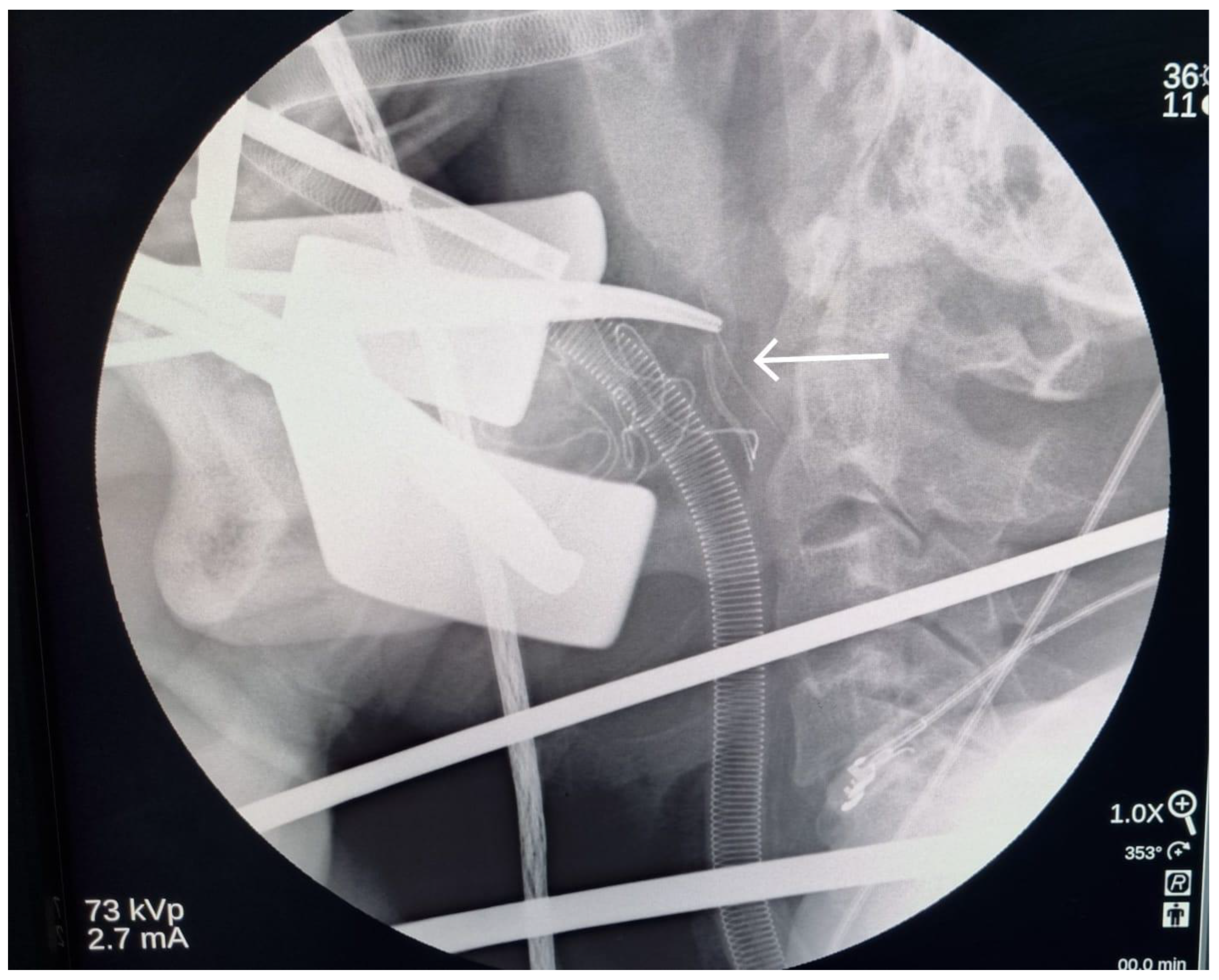
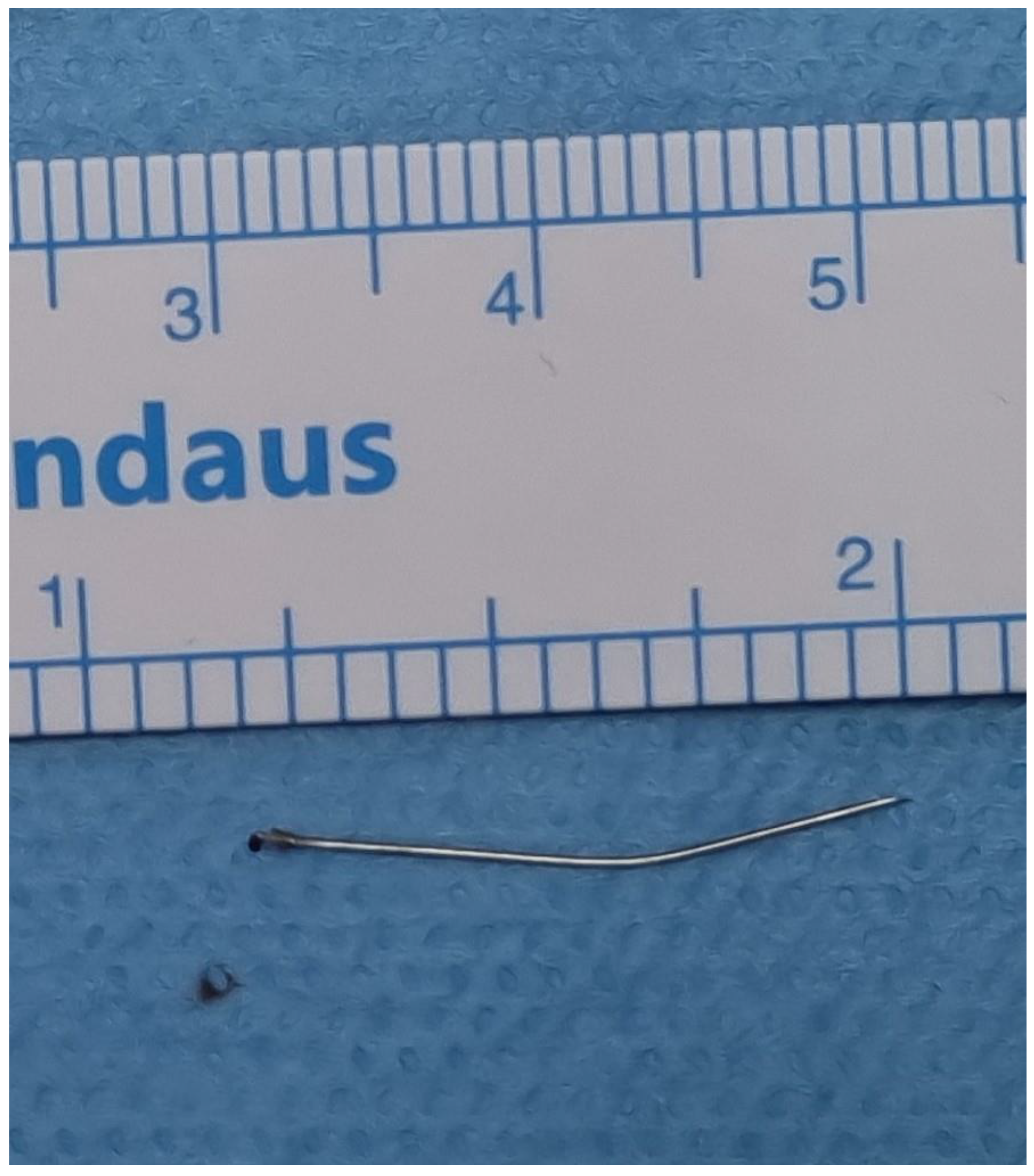
A Case of Broken Local Anesthetic Needle in the Pterygomandibular Space; Diagnostic Approaches and Surgical Management
Abstract
:

Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Augello, M.; von Jackowski, J.; Gratz, K.W.; Jacobsen, C. Needle breakage during local anesthesia in the oral cavity-a retrospective of the last 50 years with guidelines for treatment and prevention. Clin. Oral. Investig. 2011, 15, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Pogrel, M.A. Broken local anesthetic needles: A case series of 16 patients, with recommendations. J. Am. Dent. Assoc. 2009, 140, 1517–1522. [Google Scholar] [CrossRef] [PubMed]
- Cirulli, N.; Patano, A.; Palmieri, G.; Di Pede, C.; Settanni, V.; Piras, F.; Inchingolo, A.D.; Mancini, A.; Rapone, B.; Malcangi, G.; et al. Needle Fracture in Pterygomandibular Space during Loco-Regional Dental Anesthesia: Systematic Review. Appl. Sci. 2023, 13, 4421. [Google Scholar] [CrossRef]
- Elsayed, S.A.; Abdullah, A.A.B.; Dar-Odeh, N.; Altaweel, A.A. Intraoral Wound Dehiscence after Open Reduction Internal Fixation of Mandibular Fractures: A Retrospective Cohort Study. Wounds 2021, 33, 60–64. [Google Scholar] [PubMed]
- Rahman, N.; Clarke, M.; Stassen, L.F. Case report: Management of broken dental needles in practice. J. Ir. Dent. Assoc. 2013, 59, 241–245. [Google Scholar] [PubMed]
- El Khateeb, S.M.; Abu-Hammad, O.; Fadel, H.; Dar-Odeh, N. A Retrospective Analysis of Radiographic Jaw Findings in Young Women; Prevalence and Predictors. J. Int. Soc. Prev. Community Dent. 2017, 7, 22–27. [Google Scholar] [PubMed]
- Sghaireen, M.G.; Srivastava, K.C.; Shrivastava, D.; Ganji, K.K.; Patil, S.R.; Abuonq, A.; Mousa, M.A.; Dar-Odeh, N.; Sghaireen, G.M.; Kamal, M.A.; et al. A CBCT Based Three-Dimensional Assessment of Mandibular Posterior Region for Evaluating the Possibility of Bypassing the Inferior Alveolar Nerve While Placing Dental Implants. Diagnostics 2020, 10, 406. [Google Scholar] [CrossRef] [PubMed]
- Abu-Hammad, O.; Zain-Alabedeen, E.; Abu-Hammad, S.; Abdouh, I.; Ayed, Y.; Abu-Hammad, A.; Dar-Odeh, N. Imaging Techniques for assessment of Cranio-Maxillofacial Complications of COVID-19, A Systematic Review. Open Dent. J. 2023, 17, e187421062304121. [Google Scholar] [CrossRef]
- Lukas, D.; Jan, M.; Constantinus, P.; Paul, L. Fractured Needle Removal with a 3-Dimensionally Printed Surgical Guide: A Case Report and Literature Review. J. Oral Maxillofac. Surg. 2021, 79, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Enomoto, K.; Nishimura, H.; Inohara, H.; Murata, J.; Horii, A.; Doi, K.; Kubo, T. A rare case of a glass foreign body in the parapharyngeal space: Pre-operative assessment by contrast-enhanced CT and three-dimensional CT images. Dentomaxillofac Radiol. 2009, 38, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Thompson, M.; Wright, S.; Cheng, L.H.; Starr, D. Locating broken dental needles. Int. J. Oral Maxillofac. Surg. 2003, 32, 642–644. [Google Scholar] [CrossRef] [PubMed]
- Marinheiro, B.H.; Araújo, R.T.E.; Sverzut, T.F.V.; Trivellato, A.E.; Sverzut, C.E. Migration and surgical retrieval of a broken dental needle: A literature review and case report. Gen. Dent. 2019, 67, 34–37. [Google Scholar] [PubMed]
- Crouse, V. Migration of a broken anesthetic needle: Report of a case. South Carol. Dent. J. 1970, 28, 16–19. [Google Scholar]
- Moore, U.J.; Fanibunda, K.; Gross, M.J. The use of a metal detector for localisation of a metallic foreign body in the floor of the mouth. Br. J. Oral Maxillofac. Surg. 1993, 31, 191–192. [Google Scholar] [CrossRef] [PubMed]
- Steelman, V.M.; Alasagheirin, M.H. Assessment of Radiofrequency Device Sensitivity for the Detection of Retained Surgical Sponges in Patients with Morbid Obesity. Arch. Surg. 2012, 147, 955–1556. [Google Scholar] [CrossRef] [PubMed]
- Johansson, B.; Krekmanov, L. Fragment of broken instrument removed from field of operation by an electromagnet. Br. J. Oral Maxillofac. Surg. 1987, 25, 265–266. [Google Scholar] [CrossRef]
- Lee, T.Y.; Zaid, W.S. Broken dental needle retrieval using a surgical navigation system: A case report and literature review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 119, e55–e59. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, A.E.; Scangas, G.A.; Jafari, A.; Metson, R. Endoscopic Transoral Image-Guided Retrieval of Infratemporal Fossa Foreign Bodies. OTO Open. 2020, 4, 2473974X20947026. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malkawi, Z.; Alayeh, A.; Alshawa, A.; Shaban, O.; Al Saraireh, O.; Malkawi, H.; Babkair, H.; Abdouh, I.; Dar-Odeh, N. A Case of Broken Local Anesthetic Needle in the Pterygomandibular Space; Diagnostic Approaches and Surgical Management. Diagnostics 2023, 13, 3050. https://doi.org/10.3390/diagnostics13193050
Malkawi Z, Alayeh A, Alshawa A, Shaban O, Al Saraireh O, Malkawi H, Babkair H, Abdouh I, Dar-Odeh N. A Case of Broken Local Anesthetic Needle in the Pterygomandibular Space; Diagnostic Approaches and Surgical Management. Diagnostics. 2023; 13(19):3050. https://doi.org/10.3390/diagnostics13193050
Chicago/Turabian StyleMalkawi, Ziad, Alaa Alayeh, Abedalaziz Alshawa, Ola Shaban, Omar Al Saraireh, Hashem Malkawi, Hamzah Babkair, Ismail Abdouh, and Najla Dar-Odeh. 2023. "A Case of Broken Local Anesthetic Needle in the Pterygomandibular Space; Diagnostic Approaches and Surgical Management" Diagnostics 13, no. 19: 3050. https://doi.org/10.3390/diagnostics13193050
APA StyleMalkawi, Z., Alayeh, A., Alshawa, A., Shaban, O., Al Saraireh, O., Malkawi, H., Babkair, H., Abdouh, I., & Dar-Odeh, N. (2023). A Case of Broken Local Anesthetic Needle in the Pterygomandibular Space; Diagnostic Approaches and Surgical Management. Diagnostics, 13(19), 3050. https://doi.org/10.3390/diagnostics13193050





