Contemporary Features and Management of Endocarditis
Abstract
:1. Introduction
2. Etiology
3. Epidemiology
4. Clinical Features
5. Evaluation and Diagnosis
6. Native Valve Endocarditis
7. Prosthetic Valve Endocarditis
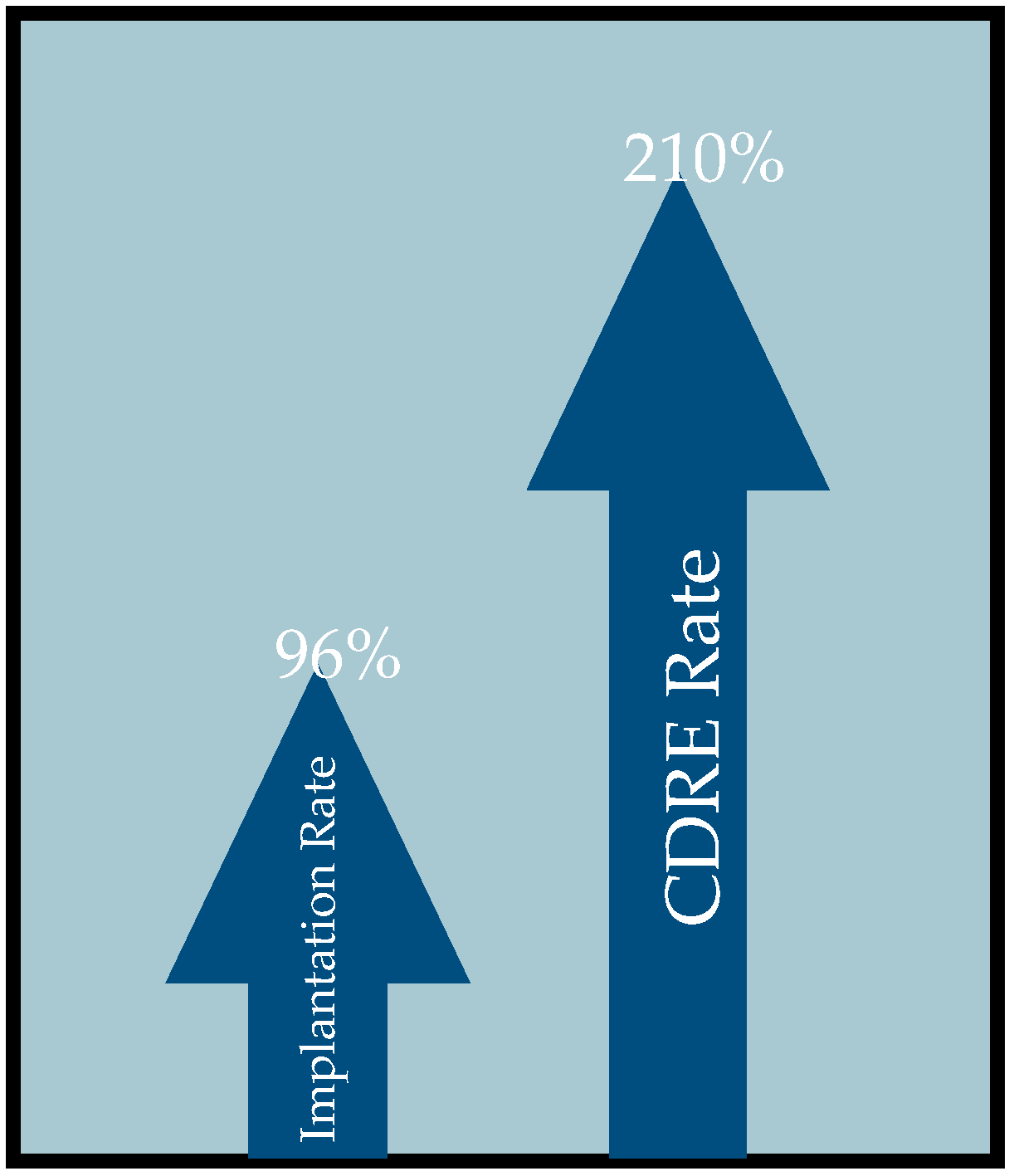
8. Cardiac Device-Related Endocarditis
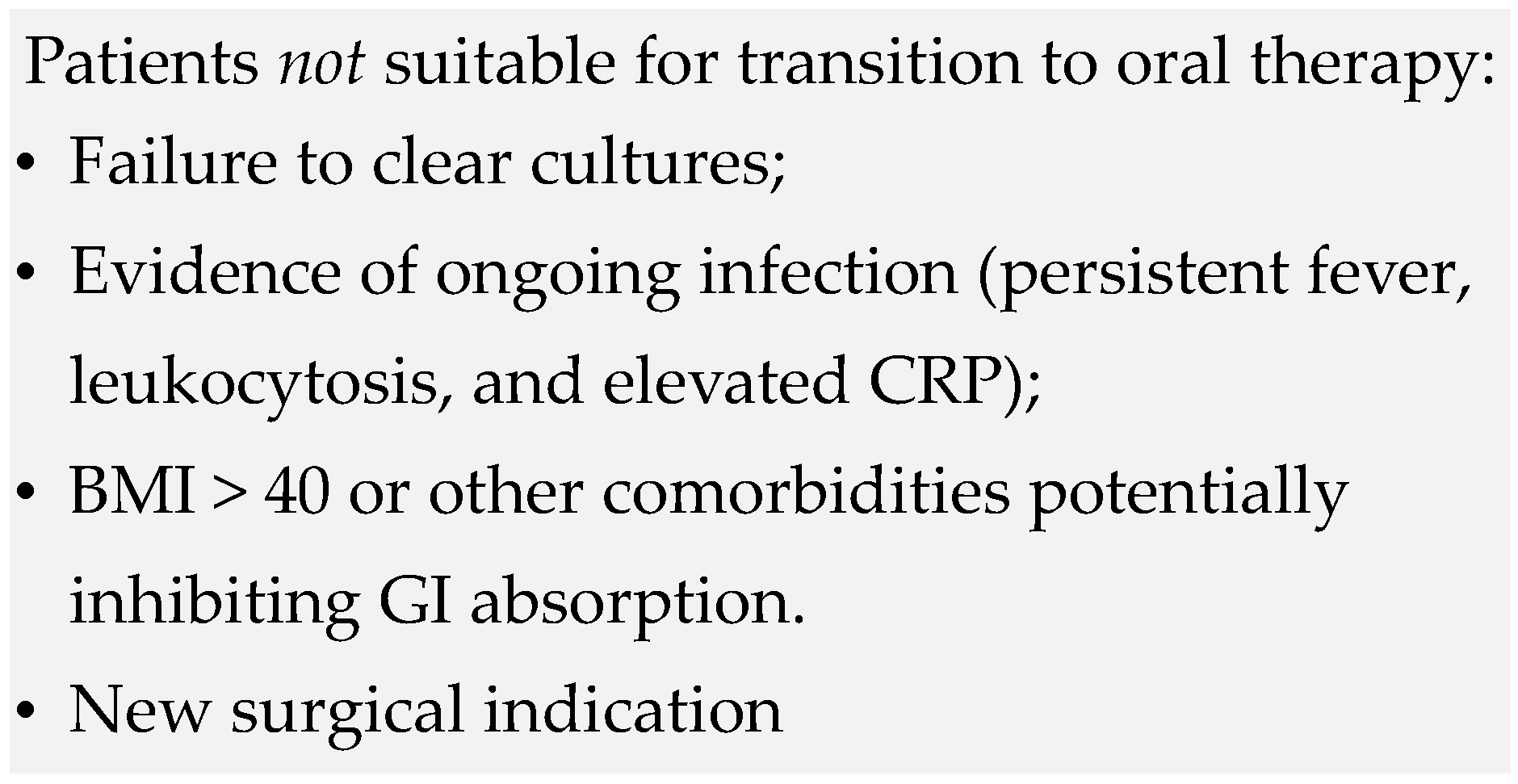
9. Management
10. Conclusions
11. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Slipczuk, L.; Codolosa, J.N.; Davila, C.D.; Romero-Corral, A.; Yun, J.; Pressman, G.S.; Figueredo, V.M. Infective Endocarditis Epidemiology Over Five Decades: A Systematic Review. PLoS ONE 2013, 9, e111564. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Athan, E.; Pappas, P.A.; Fowler, V.G., Jr.; Olaison, L.; Paré, C.; Almirante, B.; Muñoz, P.; Rizzi, M.; Naber, C.; et al. Contemporary Clinical Profile and Outcome of Prosthetic Valve Endocarditis. JAMA J. Am. Med. Assoc. 2007, 297, 1354–1361. [Google Scholar] [CrossRef]
- Cresti, A.; Chiavarelli, M.; Scalese, M.; Nencioni, C.; Valentini, S.; Guerrini, F.; D’Aiello, I.; Picchi, A.; De Sensi, F.; Habib, G. Epidemiological and mortality trends in infective endocarditis, a 17-year population-based prospective study. Cardiovasc. Diagn Ther. 2017, 7, 27–35. [Google Scholar] [CrossRef]
- Cahill, T.J.; Prendergast, B.D. Infective endocarditis. Lancet. 2016, 387, 882–893. [Google Scholar] [CrossRef]
- Pant, S.; Patel, N.J.; Deshmukh, A.; Golwala, H.; Patel, N.; Badheka, A.; Hirsch, G.A.; Mehta, J.L. Trends in Infective Endocarditis Incidence, Microbiology, and Valve Replacement in the United States From 2000 to 2011. J. Am. Coll. Cardiol. 2015, 65, 2070–2076. [Google Scholar] [CrossRef] [PubMed]
- Otto, C.M.; Nishimura, R.A.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P., III; Gentile, F.; Jneid, H.; Krieger, E.V.; Mack, M.; McLeod, C.; et al. 2020 ACC/AHA Guideline for the Management of Patients with Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 2021, 143, e72–e227. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zhan, Y.; Zhang, K.; Gao, Y.; Chen, L.; Zhan, J.; Chen, Z.; Zeng, Z. The Global, Regional, and National Burden and Trends of Infective Endocarditis From 1990 to 2019: Results from the Global Burden of Disease Study 2019. Front. Med. 2022, 9, 774224. [Google Scholar] [CrossRef]
- Selton-Suty, C.; Célard, M.; Le Moing, V.; Doco-Lecompte, T.; Chirouze, C.; Iung, B.; Strady, C.; Revest, M.; Vandenesch, F.; Bouvet, A.; et al. Preeminence of Staphylococcus aureus in Infective Endocarditis: A 1-Year Population-Based Survey. Clin. Infect. Dis. 2012, 54, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Tleyjeh, I.M.; Abdel-Latif, A.; Rahbi, H.; Scott, C.G.; Bailey, K.R.; Steckelberg, J.M.; Wilson, W.R.; Baddour, L.M. A Systematic Review of Population-Based Studies of Infective Endocarditis. Chest 2007, 132, 1025–1035. [Google Scholar] [CrossRef]
- Baddour, L.M.; Wilson, W.R.; Bayer, A.S.; Fowler, V.G.J.; Tleyjeh, I.M.; Rybak, M.J.; Barsic, B.; Lockhart, P.B.; Gewitz, M.H.; Levison, M.E.; et al. Infective endocarditis in adults: Diagnosis, antimicrobial therapy, and management of complications: A scientific statement for healthcare professionals from the American Heart. Association. Circulation 2015, 132, 1435–1486. [Google Scholar] [CrossRef]
- Chambers, H.F.; Bayer, A.S. Native-Valve Infective Endocarditis. N. Engl. J. Med. 2020, 383, 567–576. [Google Scholar] [CrossRef]
- Murdoch, D.R.; Corey, G.R.; Hoen, B.; Miro, J.M.; Fowler, V.G., Jr.; Bayer, A.S.; Karchmer, A.W.; Olaison, L.; Pappas, P.A.; Moreillon, P.; et al. International Collaboration on Endocarditis-Prospective Cohort Study (ICE-PCS) Investigators. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: The International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern. Med. 2009, 169, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Saby, L.; Laas, O.; Habib, G.; Cammilleri, S.; Mancini, J.; Tessonnier, L.; Casalta, J.P.; Gouriet, F.; Riberi, A.; Avierinos, J.F.; et al. Positron emission tomography/computed tomography for diagnosis of prosthetic valve endocarditis: Increased valvular 18F-fluorodeoxyglucose uptake as a novel major criterion. J. Am. Coll. Cardiol. 2013, 61, 2374–2382. [Google Scholar] [CrossRef] [PubMed]
- Eder, M.D.; Upadhyaya, K.; Park, J.; Ringer, M.; Malinis, M.; Young, B.D.; Sugeng, L.; Hur, D.J. Multimodality Imaging in the Diagnosis of Prosthetic Valve Endocarditis: A Brief Review. Front. Cardiovasc. Med. 2021, 8, 750573. [Google Scholar] [CrossRef]
- Pizzi, M.N.; Roque, A.; Fernández-Hidalgo, N.; Cuéllar-Calabria, H.; Ferreira-González, I.; Gonzàlez-Alujas, M.T.; Oristrell, G.; Gracia-Sánchez, L.; González, J.J.; Rodríguez-Palomares, J.; et al. Improving the Diagnosis of Infective Endocarditis in Prosthetic Valves and Intracardiac Devices with 18F-Fluordeoxyglucose Positron Emission Tomography/Computed Tomography Angiography. Circulation 2015, 132, 1113–1126. [Google Scholar] [CrossRef] [PubMed]
- Hadji-Turdeghal, K.; Jensen, A.D.; Bruun, N.E.; Iversen, K.K.; Bundgaard, H.; Smerup, M.; Kober, L.; Østergaard, L.; Fosbøl, E.L. Temporal trends in the incidence of infective endocarditis in patients with a prosthetic heart valve. Open Heart 2023, 10, e002269. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, N.; Chikwe, J.; Itagaki, S.; Gelijns, A.C.; Adams, D.H.; Egorova, N.N. Trends in Infective Endocarditis in California and New York State, 1998–2013. JAMA 2017, 317, 1652–1660. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Burner, K.D.; Fealey, M.E.; Edwards, W.D.; Tazelaar, H.D.; Orszulak, T.A.; Wright, A.J.; Baddour, L.M. Prosthetic valve endocarditis: Clinicopathological correlates in 122 surgical specimens from 116 patients (1985–2004). Cardiovasc. Pathol. 2011, 20, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Luciani, N.; Mossuto, E.; Ricci, D.; Luciani, M.; Russo, M.; Salsano, A.; Pozzoli, A.; Pierri, M.D.; D’Onofrio, A.; Chiariello, G.A.; et al. Prosthetic valve endocarditis: Predictors of early outcome of surgical therapy. A multicentric study. Eur. J. Cardio-Thorac. Surg. 2017, 52, 768–774. [Google Scholar] [CrossRef] [PubMed]
- Summers, M.R.; Leon, M.B.; Smith, C.R.; Kodali, S.K.; Thourani, V.H.; Herrmann, H.C.; Makkar, R.R.; Pibarot, P.; Webb, J.G.; Leipsic, J.; et al. Prosthetic Valve Endocarditis After TAVR and SAVR. Circulation 2019, 140, 1984–1994. [Google Scholar] [CrossRef]
- Dilsizian, V.; Budde, R.P.J.; Chen, W.; Mankad, S.V.; Lindner, J.R.; Nieman, K. Best Practices for Imaging Cardiac Device–Related Infections and Endocarditis. JACC Cardiovasc. Imaging 2022, 15, 891–911. [Google Scholar] [CrossRef]
- Greenspon, A.J.; Patel, J.D.; Lau, E.; Ochoa, J.A.; Frisch, D.R.; Ho, R.T.; Pavri, B.B.; Kurtz, S.M. 16-Year Trends in the Infection Burden for Pacemakers and Implantable Cardioverter-Defibrillators in the United States. J. Am. Coll. Cardiol. 2011, 58, 1001–1006. [Google Scholar] [CrossRef]
- Han, H.C.; Hawkins, N.M.; Pearman, C.M.; Birnie, D.H.; Krahn, A.D. Epidemiology of cardiac implantable electronic device infections: Incidence and risk factors. EP Eur. 2021, 23 (Suppl. S4), iv3–iv10. [Google Scholar] [CrossRef] [PubMed]
- Polyzos, K.A.; Konstantelias, A.A.; Falagas, M.E. Risk factors for cardiac implantable electronic device infection: A systematic review and meta-analysis. EP Eur. 2015, 17, 767–777. [Google Scholar] [CrossRef] [PubMed]
- Defaye, P.; Carabelli, A. Lead Extraction of Infected Cardiovascular Implantable Devices: The Sooner, the Better? JACC Clin. Electrophysiol. 2021, 7, 764–766. [Google Scholar] [CrossRef] [PubMed]
- Duval, X.; Delahaye, F.; Alla, F.; Tattevin, P.; Obadia, J.-F.; Le Moing, V.; Doco-Lecompte, T.; Celard, M.; Poyart, C.; Strady, C.; et al. Temporal trends in infective endocarditis in the context of prophylaxis guideline modifications: Three successive population-based surveys. J. Am. Coll. Cardiol. 2012, 59, 1968–1976. [Google Scholar] [CrossRef]
- Calais, J.; Touati, A.; Grall, N.; Laouénan, C.; Benali, K.; Mahida, B.; Vigne, J.; Hyafil, F.; Iung, B.; Duval, X.; et al. Diagnostic Impact of 18F-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography and White Blood Cell SPECT/Computed Tomography in Patients with Suspected Cardiac Implantable Electronic Device Chronic Infection. Circ. Cardiovasc. Imaging 2019, 12, e007188. [Google Scholar] [CrossRef]
- Bensimhon, L.; Lavergne, T.; Hugonnet, F.; Mainardi, J.-L.; Latremouille, C.; Maunoury, C.; Lepillier, A.; Le Heuzey, J.-Y.; Faraggi, M. Whole body [18F]fluorodeoxyglucose positron emission tomography imaging for the diagnosis of pacemaker or implantable cardioverter defibrillator infection: A preliminary prospective study. Clin. Microbiol. Infect. 2011, 17, 836–844. [Google Scholar] [CrossRef]
- Ploux, S.; Riviere, A.; Amraoui, S.; Whinnett, Z.; Barandon, L.; Lafitte, S.; Ritter, P.; Papaioannou, G.; Clementy, J.; Jais, P.; et al. Positron emission tomography in patients with suspected pacing system infections may play a critical role in difficult cases. Heart Rhythm 2011, 8, 1478–1481. [Google Scholar] [CrossRef]
- Sarrazin, J.-F.; Philippon, F.; Tessier, M.; Guimond, J.; Molin, F.; Champagne, J.; Nault, I.; Blier, L.; Nadeau, M.; Charbonneau, L.; et al. Usefulness of Fluorine-18 Positron Emission Tomography/Computed Tomography for Identification of Cardiovascular Implantable Electronic Device Infections. J. Am. Coll. Cardiol. 2012, 59, 1616–1625. [Google Scholar] [CrossRef]
- Delgado, V.; Marsan, N.A.; de Waha, S.; Bonaros, N.; Brida, M.; Burri, H.; Caselli, S.; Doenst, T.; Ederhy, S.; Erba, P.A.; et al. 2023 ESC Guidelines for the management of endocarditis: Developed by the task for on the management of endocarditis of the European Society of Cardiology (ESC) Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), andthe European Association of Nuclear Medicine (EANM). Eur. Heart J. 2023. [Google Scholar] [CrossRef]
- Oliveira, M.; Guittet, L.; Hamon, M.; Hamon, M. Comparative Value of Cardiac CT and Transesophageal Echocardiography in Infective Endocarditis: A Systematic Review and Meta-Analysis. Radiol. Cardiothorac. Imaging. 2020, 2, e190189. [Google Scholar] [CrossRef]
- Habets, J.; Tanis, W.; Reitsma, J.B.; van den Brink, R.B.A.; Mali, W.P.T.M.; Chamuleau, S.A.J.; Budde, R.P.J. Are novel non-invasive imaging techniques needed in patients with suspected prosthetic heart valve endocarditis? A systematic review and meta-analysis. Eur. Radiol. 2015, 25, 2125–2133. [Google Scholar] [CrossRef]
- Feuchtner, G.M.; Stolzmann, P.; Dichtl, W.; Schertler, T.; Bonatti, J.; Scheffel, H.; Mueller, S.; Plass, A.; Mueller, L.; Bartel, T.; et al. Multislice Computed Tomography in Infective Endocarditis: Comparison with Transesophageal Echocardiography and Intraoperative Findings. J. Am. Coll. Cardiol. 2009, 53, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.-P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC) Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 2015, 36, 3075–3128. [Google Scholar] [CrossRef]
- Bin Abdulhak, A.A.; Baddour, L.M.; Erwin, P.J.; Hoen, B.; Chu, V.H.; Mensah, G.A.; Tleyjeh, I.M. Global and Regional Burden of Infective Endocarditis, 1990–2010: A Systematic Review of the Literature. Glob. Heart 2014, 9, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Davis, A.P. Adding Fuel to the Fire: Infective Endocarditis and the Challenge of Cerebrovascular Complications. Curr. Cardiol. Rep. 2023, 25, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Ambrosioni, J.; Hernandez-Meneses, M.; Téllez, A.; Pericàs, J.; Falces, C.; Tolosana, J.M.; Vidal, B.; Almela, M.; Quintana, E.; Llopis, J.; et al. The Changing Epidemiology of Infective Endocarditis in the Twenty-First Century. Curr. Infect. Dis. Rep. 2017, 19, 21. [Google Scholar] [CrossRef]
- AATS Surgical Treatment of Infective Endocarditis Consensus Guidelines Writing Committee. 2016 The American Association for Thoracic Surgery (AATS) consensus guidelines: Surgical treatment of infective endocarditis: Executive summary. J. Thorac. Cardiovasc. Surg. 2017, 153, 1241–1258.e29. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.; Erba, P.A.; Iung, B.; Donal, E.; Cosyns, B.; Laroche, C.; Popescu, B.A.; Prendergast, B.; Tornos, P.; Sadeghpour, A.; et al. Clinical presentation, aetiology and outcome of infective endocarditis: Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: A prospective cohort study. Eur. Heart J. 2019, 40, 3222–3232. [Google Scholar] [CrossRef]
- Krahn, A.D.; Longtin, Y.; Philippon, F.; Birnie, D.H.; Manlucu, J.; Angaran, P.; Rinne, C.; Coutu, B.; Low, R.A.; Essebag, V.; et al. Prevention of Arrhythmia Device Infection Trial. J. Am. Coll. Cardiol. 2018, 72, 3098–3109. [Google Scholar] [CrossRef] [PubMed]
- Andrew, V.; Alaa, S.; Samir, S. Rising Rates of Cardiac Rhythm Management Device Infections in the United States: 1996 through 2003. J. Am. Coll. Cardiol. 2006, 48, 590–591. [Google Scholar] [CrossRef]
- Dai, M.; Cai, C.; Vaibhav, V.; Sohail, M.R.; Hayes, D.L.; Hodge, D.O.; Tian, Y.; Asirvatham, R.; Cochuyt, J.J.; Huang, C.; et al. Trends of Cardiovascular Implantable Electronic Device Infection in 3 Decades. JACC Clin. Electrophysiol. 2019, 5, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- Downey, B.C.; Juselius, W.E.; Pandian, N.G.; Estes, N.A., III; Link, M.S. Incidence and Significance of Pacemaker and Implantable Cardioverter-Defibrillator Lead Masses Discovered during Transesophageal Echocardiography. Pacing Clin. Electrophysiol. 2011, 34, 679–683. [Google Scholar] [CrossRef]
- Mohammadreza, H.S.; Guy, R.; Ihsan, K.M.; Jennifer, G. NRJ Safety and In-Hospital Outcomes of Transvenous Lead Extraction for Cardiac Implantable Device–Related Infections. JACC Clin. Electrophysiol. 2019, 5, 1450–1458. [Google Scholar] [CrossRef]
- Lee, J.Z.; Majmundar, M.; Kumar, A.; Thakkar, S.; Patel, H.P.; Sorajja, D.; Valverde, A.M.; Kalra, A.; Cha, Y.-M.; Mulpuru, S.K.; et al. Impact of timing of transvenous lead removal on outcomes in infected cardiac implantable electronic devices. Heart Rhythm 2022, 19, 768–775. [Google Scholar] [CrossRef]
- Viganego, F.; O’Donoghue, S.; Eldadah, Z.; Shah, M.H.; Rastogi, M.; Mazel, J.A.; Platia, E.V. Effect of Early Diagnosis and Treatment with Percutaneous Lead Extraction on Survival in Patients with Cardiac Device Infections. Am. J. Cardiol. 2012, 109, 1466–1471. [Google Scholar] [CrossRef] [PubMed]
- Rajani, R.; Klein, J.L. Infective endocarditis: A contemporary update. Clin. Med. 2020, 20, 31. [Google Scholar] [CrossRef]
- Iversen, K.; Ihlemann, N.; Gill, S.U.; Madsen, T.; Elming, H.; Jensen, K.T.; Bruun, N.E.; Høfsten, D.E.; Fursted, K.; Christensen, J.J.; et al. Partial Oral versus Intravenous Antibiotic Treatment of Endocarditis. N. Engl. J. Med. 2018, 380, 415–424. [Google Scholar] [CrossRef]
- Pries-Heje, M.M.; Wiingaard, C.; Ihlemann, N.; Gill, S.U.; Bruun, N.E.; Elming, H.; Povlsen, J.A.; Madsen, T.; Jensen, K.T.; Fursted, K.; et al. Five-Year Outcomes of the Partial Oral Treatment of Endocarditis (POET) Trial. N. Engl. J. Med. 2022, 386, 601–602. [Google Scholar] [CrossRef]
- Anders, P.; Victoria, F.; Svensson Gunnar, S.J. Surgical Treatment for Infective Endocarditis: A Single-Centre Experience. Thorac. Cardiovasc. Surg. 2017, 65, 166–173. [Google Scholar] [CrossRef]
- Kang, D.-H.; Kim, Y.-J.; Kim, S.-H.; Sun, B.J.; Kim, D.-H.; Yun, S.-C.; Song, J.-M.; Choo, S.J.; Chung, C.-H.; Song, J.-K.; et al. Early Surgery versus Conventional Treatment for Infective Endocarditis. N. Engl. J. Med. 2012, 366, 2466–2473. [Google Scholar] [CrossRef] [PubMed]
- Baddour, L.M.; Epstein, A.E.; Erickson, C.C.; Knight, B.P.; Levison, M.E.; Lockhart, P.B.; Masoudi, F.A.; Okum, E.J.; Wilson, W.R.; Beerman, L.B.; et al. Update on cardiovascular implantable electronic device infections and their management: A scientific statement from the american heart association. Circulation 2010, 121, 458–477. [Google Scholar] [CrossRef]
- Calderón-Parra, J.; Kestler, M.; Ramos-Martínez, A.; Bouza, E.; Valerio, M.; de Alarcón, A.; Luque, R.; Goenaga, M.Á.; Echeverría, T.; Fariñas, M.C.; et al. Clinical factors associated with reinfection versus relapse in infective endocarditis: Prospective cohort study. J. Clin. Med. 2021, 10, 748. [Google Scholar] [CrossRef] [PubMed]
| Pathogen | Recommended Therapy |
|---|---|
| Native Valve | |
| VGS and Streptococcus gallolyticus (bovis) PCN susceptible | Penicillin G 12–18 million U/24 h IV either continuously or in 4 or 6 equally divided doses for 4 weeks OR Ceftriaxone 2 g/24 h IV/IM in 1 dose for 4 weeks. Alternatively Penicillin G 12–18 million U/24 h IV either continuously or in 6 equally divided doses for 2 weeks or Ceftriaxone 2 g/24 h IV/IM in 1 dose for 2 weeks PLUS Gentamicin 3 mg/kg/24 h IV or IM in 1 dose for 2 weeks and vancomycin 30 mg/kg/24 h IV in 2 equally divided doses) |
| VGS and Streptococcus gallolyticus (bovis) PCN resistant | Penicillin G 24 million u/24 h IV either continuously or in 4–6 equally divided doses for 4 weeks PLUS Gentamicin 3 mg/kg per 24 h IV or IM in 1 dose for 2 weeks AND vancomycin 30 mg/kg/24 h IV in 2 equally divided doses for 4 weeks |
| Staphylococcus methicillin-susceptible | Nafcillin or oxacillin 12 g/24 h in 4–6 equally divided doses for 6 weeks (complicated right-sided and left-sided IE; 2 weeks for uncomplicated right-sided) OR cefazolin 6 g/24 h IV in 3 equally divided doses (if anaphylactoid hypersensitivity to β-lactams use vancomycin). |
| Staphylococcus methicillin-resistant | Vancomycin 30 mg/kg/24 h in 2 equally divided doses for 6 weeks OR daptomycin ≥8 mg/kg/dose for 6 weeks. |
| Enterococcus susceptible to penicillin and gentamicin | Ampicillin 2 g IV every 4 h for 4 weeks (sx < 3 months) or 6 weeks (sx >3 months) OR Penicillin G 18–30 million U/24 h IV either continuously or in 6 equally divided doses for 4 weeks PLUS Gentamicin 3 mg/kg ideal body weight in 2–3 equally divided doses. An alternative regimen is double β-lactam Ampicillin 2 g IV every 4 h for 6 weeks PLUS Ceftriaxone 2 g every 12 h for 6 weeks (recommended for patients with creatinine clearance < 50 mL/min). |
| Enterococcus susceptible to penicillin and resistant to Aminoglycosides or Streptomycin-Susceptible Gentamicin-Resistant | Double β-lactam Ampicillin 2 g IV every 4 h PLUS Ceftriaxone 2 g IV every 12 h for 6 weeks. Alternative for Streptomycin-Susceptible Gentamicin-Resistant includes Ampicillin 2 g every 4 h for 4 weeks OR Penicillin G 18–30 million U/24 h IV either continuously or in 6 equally divided doses PLUS Streptomycin 15 mg/kg ideal body weight/24 h IV/IM in 2 equally divided doses for 4 weeks (Patients with creatinine clearance < 50 mL/min or develop creatinine clearance < 50 mL/min during treatment should be treated with double–β-lactam regimen. Patients with abnormal cranial nerve VIII function should be treated with double–β-lactam regimen). |
| Enterococcus Vancomycin- and Aminoglycoside-susceptible Penicillin-Resistant unable to tolerate β-lactam: | Vancomycin 30 mg/kg/24 h IV in 2 equally divided doses PLUS Gentamicin 3 mg/kg/24 h IV/IM in 3 equally divided doses for 6 weeks. |
| Enterococcus Penicillin-, aminoglycoside-, and vancomycin-resistant: | Linezolid 600 mg IV/PO every 12 h for >6 weeks OR Daptomycin 10–12 mg/kg per dose for >6 weeks |
| HACEK | Ceftriaxone 2 g/24 h IV/IM in 1 dose for 4 weeks OR Ampicillin 2 g IV every 4 h for 4 weeks OR Ciprofloxacin 1 g/24 h PO or 800 mg/24 h IV in 2 equally divided doses for 4 weeks. |
| Prosthetic valve | |
| VGS and Streptococcus gallolyticus (bovis) PCN susceptible: | Penicillin G 24 million U/24 h IV either continuously or in 4–6 equally divided doses for 6 weeks OR Ceftriaxone 2 g/24 h IV or IM in 1 dose for 6 weeks PLUS Gentamicin 3 mg/kg/24 h IV or IM in 1 dose for 2 weeks (Vancomycin 30 mg/kg per 24 h IV in 2 equally divided doses for patients intolerant of PCN or CTX). |
| Staphylococcus methicillin-susceptible | Nafcillin or oxacillin 12 g/24 h in 4–6 equally divided doses for ≥6 weeks (Vancomycin should be used for immediate-type hypersensitivity reactions to β-lactam antibiotics) PLUS cefazolin 6 g/24 h IV in 3 equally divided doses for ≥6 weeks (cefazolin may be substituted for non-immediate-type hypersensitivity reactions to penicillins) PLUS Gentamicin 3 mg/kg/24 h IV or IM in 2 or 3 equally divided doses for 2 weeks. |
| Staphylococcus methicillin-resistant | Vancomycin 30 mg/kg/24 h in 2 equally divided doses for ≥6 weeks PLUS Rifampin 900 mg/24 h IV/PO in 3 equally divided doses for ≥6 weeks PLUS Gentamicin 3 mg/kg/24 h IV/IM in 2 or 3 equally divided doses for 2 weeks. |
| Enterococcus susceptible to penicillin and gentamicin | Ampicillin 2 g IV every 4 h for 6 weeks (sx < 3 months) or 6 weeks (sx > 3 months) OR Penicillin G 18–30 million U/24 h IV either continuously or in 6 equally divided doses for 6 weeks PLUS Gentamicin 3 mg/kg ideal body weight in 2–3 equally divided doses. An alternative regimen is double β-lactam Ampicillin 2 g IV every 4 h for 6 weeks PLUS Ceftriaxone 2 g every 12 h for 6 weeks (recommended for patients with creatinine clearance < 50 mL/min). |
| Enterococcus susceptible to penicillin and resistant to Aminoglycosides or Streptomycin-Susceptible Gentamicin-Resistant: | Double β-lactam Ampicillin 2 g IV every 4 h PLUS Ceftriaxone 2 g IV every 12 h for 6 weeks. Alternative for Streptomycin-Susceptible Gentamicin-Resistant includes Ampicillin 2 g every 4 h for 6 weeks OR Penicillin G 18–30 million U/24 h IV either continuously or in 6 equally divided doses PLUS Streptomycin 15 mg/kg ideal body weight/24 h IV/IM in 2 equally divided doses for 6 weeks (Patients with creatinine clearance < 50 mL/min or develop creatinine clearance < 50 mL/min during treatment should be treated with double–β-lactam regimen. Patients with abnormal cranial nerve VIII function should be treated with double–β-lactam regimen). |
| Enterococcus Vancomycin- and Aminoglycoside-susceptible Penicillin-Resistant unable to tolerate β-lactam | Vancomycin 30 mg/kg/24 h IV in 2 equally divided doses PLUS Gentamicin 3 mg/kg/24 h IV/IM in 3 equally divided doses for 6 weeks. |
| Enterococcus Penicillin-, aminoglycoside-, and vancomycin-resistant | Linezolid 600 mg IV/PO every 12 h for >6 weeks OR Daptomycin 10–12 mg/kg per dose for >6 weeks (Linezolid use may be associated with potentially severe bone marrow suppression. Patients should be treated by a care team including specialists in infectious diseases, cardiology, cardiac surgery, and clinical pharmacy. Of note, cardiac valve replacement may be necessary for cure). |
| HACEK | Ceftriaxone 2 g/24 h IV/IM in 1 dose for 6 weeks OR Ampicillin 2 g IV every 4 h for 6 weeks OR Ciprofloxacin 1 g/24 h PO or 800 mg/24 h IV in 2 equally divided doses for 6 weeks. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comeaux, S.; Jamison, K.; Voeltz, M. Contemporary Features and Management of Endocarditis. Diagnostics 2023, 13, 3086. https://doi.org/10.3390/diagnostics13193086
Comeaux S, Jamison K, Voeltz M. Contemporary Features and Management of Endocarditis. Diagnostics. 2023; 13(19):3086. https://doi.org/10.3390/diagnostics13193086
Chicago/Turabian StyleComeaux, Shelby, Kiara Jamison, and Michele Voeltz. 2023. "Contemporary Features and Management of Endocarditis" Diagnostics 13, no. 19: 3086. https://doi.org/10.3390/diagnostics13193086
APA StyleComeaux, S., Jamison, K., & Voeltz, M. (2023). Contemporary Features and Management of Endocarditis. Diagnostics, 13(19), 3086. https://doi.org/10.3390/diagnostics13193086





