The Effect of TMJ Intervention on Instant Postural Changes and Dystonic Contractions in Patients Diagnosed with Dystonia: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
- Subjects between the ages of 18 and 75;
- Subjects who have referred to the clinic with complaints of bruxism and/or myofascial pain;
- Subjects who have received a diagnosis of dystonia by a neurology specialist;
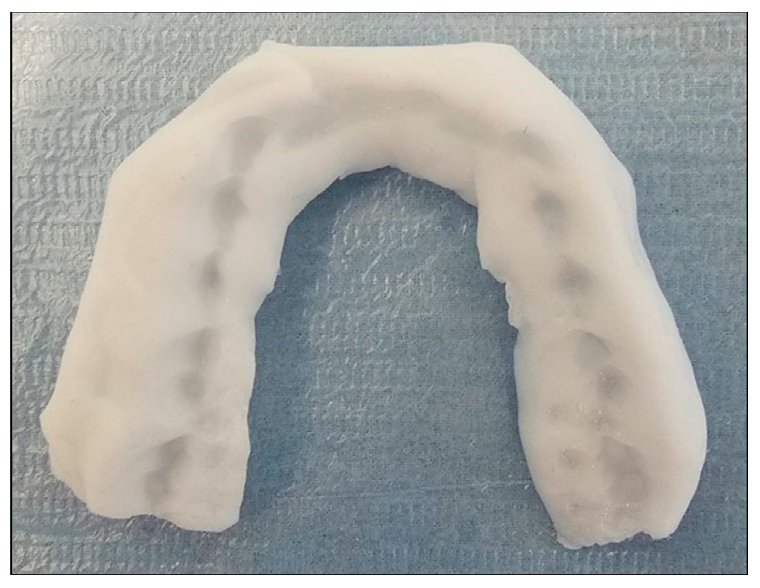
- Subjects who have started bruxism and TMJ treatment with the first phase of IDTT;
- Subjects with complete records related to postural assessment before and after intervention.
- Congenital anomaly;
- Incomplete photograph and video records;
- Subjects who received botox treatment within the last 4 months;
- Subjects who started or quit a new medication for the treatment of dystonia within 1 month.
2.1. Measurement Method
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hayashi, H.; Fujita, T.; Shirakura, M.; Tsuka, Y.; Fujii, E.; Terao, A.; Tanimoto, K. Role of articular disc in condylar regeneration of the mandible. Exp. Anim. 2014, 63, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Yadav, U.; Ahmed, J.; Ongole, R.; Shenoy, N.; Sujir, N.; Natarajan, S. Influence of psychosocial factors and parafunctional habits in temporomandibular disorders: A cross-sectional study. Perm. J. 2020, 24, 144. [Google Scholar] [CrossRef] [PubMed]
- Sójka, A.; Stelcer, B.; Roy, M.; Mojs, E.; Pryliński, M. Is there a relationship between psychological factors and TMD? Brain Behav. 2019, 9, e01360. [Google Scholar] [CrossRef] [PubMed]
- Santana-Mora, U.; López-Cedrún, J.; Suárez-Quintanilla, J.; Varela-Centelles, P.; Mora, M.J.; Da Silva, J.L.; Figueiredo-Costa, F.; Santana-Penín, U. Asymmetry of dental or joint anatomy or impaired chewing function contribute to chronic temporomandibular joint disorders. Ann. Anat. 2021, 238, 151793. [Google Scholar] [CrossRef]
- Manfredini, D.; Lombardo, L.; Siciliani, G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: End of an era? J. Oral Rehabil. 2017, 44, 908–923. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Perez, D.; Ellis III, E. Do patients with malocclusion have a higher prevalence of temporomandibular disorders than controls both before and after orthognathic surgery? A systematic review and meta-analysis. J. Craniomaxillofac. Surg. 2017, 45, 1716–1723. [Google Scholar] [CrossRef]
- Macrì, M.; Murmura, G.; Scarano, A.; Festa, F. Prevalence of temporomandibular disorders and its association with malocclusion in children: A transversal study. Front. Public Health 2022, 10, 860833. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Perinetti, G.; Guarda-Nardini, L. Dental malocclusion is not related to temporomandibular joint clicking: A logistic regression analysis in a patient population. Angle Orthod. 2014, 84, 310–315. [Google Scholar] [CrossRef]
- Medina, A.; Nilles, C.; Martino, D.; Pelletier, C.; Pringsheim, T. The Prevalence of Idiopathic or Inherited Isolated Dystonia: A Systematic Review and Meta-Analysis. Mov. Disord. Clin. Pract. 2022, 9, 860–868. [Google Scholar] [CrossRef]
- Grütz, K.; Klein, C. Dystonia updates: Definition, nomenclature, clinical classification, and etiology. J. Neural Transm. 2021, 128, 395–404. [Google Scholar] [CrossRef]
- Albanese, A.; Di Giovanni, M.; Lalli, S. Dystonia: Diagnosis and management. Eur. J. Neurol. 2019, 26, 5–17. [Google Scholar] [CrossRef]
- Pastorelli, F.; Pasquetti, P. Biomechanical analysis and rehabilitation in athletes. Clin. Cases Miner Bone Metab. 2013, 10, 96. [Google Scholar]
- Salkar, R.G.; Radke, U.M.; Deshmukh, S.P.; Radke, P.M. Relationship between temporomandibular joint disorders and body posture. Int. J. Dent. Health Sci. 2015, 2, 1523–1530. [Google Scholar]
- Fiorillo, L. Spine and TMJ: A Pathophysiology report. J. Funct. Morphol. Kinesiol. 2020, 5, 24. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L.; Musumeci, G. TMJ dysfunction and systemic correlation. J. Funct. Morphol. Kinesiol. 2020, 5, 20. [Google Scholar] [CrossRef] [PubMed]
- Sheskin, D.J. Handbook of Parametric and Nonparametric Statistical Procedures, 3rd ed.; Chapman and Hall/CRC Press: London, UK, 2003; pp. 1–1193. [Google Scholar]
- Paus, S.; Gross, J.; Moll-Müller, M.; Hentschel, F.; Spottke, A.; Wabbels, B.; Klockgether, T.; Abele, M. Impaired sleep quality and restless legs syndrome in idiopathic focal dystonia: A controlled study. J. Neurol. 2011, 258, 1835–1840. [Google Scholar] [CrossRef]
- Watts, M.W.; Tan, E.K.; Jankovic, J. Bruxism and cranial-cervical dystonia: Is there a relationship? Cranio 1999, 17, 196–201. [Google Scholar] [CrossRef]
- Singer, C.; Papapetropoulos, S. A comparison of jaw-closing and jaw-opening idiopathic oromandibular dystonia. Park. Relat. Disord. 2006, 12, 115–118. [Google Scholar] [CrossRef]
- Machado, N.A.G.; Costa, Y.M.; Quevedo, H.M.; Stuginski-Barbosa, J.; Valle, C.M.; Bonjardim, L.R.; Garib, D.G.; Conti, P.C.R. The association of self-reported awake bruxism with anxiety, depression, pain threshold at pressure, pain vigilance, and quality of life in patients undergoing orthodontic treatment. J. Appl. Oral Sci. 2020, 28, e20190407. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R. Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications. J. Am. Dent. Assoc. 2016, 147, 438–445. [Google Scholar] [CrossRef]
- Lavigne, G.J.; Montplaisir, J.V. Bruxism: Epidemiology, diagnosis, pathophysiology, and pharmacology. In Orofacial Pain and Temporomandibular Disorders: Advances in Pain Research and Therapy, 1st ed.; Fricton, J.R., Dubner, R., Eds.; Raven Press: New York, NY, USA, 1995; Volume 21, pp. 387–404. [Google Scholar]
- Iacob, S.M.; Chisnoiu, A.M.; Lascu, L.M.; Berar, A.M.; Studnicska, D.; Fluerasu, M.I. Is PostureScreen® Mobile app an accurate tool for dentists to evaluate the correlation between malocclusion and posture? Cranio 2020, 38, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.G.L.; Montezuma, T.; Perez, C.S.; Sverzut, C.E.; Trivellato, A.E.; de Oliveira Guirro, E.C. Body postural realignment in the first 2 months after orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 2021, 159, e281–e290. [Google Scholar] [CrossRef] [PubMed]
- Welling, A.; Gurudut, P.; Shirodkar, G.; Shetye, N.; Khan, S. Validation of non-radiographic APECS software in comparison with standard radiographic measurement of full-length lower limb hip-knee-ankle angle in elderly obese women. Physiother. Q. 2023, 31, 90–94. [Google Scholar] [CrossRef]
- Comella, C.L.; Leurgans, S.; Wuu, J.; Stebbins, G.T.; Chmura, T.; Dystonia Study Group. Rating scales for dystonia: A multicenter assessment. Mov. Disord. 2003, 18, 303–312. [Google Scholar] [CrossRef]
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 6th ed.; Elsevier: St. Louis, MO, USA, 1989. [Google Scholar]
- Seifeldin, S.A.; Elhayes, K.A. Soft versus hard occlusal splint therapy in the management of temporomandibular disorders (TMDs). Saudi Dent. J. 2015, 27, 208–214. [Google Scholar] [CrossRef]
- Okeson, J.P. The effects of hard and soft occlusal splints on nocturnal bruxism. J. Am. Dent. Assoc. 1987, 114, 788–791. [Google Scholar] [CrossRef]
- Harkins, S.; Marteney, J.L.; Cueva, O.; Cueva, L. Application of soft occlusal splints in patients suffering from clicking temporomandibular joints. Cranio 1988, 6, 71–76. [Google Scholar] [CrossRef]
- Benli, M.; Özcan, M. Short-term effect of material type and thickness of occlusal splints on maximum bite force and sleep quality in patients with sleep bruxism: A randomized controlled clinical trial. Clin. Oral Investig. 2023, 27, 4313–4322. [Google Scholar] [CrossRef]
- Kolcakoglu, K.; Dogan, S.; Tulga Oz, F.; Aydınbelge, M. A comparison of hard and soft occlusal splints for the treatment of nocturnal bruxism in children using the BiteStrip®. J. Clin. Pediatr. Dent. 2022, 46, 219–224. [Google Scholar] [CrossRef]
- Lei, Q.; Lin, D.; Liu, Y.; Lin, K.; Huang, W.; Wu, D. Neuromuscular and occlusion analysis to evaluate the efficacy of three splints on patients with bruxism. BMC Oral Health 2023, 23, 325. [Google Scholar] [CrossRef]
- Todić, J.T.; Mitić, A.; Lazić, D.; Radosavljević, R.; Staletović, M. Effects of bruxism on the maximum bite force. Vojn. Pregl. 2017, 74, 138–144. [Google Scholar] [CrossRef]
- Navrotchi, C.; Badea, M.E. The influence of occlusal stabilization appliances on cervical dystonia symptoms. Clujul Med. 2017, 90, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Nomoto, S.; Nakamura, M.; Sato, T.; Hisanaga, R. Occlusal treatment with bite splint improves dyskinesia in Parkinson’s disease patient: A case report. Bull. Tokyo Dent. Coll. 2013, 54, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Sims, A.B.; Stack, B.C.; Demerjian, G.G. Spasmodic torticollis: The dental connection. Cranio 2012, 30, 188–193. [Google Scholar] [CrossRef]
- Raine, S.; Twomey, L.T. Head and Shoulder Posture Variations in 160 Asymptomatic Women and Men. Arch. Phys. Med. Rehabil. 1997, 78, 1215–1223. [Google Scholar] [CrossRef]
- Trovato, B.; Roggio, F.; Sortino, M.; Zanghì, M.; Petrigna, L.; Giuffrida, R.; Musumeci, G. Postural Evaluation in Young Healthy Adults through a Digital and Reproducible Method. J. Funct. Morphol. Kinesiol. 2022, 7, 98. [Google Scholar] [CrossRef]
- Alkhateeb, A.M.; Daher, N.S.; Forrester, B.J.; Martin, B.D.; Jaber, H.M. Effects of adjustments to wheelchair seat to back support angle on head, neck, and shoulder postures in subjects with cerebral palsy. Assist. Technol. 2021, 33, 326–332. [Google Scholar] [CrossRef]
- Nemmers, T.M.; Miller, J.W.; Hartman, M.D. Variability of the forward head posture in healthy community-dwelling older women. J. Geriatr. Phys. Ther. 2009, 32, 10–14. [Google Scholar] [CrossRef]
- Ruivo, R.M.; Pezarat-Correia, P.; Carita, A.I. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Braz. J. Phys. Ther. 2014, 18, 364–371. [Google Scholar] [CrossRef]
- Herrington, L. Assessment of the degree of pelvic tilt within a normal asymptomatic population. Man. Ther. 2011, 16, 646–648. [Google Scholar] [CrossRef]
- Medina McKeon, J.M.; Hertel, J. Sex differences and representative values for 6 lower extremity alignment measures. J. Athl. Train. 2009, 44, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J. Bone Jt. Surg. Am. 2005, 87, 260–267. [Google Scholar] [CrossRef]
- Nguyen, A.D.; Shultz, S.J. Sex differences in clinical measures of lower extremity alignment. J. Orthop. Sports Phys. Ther. 2007, 37, 389–398. [Google Scholar] [CrossRef] [PubMed]
- Alizadeh, S.; Mattes, K. How anterior pelvic tilt affects the lower extremity kinematics during the late swing phase in soccer players while running: A time series analysis. Hum. Mov. Sci. 2019, 66, 459–466. [Google Scholar] [CrossRef] [PubMed]
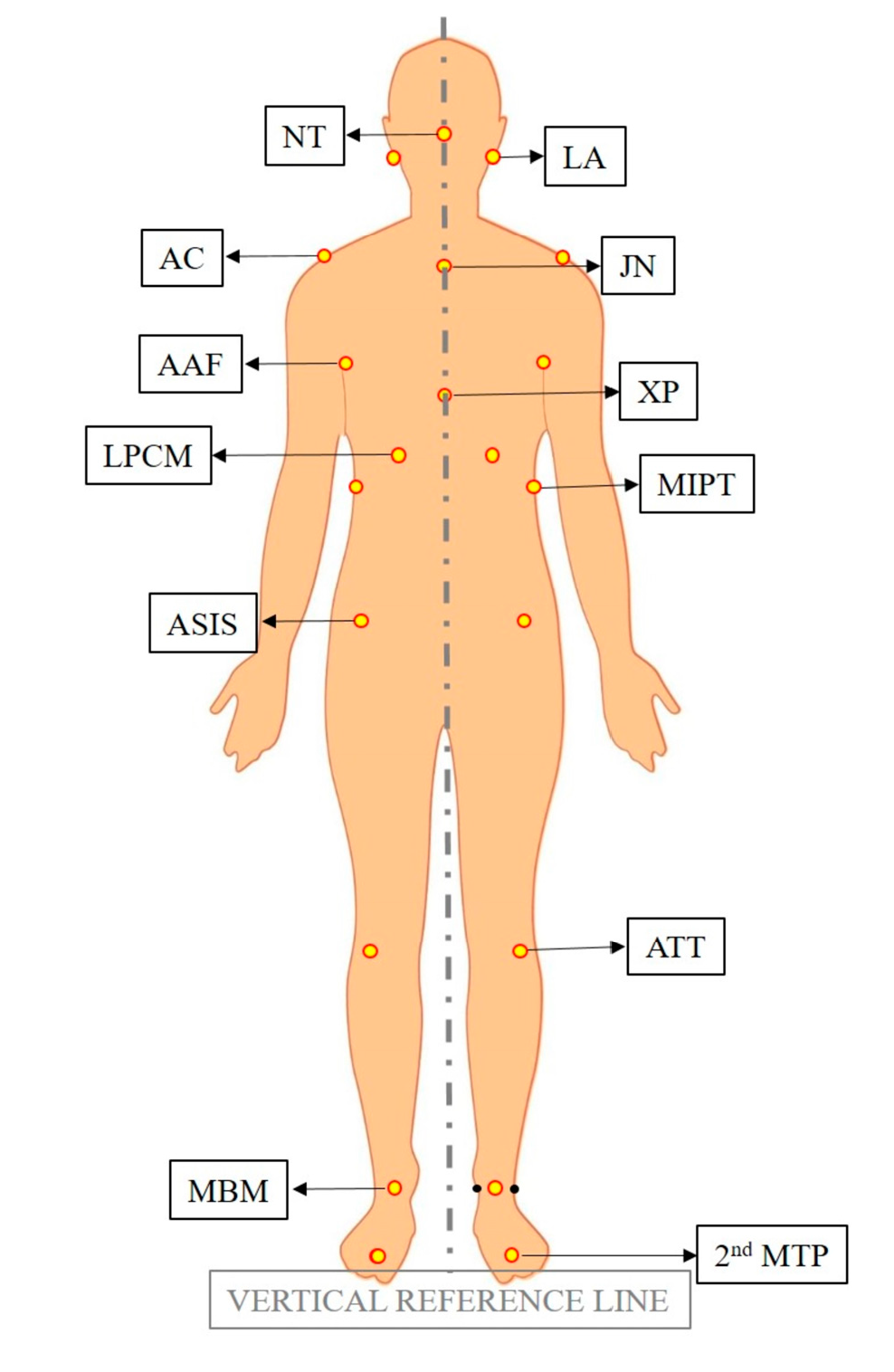


| Landmark | Abbreviation | Description |
|---|---|---|
| Lobulus auriculae | LA | The lowest part of the ear. |
| Nose tip | NT | The tip of the nose. |
| Acromion | AC | The outer end of the scapula, extending over the shoulder joint and forming the highest point of the shoulder to which the clavicle is attached. |
| Jugular notch | JN | The largest visible dip in between the neck and the two clavicles in the superior margin of the sternum. |
| Anterior axillary fold | AAF | The ridge of the skin-covered inferior border of the pectoralis major muscle along the anterior sides of the chest where the underside of each arm meets the shoulder. |
| Xiphoid process | XP | The pointed process of the cartilage at the lowest part of the sternum. |
| Lowest point of costal margin | LPCM | The most intended point on the contour of the torso inferiorly. |
| Most intended point of the trunk | MIPT | The most intended point on the contour of the torso laterally. |
| ASIS | ASIS | The prominence at the anterior projection of the iliac crest. |
| Anterior tibial tuberosity | ATT | The large oblong elevation on the proximal anterior aspect of the tibia. |
| Midpoint between malleoli | MBM | A midpoint of the line joining the most prominent bone on the outer side of the ankle and the most prominent bone on the inner side of the ankle. |
| Second metatarsophalangeal joint | 2nd MTP | The joint between the metatarsal bone of the foot and the second proximal phalange. |
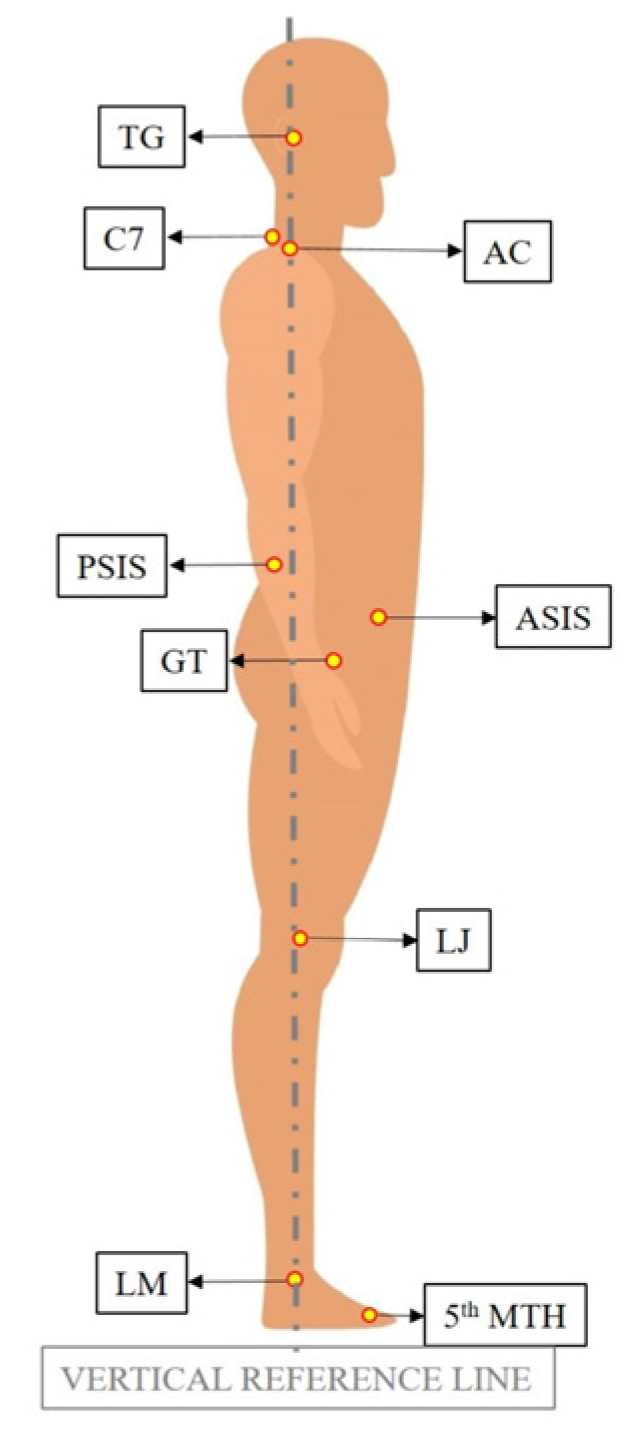
| Landmark | Abbreviation | Description |
|---|---|---|
| Tragus | TG | A small pointed prominence of the external ear, situated in front of the ear canal. |
| C7 vertebra | C7 | The most visible protrusion at the base of the neck. |
| Acromion | AC | The outer end of the scapula, extending over the shoulder joint and forming the highest point of the shoulder, to which the clavicle is attached. |
| ASIS | ASIS | The prominence at the anterior projection of the iliac crest. |
| PSIS | PSIS | The dimples between the buttocks and waist. |
| Greater trochanter | GT | A large protrusion located toward the top part of the shaft of the femur, facing outward. |
| Lateral joint | LJ | A slightly rounded enlargement on the surface of the knee. |
| Lateral malleolus | LM | The most prominent bone on the outer side of the ankle. |
| Head of the 5th metatarsal bone | 5th MTH | A point at the prominence of the long bone (palpable along the distal outer edges of the feet) that connects the fifth proximal phalange to tarsal bone. |
| Parameter | Abbreviation | Description |
|---|---|---|
| Body Alignment Frontal | BAF | The angle formed between the vertical reference line and the line passing through the JN and the midpoint between the MBM points on the right and left sides. |
| Head Tilt | HT | The angle formed by the horizontal reference plane and the line joining the LA right and the LA left. |
| Shoulder Alignment | SAF | The angle formed by the horizontal reference plane and the line joining the AC right and the AC left. |
| Axillae Alignment | AA | The angle formed by the horizontal reference plane and the line joining the AAF right and the AAF left. |
| Ribcage Tilt | RT | The angle formed by the horizontal reference plane and the line joining the LPCM right and the LPCM left. |
| Most intended point of the trunk Tilt | MIPTT | The angle formed by the horizontal reference plane and the line joining the MIPT right and the MIIPT left. |
| Pelvic Tilt Frontal | PTF | The angle formed by the horizontal reference plane and the line joining the ASIS right and the ASIS left. |
| Right Knee Angle | KAR | The acute angle formed between the line connecting the ASIS right and the ATT right, as well as the line connecting the ATT right and the MBM right. |
| Left Knee Angle | KAL | The acute angle formed between the line connecting the ASIS left and the ATT left, as well as the line connecting the ATT left and the MBM left. |
| Right Foot Rotation | FRR | The angle between the vertical reference line passing through the MBM right and the line connecting the MBM right and the 2nd MTP right. |
| Left Foot Rotation | FRL | The angle between the vertical reference line passing through the MBM left and the line connecting the MBM left and the 2nd MTP left. |
| Parameter | Abbreviation | Description |
|---|---|---|
| Body Alignment Lateral | BAL | The angle between the vertical reference line and the line connecting the LM and TG points. |
| Head Shift | HS | The angle between the vertical reference line and the line connecting the C7 and TG points. |
| Shoulder Angle | SAL | The angle between the horizontal reference line and the line connecting the C7 and AC points.. |
| Pelvic Tilt Lateral | PTL | The acute angle between the horizontal reference line and the line connecting the ASIS and PSIS points. |
| Knee Angle | KA | The acute angle between the vertical reference line and the line connecting the GT and LJ points. |
| Tibia Angle | TA | The acute angle between the vertical reference line and the line connecting the LJ and LM points. |
| Foot Angle | FA | The angle between the horizontal reference line and the line connecting the LM and 5th MTH points. |
| Intra-Class Correlation | 95% Confidence Interval | F Test with True Value 0 | |||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | Value | df1 | ||
| Average Measures | 90.4% | 0.860 | 0.935 | 10.434 | 107 |
| N | % | Age | Height | Weight | |||||
|---|---|---|---|---|---|---|---|---|---|
| Range | Mean | S.D | Mean | S.D. | Mean | S.D. | |||
| Female | 8 | 66.67% | 26–60 | 42.8 | 12.8 | 164 | 4.5 | 66.0 | 13.2 |
| Male | 4 | 33.33% | 26–49 | 39 | 10 | 173.5 | 2.6 | 72.3 | 6.1 |
| Total | 12 | 100% | 26–60 | 41.5 | 11.6 | 167.2 | 6 | 68.1 | 11.4 |
| N | Range | Minimum | Maximum | Mean | S.D. | ||
|---|---|---|---|---|---|---|---|
| Statistic | Std. Error | Statistic | |||||
| Severity of Dystonic Contraction-SDC-Pre | 12 | 60.00 | 0.00 | 60.00 | 45.67 | 5.47 | 18.97 |
| Severity of Dystonic Contraction-SDC-Post | 12 | 26.00 | 0.00 | 26.00 | 12.17 | 2.53 | 8.78 |
| Body Alignment Frontal-BAF-Pre | 12 | 2.00 | 1.00 | 3.00 | 1.42 | 0.19 | 0.67 |
| Body Alignment Frontal-BAF-Post | 12 | 1.00 | 0.00 | 1.00 | 0.08 | 0.08 | 0.29 |
| Head Tilt-HT-Pre | 12 | 24.00 | 1.00 | 25.00 | 9.92 | 2.04 | 7.06 |
| Head Tilt-HT-Post | 12 | 4.00 | 0.00 | 4.00 | 1.25 | 0.41 | 1.42 |
| Shoulder Alignment-SAF-Pre | 12 | 9.00 | 0.00 | 9.00 | 2.83 | 0.73 | 2.52 |
| Shoulder Alignment-SAF-Post | 12 | 2.00 | 0.00 | 2.00 | 0.33 | 0.19 | 0.65 |
| Axillae Alignment-AA-Pre | 12 | 10.00 | 0.00 | 10.00 | 2.75 | 0.84 | 2.90 |
| Axillae Alignment-AA-Post | 12 | 2.00 | 0.00 | 2.00 | 0.58 | 0.19 | 0.67 |
| Ribcage Tilt-RT-Pre | 12 | 6.00 | 0.00 | 6.00 | 1.50 | 0.49 | 1.68 |
| Ribcage Tilt-RT-Post | 12 | 3.00 | 0.00 | 3.00 | 0.83 | 0.32 | 1.12 |
| Most intended point of the trunk Tilt-MIPTT-Pre | 12 | 3.00 | 0.00 | 3.00 | 0.83 | 0.32 | 1.12 |
| Most intended point of the trunk Tilt-MIPTT-Post | 12 | 1.00 | 0.00 | 1.00 | 0.42 | 0.15 | 0.52 |
| Pelvic Tilt Frontal-PTF-Pre | 12 | 5.00 | 0.00 | 5.00 | 2.33 | 0.50 | 1.72 |
| Pelvic Tilt Frontal-PTF-Post | 12 | 2.00 | 0.00 | 2.00 | 0.83 | 0.24 | 0.84 |
| Right Knee Angle-KAR-Pre | 12 | 11.00 | 1.00 | 12.00 | 6.75 | 0.85 | 2.96 |
| Right Knee Angle-KAR-Post | 12 | 11.00 | 1.00 | 12.00 | 6.67 | 0.87 | 3.03 |
| Left Knee Angle-KAL-Pre | 12 | 11.00 | 3.00 | 14.00 | 6.75 | 1.03 | 3.57 |
| Left Knee Angle-KAL-Post | 12 | 10.00 | 3.00 | 13.00 | 6.50 | 0.10 | 3.45 |
| Right Foot Rotation-FRR-Pre | 12 | 36.00 | −8.00 | 28.00 | 5.75 | 2.44 | 8.43 |
| Right Foot Rotation-FRR-Post | 12 | 21.00 | 0.00 | 21.00 | 5.92 | 1.60 | 5.53 |
| Left Foot Rotation-FRL-Pre | 12 | 25.00 | −7.00 | 18.00 | 5.92 | 2.15 | 7.44 |
| Left Foot Rotation-FRL-Post | 12 | 21.00 | 0.00 | 21.00 | 6.25 | 1.89 | 6.54 |
| Body Alignment Lateral-BAL-Pre | 12 | 7.00 | 1.00 | 8.00 | 3.58 | 0.65 | 2.23 |
| Body Alignment Lateral-BAL-Post | 12 | 3.00 | 0.00 | 3.00 | 1.00 | 0.30 | 1.05 |
| Head Shift-HS-Pre | 12 | 80.00 | 29.00 | 109.00 | 49.75 | 6.18 | 21.41 |
| Head Shift-HS-Post | 12 | 26.00 | 21.00 | 47.00 | 36.17 | 2.06 | 7.13 |
| Shoulder Angle-SAL-Pre | 12 | 53.00 | 6.00 | 59.00 | 23.83 | 4.40 | 15.23 |
| Shoulder Angle-SAL-Post | 12 | 47.00 | 18.00 | 65.00 | 39.42 | 4.00 | 13.85 |
| Pelvic Tilt Lateral-PTL-Pre | 12 | 12.00 | 9.00 | 21.00 | 13.25 | 1.03 | 3.57 |
| Pelvic Tilt Lateral-PTL-Post | 12 | 11.00 | 6.00 | 17.00 | 11.75 | 0.91 | 3.14 |
| Knee Angle-KA-Pre | 12 | 6.00 | 0.00 | 6.00 | 3.42 | 0.57 | 1.98 |
| Knee Angle-KA-Post | 12 | 5.00 | 0.00 | 5.00 | 2.92 | 0.48 | 1.68 |
| Tibia Angle-TA-Pre | 12 | 10.00 | 1.00 | 11.00 | 5.75 | 0.83 | 2.86 |
| Tibia Angle-TA-Post | 12 | 9.00 | 0.00 | 9.00 | 4.75 | 0.77 | 2.67 |
| Foot Angle-FA-Pre | 12 | 22.00 | 16.00 | 38.00 | 28.25 | 1.92 | 6.65 |
| Foot Angle-FA-Post | 12 | 18.00 | 17.00 | 35.00 | 27.58 | 1.75 | 6.05 |
| Total N | Test Statistic | Standard Error | Standardized Test Statistic | Asymptotic Sig. (2-Sided Test) | ||
|---|---|---|---|---|---|---|
| Severity of Dystonic Contraction-SDC | 12 | 0.000 | 11.247 | −2.934 | 0.003 * | |
| Frontal View | Body Alignment Frontal-BAF | 12 | 0.000 | 10.909 | −3.025 | 0.002 * |
| Head Tilt-HT | 12 | 0.000 | 11.242 | −2.936 | 0.003 * | |
| Shoulder Alignment-SAF | 12 | 0.000 | 9.753 | −2.820 | 0.005 * | |
| Axillae Alignment-AA | 12 | 2.000 | 9.753 | −2.615 | 0.009 * | |
| Ribcage Tilt-RT | 12 | 0.000 | 4.500 | −2.333 | 0.020 * | |
| Most intended point of the trunk Tilt-MIPTT | 12 | 2.000 | 3.623 | −1.518 | 0.129 | |
| Pelvic Tilt Frontal-PTF | 12 | 0.000 | 9.657 | −2.848 | 0.004 * | |
| Right Knee Angle-KAR | 12 | 4.000 | 2.646 | −0.378 | 0.705 | |
| Left Knee Angle-KAL | 12 | 0.000 | 1.732 | −1.732 | 0.083 | |
| Right Foot Rotation-FRR | 12 | 4.000 | 2.739 | −0.365 | 0.715 | |
| Left Foot Rotation-FRL | 12 | 13.500 | 7.045 | −0.639 | 0.523 | |
| Lateral View | Body Alignment Lateral-BAL | 12 | 0.000 | 11.164 | −2.956 | 0.003 * |
| Head Shift-HS | 12 | 0.000 | 12.723 | −3.065 | 0.002 * | |
| Shoulder Angle-SAL | 12 | 66.000 | 11.247 | 2.934 | 0.003 * | |
| Pelvic Tilt Lateral-PTL | 12 | 6.000 | 9.657 | −2.226 | 0.026 * | |
| Knee Angle-KA | 12 | 0.000 | 4.287 | −2.449 | 0.014 * | |
| Tibia Angle-TA | 12 | 0.000 | 8.147 | −2.762 | 0.006 * | |
| Foot Angle-FA | 12 | 8.000 | 8.016 | −1.809 | 0.070 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akbulut, A.S. The Effect of TMJ Intervention on Instant Postural Changes and Dystonic Contractions in Patients Diagnosed with Dystonia: A Pilot Study. Diagnostics 2023, 13, 3177. https://doi.org/10.3390/diagnostics13203177
Akbulut AS. The Effect of TMJ Intervention on Instant Postural Changes and Dystonic Contractions in Patients Diagnosed with Dystonia: A Pilot Study. Diagnostics. 2023; 13(20):3177. https://doi.org/10.3390/diagnostics13203177
Chicago/Turabian StyleAkbulut, Ayse Selenge. 2023. "The Effect of TMJ Intervention on Instant Postural Changes and Dystonic Contractions in Patients Diagnosed with Dystonia: A Pilot Study" Diagnostics 13, no. 20: 3177. https://doi.org/10.3390/diagnostics13203177
APA StyleAkbulut, A. S. (2023). The Effect of TMJ Intervention on Instant Postural Changes and Dystonic Contractions in Patients Diagnosed with Dystonia: A Pilot Study. Diagnostics, 13(20), 3177. https://doi.org/10.3390/diagnostics13203177






