Correlation between Statin Solubility and Mortality in Patients on Chronic Hemodialysis
Abstract
:1. Introduction
2. Materials and Methods
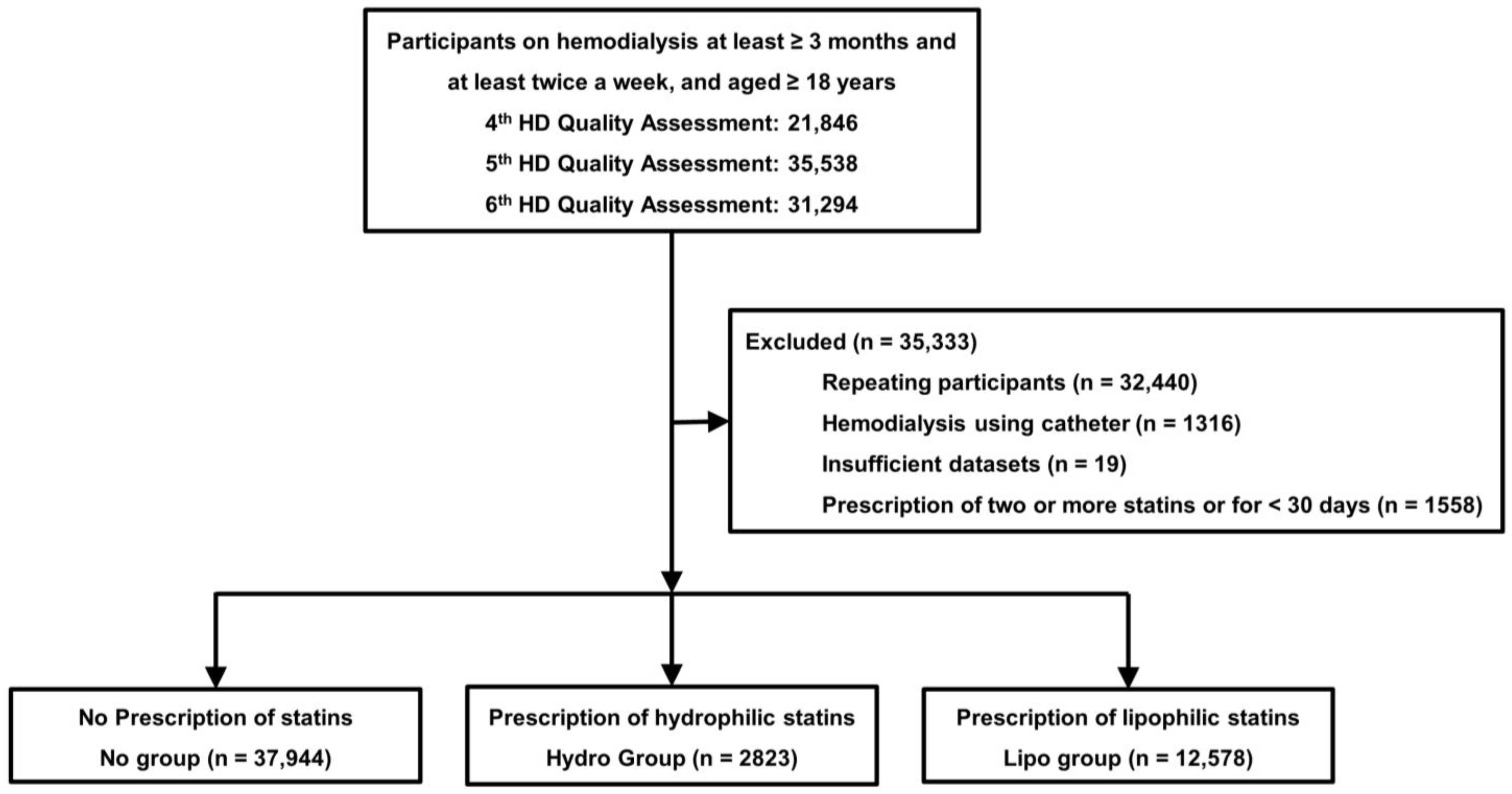
2.1. Dataset and Study’s Population
2.2. Study’s Variables
2.3. Statistical Analyses
3. Results
3.1. Participant’s Clinical Characteristics
3.2. Survival Analyses
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Choi, H.; Kim, M.; Kim, H.; Lee, J.P.; Lee, J.; Park, J.T.; Kim, K.H.; Ahn, H.S.; Hann, H.J.; Ryu, D.R. Excess mortality among patients on dialysis: Comparison with the general population in Korea. Kidney Res. Clin. Pract. 2014, 33, 89–94. [Google Scholar] [CrossRef] [PubMed]
- ESRD Registry Committee: Korean Society of Nephrology. Factsheet: CKD in Korea. Available online: https://ksn.or.kr/bbs/index.php?page=2&code=Factsheet (accessed on 31 August 2023).
- Yao, Q.; Pecoits-Filho, R.; Lindholm, B.; Stenvinkel, P. Traditional and non-traditional risk factors as contributors to atherosclerotic cardiovascular disease in end-stage renal disease. Scand. J. Urol. Nephrol. 2004, 38, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Kidney Disease: Improving Global Outcomes (KDIGO) Lipid Work Group. KDIGO clinical practice guideline for lipid management in chronic kidney disease. Kidney Int. Suppl. 2013, 3, 259–305. [Google Scholar]
- Ferri, N.; Corsini, A. Clinical Pharmacology of Statins: An Update. Curr. Atheroscler. Rep. 2020, 22, 26. [Google Scholar] [CrossRef] [PubMed]
- Oesterle, A.; Laufs, U.; Liao, J.K. Pleiotropic Effects of Statins on the Cardiovascular System. Circ. Res. 2017, 120, 229–243. [Google Scholar] [CrossRef]
- Mansi, I.A.; Sumithran, P.; Kinaan, M. Risk of diabetes with statins. BMJ 2023, 381, e071727. [Google Scholar] [CrossRef]
- Wanner, C.; Krane, V.; Marz, W.; Olschewski, M.; Mann, J.F.; Ruf, G.; Ritz, E.; German Diabetes and Dialysis Study Investigators. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N. Engl. J. Med. 2005, 353, 238–248. [Google Scholar] [CrossRef]
- Fellstrom, B.C.; Jardine, A.G.; Schmieder, R.E.; Holdaas, H.; Bannister, K.; Beutler, J.; Chae, D.W.; Chevail, A.; Cobbe, S.M.; Grönhagen-Riska, C.; et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N. Engl. J. Med. 2009, 360, 1395–1407. [Google Scholar] [CrossRef]
- Baigent, C.; Landray, M.J.; Reith, C.; Emberson, J.; Wheeler, D.C.; Tomson, C.; Wanner, C.; Krane, V.; Cass, A.; Craig, J.; et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): A randomised placebo-controlled trial. Lancet 2011, 377, 2181–2192. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Block, G.; Humphreys, M.H.; Kopple, J.D. Reverse epidemiology of cardiovascular risk factors in maintenance dialysis patients. Kidney Int. 2003, 63, 793–808. [Google Scholar] [CrossRef]
- Chen, Z.; Qureshi, A.R.; Parini, P.; Hurt-Camejo, E.; Ripsweden, J.; Brismar, T.B.; Barany, P.; Jaminon, A.M.; Schurgers, L.J.; Heimbürger, O.; et al. Does statins promote vascular calcification in chronic kidney disease? Eur. J. Clin. Investig. 2017, 47, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Arnaboldi, L.; Corsini, A. Do structural differences in statins correlate with clinical efficacy? Curr. Opin. Lipidol. 2010, 21, 298–304. [Google Scholar] [CrossRef]
- Backes, J.M.; Howard, P.A.; Ruisinger, J.F.; Moriarty, P.M. Does simvastatin cause more myotoxicity compared with other statins? Ann. Pharmacother. 2009, 43, 2012–2020. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.C.; Ahn, Y.; Jang, S.Y.; Cho, K.H.; Hwang, S.H.; Lee, M.G.; Ko, J.S.; Park, K.H.; Sim, D.S.; Yoon, N.S.; et al. Comparison of clinical outcomes of hydrophilic and lipophilic statins in patients with acute myocardial infarction. Korean J. Intern. Med. 2011, 26, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, T.; Takada, M.; Nishibori, Y.; Fujita, K.; Miki, K.; Masuda, S.; Horimatsu, T.; Hasuike, T. Comparison of preventive effect on cardiovascular events with different statins. -The CIRCLE study-. Circ. J. 2011, 75, 1951–1959. [Google Scholar] [CrossRef] [PubMed]
- Bielecka-Dabrowa, A.; Bytyçi, I.; Von Haehling, S.; Anker, S.; Jozwiak, J.; Rysz, J.; Hernandez, A.V.; Bajraktari, G.; Mikhailidis, D.P.; Banach, M. Association of statin use and clinical outcomes in heart failure patients: A systematic review and meta-analysis. Lipids Health Dis. 2019, 18, 188. [Google Scholar] [CrossRef] [PubMed]
- Bytyçi, I.; Bajraktari, G.; Bhatt, D.L.; Morgan, C.J.; Ahmed, A.; Aronow, W.S.; Banach, M.; Lipid and Blood Pressure Meta-analysis Collaboration (LBPMC) Group. Hydrophilic vs lipophilic statins in coronary artery disease: A meta-analysis of randomized controlled trials. J. Clin. Lipidol. 2017, 11, 624–637. [Google Scholar] [CrossRef]
- Wang, S.W.; Li, L.C.; Su, C.H.; Yang, Y.H.; Hsu, T.W.; Hsu, C.N. Association of Statin and Its Lipophilicity With Cardiovascular Events in Patients Receiving Chronic Dialysis. Clin. Pharmacol. Ther. 2020, 107, 1312–1324. [Google Scholar] [CrossRef]
- Kang, M.H.; Kim, W.; Kim, J.S.; Jeong, K.H.; Jeong, M.H.; Hwang, J.Y.; Hur, S.H.; Hwang, H.S. Hydrophilic Versus Lipophilic Statin Treatments in Patients With Renal Impairment After Acute Myocardial Infarction. J. Am. Heart Assoc. 2022, 11, e024649. [Google Scholar] [CrossRef]
- Kang, S.H.; Kim, B.Y.; Son, E.J.; Kim, G.O.; Do, J.Y. Comparison of Patient Survival According to Erythropoiesis-Stimulating Agent Type of Treatment in Maintenance Hemodialysis Patients. J. Clin. Med. 2023, 12, 625. [Google Scholar] [CrossRef]
- Health Insurance Review & Assessment Service. 6th Hemodialysis Quality Assessment Program. Available online: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020002000100&brdScnBltNo=4&brdBltNo=6619#none (accessed on 15 December 2022).
- Daugirdas, J.T. Second generation logarithmic estimates of single-pool variable volume Kt/V: An analysis of error. J. Am. Soc. Nephrol. 1993, 4, 1205–1213. [Google Scholar] [CrossRef] [PubMed]
- Climent, E.; Benaiges, D.; Pedro-Botet, J. Hydrophilic or Lipophilic Statins? Front Cardiovasc. Med. 2021, 8, 687585. [Google Scholar] [CrossRef] [PubMed]
- Stone, N.J.; Robinson, J.G.; Lichtenstein, A.H.; Bairey Merz, C.N.; Blum, C.B.; Eckel, R.H.; Goldberg, A.C.; Gordon, D.; Levy, D.; Lloyd-Jones, D.M.; et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 129, S1–S45. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef]
- Endo, A.A. historical perspective on the discovery of statins. Proc. Jpn. Acad. Ser B Phys. Biol. Sci. 2010, 86, 484–493. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e1046–e1081. [Google Scholar]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e563–e595. [Google Scholar] [PubMed]
- Virani, S.S.; Smith, S.C.; Stone, N.J., Jr.; Grundy, S.M. Secondary Prevention for Atherosclerotic Cardiovascular Disease: Comparing Recent US and European Guidelines on Dyslipidemia. Circulation 2020, 141, 1121–1123. [Google Scholar] [CrossRef]
- Germershausen, J.I.; Hunt, V.M.; Bostedor, R.G.; Bailey, P.J.; Karkas, J.D.; Alberts, A.W. Tissue selectivity of the cholesterol-lowering agents lovastatin, simvastatin and pravastatin in rats in vivo. Biochem. Biophys. Res. Comm. 1989, 158, 667–675. [Google Scholar] [CrossRef]
- McKenney, J.M. Pharmacologic characteristics of statins. Clin. Cardiol. 2003, 26, S32–S38. [Google Scholar] [CrossRef]
- Davignon, J. Pleiotropic effects of pitavastatin. Br. J. Clin. Pharmacol. 2012, 73, 518–535. [Google Scholar] [CrossRef] [PubMed]
- Ichihara, K.; Satoh, K. Disparity between angiographic regression and clinical event rates with hydrophobic statins. Lancet 2002, 359, 2195–2198. [Google Scholar] [CrossRef]
- Chung, C.M.; Lin, M.S.; Chang, C.H.; Cheng, H.W.; Chang, S.T.; Wang, P.C.; Chang, H.Y.; Lin, Y.S. Moderate to high intensity statin in dialysis patients after acute myocardial infarction: A national cohort study in Asia. Atherosclerosis 2017, 267, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.Y.; Hsieh, T.H.; Hung, S.C. Association of secondary prevention medication use after myocardial infarction with mortality in hemodialysis patients. Clin. Kidney J. 2022, 15, 2135–2143. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Choi, W.J.; Lee, Y.; Lee, K.; Park, M.W.; Myong, J.P.; Kim, D.W. Association between statin therapy and mortality in patients on dialysis after atherosclerotic cardiovascular diseases. Sci. Rep. 2023, 13, 10940. [Google Scholar] [CrossRef]

| No Group (n = 37,944) | Hydro Group (n = 2823) | Lipo Group (n = 12,578) | p | |
|---|---|---|---|---|
| Age (years) | 59.4 ± 13.3 | 62.1 ± 11.9 * | 62.1 ± 12.1 * | <0.001 |
| Sex (male, %) | 23,450 (61.8%) | 1555 (55.1%) | 6906 (54.9%) | <0.001 |
| Hemodialysis vintage (months) | 56.4 ± 59.0 | 40.4 ± 46.2 * | 42.2 ± 47.4 * | <0.001 |
| Underlying causes of ESRD | <0.001 | |||
| Diabetes mellitus | 14,642 (38.6%) | 1589 (56.3%) | 7028 (55.9%) | |
| Hypertension | 10,707 (28.2%) | 626 (22.2%) | 2726 (21.7%) | |
| Glomerulonephritis | 4453 (11.7%) | 190 (6.7%) | 1048 (8.3%) | |
| Others | 3538 (9.3%) | 182 (6.4%) | 785 (6.2%) | |
| Unknown | 4604 (12.1%) | 236 (8.4%) | 991 (7.9%) | |
| CCI score | 7.2 ± 2.9 | 8.4 ± 2.7 * | 8.1 ± 2.8 *# | <0.001 |
| Follow-up duration (months) | 62.2 ± 29.2 | 56.1 ± 25.1 * | 59.0 ± 27.1 *# | <0.001 |
| Type of vascular access | <0.001 | |||
| Arteriovenous fistula | 32,538 (85.8%) | 2366 (83.8%) | 10,596 (84.2%) | |
| Arteriovenous graft | 5406 (14.2%) | 457 (16.2%) | 1982 (15.8%) | |
| Kt/Vurea | 1.53 ± 0.27 | 1.54 ± 0.27 | 1.53 ± 0.27 * | 0.006 |
| Ultrafiltration volume (L/session) | 2.29 ± 0.96 | 2.22 ± 0.91 * | 2.23 ± 0.94 * | <0.001 |
| Hemoglobin (g/dL) | 10.6 ± 0.8 | 10.7 ± 0.7 * | 10.7 ± 0.7 * | <0.001 |
| Serum albumin (g/dL) | 3.99 ± 0.34 | 3.99 ± 0.34 | 3.98 ± 0.33 * | 0.041 |
| Serum phosphorus (mg/dL) | 5.0 ± 1.4 | 4.8 ± 1.3 * | 4.8 ± 1.3 * | <0.001 |
| Serum calcium (mg/dL) | 8.9 ± 0.8 | 8.8 ± 0.7 * | 8.9 ± 0.8 * | <0.001 |
| Systolic blood pressure (mmHg) | 141 ± 16 | 142 ± 16 | 141 ± 16 | 0.580 |
| Diastolic blood pressure (mmHg) | 79 ± 9 | 76 ± 10 * | 77 ± 10 *# | <0.001 |
| Serum creatinine (mg/dL) | 9.67 ± 2.77 | 8.94 ± 2.63 * | 9.09 ± 2.60 *# | <0.001 |
| Use of RASB | 11,161 (29.4%) | 876 (31.0%) | 4228 (33.6%) | <0.001 |
| Use of aspirin | 13,898 (36.6%) | 1591 (56.4%) | 7146 (56.8%) | <0.001 |
| Use of clopidogrel | 4268 (11.2%) | 837 (29.6%) | 3484 (27.7%) | <0.001 |
| MI or CHF | 15,945 (42.0%) | 1606 (56.9%) | 6524 (51.9%) | <0.001 |
| Dosage of statin | <0.001 | |||
| Low | – | 298 (10.6%) | 402 (3.2%) | |
| Moderate | – | 2287 (81.0%) | 11,873 (94.4%) | |
| High | – | 238 (8.4%) | 303 (2.4%) |
| Univariate | Multivariable | |||
|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | |
| Group | ||||
| Ref: No group | ||||
| Hydro group | 1.10 (1.03–1.17) | 0.005 | 0.95 (0.88–1.03) | 0.215 |
| Lipo group | 1.09 (1.06–1.13) | <0.001 | 0.92 (0.88–0.96) | <0.001 |
| Ref: Hydro group | ||||
| Lipo group | 0.99 (0.93–1.06) | 0.783 | 0.97 (0.89–1.06) | 0.511 |
| Age (increase per 1 year) | 1.06 (1.06–1.06) | <0.001 | 1.06 (1.06–1.06) | <0.001 |
| Sex (ref: male) | 0.87 (0.84–0.89) | <0.001 | 0.75 (0.72–0.78) | <0.001 |
| Underlying cause of ESRD (ref: DM) | 0.81 (0.80–0.82) | <0.001 | 0.90 (0.89–0.91) | <0.001 |
| Vascular access (ref: arteriovenous fistula) | 1.51 (1.46–1.56) | <0.001 | 1.18 (1.13–1.23) | <0.001 |
| Hemodialysis vintage (increase per 1 month) | 0.99 (0.99–1.00) | 0.100 | 1.00 (1.00–1.01) | <0.001 |
| CCI score (increase per 1 score) | 1.14 (1.13–1.14) | <0.001 | 1.06 (1.06–1.07) | <0.001 |
| UFV (increase per 1 kg/session) | 0.92 (0.90–0.93) | <0.001 | 1.07 (1.05–1.09) | <0.001 |
| KtVurea (increase per 1 unit) | 0.91 (0.86–0.96) | <0.001 | 0.80 (0.75–0.87) | <0.001 |
| Hemoglobin (increase per 1 g/dL) | 0.87 (0.85–0.88) | <0.001 | 0.91 (0.89–0.93) | <0.001 |
| Serum albumin (increase per 1 g/dL) | 0.37 (0.36–0.39) | <0.001 | 0.63 (0.59–0.66) | <0.001 |
| Serum creatinine (increase per 1 mg/dL) | 0.87 (0.86–0.87) | <0.001 | 0.94 (0.93–0.94) | <0.001 |
| Serum phosphorus (increase per 1 mg/dL) | 0.85 (0.84–0.86) | <0.001 | 1.04 (1.03–1.06) | <0.001 |
| Serum calcium (increase per 1 mg/dL) | 0.93 (0.92–0.95) | <0.001 | 1.06 (1.04–1.08) | <0.001 |
| SBP (increase per 1 mmHg) | 1.01 (1.01–1.01) | <0.001 | 1.01 (1.00–1.01) | <0.001 |
| DBP (increase per 1 mmHg) | 0.98 (0.98–0.98) | <0.001 | 1.00 (1.00–1.01) | 0.020 |
| Use of renin angiotensin system blocker | 1.15 (1.12–1.18) | <0.001 | 1.01 (0.98–1.05) | 0.584 |
| Use of clopidogrel | 1.53 (1.49–1.59) | <0.001 | 1.15 (1.10–1.20) | <0.001 |
| Use of aspirin | 1.16 (1.13–1.19) | <0.001 | 0.96 (0.93–0.99) | 0.016 |
| MI or CHF | 1.49 (1.45–1.53) | <0.001 | 1.05 (1.01–1.09) | 0.011 |
| Dosage of statin (ref: low) | ||||
| Moderate | 0.95 (0.85–1.07) | 0.404 | 0.97 (0.84–1.12) | 0.678 |
| High | 1.11 (0.93–1.32) | 0.254 | 1.05 (0.84–1.30) | 0.679 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, S.-H.; Kim, G.-O.; Kim, B.-Y.; Son, E.-J.; Do, J.-Y. Correlation between Statin Solubility and Mortality in Patients on Chronic Hemodialysis. Diagnostics 2023, 13, 3290. https://doi.org/10.3390/diagnostics13203290
Kang S-H, Kim G-O, Kim B-Y, Son E-J, Do J-Y. Correlation between Statin Solubility and Mortality in Patients on Chronic Hemodialysis. Diagnostics. 2023; 13(20):3290. https://doi.org/10.3390/diagnostics13203290
Chicago/Turabian StyleKang, Seok-Hui, Gui-Ok Kim, Bo-Yeon Kim, Eun-Jung Son, and Jun-Young Do. 2023. "Correlation between Statin Solubility and Mortality in Patients on Chronic Hemodialysis" Diagnostics 13, no. 20: 3290. https://doi.org/10.3390/diagnostics13203290
APA StyleKang, S.-H., Kim, G.-O., Kim, B.-Y., Son, E.-J., & Do, J.-Y. (2023). Correlation between Statin Solubility and Mortality in Patients on Chronic Hemodialysis. Diagnostics, 13(20), 3290. https://doi.org/10.3390/diagnostics13203290






