neurooncol. 2019, 144, 573–582. [Google Scholar] [CrossRef]
- Papagno, C.; Casarotti, A.; Comi, A.; Pisoni, A.; Lucchelli, F.; Bizzi, A.; Riva, M.; Bello, L. Long-term proper name anomia after removal of the uncinate fasciculus. Brain Struct Funct. 2016, 221, 687–694. [Google Scholar] [CrossRef]
- Zacharia, T.T.; Eslinger, P.J. Functional MRI activation patterns of cerebellum in patients with epilepsy and brain tumors. Clin. Anat. 2019, 32, 1053–1060. [Google Scholar] [CrossRef]
- Ahmadian, N.; van Baarsen, K.; van Zandvoort, M.; Robe, P.A. The Cerebellar Cognitive Affective Syndrome-a Meta-analysis. Cerebellum 2019, 18, 941–950. [Google Scholar] [CrossRef]
- Schmahmann, J.D.; Sherman, J.C. The cerebellar cognitive affective syndrome. Brain 1998, 121 Pt 4, 561–579. [Google Scholar] [CrossRef]
- Sagberg, L.M.; Iversen, D.H.; Fyllingen, E.H.; Jakola, A.S.; Reinertsen, I.; Solheim, O. Brain atlas for assessing the impact of tumor location on perioperative quality of life in patients with high-grade glioma: A prospective population-based cohort study. Neuroimage Clin. 2019, 21, 101658. [Google Scholar] [CrossRef] [PubMed]
- Mugge, L.; Mansour, T.R.; Crippen, M.; Alam, Y.; Schroeder, J. Depression and glioblastoma, complicated concomitant diseases: A systemic review of published literature. Neurosurg. Rev. 2020, 43, 497–511. [Google Scholar] [CrossRef] [PubMed]
- Bunevicius, A. Personality traits, patient-centered health status and prognosis of brain tumor patients. J. Neurooncol. 2018, 137, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Fabi, A.; Bhargava, R.; Fatigoni, S.; Guglielmo, M.; Horneber, M.; Roila, F.; Weis, J.; Jordan, K.; Ripamonti, C.I. ESMO Guidelines Committee. Electronic address: Clinicalguidelines@esmo.org. Cancer-related fatigue: ESMO Clinical Practice Guidelines for diagnosis and treatment. Ann. Oncol. 2020, 31, 713–723. [Google Scholar] [CrossRef] [PubMed]
- Coomans, M.B.; Dirven, L.; Aaronson, N.K.; Baumert, B.G.; Van Den Bent, M.; Bottomley, A.; Brandes, A.A.; Chinot, O.; Coens, C.; Gorlia, T.; et al. Symptom clusters in newly diagnosed glioma patients: Which symptom clusters are independently associated with functioning and global health status? Neuro Oncol. 2019, 21, 1447–1457. [Google Scholar] [CrossRef] [PubMed]
- Molassiotis, A.; Wilson, B.; Brunton, L.; Chaudhary, H.; Gattamaneni, R.; McBain, C. Symptom experience in patients with primary brain tumours: A longitudinal exploratory study. Eur. J. Oncol. Nurs. 2010, 14, 410–416. [Google Scholar] [CrossRef] [PubMed]
- de Dreu, M.J.; Schouwenaars, I.T.; Rutten, G.J.M.; Ramsey, N.F.; Jansma, J.M. Fatigue in brain tumor patients, towards a neuronal biomarker. Neuroimage Clin. 2020, 28, 102406. [Google Scholar] [CrossRef] [PubMed]
- Röttgering, J.G.; Douw, L.; de Witt Hamer, P.C.; Kouwenhoven, M.C.M.; Würdinger, T.; van de Ven, P.M.; Sharpe, L.; Knoop, H.; Klein, M. Reducing severe fatigue in patients with diffuse glioma: A study protocol for an RCT on the effect of blended cognitive behavioural therapy. Trials 2022, 23, 568. [Google Scholar] [CrossRef]
- Song, L.; Quan, X.; Su, L.; Wang, K.; Wang, H.; Wu, L.; Chen, C.; Li, S.; Xiang, W.; Chen, L.; et al. Inflammation and behavioral symptoms in preoperational glioma patients: Is depression, anxiety, and cognitive impairment related to markers of systemic inflammation? Brain Behav. 2020, 10, e01771. [Google Scholar] [CrossRef]
- Alsumali, A.; Cote, D.J.; Regestein, Q.R.; Crocker, E.; Alzarea, A.; Zaidi, H.A.; Bi, W.L.; Dawood, H.Y.; Broekman, M.L.; van Zandvoort, M.J.E.; et al. The impact of transsphenoidal surgery on neurocognitive function: A systematic review. J. Clin. Neurosci. 2017, 42, 1–6. [Google Scholar] [CrossRef]
- Hendrix, P.; Hans, E.; Griessenauer, C.J.; Simgen, A.; Oertel, J.; Karbach, J. Neurocognitive status in patients with newly-diagnosed brain tumors in good neurological condition: The impact of tumor type, volume, and location. Clin. Neurol Neurosurg. 2017, 156, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Tiemensma, J.; Kaptein, A.A.; Pereira, A.M.; Smit, J.W.; Romijn, J.A.; Biermasz, N.R. Coping strategies in patients after treatment for functioning or nonfunctioning pituitary adenomas. J. Clin. Endocrinol. Metab. 2011, 96, 964–971. [Google Scholar] [CrossRef] [PubMed]
- Pertichetti, M.; Serioli, S.; Belotti, F.; Mattavelli, D.; Schreiber, A.; Cappelli, C.; Padovani, A.; Gasparotti, R.; Nicolai, P.; Fontanella, M.M.; et al. Pituitary adenomas and neuropsychological status: A systematic literature review. Neurosurg Rev. 2020, 43, 1065–1078. [Google Scholar] [CrossRef]
- Wang, X.; Tong, X.; Zou, Y.; Tian, X.; Mao, Z.; Sun, Z. The impact on cognitive functions of patients with pituitary adenoma before and after surgery. Neurol Sci. 2017, 38, 1315–1321. [Google Scholar] [CrossRef]
- Mauri, M.; Sinforiani, E.; Bono, G.; Vignati, F.; Berselli, M.E.; Attanasio, R.; Nappi, G. Memory impairment in Cushing’s disease. Acta Neurol Scand. 1993, 87, 52–55. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.; Resmini, E.; Pascual, J.C.; Crespo, I.; Webb, S.M. Psychiatric Symptoms in Patients with Cushing’s Syndrome: Prevalence, Diagnosis and Management. Drugs 2017, 77, 829–842. [Google Scholar] [CrossRef]
- Feelders, R.A.; Pulgar, S.J.; Kempel, A.; Pereira, A.M. The burden of Cushing’s disease: Clinical and health-related quality of life aspects. Eur. J. Endocrinol. 2012, 167, 311–326. [Google Scholar] [CrossRef]
- Sievers, C.; Ising, M.; Pfister, H.; Dimopoulou, C.; Schneider, H.J.; Roemmler, J.; Schopohl, J.; Stalla, G.K. Personality in patients with pituitary adenomas is characterized by increased anxiety-related traits: Comparison of 70 acromegalic patients with patients with non-functioning pituitary adenomas and age- and gender-matched controls. Eur. J. Endocrinol. 2009, 160, 367–373. [Google Scholar] [CrossRef]
- Wagenmakers, M.A.; Netea-Maier, R.T.; Prins, J.B.; Dekkers, T.; den Heijer, M.; Hermus, A.R. Impaired quality of life in patients in long-term remission of Cushing’s syndrome of both adrenal and pituitary origin: A remaining effect of long-standing hypercortisolism? Eur. J. Endocrinol. 2012, 167, 687–695. [Google Scholar] [CrossRef]
- Pereira, A.M.; Tiemensma, J.; Romijn, J.A. Neuropsychiatric disorders in Cushing’s syndrome. Neuroendocrinology 2010, 92 (Suppl. 1), 65–70. [Google Scholar] [CrossRef]
- Kindratt, T.B.; Atem, F.; Dallo, F.J.; Allicock, M.; Balasubramanian, B.A. The Influence of Patient-Provider Communication on Cancer Screening. J. Patient Exp. 2020, 7, 1648–1657. [Google Scholar] [CrossRef] [PubMed]
- Peterson, E.B.; Ostroff, J.S.; DuHamel, K.N.; D’Agostino, T.A.; Hernandez, M.; Canzona, M.R.; Bylund, C.L. Impact of provider-patient communication on cancer screening adherence: A systematic review. Prev. Med. 2016, 93, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Baccolini, V.; Isonne, C.; Salerno, C.; Giffi, M.; Migliara, G.; Mazzalai, E.; Turatto, F.; Sinopoli, A.; Rosso, A.; De Vito, C.; et al. The association between adherence to cancer screening programs and health literacy: A systematic review and meta-analysis. Prev. Med. 2022, 155, 106927. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Davis, T.C.; McCormack, L. Health literacy: What is it? J. Health Commun. 2010, 15 (Suppl. 2), 9–19. [Google Scholar] [CrossRef]
- Papadakos, J.K.; Hasan, S.M.; Barnsley, J.; Berta, W.; Fazelzad, R.; Papadakos, C.J.; Giuliani, M.E.; Howell, D. Health literacy and cancer self-management behaviors: A scoping review. Cancer 2018, 124, 4202–4210. [Google Scholar] [CrossRef]
- Housten, A.J.; Gunn, C.M.; Paasche-Orlow, M.K.; Basen-Engquist, K.M. Health Literacy Interventions in Cancer: A Systematic Review. J. Cancer Educ. 2021, 36, 240–252. [Google Scholar] [CrossRef]
- Hasannejadasl, H.; Roumen, C.; Smit, Y.; Dekker, A.; Fijten, R. Health Literacy and eHealth: Challenges and Strategies. JCO Clin. Cancer Inform. 2022, 6, e2200005. [Google Scholar] [CrossRef]
- Koay, K.; Schofield, P.; Jefford, M. Importance of health literacy in oncology. Asia Pac. J. Clin. Oncol. 2012, 8, 14–23. [Google Scholar] [CrossRef]
- Petersen, G.S.; Laursen, S.G.W.; Jensen, H.; Maindal, H.T.; Pedersen, A.F.; Vedsted, P.; Virgilsen, L.F. Patients’ health literacy is associated with timely diagnosis of cancer-A cross-sectional study in Denmark. Eur. J. Cancer Care 2022, 31, e13532. [Google Scholar] [CrossRef]
- Moore, C.; Hassett, D.; Dunne, S. Health literacy in cancer caregivers: A systematic review. J. Cancer Surviv. 2021, 15, 825–836. [Google Scholar] [CrossRef]
- Buyens, G.; van Balken, M.; Oliver, K.; Price, R.; Venegoni, E.; Lawler, M.; Battisti, N.M.L.; Van Poppel, H. Cancer literacy—Informing patients and implementing shared decision making. J. Cancer Policy 2022, 35, 100375. [Google Scholar] [CrossRef]
- Kim, H.; Goldsmith, J.V.; Sengupta, S.; Mahmood, A.; Powell, M.P.; Bhatt, J.; Chang, C.F.; Bhuyan, S.S. Mobile Health Application and e-Health Literacy: Opportunities and Concerns for Cancer Patients and Caregivers. J. Cancer Educ. 2019, 34, 3–8. [Google Scholar] [CrossRef]
- Chawla, N.; Blanch-Hartigan, D.; Virgo, K.S.; Ekwueme, D.U.; Han, X.; Forsythe, L.; Rodriguez, J.; McNeel, T.S.; Yabroff, K.R. Quality of Patient-Provider Communication Among Cancer Survivors: Findings From a Nationally Representative Sample. J. Oncol. Pract. 2016, 12, e964–e973. [Google Scholar] [CrossRef]
- Lobb, E.A.; Halkett, G.K.; Nowak, A.K. Patient and caregiver perceptions of communication of prognosis in high grade glioma. J. Neurooncol. 2011, 104, 315–322. [Google Scholar] [CrossRef]
- Gilligan, T.; Salmi, L.; Enzinger, A. Patient-Clinician Communication Is a Joint Creation: Working Together Toward Well-Being. Am. Soc. Clin. Oncol. Educ. Book 2018, 38, 532–539. [Google Scholar] [CrossRef]
- Comelli, I.; Lippi, G.; Campana, V.; Servadei, F.; Cervellin, G. Clinical presentation and epidemiology of brain tumors firstly diagnosed in adults in the Emergency Department: A 10-year, single center retrospective study. Ann. Transl. Med. 2017, 5, 269. [Google Scholar] [CrossRef]
- van de Belt, T.H.; Nijmeijer, H.; Grim, D.; Engelen, L.J.L.P.G.; Vreeken, R.; van Gelder, M.M.H.J.; Ter Laan, M. Patient-Specific Actual-Size Three-Dimensional Printed Models for Patient Education in Glioma Treatment: First Experiences. World Neurosurg. 2018, 117, e99–e105. [Google Scholar] [CrossRef]
- Bragard, I.; Razavi, D.; Marchal, S.; Merckaert, I.; Delvaux, N.; Libert, Y.; Reynaert, C.; Boniver, J.; Klastersky, J.; Scalliet, P.; et al. Teaching communication and stress management skills to junior physicians dealing with cancer patients: A Belgian Interuniversity Curriculum. Support Care Cancer 2006, 14, 454–461. [Google Scholar] [CrossRef]
- Ley, A.; Kamp, M.; von Sass, C.; Hänggi, D.; Sabel, M.; Rapp, M. Psychooncological distress in low-grade glioma patients-a monocentric study. Acta Neurochir. 2022, 164, 713–722. [Google Scholar] [CrossRef]
- Hartung, T.J.; Brähler, E.; Faller, H.; Härter, M.; Hinz, A.; Johansen, C.; Keller, M.; Koch, U.; Schulz, H.; Weis, J.; et al. The risk of being depressed is significantly higher in cancer patients than in the general population: Prevalence and severity of depressive symptoms across major cancer types. Eur. J. Cancer 2017, 72, 46–53. [Google Scholar] [CrossRef]
- Adduci, A.; Jankovic, M.; Strazzer, S.; Massimino, M.; Clerici, C.; Poggi, G. Parent-child communication and psychological adjustment in children with a brain tumor. Pediatr. Blood Cancer 2012, 59, 290–294. [Google Scholar] [CrossRef]
- Stein, A.; Dalton, L.; Rapa, E.; Bluebond-Langner, M.; Hanington, L.; Stein, K.F.; Ziebland, S.; Rochat, T.; Harrop, E.; Kelly, B.; et al. Communication with children and adolescents about the diagnosis of their own life-threatening condition. Lancet 2019, 393, 1150–1163. [Google Scholar] [CrossRef]
- The Lancet. Let’s talk with children about life-threatening diseases. Lancet 2019, 393, 1072. [Google Scholar] [CrossRef]
- Back, A.L.; Arnold, R.M.; Baile, W.F.; Fryer-Edwards, K.A.; Alexander, S.C.; Barley, G.E.; Gooley, T.A.; Tulsky, J.A. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch. Intern. Med. 2007, 167, 453–460. [Google Scholar] [CrossRef]
- Brandes, K.; Butow, P.N.; Tattersall, M.H.; Clayton, J.M.; Davidson, P.M.; Young, J.; Epstein, R.M.; Walczak, A. Advanced cancer patients’ and caregivers’ use of a Question Prompt List. Patient Educ. Couns. 2014, 97, 30–37. [Google Scholar] [CrossRef]
- Sacks, P.; Rahman, M. Epidemiology of Brain Metastases. Neurosurg. Clin. N. Am. 2020, 31, 481–488. [Google Scholar] [CrossRef]
- Mela, A.; Poniatowski, Ł.A.; Drop, B.; Furtak-Niczyporuk, M.; Jaroszyński, J.; Wrona, W.; Staniszewska, A.; Dąbrowski, J.; Czajka, A.; Jagielska, B.; et al. Overview and Analysis of the Cost of Drug Programs in Poland: Public Payer Expenditures and Coverage of Cancer and Non-Neoplastic Diseases Related Drug Therapies from 2015–2018 Years. Front. Pharmacol. 2020, 11, 1123. [Google Scholar] [CrossRef]
- Mela, A.; Rdzanek, E.; Tysarowski, A.; Sakowicz, M.; Jaroszyński, J.; Furtak-Niczyporuk, M.; Żurek, G.; Poniatowski, Ł.A.; Jagielska, B. The impact of changing the funding model for genetic diagnostics and improved access to personalized medicine in oncology. Expert Rev. Pharmacoecon. Outcomes Res. 2023, 23, 43–54. [Google Scholar] [CrossRef]
- Walker, E.V.; Ross, J.; Yuan, Y.; Smith, T.R.; Davis, F.G. Brain cancer survival in Canada 1996–2008: Effects of sociodemographic characteristics. Curr. Oncol. 2019, 26, e292–e299. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chieffo, D.P.R.; Lino, F.; Ferrarese, D.; Belella, D.; Della Pepa, G.M.; Doglietto, F. Brain Tumor at Diagnosis: From Cognition and Behavior to Quality of Life. Diagnostics 2023, 13, 541. https://doi.org/10.3390/diagnostics13030541
Chieffo DPR, Lino F, Ferrarese D, Belella D, Della Pepa GM, Doglietto F. Brain Tumor at Diagnosis: From Cognition and Behavior to Quality of Life. Diagnostics. 2023; 13(3):541. https://doi.org/10.3390/diagnostics13030541
Chicago/Turabian StyleChieffo, Daniela Pia Rosaria, Federica Lino, Daniele Ferrarese, Daniela Belella, Giuseppe Maria Della Pepa, and Francesco Doglietto. 2023. "Brain Tumor at Diagnosis: From Cognition and Behavior to Quality of Life" Diagnostics 13, no. 3: 541. https://doi.org/10.3390/diagnostics13030541
APA StyleChieffo, D. P. R., Lino, F., Ferrarese, D., Belella, D., Della Pepa, G. M., & Doglietto, F. (2023). Brain Tumor at Diagnosis: From Cognition and Behavior to Quality of Life. Diagnostics, 13(3), 541. https://doi.org/10.3390/diagnostics13030541







