The Conceptual Independence of Health Status, Respiratory Symptoms and Dyspnea in Chronic Obstructive Pulmonary Disease in Real Clinical Practice
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measurements
2.3. Patient-Reported Measurements
2.4. Statistical Methods
3. Results
3.1. Subject Characteristics
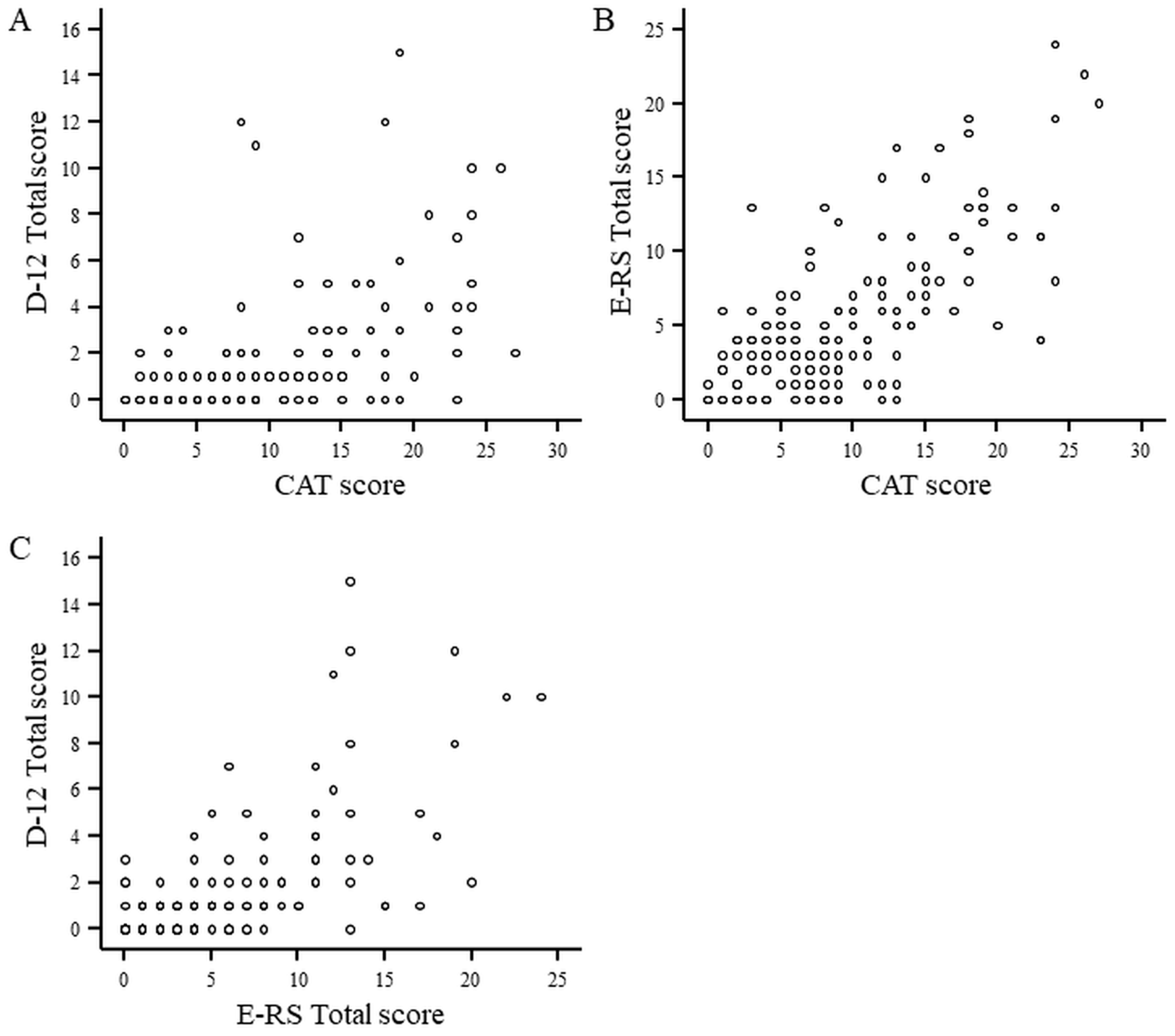
3.2. Distribution of Scores and Correlation between Tools
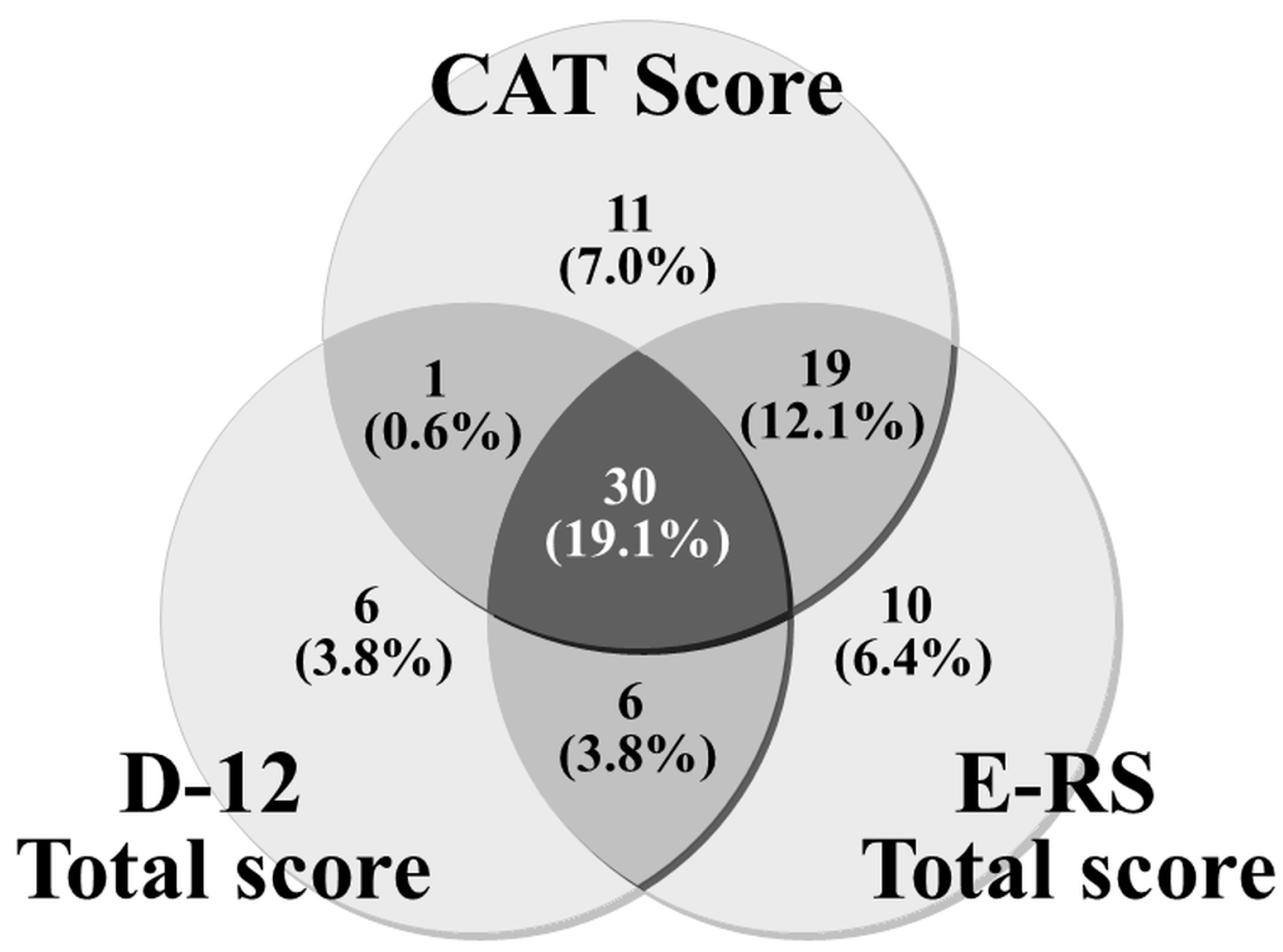
3.3. Relationship between Tools Using the Thresholds
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ekstrom, M.; Sundh, J.; Larsson, K. Patient reported outcome measures in chronic obstructive pulmonary disease: Which to use? Expert Rev. Respir. Med. 2016, 10, 351–362. [Google Scholar] [CrossRef]
- Jahagirdar, D.; Kroll, T.; Ritchie, K.; Wyke, S. Patient-reported outcome measures for chronic obstructive pulmonary disease: The exclusion of people with low literacy skills and learning disabilities. Patient 2013, 6, 11–21. [Google Scholar] [CrossRef]
- Jones, P.W.; Quirk, F.H.; Baveystock, C.M.; Littlejohns, P. A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory Questionnaire. Am. Rev. Respir. Dis. 1992, 145, 1321–1327. [Google Scholar] [CrossRef]
- Jones, P.; Harding, G.; Wiklund, I.; Berry, P.; Leidy, N. Improving the process and outcome of care in COPD: Development of a standardised assessment tool. Prim. Care Respir. J. 2009, 18, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.W.; Brusselle, G.; Dal Negro, R.W.; Ferrer, M.; Kardos, P.; Levy, M.L.; Perez, T.; Soler Cataluna, J.J.; van der Molen, T.; Adamek, L.; et al. Properties of the COPD assessment test in a cross-sectional European study. Eur. Respir. J. 2011, 38, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.W.; Tabberer, M.; Chen, W.H. Creating scenarios of the impact of COPD and their relationship to COPD Assessment Test (CAT) scores. BMC Pulm. Med. 2011, 11, 42. [Google Scholar] [CrossRef] [PubMed]
- Yorke, J.; Moosavi, S.H.; Shuldham, C.; Jones, P.W. Quantification of dyspnoea using descriptors: Development and initial testing of the Dyspnoea-12. Thorax 2010, 65, 21–26. [Google Scholar] [CrossRef]
- Yorke, J.; Swigris, J.; Russell, A.M.; Moosavi, S.H.; Ng Man Kwong, G.; Longshaw, M.; Jones, P.W. Dyspnea-12 is a valid and reliable measure of breathlessness in patients with interstitial lung disease. Chest 2011, 139, 159–164. [Google Scholar] [CrossRef]
- Yorke, J.; Armstrong, I. The assessment of breathlessness in pulmonary arterial hypertension: Reliability and validity of the Dyspnoea-12. Eur. J. Cardiovasc. Nurs. 2014, 13, 506–514. [Google Scholar] [CrossRef]
- Hajiro, T.; Nishimura, K.; Tsukino, M.; Ikeda, A.; Koyama, H.; Izumi, T. Comparison of discriminative properties among disease-specific questionnaires for measuring health-related quality of life in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 1998, 157, 785–790. [Google Scholar] [CrossRef] [PubMed]
- Vestbo, J.; Hurd, S.S.; Agusti, A.G.; Jones, P.W.; Vogelmeier, C.; Anzueto, A.; Barnes, P.J.; Fabbri, L.M.; Martinez, F.J.; Nishimura, M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease: GOLD Executive Summary. Am. J. Respir. Crit. Care Med. 2013, 187, 347–365. [Google Scholar] [CrossRef]
- Jones, P.W.; Adamek, L.; Nadeau, G.; Banik, N. Comparisons of health status scores with MRC grades in COPD: Implications for the GOLD 2011 classification. Eur. Respir. J. 2013, 42, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Rhee, C.K.; Kim, J.W.; Hwang, Y.I.; Lee, J.H.; Jung, K.S.; Lee, M.G.; Yoo, K.H.; Lee, S.H.; Shin, K.C.; Yoon, H.K. Discrepancies between modified Medical Research Council dyspnea score and COPD assessment test score in patients with COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2015, 10, 1623–1631. [Google Scholar] [CrossRef] [PubMed]
- Tsiligianni, I.G.; Alma, H.J.; de Jong, C.; Jelusic, D.; Wittmann, M.; Schuler, M.; Schultz, K.; Kollen, B.J.; van der Molen, T.; Kocks, J.W. Investigating sensitivity, specificity, and area under the curve of the Clinical COPD Questionnaire, COPD Assessment Test, and Modified Medical Research Council scale according to GOLD using St George’s Respiratory Questionnaire cutoff 25 (and 20) as reference. Int. J. Chron. Obstruct. Pulmon. Dis. 2016, 11, 1045–1052. [Google Scholar] [CrossRef] [PubMed]
- Mittal, R.; Chhabra, S.K. GOLD Classification of COPD: Discordance in Criteria for Symptoms and Exacerbation Risk Assessment. COPD 2017, 14, 1–6. [Google Scholar] [CrossRef]
- Cheng, S.L.; Lin, C.H.; Wang, C.C.; Chan, M.C.; Hsu, J.Y.; Hang, L.W.; Perng, D.W.; Yu, C.J.; Wang, H.C.; Taiwan Clinical Trial Consortium for Respiratory, D. Comparison between COPD Assessment Test (CAT) and modified Medical Research Council (mMRC) dyspnea scores for evaluation of clinical symptoms, comorbidities and medical resources utilization in COPD patients. J. Formos. Med. Assoc. 2019, 118, 429–435. [Google Scholar] [CrossRef]
- Moya-Alvarez, V.; Quevedo-Marin, J.L.; Ji, Z.; Navarro-Jimenez, C.; Jimenez-Garcia, R.; Lopez-de-Andres, A.; Perez-Trullen, A.; de Miguel-Diez, J. Variation in Assignment of the COPD Patients into a GOLD Group According to Symptoms Severity. Int. J. Chron. Obstruct. Pulmon. Dis. 2020, 15, 1987–1995. [Google Scholar] [CrossRef]
- Casanova, C.; Marin, J.M.; Martinez-Gonzalez, C.; de Lucas-Ramos, P.; Mir-Viladrich, I.; Cosio, B.; Peces-Barba, G.; Solanes-Garcia, I.; Aguero, R.; Feu-Collado, N.; et al. Differential Effect of Modified Medical Research Council Dyspnea, COPD Assessment Test, and Clinical COPD Questionnaire for Symptoms Evaluation within the New GOLD Staging and Mortality in COPD. Chest 2015, 148, 159–168. [Google Scholar] [CrossRef]
- Ertan Yazar, E.; Niksarlioglu, E.Y.; Yigitbas, B.; Bayraktaroglu, M. How to Utilize CAT and mMRC Scores to Assess Symptom Status of Patients with COPD in Clinical Practice? Medeni Med. J. 2022, 37, 173–179. [Google Scholar] [CrossRef]
- Leidy, N.K.; Wilcox, T.K.; Jones, P.W.; Murray, L.; Winnette, R.; Howard, K.; Petrillo, J.; Powers, J.; Sethi, S.; Group, E.-P.S. Development of the EXAcerbations of Chronic Obstructive Pulmonary Disease Tool (EXACT): A patient-reported outcome (PRO) measure. Value Health 2010, 13, 965–975. [Google Scholar] [CrossRef] [PubMed]
- Leidy, N.K.; Wilcox, T.K.; Jones, P.W.; Roberts, L.; Powers, J.H.; Sethi, S.; Group, E.-P.S. Standardizing measurement of chronic obstructive pulmonary disease exacerbations. Reliability and validity of a patient-reported diary. Am. J. Respir. Crit. Care Med. 2011, 183, 323–329. [Google Scholar] [CrossRef]
- Leidy, N.K.; Murray, L.T.; Monz, B.U.; Nelsen, L.; Goldman, M.; Jones, P.W.; Dansie, E.J.; Sethi, S. Measuring respiratory symptoms of COPD: Performance of the EXACT- Respiratory Symptoms Tool (E-RS) in three clinical trials. Respir. Res. 2014, 15, 124. [Google Scholar] [CrossRef]
- Leidy, N.K.; Sexton, C.C.; Jones, P.W.; Notte, S.M.; Monz, B.U.; Nelsen, L.; Goldman, M.; Murray, L.T.; Sethi, S. Measuring respiratory symptoms in clinical trials of COPD: Reliability and validity of a daily diary. Thorax 2014, 69, 443–449. [Google Scholar] [CrossRef][Green Version]
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.; van der Grinten, C.P.; Gustafsson, P.; et al. Standardisation of spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef]
- Sasaki, H.; Nakamura, M.; Kida, K.; Kambe, M.; Takahashi, K.; Fujimura, M. Reference values for spirogram and blood gas analysis in Japanese adults. J. Jpn. Respir. Soc. 2001, 39, S1–S17. [Google Scholar]
- Tsuda, T.; Suematsu, R.; Kamohara, K.; Kurose, M.; Arakawa, I.; Tomioka, R.; Kawayama, T.; Hoshino, T.; Aizawa, H. Development of the Japanese version of the COPD Assessment Test. Respir. Investig. 2012, 50, 34–39. [Google Scholar] [CrossRef]
- Nishimura, K.; Oga, T.; Nakayasu, K.; Taniguchi, H.; Ogawa, T.; Watanabe, F.; Arizono, S.; Kusunose, M.; Sanda, R.; Shibayama, A.; et al. Comparison between tools for measuring breathlessness: Cross-sectional validation of the Japanese version of the Dyspnoea-12. Clin. Respir. J. 2021, 15, 1201–1209. [Google Scholar] [CrossRef] [PubMed]
- Hyland, M.E.; Sodergren, S.C. Development of a new type of global quality of life scale, and comparison of performance and preference for 12 global scales. Qual. Life Res. 1996, 5, 469–480. [Google Scholar] [CrossRef]
- Nishimura, K.; Oga, T.; Ikeda, A.; Hajiro, T.; Tsukino, M.; Koyama, H. Comparison of health-related quality of life measurements using a single value in patients with asthma and chronic obstructive pulmonary disease. J. Asthma 2008, 45, 615–620. [Google Scholar] [CrossRef]
- Nishimura, K.; Oga, T.; Nakayasu, K.; Ogasawara, M.; Hasegawa, Y.; Mitsuma, S. How different are COPD-specific patient reported outcomes, health status, dyspnoea and respiratory symptoms? An observational study in a working population. BMJ Open 2019, 9, e025132. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, K.; Mitsuma, S.; Kobayashi, A.; Yanagida, M.; Nakayasu, K.; Hasegawa, Y.; Jones, P.W. COPD and disease-specific health status in a working population. Respir. Res. 2013, 14, 61. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pinto, L.M.; Gupta, N.; Tan, W.; Li, P.Z.; Benedetti, A.; Jones, P.W.; Bourbeau, J.; Can, C.s.g. Derivation of normative data for the COPD assessment test (CAT). Respir. Res. 2014, 15, 68. [Google Scholar] [CrossRef] [PubMed]
| Mean | SD | Max. | Min. | Correlations (Rs) with | |||||
|---|---|---|---|---|---|---|---|---|---|
| D-12 Total Score | CAT Score | E-RS Total Score | |||||||
| Age | years | 75.1 | 6.8 | 89.0 | 51.0 | — | — | — | |
| BMI | kg/m2 | 22.7 | 3.3 | 35.7 | 14.0 | — | — | — | |
| Cumulative Smoking | pack-years | 57.7 | 30.9 | 204.0 | 10.0 | — | — | — | |
| SVC | % pred. | 95.7 | 18.1 | 145.9 | 56.7 | −0.250 ** | −0.207 ** | −0.203 * | |
| FEV1 | % pred. | 69.8 | 20.4 | 132.5 | 21.8 | −0.340 *** | −0.335 *** | −0.381 *** | |
| FEV1/FVC | % | 56.3 | 10.8 | 69.9 | 22.4 | −0.251 ** | −0.311 *** | −0.391 *** | |
| RV(1) | % pred. | 125.1 | 63.7 | 718.9 | 28.4 | — | 0.189 * | 0.214 ** | |
| RV/TLC (1) | % | 44.9 | 9.7 | 85.1 | 18.1 | — | 0.242 ** | 0.258 ** | |
| DLco (2) | % pred. | 53.4 | 20.6 | 163.9 | 8.0 | −0.183 * | −0.285 *** | −0.248 ** | |
| PaO2 (3) | mmHg | 79.2 | 8.9 | 101.8 | 56.6 | −0.188 * | −0.301 *** | −0.289 *** | |
| SGRQ Total Score | (0–100) | 22.8 | 15.3 | 63.1 | 0.9 | 0.602 *** | 0.667 *** | 0.636 *** | |
| SGRQ Symptoms | (0–100) | 37.9 | 20.0 | 85.3 | 0.0 | 0.508 *** | 0.549 *** | 0.586 *** | |
| SGRQ Activity | (0–100) | 32.1 | 23.6 | 87.2 | 0.0 | 0.553 *** | 0.616 *** | 0.578 *** | |
| SGRQ Impact | (0–100) | 13.1 | 13.1 | 55.2 | 0.0 | 0.533 *** | 0.553 *** | 0.519 *** | |
| Hyland Scale Score | (0–100) | 66.6 | 16.0 | 100 | 20.0 | −0.381 *** | −0.513 *** | −0.437 *** | |
| D-12 Total Score | (0–36) | 1.5 | 2.6 | 15.0 | 0.0 | NA | 0.603 *** | 0.655 *** | |
| CAT Score | (0–40) | 9.1 | 6.7 | 27.0 | 0.0 | 0.603 *** | NA | 0.675 *** | |
| E-RS Total Score | (0–40) | 5.2 | 5.2 | 24.0 | 0.0 | 0.655 *** | 0.675 *** | NA | |
| Stage 1 (n = 53) | Stage 2 (n = 79) | Stage 3 + 4 (n = 25) | |||
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |||
| Age | years | 75.5 ± 6.6 | 74.8 ± 7.0 | 74.7 ± 6.7 | |
| BMI | kg/m2 | 23.1 ± 2.8 | 22.9 ± 3.6 | 21.4 ± 3.1 | |
| Cumulative Smoking | pack-years | 47.4 ** ± 23.3 | 63.5 ± 34.0 | 61.4 ± 30.5 | |
| SVC | % pred. | 109.7 *** ± 12.6 | 92.0 §§§ ± 15.8 | 77.8 ¶¶¶ ± 13.0 | |
| FEV1 | % pred. | 91.7 *** ± 10.1 | 64.9 §§§ ± 9.1 | 38.7 ¶¶¶ ± 8.7 | |
| FEV1/FVC | % | 63.7 *** ± 4.9 | 56.4 §§§ ± 8.4 | 40.2 ¶¶¶ ± 9.2 | |
| RV (1) | % pred. | 108.5 ± 31.5 | 122.0 §§§ ± 47.4 | 169.3 ¶¶ ± 119.0 | |
| RV/TLC (1) | % | 39.3 *** ± 7.3 | 45.4 §§§ ± 8.8 | 54.7 ¶¶¶ ± 8.7 | |
| DLco (2) | % pred. | 58.9 * ± 14.3 | 53.5 §§§ ± 23.1 | 41.4 ¶ ± 19.3 | |
| PaO2 (3) | mmHg | 81.7 ± 8.9 | 79.2 §§ ± 8.9 | 74.4 ¶ ± 6.9 | |
| SGRQ Total Score | (0–100) | 15.0 ** ± 9.9 | 22.7 §§§ ± 14.3 | 40.0 ¶¶¶ ± 13.9 | |
| SGRQ Symptoms | (0–100) | 31.2 ± 16.3 | 37.0 §§§ ± 19.9 | 54.9 ¶¶¶ ± 17.9 | |
| SGRQ Activity | (0–100) | 20.4 ** ± 19.0 | 31.7 §§§ ± 21.4 | 58.1 ¶¶¶ ± 18.2 | |
| SGRQ Impact | (0–100) | 7.1 * ± 7.7 | 13.3 §§§ ± 12.7 | 25.1 ¶¶ ± 15.1 | |
| Hyland Scale Score | (0–100) | 72 ± 15 | 67 §§§ ± 15 | 54 ¶¶ ± 14 | |
| D-12 Total Score | (0–36) | 0.8 ± 1.8 | 1.4 §§§ ± 2.3 | 3.7 ¶¶ ± 3.9 | |
| CAT Score | (0–40) | 7.0 ± 5.4 | 8.3 §§§ ± 6.1 | 16.3 ¶¶¶ ± 6.7 | |
| E-RS Total Score | (0–40) | 3.4 ± 3.5 | 4.8 §§§ ± 5.0 | 10.2 ¶¶¶ ± 6.0 | |
| Patient-Reported Outcomes | Possible Score Range | Items | Score Distribution | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n) | Mean | SD | Median | 75th Percentile | 25th Percentile | Max. | Min. | Floor Effect | Ceiling Effect | |||
| D-12 Total Score | 0–36 | 12 | 1.5 | 2.6 | 1.0 | 2.0 | 0.0 | 15.0 | 0.0 | 47.8% | 0% | |
| D-12 Physical Score | 0–21 | 7 | 1.4 | 2.1 | 1.0 | 2.0 | 0.0 | 10.0 | 0.0 | 48.4% | 0% | |
| D-12 Affective Score | 0–15 | 5 | 0.2 | 0.9 | 0.0 | 0.0 | 0.0 | 5.0 | 0.0 | 93.6% | 0% | |
| CAT Score | 0–40 | 8 | 9.1 | 6.7 | 8.0 | 13.0 | 3.0 | 27.0 | 0.0 | 5.1% | 0% | |
| E-RS Total Score | 0–40 | 11 | 5.2 | 5.2 | 4.0 | 8.0 | 1.0 | 24.0 | 0.0 | 19.7% | 0% | |
| RS—Breathlessness | 0–17 | 5 | 2.3 | 3.2 | 0.0 | 4.0 | 0.0 | 15.0 | 0.0 | 50.3% | 0% | |
| RS—Cough and Sputum | 0–11 | 3 | 1.9 | 1.7 | 2.0 | 3.0 | 0.0 | 7.0 | 0.0 | 32.5% | 0% | |
| RS—Chest Symptoms | 0–12 | 3 | 1.0 | 1.6 | 0.0 | 2.0 | 0.0 | 6.0 | 0.0 | 60.5% | 0% | |
| Real-World Clinic n (%) | On the Hypothesis | |||||
|---|---|---|---|---|---|---|
| D-12 | ∩ | E-RS | ∩ | CAT | 30 (19.1%) | present, a centrical position |
| ∩ | E-RS | ∩ | CAT | 19 (12.1%) | possible | |
| ∩ | ∩ | CAT | 11 (7.0%) | possible | ||
| ∩ | E-RS | ∩ | 10 (6.4%) | no | ||
| D-12 | ∩ | E-RS | ∩ | 6 (3.8%) | no | |
| D-12 | ∩ | ∩ | 6 (3.8%) | no | ||
| D-12 | ∩ | ∩ | CAT | 1 (0.6%) | no | |
| ∩ | ∩ | 74 (47.1%) | present |
| COPD Assessment Test (CAT) and Evaluating Respiratory Symptoms in COPD (E-RS) | |||
| E-RS Total Score | |||
| 0–4 | 5 or more | ||
| CAT Score | 0–9 | 80 (51.0%) | 16 (10.2%) |
| 10 or more | 12 (7.6%) | 49 (31.2%) | |
| COPD Assessment Test (CAT) and Dyspnea-12 (D-12) | |||
| D-12 Total Score | |||
| 0–1 | 2 or more | ||
| CAT Score | 0–9 | 84 (53.5%) | 12 (7.6%) |
| 10 or more | 30 (19.1%) | 31 (19.7%) | |
| Evaluating Respiratory Symptoms in COPD (E-RS) and Dyspnea-12 (D-12) | |||
| D-12 Total Score | |||
| 0–1 | 2 or more | ||
| E-RS Total Score | 0–4 | 85 (54.1%) | 7 (4.5%) |
| 5 or more | 29 (18.5%) | 36 (22.9%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nishimura, K.; Kusunose, M.; Mori, M.; Shibayama, A.; Nakayasu, K. The Conceptual Independence of Health Status, Respiratory Symptoms and Dyspnea in Chronic Obstructive Pulmonary Disease in Real Clinical Practice. Diagnostics 2023, 13, 2492. https://doi.org/10.3390/diagnostics13152492
Nishimura K, Kusunose M, Mori M, Shibayama A, Nakayasu K. The Conceptual Independence of Health Status, Respiratory Symptoms and Dyspnea in Chronic Obstructive Pulmonary Disease in Real Clinical Practice. Diagnostics. 2023; 13(15):2492. https://doi.org/10.3390/diagnostics13152492
Chicago/Turabian StyleNishimura, Koichi, Masaaki Kusunose, Mio Mori, Ayumi Shibayama, and Kazuhito Nakayasu. 2023. "The Conceptual Independence of Health Status, Respiratory Symptoms and Dyspnea in Chronic Obstructive Pulmonary Disease in Real Clinical Practice" Diagnostics 13, no. 15: 2492. https://doi.org/10.3390/diagnostics13152492
APA StyleNishimura, K., Kusunose, M., Mori, M., Shibayama, A., & Nakayasu, K. (2023). The Conceptual Independence of Health Status, Respiratory Symptoms and Dyspnea in Chronic Obstructive Pulmonary Disease in Real Clinical Practice. Diagnostics, 13(15), 2492. https://doi.org/10.3390/diagnostics13152492







