Abstract
(1) Background: The aim of our study is to investigate the effectiveness of bronchoscopic airway clearance therapy (B-ACT) on severe pneumonia (SP) patients with invasive mechanical ventilation (IMV) in the intensive care unit (ICU). (2) Methods: Our study retrospectively enrolled 49 patients with sputum aspiration and 99 patients with B-ACT, and the latter were divided into the ≤once every 3 days group (n = 50) and >once every 3 days group (n = 49). (3) Results: We found most laboratory blood results were significantly improved in the B-ACT group as compared with those in sputum aspiration group (p < 0.05). Patients in the B-ACT group and those in ≤once every 3 days group also had significantly better survival to hospital discharge than those in their counterpart groups (Logrank p < 0.001). In patients with cardiopulmonary diseases or positive cultures for bacteria, the B-ACT group and those in the ≤once every 3 days group had significantly better survival outcomes to discharge than those in their counterpart groups (Logrank p < 0.001). B-ACT and the average frequency of ≤once every 3 days had significantly better impact on survival outcomes than their counterpart groups (HR: 0.444, 95% CI: 0.238–0.829, p = 0.011; HR: 0.285, 95% CI: 0163–0.498, p < 0.001). (4) Conclusions: In the future, flexible bronchoscopes may paly an important role in ACT for SP patients with IMV.
1. Introduction
Among all infectious diseases, pneumonia is the leading cause of death for all age groups worldwide [1]. Pneumonia patients with acute respiratory failure requiring endotracheal intubation and invasive mechanical ventilation (IMV) can be diagnosed with severe pneumonia (SP), for whom direct admission to an intensive care unit (ICU) is strongly recommended [2]. The mortality rate of SP is as high as 30–50% in the ICU [3]. Compared with patients with non-invasive ventilation, SP patients receiving IMV have more deposition of mucus and microbial secretions mainly because of biofilm formation in the endotracheal tube and medical device-related infections, which may lead to a decline in airway patency, and even aggravate the lung inflammation after long-term ventilation [4]. Therefore, it is very important to improve the airway clearance therapy (ACT) of SP patients during IMV in ICU [5].
Clinically, conventional ACT mainly includes: cough or breathing exercise, auxiliary positive pressure ventilation, chest wall oscillation sputum expulsion, artificial sputum aspiration, and postural drainage [6]. Bronchoscopic airway clearance therapy (B-ACT) is a new technology which inserts the flexible bronchoscope into the primary bronchus and the subsegmental bronchi to perform artificial sputum aspiration and even give alveolar lavage for the sake of clearing airway secretions and reducing pulmonary inflammation [7]. Considering the pandemic of COVID-19 or other infectious diseases recently and the risk of pathogen transmission, B-ACT is increasingly widely used in patients with pulmonary infectious diseases in recent years [8]. Infectious Diseases Society of America/American Thoracic Society consensus guidelines highlight that further trials are urgently needed to evaluate the effects of ICU care, especially the ACT, in SP patients with IMV [9]. Currently, the Respiratory Endoscopy Committee of the Chinese Medical Association also recommended the appropriate application of flexible bronchoscopes in critically ill patients in the ICU [10]. However, the effectiveness of B-ACT in SP patients during IMV remains controversial over the years, knowing that B-ACT recommendations in currently available guidelines mainly rely on studies enrolling SP patients without undergoing IMV [11,12]. In addition, to the best of our knowledge, there are few studies reporting the optimal frequency of B-ACT and the target groups patients that benefit most from it in SP patients undergoing IMV, especially in the ICU.
The aim of our study was to explore the benefits and risks of B-ACT in SP patients undergoing IMV in the ICU. We also want to determine the mean optimal frequency of B-ACT to some extent and special patient populations that benefit most from this new technology, knowing that it will have a positive impact on promoting the clinical application of flexible bronchoscopes and improving airway management of these critically ill patients in future.
2. Materials and Methods
2.1. Patients
Initially enrolled in this retrospective study were 868 patients diagnosed with SP during hospitalization in Shanghai Tenth People’s Hospital (Shanghai, China) from January 2020 to December 2022, of whom 230 SP patients undergoing IMV because of severe pneumonia met the major criteria of endotracheal intubation and IMV specified by the Infectious Diseases Society of America/American Thoracic Society consensus guidelines and were included for analysis [2]. We continued to screen these patients according to our exclusion criteria: (I) no ACT performed during hospitalization; (II) incomplete medical records and orders related to bronchoscopy; and (III) bronchoscopy for reasons other than airway clearance (Figure 1). Finally, 99 patients with B-ACT and 49 patients with artificial sputum aspiration were enrolled in this study.
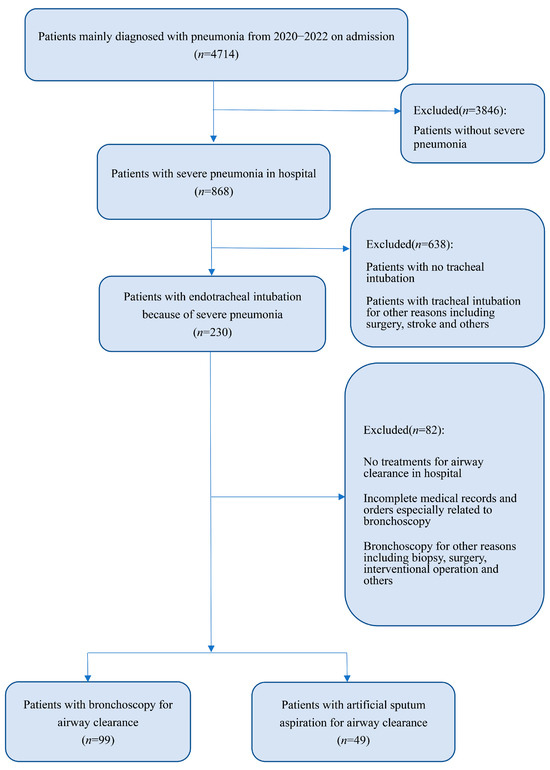
Figure 1.
Flow diagram.
2.2. Treatment Methods
In our study, the principles and procedures of bronchoscopy for patients closely followed the Chinese expert consensus on the clinical application of single-use (disposable) flexible bronchoscopes [10]. SP patients in the non-bronchoscopy group were given artificial sputum aspiration for ACT based on the systemic anti-infective and symptomatic supportive therapies according to other guidelines [9]. Artificial sputum suction was conducted by negative pressure suction under IMV. SP patients in bronchoscopy group received IMV using the flexible bronchoscopes for ACT based on the anti-infective and supportive treatments. The flexible bronchoscope clinically consists of single-use flexible bronchoscopes (SUFB) and reusable flexible bronchoscopes (RFB). Most of the flexible bronchoscopes used in this study were SUFB called H-Steriscopes (Vathin Medical Instrument Co., Ltd., Hunan, China), and the rest were RFB called V-bronchoscopes (Seesheen Medical Instrument Co., Ltd., Guangdong, China). The operation steps are as follows: Firstly, the comprehensive condition of the patients was assessed to decide whether they were able to tolerate B-ACT. Preoperative discussion and analysis were conducted according to the surgical requirements. After being fully informed of the procedure, the patients or their relatives decided to accept bronchoscopy. Secondly, patients were laid supine and sedated under continuous IMV. One side of the disposable sputum cup was connected to the bronchoscope, and the other side was connected to the negative pressure. The bronchoscope was inserted into the endotracheal tube to aspirate the visible secretions under direct version of the bronchoscope. Vital signs including oxygen saturation were monitored throughout the procedure. If necessary, 100–250 mL normal saline was used for bronchoalveolar lavage according to the patient condition. Finally, the airway condition was checked carefully before withdrawal. Airway secretion microbial cultures and drug sensitive tests were routinely carried out after bronchoscopy. Surgical records, medical records and instructions should be improved. The preoperative disease evaluation and postoperative close observation were also important to the patients.
2.3. Data Collection
Due to the retrospective nature of our study, all patients’ electronic files including physician’s order sheets, nurse’s recording sheets, blood laboratory results, lung imaging tests and daily medical records were rechecked and recorded carefully. The primary outcome measure was survival to hospital discharge. The observation indicators of our study included: (i) basic characteristics: sex, age, body mass index (BMI), length of hospitalization, duration of IMV, records of tracheotomy and outcomes of hospital discharge; (ii) bronchoscopy records: specific time, number and mean frequency; (iii) laboratory results: 3–5 mL fasting cubital venous blood and arterial blood were collected from patients of the two groups 1 day before and after the whole course of B-ACT, and the blood samples were analyzed by the specialized equipment of the hospital. The laboratory results included routine blood parameters, blood gas analysis, inflammatory factors, blood biochemical parameters, and myocardium markers.
2.4. Statistical Analysis
All analyses were performed using SPSS (version 25.0) and GraphPad Prism (version 8.0) software. The Kolmogorov–Smirnov test and Levene test were used for identifying the normality and homogeneity of variables. Categorical variables are presented as frequencies and percentages, while continuous variables are presented as the mean ± standard deviation (SD) for normally distributed variables, median and interquartile range for non-normally distributed variables. An independent group t-test was applied for normally distributed variables, while Mann–Whitney U test was used for non-normally distributed variables. Categorical variables were analyzed by the Chi-square test or Fisher’s exact test. The univariate and multivariate COX regression analysis was used to assess independent risk factors for the outcomes to hospital discharge. The difference of survival to hospital discharge between different groups were compared by the Kaplan–Meier analysis. p < 0.05 was considered statistically significant.
3. Results
3.1. Baseline Cohort Characteristics
There were no significant differences in the baseline characteristics including age, BMI, gender and commodities between the bronchoscopy and non-bronchoscopy groups (all p > 0.05) (Table 1). Next, patients in the bronchoscopy group were divided into ≤once every 3 days group (n = 50) and >once every 3 days group (n = 49) according to the mean frequency of bronchoscopy (mean frequency of bronchoscopy = days of bronchoscopy/numbers of bronchoscopies). The general characteristics of the patients were also similar in terms of age, BMI, gender and commodities between the two groups (all p > 0.05) (Table 1).

Table 1.
Baseline characteristics of SP patients undergoing IMV between different groups.
3.2. Preoperative and Postoperative Blood Laboratory Results
There were no significant differences in all routine blood parameters, blood gas analysis, inflammatory factors, blood biochemical parameters and myocardium markers before bronchoscopy between the bronchoscopy and non-bronchoscopy groups (all p > 0.05). There was significant improvement in most of the above blood laboratory results in the same group before and after B-ACT (p < 0.05) (Table 2; see Supplementary Table S1). Most importantly, the number of WBC (p < 0.001), percentage of neutrophils (N%; p = 0.001), the levels of arterial oxygen pressure (PO2; p = 0.005), oxygen saturation (SO2; p < 0.001), procalcitonin (PCT; p < 0.001) and C-reactive protein (CRP; p = 0.005) were all significantly improved in the bronchoscopy group as compared with those in the non-bronchoscopy group after B-ACT (Table 2). In addition, the levels of blood glucose (Glu; p < 0.001), urea (p = 0.037), creatinine (Cr; p < 0.001), albumin (Alb; p < 0.001), troponin I (TnI; p < 0.001), brain natriuretic peptide (BNP; p < 0.001) and D-dimer (p < 0.001) in the bronchoscopy group were also significantly better than those in the non-bronchoscopy group after B-ACT (see Supplementary Table S1). The above analysis indicated that B-ACT could help improve the function of multiple organs including lung, heart and kidney.

Table 2.
Comparisons of important laboratory results between bronchoscopy and non-bronchoscopy groups.
3.3. Comparison of Changes of Important Indicators
Furthermore, the violin plots showed that the changes of PCT (−5.43 vs. −3.96, p= 0.0059; Figure 2A) and CRP value (−109.2 vs. −73.99, p = 0.0198; Figure 2B) in the bronchoscopy group were more pronounced than those in the non-bronchoscopy group. The decline range of WBC (−6.24 vs. −3, p = 0.015; Figure 2D) and N% value (−16 vs. −6.2, p = 0.0004; Figure 2C) in the bronchoscopy group were larger than that in the non-bronchoscopy group. Also, the improvement of PO2 (19 vs. 9.6, p = 0.0108; Figure 2E) and SO2 (26.8 vs. 16.8; Figure 2F) in the bronchoscopy group was more remarkable than that in the non-bronchoscopy group.
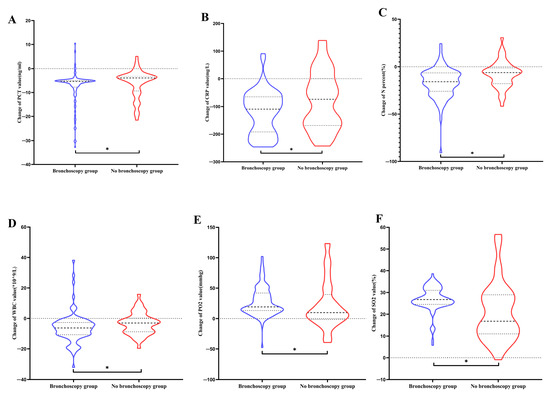
Figure 2.
The violin plots of changes of important indicators between bronchoscopy and non-bronchoscopy groups. (A) Change in PCT value. (B) Change in CRP value. (C) Change in N%. (D) Change in WBC value. (E) Change in PO2 value. (F) Change in SO2 value. Abbreviations: PCT: procalcitonin; CRP: C-reactive protein; WBC: white blood cell; N: neutrophils; PO2: arterial oxygen pressure; SO2: oxygen saturation. The asterisk represented the significant differences.
3.4. The Kaplan–Meier Analysis and Survival Curves
Survival to hospital discharge of the patients in the bronchoscopy group was significantly better than that in the non-bronchoscopy group (Logrank p < 0.001; Figure 3A). The median survival time to discharge in the bronchoscopy group was significantly better than that in the non-bronchoscopy group (38 days vs. 17 days; see Supplementary Table S2). The mortality rate in the bronchoscopy group was significantly lower than that in the bronchoscopy group at day 14, 28 and 90 of hospitalization (60.5% vs. 91.7%; 24.3% vs. 71.9%; 4.9% vs. 17.1%) (see Supplementary Table S2). According to the mean frequency of bronchoscopy, we divided the patients of the bronchoscopy group into two groups: ≤once every 3 days and >once every 3 days. The survival curves showed that survival to discharge in the ≤once every 3 days group was significantly better than that in the > once every 3 days group (Logrank p < 0.001; Figure 3B). The median survival time to discharge also significantly better in the ≤once every 3 days group than that in the >once every 3 days group (53 days vs. 26 days; see Supplementary Table S2). The mortality rate in the ≤once every 3 days group was significantly lower than that in ≤once every 3-day group at day 14, 28 and 90 of hospitalization (89.1% vs. 94%;46.3% vs. 91.8%; 3.9% vs. 26.6%) (see Supplementary Table S2). Next, we divided them into various groups according to patients’ different characteristics. In patients with cardiopulmonary or cerebrovascular diseases, as well as patients with positive cultures for bacteria, we found that the bronchoscopy group had significantly better survival outcomes than non-bronchoscopy group (all Logrank p < 0.05; see Supplementary Figure S1). Similarly, we also found that ≤once every 3 days group had significantly better survival rates than >once every 3 days group in patients with cardiopulmonary diseases, or positive cultures for bacteria (all Logrank p < 0.05; see Supplementary Figure S2).
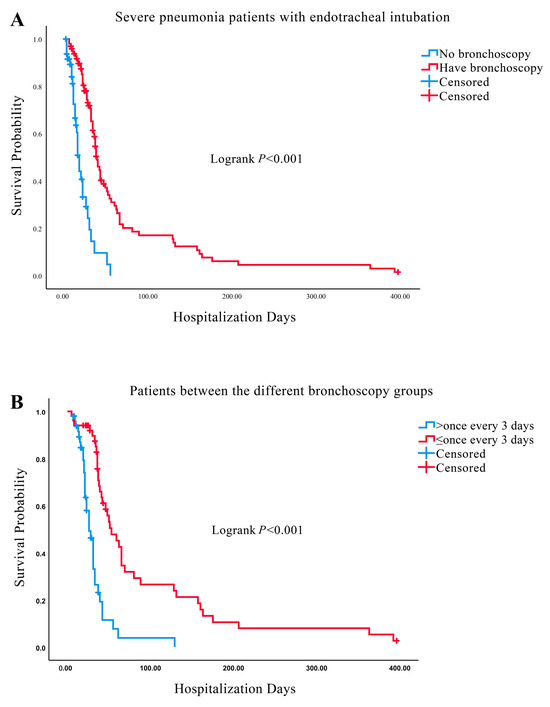
Figure 3.
Survival curves between different groups. (A) Survival curves between bronchoscopy and non-bronchoscopy groups. (B) Survival curves between ≤once every 3 days and >once every 3 days groups.
3.5. Univariate and Multivariate COX Regression Analysis
After adjusting for all covariates as confounding factors, the overall survival outcome to hospital discharge in the bronchoscopy group was significantly better than that in the non-bronchoscopy group (HR:0.444, 95% CI: 0.238–0.829, p = 0.011) (Table 3). Then, we divided the patients in the bronchoscopy group into two groups: ≤once every 3 days and >once every 3 days. After adjustment for all confounders, the overall survival outcome in the patients of the ≤once every 3 days group was significantly better than that in the once every 3 days group (HR: 0.285, 95% CI: 0.163–0.498, p < 0.001) (Table 4). In addition, the forest plots of HRs for survival to hospital discharge were generated to show the above analysis results between different groups more visually (Figure 4).

Table 3.
COX regression analysis of survival outcomes to hospital discharge in patients undergoing bronchoscopy or not.

Table 4.
COX regression analysis of survival outcomes to hospital discharge in patients undergoing bronchoscopy.
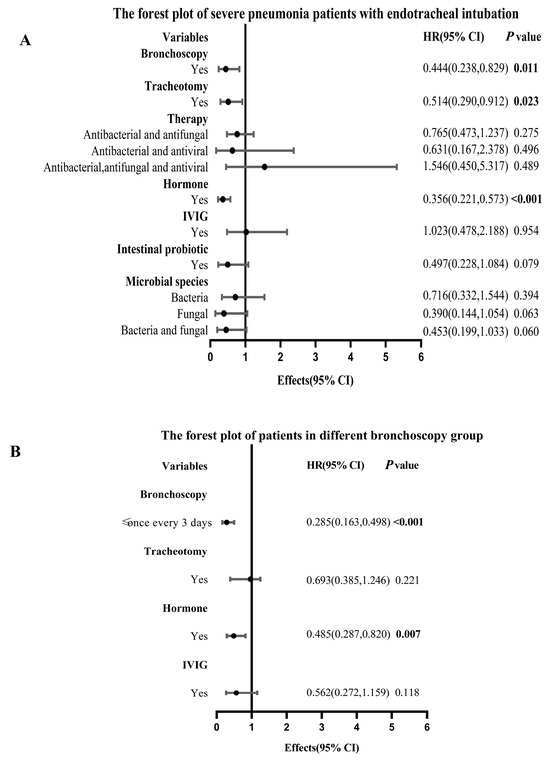
Figure 4.
Forest plots between different groups. (A) The forest plot of SP patients undergoing bronchoscopy or not during IMV. (B) The forest plot of SP patients undergoing bronchoscopy during IMV. Abbreviations: SP: severe pneumonia; IMV: invasive mechanical ventilation; IVIG: intravenous immunoglobin; HR: hazard ratio; CI: confidence interval.
4. Discussion
In this study, we used flexible bronchoscopes to perform B-ACT in SP patients undergoing IMV. The results showed that the improvement of routine blood parameters (WBC# and N%), blood gas analysis (PO2, SO2) and inflammatory factors (PCT and CRP) in the bronchoscopy group was more pronounced than that in the non-bronchoscopy group. Survival to hospital discharge in the bronchoscopy group was significantly better than that in the non-bronchoscopy group. In addition, B-ACT had significantly positive impact on the survival to discharge of these patients. Especially in the patients with cardiopulmonary diseases or positive cultures for bacteria, B-ACT group and those in ≤once every 3 days group had pronounced better survival outcomes than those in their counterpart groups. Furthermore, we also explored the mean optimal frequency of bronchoscopy for SP patients undergoing B-ACT, and found that survival to discharge in the ≤once every 3 days group was significantly better than that in the >once every 3 days group, suggesting that more frequent bronchoscopy may to some extent be related to better prognosis of these patients. To summarize, B-ACT showed encouraging effects and advantages in various aspects including improvement of laboratory results and decrease in hospital morality, and average frequency of ≤once every 3 days may be a preferred mean optimal frequency of bronchoscopy for SP patients undergoing IMV.
Some previous studies have already demonstrated that B-ACT is significantly beneficial for children with SP [13,14], but its specific effectiveness for adults with SP has long been debated. Our analysis showed that B-ACT could improve some important laboratory results including some inflammatory factors (CRP and PCT), routine blood parameters (WBC# and N%) and blood gas analysis (PO2 and SO2). Consistent with our results, a retrospective study admitting 81 SP patients with IMV reported that not only inflammation indicators including tumor necrosis factor-a (TNF-α), CRP, IL-8 and IL-6 but also blood gas indexes including PO2 and SO2 were significantly better in the bronchoalveolar lavage (BAL) group than those in the control group after bronchoscopy, in which hospital stay, IMV time, and infection control window appearance time in the observation group were significantly shorter than those in the control group after bronchoscopy (all p < 0.05) [15]. Moreover, a prospective study enrolling 103 SP patients including patients with IMV demonstrated that the changes of APACHE II scores, inflammatory indicators (CRP, TNF-αand PCT) and blood gas analysis (oxygenation index (OI), PO2 and SO2) in the bronchoscopy group were more pronounced than those in the control group after treatment, and the length of stay in ICU, IMV time and duration of antibiotics of the bronchoscopy group were shorter than those of the control group after treatment (all p < 0.05) [16]. Consistently, a randomized controlled trial recruited 100 patients including patients with SP occurring within 48 h after tracheal intubation or 48 h after extubation, and demonstrated that the interleukin-8(IL-8), CRP, and PCT levels, as well as some respiratory mechanics indexes in the bronchoscopy group, were significantly lower than those in the control group after treatment (all p < 0.05) [17]. However, another retrospective case–control study that enrolled SP 72 patients including those with IMV concluded that BAL under bronchoscopy could increase PCT levels within 24 h, and markedly decreased PCT levels after 48 h (p < 0.05), which may indicate that more long-term clinical studies were urgently needed in the impacts of B-ACT on the different laboratory results in those patients after treatment [18].
Recently, the application of bedside B-ACT has been increasingly applied to airway management of SP patients undergoing IMV in the ICU. Our study indicated that B-ACT was significantly beneficial to the survival to hospital discharge of these patients. Consistently, a retrospective study divided 1560 with SP patients undergoing IMV into the bronchoscopy group and non-bronchoscopy group, and demonstrated that bronchoscopy during IMV was associated with reducing the risk of ICU (HR: 0.33, 95% CI:0.20–0.55, p < 0.001) and in-hospital mortality (HR: 0.40, 95% CI: 0.26–0.60, p < 0.001) in these patients [19]. However, very little research has investigated the optimal time and the number or frequency of B-ACT in SP patients undergoing IMV. It was found in our study that the mean bronchoscopy frequency of ≤once every 3 days may, to some extent, better improve the survival outcome to hospital discharge than that of >once every 3 days for SP patients during IMV. A retrospective cohort study found that the in-ICU mortality and 90-day mortality in the early bronchoscopy group (bronchoscopy within 24 h after intubation) were significantly lower than those in the late bronchoscopy group (in-ICU: 4.9% vs. 24.6%; 90-day: 11.8 vs. 32.8%), and was associated with lower 90-day mortality in multivariate analysis (HR:0.412, 95% CI: 0.192–0.883, p = 0.023), indicating that early bronchoscopy benefits the clinical outcome of mechanically ventilated patients with SP [20]. However, another retrospective observational study divided 229 SP children into the IMV group and non-IMV group, as well as the early BAL group (receiving BAL within 1 day of admission) and late BAL group, and found that early BAL under bronchoscopy could not improve the survival rate but can reduce the hospitalization and ICU time, exhibiting that B-ACT is still beneficial to the prognosis of SP patients [21]. Therefore, it is still necessary to have further prospective research to explore the appropriate number, time or frequency of B-ACT for SP patients undergoing IMV, knowing that more accurate, individualized and comprehensive airway clearance management is urgently required in such patients.
Furthermore, our analysis showed that more frequent bronchoscopy groups had better survival rates in hospital than control groups in SP patients with cardiopulmonary diseases or positive cultures for bacteria during IMV, which suggested that B-ACT may be more suitable for improving prognosis of these groups of patients. A previous study had demonstrated that B-ACT can improve the therapeutic effects on chronic obstructive pulmonary disease (COPD) patients complicated with SP during IMV, which can significantly reduce the ventilation time, hospital stay, reintubation rate and fatality rate, while increasing the weaning success rate [22]. However, some other studies demonstrated that beside B-ACT is also beneficial in improving pulmonary ventilation and reducing systemic inflammatory response of pneumonia patients with cerebral ischemic or hemorrhagic stroke [23,24,25]. In addition, polymerase chain reaction (PCR) or metagenomic next-generation sequencing (mNGS) based on the fluid of BAL after bronchoscopy can provide a higher identification rate of pathogens involved in pneumonia than direct examination and culture, which would hopefully improve early diagnosis and prognosis of critically ill patients, especially those with bacterium/fungus-associated pneumonia [26,27]. Therefore, further studies are needed to investigate the impacts of B-ACT on these critically ill patients with different genders, ages, regions or other characteristics, suggesting great value in clinical application [28].
As a new technology, B-ACT has both advantages and disadvantages. The biggest advantage of B-ACT is that flexible bronchoscopy could remove sputum and other secretions in deep airways effectively, which is beneficial to reducing further airway damage and lung inflammation by halting bacterial colonization [29]. Specifically, SUFB can replace sterile devices directly without disinfection, which not only reduces the spread of pathogens through aerosols and the risk of infection, but also makes it easier to sterilize and preserve other devices such as portable screens, thus reducing the procedures and costs of cleaning and storage in hospital [10,30,31]. RFB can provide better image quality, suction, maneuverability and medical record integration, which is more extensively used for advanced diagnostic and therapeutic procedures compared to SUFB [32]. After the current COVID-19 pandemic or other infectious diseases, it is more recommended to use SUFB in the airway management of patients with pulmonary infectious diseases than in the ICU [33]. However, over-frequent B-ACT may aggravate airway damage and lung inflammation [34]. The arterial partial pressure of oxygen could drop during bronchoscopy, which may increase the risk of respiratory failure in patients with mechanical ventilation [35]. Although the bronchoscopy procedure could be safely performed, some patients still have rare adverse events such as airway edema, submucosal hemorrhage, increased secretions, bronchospasm and even dyspnea after bronchoscopy [36]. Therefore, we should not only improve the safety and efficiency of flexible bronchoscopes, but explore the optimal operation of B-ACT including the appropriate time or number according to patients’ individual conditions in the future.
There are some limitations in our study. First, this study was a single-center retrospective study, not a randomized controlled trial, which may cause analysis bias. For example, the past original records did not include some bronchoscopy details such as postoperative complications, basic vital signs during bronchoscopy, immunology factors, pulmonary function tests and others. In addition, the 148 patients may not be able to represent all SP patients with IMV, leading to limited generalizability of conclusions. However, we discussed the specific impacts of B-ACT on the different laboratory results and the survival benefits of it in a relatively large number of SP patients with IMV for the first time. Most importantly, we compared different mean frequencies of flexible bronchoscopes affecting survival to hospital discharge of these patients, and identified appropriate group patients suitable for B-ACT, which suggested that more prospective cohort studies were needed to explore individualized and precise airway management for SP patients with IMV in future.
5. Conclusions
In this study, we demonstrated that B-ACT significantly prolonged the time of survival to hospital discharge and improved many different laboratory tests, which highlights the importance of flexible bronchoscopes in the airway management for SP patients undergoing IMV in the ICU. We also observed that the mean optimal frequency of flexible bronchoscopes affected the prognosis of such patients. It is our recommendation that the mean frequency of flexible bronchoscopes be ≤ once every 3 days in that it contributed to better survival outcomes than the mean frequency of >once every 3 days. And more frequent B-ACT may be more suitable for improving diagnosis in patients with cardiopulmonary diseases or positive cultures for bacteria. Hopefully, our study could provide a novel evidence-based individualized therapeutic reference for SP patients with IMV in the ICU.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/diagnostics13203276/s1. Table S1: Comparisons of other laboratory results between the bronchoscopy group and non-bronchoscopy group. Abbreviations: ALT: alanine aminotransferase; AST: asperate aminotransferase; Cr: creatinine; Alb: albumin; TnI: troponin I; BNP: brain natriuretic peptide. Table S2: Median survival days and 14-, 28-, and 90-day of morality in hospital between different groups. Figure S1: Survival curves between bronchoscopy and non-bronchoscopy groups in patients with different characteristics. (A) Survival curves in patients with COPD. (B) Survival curves in patients with CHD. (C) Survival curves in patients with CVA. (D) Survival curves in patients with positive cultures for bacteria. (E) Survival curves in patients with positive cultures for bacteria and fungus. (F) Survival curves in patients >65 years old. Figure S2: Survival curves between ≤once every 3 days and >once every 3 days groups in patients with different characteristics. (A) Survival curves in patients with COPD. (B) Survival curves in patients with CHD. (C) Survival curves in patients with positive cultures for bacteria. (D) Survival curves in patients with positive cultures for bacteria and fungus.
Author Contributions
Conception and design: A.Y., S.X. and C.W. Acquisition of the data: A.Y., Z.L., W.H. and H.R. Analysis and interpretation of the data: all authors. Drafting of the manuscript: A.Y., S.X. and C.W. Preparing figures and tables: A.Y., S.X. and C.W. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (82272673).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics committee of the Shanghai Tenth People’s Hospital (82272673).
Informed Consent Statement
Prior approval of each patient or relative had been obtained before bronchoscopy. The need for written informed consent was waived by the ethics committee of the Shanghai Tenth People’s Hospital due to retrospective nature of the study.
Data Availability Statement
All data generated or analyzed during current study are included in this published article, and are available from the corresponding author upon reasonable request.
Acknowledgments
We would like to thank all the patients who donated their statistical data.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
SP: Severe pneumonia; IMV: invasive mechanical ventilation; ACT: airway clearance therapy; B-ACT: bronchoscopic airway clearance therapy; ICU: intensive care unit; bronchoalveolar lavage (BAL); BMI: body mass index; SUFB: single-use flexible bronchoscopes; RFB: reusable flexible bronchoscopes; COPD: chronic obstructive pulmonary disease; CVA: cerebral vascular accident; CHD: coronary heart disease; DM: diabetes mellitus; HBP: high blood pressure; PLT: platelets; WBC: white blood cell; N: neutrophils; PH: pondus hydrogenii; PCO2: partial pressure of carbon dioxide; PO2: arterial oxygen pressure; SO2: oxygen saturation; PCT: procalcitonin; CRP: C-reactive protein; HR: hazard ratio; CI: confidence interval; IVIG: intravenous immunoglobin; Glu: blood glucose; ALT: alanine aminotransferase; AST: asperate aminotransferase; Cr: creatininase; Alb: albumin; TnI: troponin I; BNP: brain natriuretic peptide; PCR: polymerase chain reaction; mNGS: metagenomic next-generation sequencing; TNF-α: tumor necrosis factor-a; OI: oxygenation index; IL-8: interleukin-8.
References
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Bhutta, Z.A. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Mandell, L.A.; Wunderink, R.G.; Anzueto, A.; Bartlett, J.G.; Campbell, G.D.; Dean, N.C.; Dowell, S.F.; File, T.M., Jr.; Musher, D.M.; Niederman, M.S.; et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2007, 44 (Suppl. 2), S27–S72. [Google Scholar] [CrossRef] [PubMed]
- Reyes, L.F.; Garcia-Gallo, E.; Pinedo, J.; Saenz-Valcarcel, M.; Celi, L.; Rodriguez, A.; Waterer, G. Scores to Predict Long-term Mortality in Patients with Severe Pneumonia Still Lacking. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2021, 72, e442–e443. [Google Scholar] [CrossRef]
- Alves, D.; Grainha, T.; Pereira, M.O.; Lopes, S.P. Antimicrobial materials for endotracheal tubes: A review on the last two decades of technological progress. Acta Biomater. 2023, 158, 32–55. [Google Scholar] [CrossRef] [PubMed]
- Cillóniz, C.; Torres, A.; Niederman, M.S. Management of pneumonia in critically ill patients. BMJ Clin. Res. Ed. 2021, 375, e065871. [Google Scholar] [CrossRef]
- Hoo, Z.H.; Daniels, T.; Wildman, M.J.; Teare, M.D.; Bradley, J.M. Airway clearance techniques used by people with cystic fibrosis in the UK. Physiotherapy 2015, 101, 340–348. [Google Scholar] [CrossRef]
- Korkmaz Ekren, P.; Basarik Aydogan, B.; Gurgun, A.; Tasbakan, M.S.; Bacakoglu, F.; Nava, S. Can fiberoptic bronchoscopy be applied to critically ill patients treated with noninvasive ventilation for acute respiratory distress syndrome? Prospective observational study. BMC Pulm. Med. 2016, 16, 89. [Google Scholar] [CrossRef] [PubMed]
- Luo, F.; Darwiche, K.; Singh, S.; Torrego, A.; Steinfort, D.P.; Gasparini, S.; Liu, D.; Zhang, W.; Fernandez-Bussy, S.; Herth, F.J.F.; et al. Performing Bronchoscopy in Times of the COVID-19 Pandemic: Practice Statement from an International Expert Panel. Respir. Int. Rev. Thorac. Dis. 2020, 99, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flanders, S.A.; et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef] [PubMed]
- Respiratory Branch of the Chinese Medical Association; Respiratory Endoscopy Committee of the Chinese Medical Association. Expert consensus on the clinical application of single-use (disposable) flexible bronchoscopes. Chin. J. Tuberc. Respir. Dis. 2023, 46, 41–48. [Google Scholar] [CrossRef]
- Karbasy, S.H.; Sabertanha, A.; Bayati, M.; Meshkini, A.; Fatemeh Shakhs Emampour, B. Study of the effect of added bronchoscopic suction to routine treatment of ventilator associated pneumonia patients in surgical ICU. J. Pak. Med. Assoc. 2021, 71, 1326–1331. [Google Scholar] [CrossRef]
- Zhao, H.; Gu, H.; Liu, T.; Ge, J.; Shi, G. Analysis of curative effect of adjuvant therapy with bronchoalveolar lavage on COPD patients complicated with pneumonia. Exp. Ther. Med. 2018, 16, 3799–3804. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Zhao, H.R.; Wei, H.L.; Chen, C.; Qiu, R.X.; Ren, X.L.; Zhang, L.; Gao, Y.Q. Efficacy of Bronchoalveolar Lavage as Adjunct Therapy in the Treatment of Neonatal Severe Pneumonia: A Prospective Case-Control Study. J. Trop. Pediatr. 2020, 66, 528–533. [Google Scholar] [CrossRef] [PubMed]
- Pei, M.; Jiang, P.; Wang, T.; Xia, C.; Hou, R.; Sun, A.; Zou, H. Effect of bronchoalveolar lavage on the clinical efficacy, inflammatory factors, and immune function in the treatment of refractory pneumonia in children. Transl. Pediatr. 2021, 10, 921–928. [Google Scholar] [CrossRef]
- Wang, C.; Ye, S.; Wang, X.; Zhao, Y.; Ma, Q.; Wang, L. Clinical Efficacy and Safety of Mechanical Ventilation Combined with Fiberoptic Bronchoalveolar Lavage in Patients with Severe Pulmonary Infection. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 5401–5407. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Li, Z.; Cheng, W.; Zhang, B.; Zhu, W.; Lin, Z. Application of sputum suction by fiberoptic bronchoscope in patients with severe pneumonia and its effect on inflammatory factors. Am. J. Transl. Res. 2021, 13, 8409–8414. [Google Scholar]
- Wu, L.; Liu, B. The clinical effect of a bronchofiberscope in treating severe ventilator-associated pneumonia. Am. J. Transl. Res. 2021, 13, 6966–6972. [Google Scholar]
- Li, L.; Zhang, M.; Wei, Y.; Tu, X.; Lu, Z.; Cheng, Y. Clinical significance of procalcitonin in critically ill patients with pneumonia receiving bronchoalveolar lavage. Sarcoidosis Vasc. Diffus. Lung Dis. Off. J. WASOG 2022, 39, e2022031. [Google Scholar] [CrossRef]
- Zhang, L.; Li, S.; Yuan, S.; Lu, X.; Li, J.; Liu, Y.; Huang, T.; Lyu, J.; Yin, H. The Association between Bronchoscopy and the Prognoses of Patients with Ventilator-Associated Pneumonia in Intensive Care Units: A Retrospective Study Based on the MIMIC-IV Database. Front. Pharmacol. 2022, 13, 868920. [Google Scholar] [CrossRef]
- Lee, H.W.; Min, J.; Park, J.; Lee, Y.J.; Kim, S.J.; Park, J.S.; Yoon, H.I.; Lee, J.H.; Lee, C.T.; Cho, Y.J. Clinical impact of early bronchoscopy in mechanically ventilated patients with aspiration pneumonia. Respirology 2015, 20, 1115–1122. [Google Scholar] [CrossRef]
- Wu, X.; Lu, W.; Sang, X.; Xu, Y.; Wang, T.; Zhan, X.; Hao, J.; Ren, R.; Zeng, H.; Li, S. Timing of bronchoscopy and application of scoring tools in children with severe pneumonia. Ital. J. Pediatr. 2023, 49, 44. [Google Scholar] [CrossRef]
- Qiao, Z.; Yu, J.; Yu, K.; Zhang, M. The benefit of daily sputum suction via bronchoscopy in patients of chronic obstructive pulmonary disease with ventilators: A randomized controlled trial. Medicine 2018, 97, e11631. [Google Scholar] [CrossRef]
- Han, Q.; Chen, C.; Fu, R.; Tan, L.; Xia, L. Portable fibrobronchoscopic treatment for non-severe ischemic stroke-associated pneumonia patients with dysphagia: A pilot study. Neurol. Res. 2019, 41, 216–222. [Google Scholar] [CrossRef]
- Han, Q.; Chen, C.; Hu, H.Q.; Shen, J.; Yang, G.; Chen, B.; Xia, L. Effect evaluation on use of bedside fiber bronchoscope in treating stroke-associated pneumonia. Top. Stroke Rehabil. 2018, 25, 459–466. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Zhao, L.; Li, J.; Shi, J. Clinical effect of antibiotic combined with fiber bronchoscope perfusion in treatment of pneumonia after severe cerebral hemorrhage. Medicine 2022, 101, e30675. [Google Scholar] [CrossRef] [PubMed]
- Baudel, J.L.; Tankovic, J.; Dahoumane, R.; Carrat, F.; Galbois, A.; Ait-Oufella, H.; Offenstadt, G.; Guidet, B.; Maury, E. Multiplex PCR performed of bronchoalveolar lavage fluid increases pathogen identification rate in critically ill patients with pneumonia: A pilot study. Ann. Intensive Care 2014, 4, 35. [Google Scholar] [CrossRef]
- Chen, H.; Bai, X.; Gao, Y.; Liu, W.; Yao, X.; Wang, J. Profile of Bacteria with ARGs Among Real-World Samples from ICU Admission Patients with Pulmonary Infection Revealed by Metagenomic NGS. Infect. Drug Resist. 2021, 14, 4993–5004. [Google Scholar] [CrossRef]
- Zhou, W.; Zhou, C.; Liu, X.; Shi, N.; Quyang, W.; Tu, D.; Xin, Y.; Ji, L. A randomised trial on the therapeutic effectiveness of bronchoalveolar lavage under fiberoptic bronchoscopy in patients with severe lung infection living in the Tibetan plateau area. Ann. Palliat. Med. 2021, 10, 3336–3342. [Google Scholar] [CrossRef]
- Lee, D.H.; Driver, B.E.; Prekker, M.E.; Puskarich, M.A.; Plummer, D.; Mojica, E.Y.; Smith, J.C.; DeVries, P.A.; Stang, J.L.; Reardon, R.F. Bronchoscopy in the emergency department. Am. J. Emerg. Med. 2022, 58, 114–119. [Google Scholar] [CrossRef]
- Mouritsen, J.M.; Ehlers, L.; Kovaleva, J.; Ahmad, I.; El-Boghdadly, K. A systematic review and cost effectiveness analysis of reusable vs. single-use flexible bronchoscopes. Anaesthesia 2020, 75, 529–540. [Google Scholar] [CrossRef] [PubMed]
- Châteauvieux, C.; Farah, L.; Guérot, E.; Wermert, D.; Pineau, J.; Prognon, P.; Borget, I.; Martelli, N. Single-use flexible bronchoscopes compared with reusable bronchoscopes: Positive organizational impact but a costly solution. J. Eval. Clin. Pract. 2018, 24, 528–535. [Google Scholar] [CrossRef] [PubMed]
- Ho, E.; Wagh, A.; Hogarth, K.; Murgu, S. Single-Use and Reusable Flexible Bronchoscopes in Pulmonary and Critical Care Medicine. Diagnostics 2022, 12, 174. [Google Scholar] [CrossRef]
- Barron, S.P.; Kennedy, M.P. Single-Use (Disposable) Flexible Bronchoscopes: The Future of Bronchoscopy? Adv. Ther. 2020, 37, 4538–4548. [Google Scholar] [CrossRef]
- Ergan, B.; Nava, S. The use of bronchoscopy in critically ill patients: Considerations and complications. Expert Rev. Respir. Med. 2018, 12, 651–663. [Google Scholar] [CrossRef]
- Pelaia, C.; Bruni, A.; Garofalo, E.; Rovida, S.; Arrighi, E.; Cammarota, G.; Navalesi, P.; Pelaia, G.; Longhini, F. Oxygenation strategies during flexible bronchoscopy: A review of the literature. Respir. Res. 2021, 22, 253. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.M.; Arenberg, D.A.; Barjaktarevic, I.; Bhatt, S.P.; Bowler, R.P.; Christenson, S.A.; Couper, D.J.; Dransfield, M.T.; Han, M.K.; Hoffman, E.A.; et al. Safety and Tolerability of Comprehensive Research Bronchoscopy in Chronic Obstructive Pulmonary Disease. Results from the SPIROMICS Bronchoscopy Substudy. Ann. Am. Thorac. Soc. 2019, 16, 439–446. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).