Differential Protein Expression Patterns of HOXA13 and HOXB13 Are Associated with Bladder Cancer Progression
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Tissue Samples
2.2. Tissue Sectioning
2.3. Hematoxylin and Eosin (H&E) Staining
2.4. IHC Analysis
2.5. Scoring of Immunohistochemical Staining
2.6. Statistical Analysis
3. Results
3.1. Protein Expression of HOXA13 and HOXB13 in Bladder Cancer Tissues
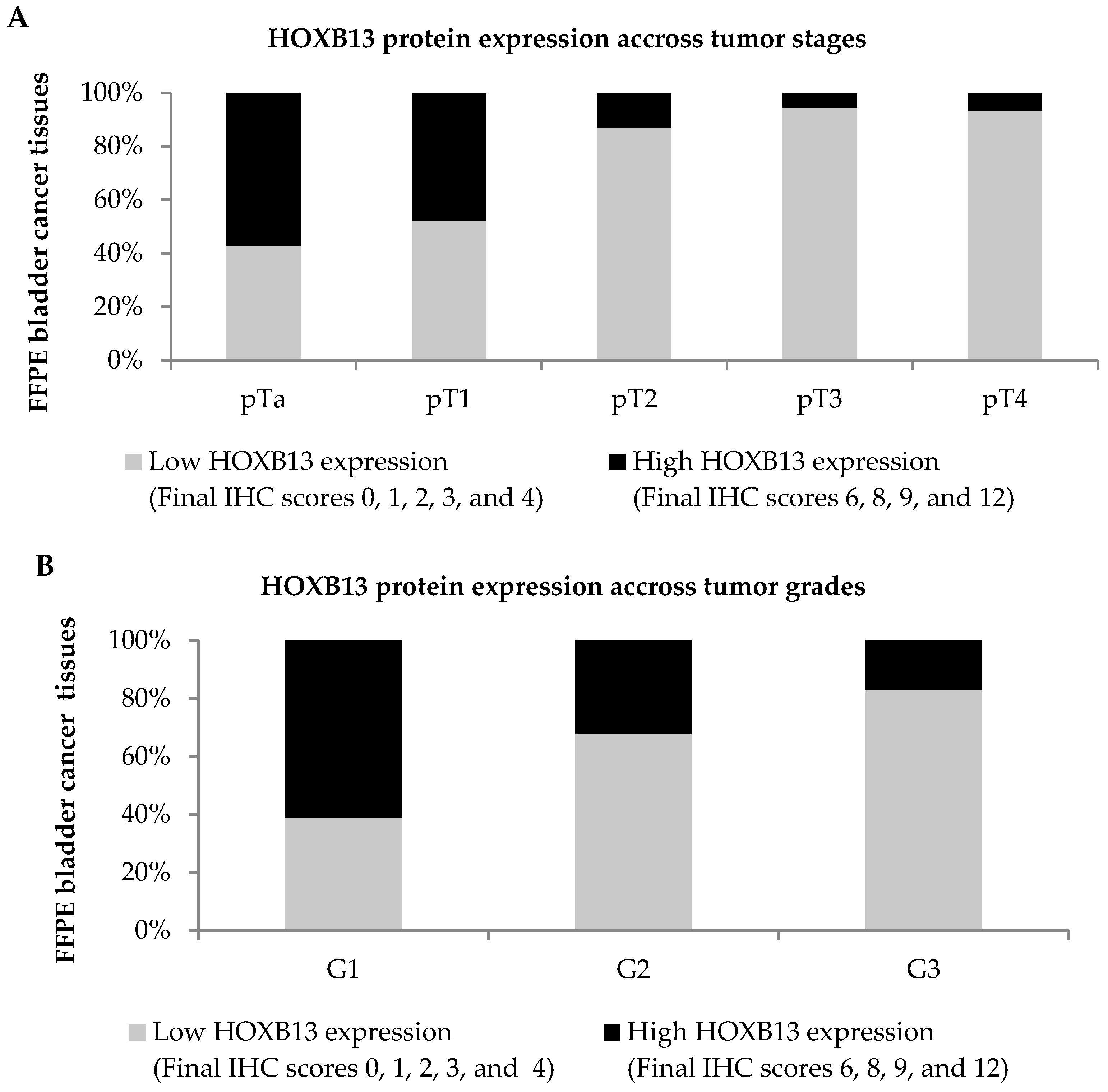
3.2. Protein Expression of HOXA13 and HOXB13 across Different Stages and Grades of Bladder Cancer
3.3. Association of HOXA13 and HOXB13 Protein Expression with Demographic and Clinicopathological Characteristics of Bladder Cancer Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Kirkali, Z.; Chan, T.; Manoharan, M.; Algaba, F.; Busch, C.; Cheng, L.; Kiemeney, L.; Kriegmair, M.; Montironi, R.; Murphy, W.M.; et al. Bladder cancer: Epidemiology, staging and grading, and diagnosis. Urology 2005, 66 (Suppl. S1), 4–34. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.I.; Amin, M.B.; Reuter, V.R.; Mostofi, F.K. The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee. Am. J. Surg. Pathol. 1998, 22, 1435–1448. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Gomez, J.; Madero, R.; Solsona, E.; Unda, M.; Martinez-Piñeiro, L.; Gonzalez, M.; Portillo, J.; Ojea, A.; Pertusa, C.; Rodriguez-Molina, J.; et al. Predicting nonmuscle invasive bladder cancer recurrence and progression in patients treated with bacillus Calmette-Guerin: The CUETO scoring model. J. Urol. 2009, 182, 2195–2203. [Google Scholar] [CrossRef] [PubMed]
- Sylvester, R.J.; van der Meijden, A.P.M.; Oosterlinck, W.; Witjes, J.A.; Bouffioux, C.; Denis, L.; Newling, D.W.W.; Kurth, K. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: A combined analysis of 2596 patients from seven EORTC trials. Eur. Urol. 2006, 49, 466–477. [Google Scholar] [CrossRef]
- Sievert, K.D.; Amend, B.; Nagele, U.; Schilling, D.; Bedke, J.; Horstmann, M.; Hennenlotter, J.; Kruck, S.; Stenzl, A. Economic aspects of bladder cancer: What are the benefits and costs? World J. Urol. 2009, 27, 295–300. [Google Scholar] [CrossRef]
- Stenzl, A.; Hennenlotter, J.; Schilling, D. Can we still afford bladder cancer? Curr. Opin. Urol. 2008, 18, 488–492. [Google Scholar] [CrossRef]
- Liu, S.; Hou, J.; Zhang, H.; Wu, Y.; Hu, M.; Zhang, L.; Xu, J.; Na, R.; Jiang, H.; Ding, Q. The evaluation of the risk factors for non-muscle invasive bladder cancer (NMIBC) recurrence after transurethral resection (TURBt) in Chinese population. PLoS ONE 2015, 10, e0123617. [Google Scholar] [CrossRef]
- Zhu, C.Z.; Ting, H.N.; Ng, K.H.; Ong, T.A. A review on the accuracy of bladder cancer detection methods. J. Cancer 2019, 10, 4038–4044. [Google Scholar] [CrossRef] [PubMed]
- Chamie, K.; Saigal, C.S.; Lai, J.; Hanley, J.M.; Setodji, C.M.; Konety, B.R.; Litwin, M.S. Urologic Diseases in America Project Compliance with guidelines for patients with bladder cancer: Variation in the delivery of care. Cancer 2012, 117, 5392–5401. [Google Scholar] [CrossRef]
- Aldoghachi, A.F.; Baharudin, A.; Ahmad, U.; Chan, S.C.; Ong, T.A.; Yunus, R.; Razack, A.H.; Yusoff, K.; Veerakumarasivam, A. Evaluation of CERS2 gene as a potential biomarker for bladder cancer. Dis. Markers 2019, 2019, 3875147. [Google Scholar] [CrossRef]
- Gurung, P.M.S.; Veerakumarasivam, A.; Williamson, M.; Counsell, N.; Douglas, J.; Tan, W.S.; Feber, A.; Crabb, S.J.; Short, S.C.; Freeman, A.; et al. Loss of expression of the tumour suppressor gene AIMP3 predicts survival following radiotherapy in muscle-invasive bladder cancer. Int. J. Cancer 2015, 136, 709–720. [Google Scholar] [CrossRef]
- Veerakumarasivam, A.; Goldstein, L.D.; Saeb-Parsy, K.; Scott, H.E.; Warren, A.; Thorne, N.P.; Mills, I.G.; Venkitaraman, A.; Neal, D.E.; Kelly, J.D. AURKA overexpression accompanies dysregulation of DNA-damage response genes in invasive urothelial cell carcinoma. Cell Cycle 2008, 7, 3525–3533. [Google Scholar] [CrossRef] [PubMed]
- Gehring, W.J.; Hiromi, Y. Homeotic genes and the homeobox. Annu. Rev. Genet. 1986, 20, 147–173. [Google Scholar] [CrossRef] [PubMed]
- Krumlauf, R. Hox genes in vertebrate development. Cell 1994, 78, 191–201. [Google Scholar] [CrossRef] [PubMed]
- HOXA13 Gene. Available online: https://ghr.nlm.nih.gov/gene/HOXA13 (accessed on 4 July 2019).
- HOXB13 Gene. Available online: https://ghr.nlm.nih.gov/gene/HOXB13 (accessed on 4 July 2019).
- Guo, B.; Che, T.; Shi, B.; Guo, L.; Yin, Y.; Li, L.; Wang, J.; Yan, D.; Chen, Y. Screening and identification of specific markers for bladder transitional cell carcinoma from urine urothelial cells with suppressive subtractive hybridization and cDNA microarray. Can. Urol. Assoc. J. 2011, 5, E129–E137. [Google Scholar] [CrossRef]
- Guo, B.; Che, T.; Shi, B.; Guo, L.; Zhang, Z.; Li, L.; Cai, C.; Chen, Y. Interaction network analysis of differentially expressed genes and screening of cancer marker in the urine of patients with invasive bladder cancer. Int. J. Clin. Exp. Med. 2015, 8, 3619–3628. [Google Scholar]
- Holyoake, A.; O’Sullivan, P.; Pollock, R.; Best, T.; Watanabe, J.; Kajita, Y.; Matsui, Y.; Ito, M.; Nishiyama, H.; Kerr, N.; et al. Development of a multiplex RNA urine test for the detection and stratification of transitional cell carcinoma of the bladder. Clin. Cancer Res. 2008, 14, 742–749. [Google Scholar] [CrossRef]
- Duan, R.; Han, L.; Wang, Q.; Wei, J.; Chen, L.; Zhang, J.; Kang, C.; Wang, L. HOXA13 is a potential GBM diagnostic marker and promotes glioma invasion by activating the Wnt and TGF-β pathways. Oncotarget 2015, 6, 27778–27793. [Google Scholar] [CrossRef]
- Gu, Z.D.; Shen, L.Y.; Wang, H.; Chen, X.M.; Li, Y.; Ning, T.; Chen, K.N. HOXA13 promotes cancer cell growth and predicts poor survival of patients with esophageal squamous cell carcinoma. Cancer Res. 2009, 69, 4969–4973. [Google Scholar] [CrossRef]
- He, Y.X.; Song, X.H.; Zhao, Z.Y.; Zhao, H. HOXA13 upregulation in gastric cancer is associated with enhanced cancer cell invasion and epithelial-to-mesenchymal transition. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 258–265. [Google Scholar] [CrossRef]
- Hu, H.Y.; Chen, Y.B.; Cheng, S.; Li, G.H.; Zhang, Z.G. Dysregulated expression of homebox gene HOXA13 is correlated with the poor prognosis in bladder cancer. Wien. Klin. Wochenschr. 2017, 129, 391–397. [Google Scholar] [CrossRef]
- Quagliata, L.; Quintavalle, C.; Lanzafame, M.; Matter, M.S.; Novello, C.; di Tommaso, L.; Pressiani, T.; Rimassa, L.; Tornillo, L.; Roncalli, M.; et al. High expression of HOXA13 correlates with poorly differentiated hepatocellular carcinomas and modulates sorafenib response in in vitro models. Lab. Investig. 2018, 98, 95–105. [Google Scholar] [CrossRef]
- Dong, Y.; Cai, Y.; Liu, B.; Jiao, X.; Li, Z.; Guo, D.; Li, X.; Wang, Y.; Yang, D. HOXA13 is associated with unfavorable survival and acts as a novel oncogene in prostate carcinoma. Futur. Oncol. 2017, 13, 1505–1516. [Google Scholar] [CrossRef] [PubMed]
- Qu, L.; Zhong, Y.; Zheng, Z.; Zhao, R. CDH17 is a downstream effector of HOXA13 in modulating the Wnt/β-catenin signaling pathway in gastric cancer. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 1234–1241. [Google Scholar]
- Miao, J.Y.; Wang, Z.C.; Provencher, H.; Muir, B.; Dahiya, S.; Carney, E.; Leong, C.O.; Sgroi, D.C.; Orsulic, S. HOXB13 promotes ovarian cancer progression. Proc. Natl. Acad. Sci. USA 2007, 104, 17093–17098. [Google Scholar] [CrossRef]
- Zhai, L.L.; Wu, Y.; Cai, C.Y.; Tang, Z.G. Overexpression of homeobox B-13 correlates with angiogenesis, aberrant expression of EMT markers, aggressive characteristics and poor prognosis in pancreatic carcinoma. Int. J. Clin. Exp. Pathol. 2015, 8, 6919–6927. [Google Scholar]
- Zhu, J.Y.; Sun, Q.K.; Wang, W.; Jia, W.D. High-level expression of HOXB13 is closely associated with tumor angiogenesis and poor prognosis of hepatocellular carcinoma. Int. J. Clin. Exp. Pathol. 2014, 7, 2925–2933. [Google Scholar] [PubMed]
- Jung, C.; Kim, R.S.; Zhang, H.; Lee, S.J.; Sheng, H.; Loehrer, P.J.; Gardner, T.A.; Jeng, M.H.; Kao, C. HOXB13 is downregulated in colorectal cancer to confer TCF4-mediated transactivation. Br. J. Cancer 2005, 92, 2233–2239. [Google Scholar] [CrossRef]
- Jung, C.Y.; Kim, R.S.; Zhang, H.J.; Lee, S.J.; Jeng, M.H. HOXB13 induces growth suppression of prostate cancer cells as a repressor of hormone-activated androgen receptor signaling. Cancer Res. 2004, 64, 9185–9192. [Google Scholar] [CrossRef] [PubMed]
- Okuda, H.; Toyota, M.; Ishida, W.; Furihata, M.; Tsuchiya, M.; Kamada, M.; Tokino, T.; Shuin, T. Epigenetic inactivation of the candidate tumor suppressor gene HOXB13 in human renal cell carcinoma. Oncogene 2006, 25, 1733–1742. [Google Scholar] [CrossRef] [PubMed]
- Kristiansen, I.; Stephan, C.; Jung, K.; Dietel, M.; Rieger, A.; Tolkach, Y.; Kristiansen, G. Sensitivity of HOXB13 as a diagnostic immunohistochemical marker of prostatic origin in prostate cancer metastases: Comparison to PSA, prostein, androgen receptor, ERG, NKX3.1, PSAP, and PSMA. Int. J. Mol. Sci. 2017, 18, 1151. [Google Scholar] [CrossRef] [PubMed]
- Haller, K.; Rambaldi, I.; Daniels, E.; Featherstone, M. Subcellular localization of multiple PREP2 isoforms is regulated by actin, tubulin, and nuclear export. J. Biol. Chem. 2004, 279, 49384–49394. [Google Scholar] [CrossRef] [PubMed]
- Stevens, K.E.; Mann, R.S. A balance between two nuclear localization sequences and a nuclear export sequence governs extradenticle subcellular localization. Genetics 2007, 175, 1625–1636. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Liu, Y.; Li, P.; Fan, L.; Wu, M. The nuclear transportation routes of membrane-bound transcription factors. Cell Commun. Signal. 2018, 16, 12. [Google Scholar] [CrossRef]
- Cantile, M.; Scognamiglio, G.; La Sala, L.; La Mantia, E.; Scaramuzza, V.; Valentino, E.; Tatangelo, F.; Losito, S.; Pezzullo, L.; Chiofalo, M.G.; et al. Aberrant expression of posterior HOX genes in well differentiated histotypes of thyroid cancers. Int. J. Mol. Sci. 2013, 14, 21727–21740. [Google Scholar] [CrossRef]
- Wen, Y.; Shu, F.; Chen, Y.; Chen, Y.; Lan, Y.; Duan, X.; Zhao, S.C.; Zeng, G. The prognostic value of HOXA13 in solid tumors: A meta-analysis. Clin. Chim. Acta 2018, 483, 64–68. [Google Scholar] [CrossRef]
- Heidari, Z.; Mahmoudzadeh-Sagheb, H.; Jahantigh, M.; Gorgich, E.A.C. Immunohistochemical expression of KI67 and HER2 in colorectal cancer compared to adenomatous and normal samples. Int. J. Cancer Manag. 2017, 10, e12252. [Google Scholar] [CrossRef]
- Scott, V.; Morgan, E.A.; Stadler, H.S. Genitourinary functions of Hoxa13 and Hoxd13. J. Biochem. 2005, 137, 671–676. [Google Scholar] [CrossRef]
- Hirohashi, S.; Kanai, Y. Cell adhesion system and human cancer morphogenesis. Cancer Sci. 2003, 94, 575–581. [Google Scholar] [CrossRef]
- Sui, B.Q.; Zhang, C.D.; Liu, J.C.; Wang, L.; Dai, D.Q. HOXB13 expression and promoter methylation as a candidate biomarker in gastric cancer. Oncol. Lett. 2018, 15, 8833–8840. [Google Scholar] [CrossRef]
- Muthusamy, V.; Duraisamy, S.; Bradbury, C.M.; Hobbs, C.; Curley, D.P.; Nelson, B.; Bosenberg, M. Epigenetic silencing of novel tumor suppressors in malignant melanoma. Cancer Res. 2006, 66, 11187–11193. [Google Scholar] [CrossRef]
- Jung, C.Y.; Kim, R.S.; Lee, S.J.; Wang, C.H.; Jeng, M.H. HOXB13 homeodomain protein suppresses the growth of prostate cancer cells by the negative regulation of T-cell factor 4. Cancer Res. 2004, 64, 3046–3051. [Google Scholar] [CrossRef] [PubMed]
- Marra, L.; Cantile, M.; Scognamiglio, G.; Marra, L.; Perdona, S.; La Mantia, E.; Cerrone, M.; Gigantino, V.; Cillo, C.; Caraglia, M.; et al. Deregulation of HOX B13 expression in urinary bladder cancer progression. Curr. Med. Chem. 2013, 20, 833–839. [Google Scholar] [CrossRef]
- Popat, S.; Chen, Z.; Zhao, D.; Pan, H.; Hearle, N.; Chandler, I.; Shao, Y.; Aherne, W.; Houlston, R.S. A prospective, blinded analysis of thymidylate synthase and p53 expression as prognostic markers in the adjuvant treatment of colorectal cancer. Ann. Oncol. 2006, 17, 1810–1817. [Google Scholar] [CrossRef] [PubMed]
- Faber, J.; Fonseca, L.M. How sample size influences research outcomes. Dental Press J. Orthod. 2014, 19, 27–29. [Google Scholar] [CrossRef] [PubMed]





| Percentage of Positive Cells | Score | Staining Intensity | Score |
|---|---|---|---|
| Less than 1% positive tumor cells | 0 | No staining | 0 |
| 1 to 30% positive tumor cells | 1 | Weak staining | 1 |
| 30 to 70% positive tumor cells | 2 | Moderate staining | 2 |
| More than 70% positive tumor cells | 3 | Strong staining | 3 |
| Percentage of Positive Cells | Score | Staining Intensity | Score |
|---|---|---|---|
| 0% positive tumor cells | 0 | No staining | 0 |
| 1 to 10% positive tumor cells | 1 | Weak staining | 1 |
| 11 to 50% positive tumor cells | 2 | Moderate staining | 2 |
| 50 to 80% positive tumor cells | 3 | Strong staining | 3 |
| More than 80% positive tumor cells | 4 |
| Characteristic | Number of Cases (%) | HOXA13 Expression | χ2 Value | p Value | Cramer’s V Value | Strength of Association | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low 2 (%) | High (%) | |||||||||
| Gender | 1.265 | 0.261 | - | - | ||||||
| Male | 105 | (95.5) | 37 | (35.2) | 68 | (64.8) | ||||
| Female | 5 | (4.5) | 3 | (60.0) | 2 | (40.0) | ||||
| Ethnicity | 3.132 | 0.372 | - | - | ||||||
| Malay | 65 | (59.1) | 25 | (38.5) | 40 | (61.5) | ||||
| Chinese | 28 | (25.5) | 7 | (25.0) | 21 | (75.0) | ||||
| Indian | 14 | (12.7) | 6 | (42.9) | 8 | (57.1) | ||||
| Others | 3 | (2.7) | 2 | (66.7) | 1 | (33.3) | ||||
| Age | 1.947 | 0.163 | - | - | ||||||
| <50 | 13 | (11.8) | 7 | (53.8) | 6 | (46.2) | ||||
| ≥50 | 97 | (88.2) | 33 | (34.0) | 64 | (66.0) | ||||
| Tumor invasiveness | 5.384 | 0.020 * | 0.221 | Moderate | ||||||
| NMIBC | 49 | (44.5) | 12 | (24.5) | 37 | (75.5) | ||||
| MIBC | 61 | (55.5) | 28 | (45.9) | 33 | (54.1) | ||||
| Tumor stage | 9.350 | 0.053 | - | - | ||||||
| pTa | 23 | (20.9) | 5 | (21.7) | 18 | (78.3) | ||||
| pT1 | 26 | (23.6) | 7 | (26.9) | 19 | (73.1) | ||||
| pT2 | 23 | (20.9) | 14 | (60.9) | 9 | (39.1) | ||||
| pT3 | 21 | (19.1) | 7 | (33.3) | 14 | (66.7) | ||||
| pT4 | 17 | (15.5) | 7 | (41.2) | 10 | (58.8) | ||||
| Tumor grade 1 | 11.414 | 0.003 * | 0.322 | Strong | ||||||
| G1 | 20 | (18.2) | 3 | (15.0) | 17 | (85.0) | ||||
| G2 | 26 | (23.6) | 16 | (61.5) | 10 | (38.5) | ||||
| G3 | 64 | (58.2) | 21 | (32.8) | 43 | (67.2) | ||||
| Lymph node metastasis | 4.901 | 0.027 * | 0.288 | Moderate | ||||||
| Yes | 26 | (23.6) | 9 | (34.6) | 17 | (65.4) | ||||
| No | 33 | (30.0) | 21 | (63.6) | 12 | (36.4) | ||||
| N/A | 51 | (46.4) | - | - | - | - | ||||
| Metastasis | 1.892 | 0.169 | - | - | ||||||
| Yes | 30 | (27.3) | 14 | (46.7) | 16 | (53.3) | ||||
| No | 80 | (72.7) | 26 | (32.5) | 54 | (67.5) | ||||
| Recurrence | 4.092 | 0.043 * | 0.193 | Weak | ||||||
| Yes | 66 | (60.0) | 19 | (28.8) | 47 | (71.2) | ||||
| No | 44 | (40.0) | 21 | (47.7) | 23 | (52.3) | ||||
| Characteristic | Number of Cases (%) | HOXA13 Localization | χ2 Value | p-Value | Cramer’s V Value | Strength of Association | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| None | Nucleus | Nucleus and Cytoplasm | ||||||||||
| Gender | 0.506 | 0.777 | - | - | ||||||||
| Male | 105 | (95.5) | 6 | (5.7) | 86 | (81.9) | 13 | (12.4) | ||||
| Female | 5 | (4.5) | 0 | (0.0) | 4 | (80.0) | 1 | (20.0) | ||||
| Ethnicity | 11.728 | 0.068 | - | - | ||||||||
| Malay | 65 | (59.1) | 3 | (4.6) | 53 | (81.5) | 9 | (13.8) | ||||
| Chinese | 28 | (25.5) | 0 | (0.0) | 24 | (85.7) | 4 | (14.3) | ||||
| Indian | 14 | (12.7) | 2 | (14.3) | 12 | (85.7) | 0 | (0.0) | ||||
| Others | 3 | (2.7) | 1 | (33.3) | 1 | (33.3) | 1 | (33.3) | ||||
| Age | 15.156 | 0.001 * | 0.371 | Strong | ||||||||
| <50 | 13 | (11.8) | 0 | (0.0) | 7 | (53.8) | 6 | (46.2) | ||||
| ≥50 | 97 | (88.2) | 6 | (6.2) | 83 | (85.6) | 8 | (8.2) | ||||
| Tumor invasiveness | 2.068 | 0.356 | - | - | ||||||||
| NMIBC | 49 | (44.5) | 1 | (2.0) | 42 | (85.7) | 6 | (12.2) | ||||
| MIBC | 61 | (55.5) | 5 | (8.2) | 48 | (78.7) | 8 | (13.1) | ||||
| Tumor stage | 11.257 | 0.188 | - | - | ||||||||
| pTa | 23 | (20.9) | 1 | (4.3) | 20 | (87.0) | 2 | (8.7) | ||||
| pT1 | 26 | (23.6) | 0 | (0.0) | 22 | (84.6) | 4 | (15.4) | ||||
| pT2 | 23 | (20.9) | 4 | (17.4) | 17 | (73.9) | 2 | (8.7) | ||||
| pT3 | 21 | (19.1) | 1 | (4.8) | 18 | (85.7) | 2 | (9.5) | ||||
| pT4 | 17 | (15.5) | 0 | (0.0) | 13 | (76.5) | 4 | (23.5) | ||||
| Tumor grade 1 | 3.438 | 0.487 | - | - | ||||||||
| G1 | 20 | (18.2) | 1 | (5.0) | 15 | (75.0) | 4 | (20.0) | ||||
| G2 | 26 | (23.6) | 1 | (3.8) | 20 | (76.9) | 5 | (19.2) | ||||
| G3 | 64 | (58.2) | 4 | (6.2) | 55 | (85.9) | 5 | (7.8) | ||||
| Lymph node metastasis | 1.336 | 0.513 | - | - | ||||||||
| Yes | 26 | (23.6) | 1 | (3.8) | 21 | (80.8) | 4 | (15.4) | ||||
| No | 33 | (30.0) | 4 | (12.1) | 25 | (75.8) | 4 | (12.1) | ||||
| N/A | 51 | (46.4) | - | - | - | - | - | - | ||||
| Metastasis | 0.140 | 0.933 | - | - | ||||||||
| Yes | 30 | (27.3) | 2 | (6.7) | 24 | (80.0) | 4 | (13.3) | ||||
| No | 80 | (72.7) | 4 | (5.0) | 66 | (82.5) | 10 | (12.5) | ||||
| Recurrence | 7.566 | 0.023 * | 0.262 | Moderate | ||||||||
| Yes | 66 | (60.0) | 1 | (1.5) | 59 | (89.4) | 6 | (9.1) | ||||
| No | 44 | (40.0) | 5 | (11.4) | 31 | (70.5) | 8 | (18.2) | ||||
| Characteristic | Number of Cases (%) | HOXB13 Expression | χ2 Value | p-Value | Cramer’s V Value | Strength of Association | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low 2 (%) | High (%) | |||||||||
| Gender | 0.346 | 0.556 | - | - | ||||||
| Male | 97 | (95.1) | 70 | (72.2) | 27 | (27.8) | ||||
| Female | 5 | (4.9) | 3 | (60.0) | 2 | (40.0) | ||||
| Ethnicity | 3.000 | 0.392 | - | - | ||||||
| Malay | 58 | (56.9) | 43 | (74.1) | 15 | (25.9) | ||||
| Chinese | 27 | (26.5) | 18 | (66.7) | 9 | (33.3) | ||||
| Indian | 14 | (13.7) | 11 | (78.6) | 3 | (21.4) | ||||
| Others | 3 | (2.9) | 1 | (33.3) | 2 | (66.7) | ||||
| Age | 0.040 | 0.841 | - | - | ||||||
| <50 | 13 | (12.7) | 9 | (69.2) | 4 | (30.8) | ||||
| ≥50 | 89 | (87.3) | 64 | (71.9) | 25 | (28.1) | ||||
| Tumor invasiveness | 23.212 | ≤0.001 * | 0.477 | Strong | ||||||
| NMIBC | 46 | (45.1) | 22 | (47.8) | 24 | (52.2) | ||||
| MIBC | 56 | (54.9) | 51 | (91.1) | 5 | (8.9) | ||||
| Tumor stage | 24.010 | ≤0.001 | 0.485 | Strong | ||||||
| pTa | 21 | (20.6) | 9 | (42.9) | 12 | (57.1) | ||||
| pT1 | 25 | (24.5) | 13 | (52.0) | 12 | (48.0) | ||||
| pT2 | 23 | (22.5) | 20 | (87.0) | 3 | (13.0) | ||||
| pT3 | 18 | (17.6) | 17 | (94.4) | 1 | (5.6) | ||||
| pT4 | 15 | (14.7) | 14 | (93.3) | 1 | (6.7) | ||||
| Tumor grade 1 | 13.427 | 0.001 * | 0.363 | Strong | ||||||
| G1 | 18 | (17.6) | 7 | (38.9) | 11 | (61.1) | ||||
| G2 | 25 | (24.5) | 17 | (68.0) | 8 | (32.0) | ||||
| G3 | 59 | (57.8) | 49 | (83.1) | 10 | (16.9) | ||||
| Lymph node metastasis | 0.789 | 0.375 | - | - | ||||||
| Yes | 24 | (23.5) | 24 | (100.0) | 0 | (0.0) | ||||
| No | 31 | (30.4) | 30 | (96.8) | 1 | (3.2) | ||||
| N/A | 47 | (46.1) | - | - | - | - | ||||
| Metastasis | 7.976 | 0.005 * | 0.280 | Moderate | ||||||
| Yes | 27 | (26.5) | 25 | (92.6) | 2 | (7.4) | ||||
| No | 75 | (73.5) | 48 | (64.0) | 27 | (36.0) | ||||
| Recurrence | 3.410 | 0.065 | - | - | ||||||
| Yes | 63 | (61.8) | 41 | (65.1) | 22 | (34.9) | ||||
| No | 39 | (38.2) | 32 | (82.1) | 7 | (17.9) | ||||
| Characteristic | Number of Cases (%) | HOXB13 Localization | χ2 Value | p-Value | Cramer’s V Value | Strength of Association | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| None | Nucleus | Nucleus and Cytoplasm | Cytoplasm | |||||||||||
| Gender | 1.437 | 0.697 | - | - | ||||||||||
| Male | 97 | (95.1) | 41 | (42.3) | 34 | (35.1) | 19 | (19.6) | 3 | (3.1) | ||||
| Female | 5 | (4.9) | 2 | (40.0) | 1 | (20.0) | 2 | (40.0) | 0 | (0.0) | ||||
| Ethnicity | 2.216 | 0.988 | - | - | ||||||||||
| Malay | 58 | (56.9) | 25 | (43.1) | 18 | (31.0) | 13 | (22.4) | 2 | (3.4) | ||||
| Chinese | 27 | (26.5) | 10 | (37.0) | 11 | (40.7) | 5 | (18.5) | 1 | (3.7) | ||||
| Indian | 14 | (13.7) | 7 | (50.0) | 5 | (35.7) | 2 | (14.3) | 0 | (0.0) | ||||
| Others | 3 | (2.9) | 1 | (33.3) | 1 | (33.3) | 1 | (33.3) | 0 | (0.0) | ||||
| Age | 3.346 | 0.341 | - | - | ||||||||||
| <50 | 13 | (12.7) | 5 | (38.5) | 3 | (23.1) | 5 | (38.5) | 0 | (0.0) | ||||
| ≥50 | 89 | (87.3) | 38 | (42.7) | 32 | (36.0) | 16 | (18.0) | 3 | (3.4) | ||||
| Tumor invasiveness | 26.927 | ≤0.001 * | 0.514 | Strong | ||||||||||
| NMIBC | 46 | (45.1) | 8 | (17.4) | 27 | (58.7) | 10 | (21.7) | 1 | (2.2) | ||||
| MIBC | 56 | (54.9) | 35 | (62.5) | 8 | (14.3) | 11 | (19.6) | 2 | (3.6) | ||||
| Tumor stage | 43.160 | ≤0.001 * | 0.376 | Strong | ||||||||||
| pTa | 21 | (20.6) | 2 | (9.5) | 16 | (76.2) | 2 | (9.5) | 1 | (4.8) | ||||
| pT1 | 25 | (24.5) | 6 | (24.0) | 11 | (44.0) | 8 | (32.0) | 0 | (0.0) | ||||
| pT2 | 23 | (22.5) | 13 | (56.5) | 3 | (13.0) | 7 | (30.4) | 0 | (0.0) | ||||
| pT3 | 18 | (17.6) | 12 | (66.7) | 3 | (16.7) | 1 | (5.6) | 2 | (11.1) | ||||
| pT4 | 15 | (14.7) | 10 | (66.7) | 2 | (13.3) | 3 | (20.0) | 0 | (0.0) | ||||
| Tumor grade 1 | 13.769 | 0.032 * | 0.260 | Moderate | ||||||||||
| G1 | 18 | (17.6) | 1 | (5.6) | 10 | (55.6) | 6 | (33.3) | 1 | (5.6) | ||||
| G2 | 25 | (24.5) | 13 | (52.0) | 9 | (36.0) | 3 | (12.0) | 0 | (0.0) | ||||
| G3 | 59 | (57.8) | 29 | (49.2) | 16 | (27.1) | 12 | (20.3) | 2 | (3.4) | ||||
| Lymph node metastasis | 0.154 | 0.985 | - | - | ||||||||||
| Yes | 24 | (23.5) | 17 | (70.8) | 3 | (12.5) | 3 | (12.5) | 1 | (4.2) | ||||
| No | 31 | (30.4) | 23 | (74.2) | 4 | (12.9) | 3 | (9.7) | 1 | (3.2) | ||||
| N/A | 47 | (46.1) | - | - | - | - | - | - | - | - | ||||
| Metastasis | 16.309 | 0.001 * | 0.400 | Strong | ||||||||||
| Yes | 27 | (26.5) | 20 | (74.1) | 3 | (11.1) | 3 | (11.1) | 1 | (3.7) | ||||
| No | 75 | (73.5) | 23 | (30.7) | 32 | (42.7) | 18 | (24.0) | 2 | (2.7) | ||||
| Recurrence | 5.611 | 0.132 | - | - | ||||||||||
| Yes | 63 | (61.8) | 21 | (33.3) | 24 | (38.1) | 16 | (25.4) | 2 | (3.2) | ||||
| No | 39 | (38.2) | 22 | (56.4) | 11 | (28.2) | 5 | (12.8) | 1 | (2.6) | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chin, F.-W.; Hussin, H.; Chau, D.-M.; Ong, T.-A.; Yunus, R.; Abdul Razack, A.H.; Yusoff, K.; Chan, S.-C.; Veerakumarasivam, A. Differential Protein Expression Patterns of HOXA13 and HOXB13 Are Associated with Bladder Cancer Progression. Diagnostics 2023, 13, 2636. https://doi.org/10.3390/diagnostics13162636
Chin F-W, Hussin H, Chau D-M, Ong T-A, Yunus R, Abdul Razack AH, Yusoff K, Chan S-C, Veerakumarasivam A. Differential Protein Expression Patterns of HOXA13 and HOXB13 Are Associated with Bladder Cancer Progression. Diagnostics. 2023; 13(16):2636. https://doi.org/10.3390/diagnostics13162636
Chicago/Turabian StyleChin, Fee-Wai, Huzlinda Hussin, De-Ming Chau, Teng-Aik Ong, Rosna Yunus, Azad Hassan Abdul Razack, Khatijah Yusoff, Soon-Choy Chan, and Abhi Veerakumarasivam. 2023. "Differential Protein Expression Patterns of HOXA13 and HOXB13 Are Associated with Bladder Cancer Progression" Diagnostics 13, no. 16: 2636. https://doi.org/10.3390/diagnostics13162636
APA StyleChin, F.-W., Hussin, H., Chau, D.-M., Ong, T.-A., Yunus, R., Abdul Razack, A. H., Yusoff, K., Chan, S.-C., & Veerakumarasivam, A. (2023). Differential Protein Expression Patterns of HOXA13 and HOXB13 Are Associated with Bladder Cancer Progression. Diagnostics, 13(16), 2636. https://doi.org/10.3390/diagnostics13162636





