Ultrasound or MRI in the Evaluation of Anterior Talofibular Ligament (ATFL) Injuries: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Material and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Data Extraction
2.5. Risk of Bias
2.6. Data Synthesis and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Waterman, B.R.; Owens, B.D.; Davey, S.; Zacchilli, M.A.; Belmont, P.J. The Epidemiology of Ankle Sprains in the United States. J. Bone Jt. Surg. 2010, 92, 2279–2284. [Google Scholar] [CrossRef] [PubMed]
- Waterman, C.B.R.; Belmont, P.; Cameron, K.; Svoboda, L.S.J.; Alitz, C.C.J.; Owens, L.B.D. Risk Factors for Syndesmotic and Medial Ankle Sprain: Role of sex, sport, and level of competition. Am. J. Sports Med. 2011, 39, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Lynch, S.A. Assessment of the Injured Ankle in the Athlete. J. Athl. Train. 2002, 37, 406–412. [Google Scholar] [PubMed]
- Liu, K.; Gustavsen, G.; Royer, T.; Wikstrom, E.A.; Glutting, J.; Kaminski, T.W. Increased Ligament Thickness in Previously Sprained Ankles as Measured by Musculoskeletal Ultrasound. J. Athl. Train. 2015, 50, 193–198. [Google Scholar] [CrossRef]
- Fong, D.T.-P.; Hong, Y.; Chan, L.K.; Yung, P.S.-H.; Chan, K.-M. A Systematic Review on Ankle Injury and Ankle Sprain in Sports. Sports Med. 2007, 37, 73–94. [Google Scholar] [CrossRef]
- Matsui, K.; Takao, M.; Tochigi, Y.; Ozeki, S.; Glazebrook, M. Anatomy of anterior talofibular ligament and calcaneofibular ligament for minimally invasive surgery: A systematic review. Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 1892–1902. [Google Scholar] [CrossRef]
- Kumai, T.; Takakura, Y.; Rufai, A.; Milz, S.; Benjamin, M. The functional anatomy of the human anterior talofibular ligament in relation to ankle sprains. J. Anat. 2002, 200, 457–465. [Google Scholar] [CrossRef]
- Herzog, M.M.; Kerr, Z.Y.; Marshall, S.W.; Wikstrom, E.A. Epidemiology of Ankle Sprains and Chronic Ankle Instability. J. Athl. Train. 2019, 54, 603–610. [Google Scholar] [CrossRef]
- Sisson, L.; Croy, T.; Saliba, S.; Hertel, J. Comparison of ankle arthrometry to stress ultrasound imaging in the assessment of ankle laxity in healthy adults. Int. J. Sports Phys. Ther. 2011, 6, 297–305. [Google Scholar]
- Hertel, J.; Denegar, C.R.; Monroe, M.M.; Stokes, W.L. Talocrural and subtalar joint instability after lateral ankle sprain. Med. Sci. Sports Exerc. 1999, 31, 1501–1508. [Google Scholar] [CrossRef]
- Lee, B.H.; Choi, K.-H.; Seo, D.Y.; Choi, S.M.; Kim, G.L. Diagnostic validity of alternative manual stress radiographic technique detecting subtalar instability with concomitant ankle instability. Knee Surg. Sport. Traumatol. Arthrosc. 2016, 24, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Frost, S.C.L.; Amendola, A. Is Stress Radiography Necessary in the Diagnosis of Acute or Chronic Ankle Instability? Clin. J. Sport Med. 1999, 9, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Amendola, A. Controversies in Diagnosis and Management of Syndesmosis Injuries of the Ankle. Foot Ankle 1992, 13, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Thès, A.; Odagiri, H.; Elkaïm, M.; Lopes, R.; Andrieu, M.; Cordier, G.; Molinier, F.; Benoist, J.; Colin, F.; Boniface, O.; et al. Arthroscopic classification of chronic anterior talo-fibular ligament lesions in chronic ankle instability. Orthop. Traumatol. Surg. Res. 2018, 104, S207–S211. [Google Scholar] [CrossRef]
- Oae, K.; Takao, M.; Uchio, Y.; Ochi, M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skelet. Radiol. 2010, 39, 41–47. [Google Scholar] [CrossRef]
- Mizrahi, D.J.; Nazarian, L.N.; Parker, L. Evaluation of the Anterior Talofibular Ligament via Stress Sonography in Asymptomatic and Symptomatic Populations. J. Ultrasound Med. 2018, 37, 1957–1963. [Google Scholar] [CrossRef]
- Nazarian, L.N.; Rawool, N.M.; Martin, C.E.; Schweitzer, M.E. Synovial fluid in the hindfoot and ankle: Detection of amount and distribution with US. Radiology 1995, 197, 275–278. [Google Scholar] [CrossRef]
- Nazarian, L.N.; Gulvartian, N.V.; Freeland, E.C.; Chao, W. Ultrasound-Guided Percutaneous Needle Fenestration and Corticosteroid Injection for Anterior and Anterolateral Ankle Impingement. Foot Ankle Spec. 2018, 11, 61–66. [Google Scholar] [CrossRef]
- Martinoli, C.; Court-Payen, M.; Michaud, J.; Padua, L.; Altafini, L.; Marchetti, A.; Perez, M.M.; Valle, M.; Hovgaard, C.; Haugegaard, M.; et al. Imaging of Neuropathies about the Ankle and Foot. Semin. Musculoskelet. Radiol. 2010, 14, 344–356. [Google Scholar] [CrossRef]
- Rossi, F.; Zaottini, F.; Picasso, R.; Martinoli, C.; Tagliafico, A.S. Ankle and Foot Ultrasound: Reliability of Side-to-Side Comparison of Small Anatomic Structures. J. Ultrasound Med. 2019, 38, 2143–2153. [Google Scholar] [CrossRef]
- Sconfienza, L.M.; Albano, D.; Allen, G.; Bazzocchi, A.; Bignotti, B.; Chianca, V.; de Castro, F.F.; Drakonaki, E.E.; Gallardo, E.; Gielen, J.; et al. Clinical indications for musculoskeletal ultrasound updated in 2017 by European Society of Musculoskeletal Radiology (ESSR) consensus. Eur. Radiol. 2018, 28, 5338–5351. [Google Scholar] [CrossRef]
- Sconfienza, L.M.; Adriaensen, M.; Albano, D.; Alcala-Galiano, A.; Allen, G.; Gómez, M.P.A.; Aringhieri, G.; Bazzocchi, A.; Beggs, I.; Chianca, V.; et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: A Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)—Part VI, foot and ankle. Eur. Radiol. 2022, 32, 1384–1394. [Google Scholar] [CrossRef] [PubMed]
- Zaottini, F.; Picasso, R.; Pistoia, F.; Perez, M.M.; Möller, I.; Rossi, F.; Bruns, A.; Tagliafico, A.S.; Martinoli, C. Ultrasound Imaging Guide for Assessment of the Intrinsic Ligaments Stabilizing the Subtalar and Midtarsal Joints. Semin. Musculoskelet. Radiol. 2020, 24, 113–124. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Gün, C.; Vandenberk, N.; Karagöz, A.; Sentürk, G.; Oyar, O. Bedside ultrasonography by emergency physicians for anterior talofibular ligament injury. J. Emergencies Trauma Shock. 2013, 6, 195–198. [Google Scholar] [CrossRef]
- Xu, Y.; He, L.; Han, Y.; Duan, D.; Ouyang, L. Evaluation of 3-Dimensional Magnetic Resonance Imaging (3D MRI) in Diagnosing Anterior Talofibular Ligament Injury. Experiment 2021, 27, e927920. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.; Elamvazuthi, I.; Jeoti, V.; George, J.; Swain, A.; Kumar, D. Impacting clinical evaluation of anterior talofibular ligament injuries through analysis of ultrasound images. Biomed. Eng. Online 2016, 15, 13. [Google Scholar] [CrossRef]
- Park, H.; Lee, S.; Park, N.; Rho, M.; Chung, E.; Park, J.; Park, S. Three-dimensional isotropic T2-weighted fast spin-echo (VISTA) ankle MRI versus two-dimensional fast spin-echo T2-weighted sequences for the evaluation of anterior talofibular ligament injury. Clin. Radiol. 2016, 71, 349–355. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kim, Y.B.; Kim, T.G.; Lee, S.W.; Park, S.H.; Lee, H.J.; Choi, Y.J.; Koh, Y.G. Reliability and Validity of Magnetic Resonance Imaging for the Evaluation of the Anterior Talofibular Ligament in Patients Undergoing Ankle Arthroscopy. Arthroscopy 2015, 31, 1540–1547. [Google Scholar] [CrossRef]
- Basha, M.A.A.; Eldib, D.B.; Zaitoun, M.M.A.; Ghandour, T.M.; Aly, T.; Mostafa, S.; Atta, D.S.; Algazzar, H.Y. The Added Diagnostic Value of the Bright Rim Sign to Conventional MRI Assessment of Anterior Talofibular Ligament Disruption. Acad. Radiol. 2021, 28, e247–e257. [Google Scholar] [CrossRef]
- Hua, Y.; Yang, Y.; Chen, S.; Cai, Y. Ultrasound examination for the diagnosis of chronic anterior talofibular ligament injury. Acta Radiol. 2012, 53, 1142–1145. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Thukral, C.L.; Gupta, K.; Singh, A. Comparison of high resolution ultrasonography with clinical findings in patients with ankle pain. J. Ultrason. 2018, 18, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Kemmochi, M.; Sasaki, S.; Fujisaki, K.; Oguri, Y.; Kotani, A.; Ichimura, S. A new classification of anterior talofibular ligament injuries based on ultrasonography findings. J. Orthop. Sci. 2016, 21, 770–778. [Google Scholar] [CrossRef]
- De Ranieri, D.; Lin, S. Applications of Musculoskeletal Ultrasound in the Pediatric Emergency Department. Pediatr. Ann. 2021, 50, e411–e418. [Google Scholar] [CrossRef]
- Kristen, K.-H.; Aspang, J.S.U.; Wiedemann, J.; Hartenbach, F.; Platzgummer, H. Reliability of ultrasonography measurement of the anterior talofibular ligament (ATFL) length in healthy subjects (in vivo), based on examiner experience and patient positioning. J. Exp. Orthop. 2019, 6, 30. [Google Scholar] [CrossRef] [PubMed]




| Author | Year | Country | Design | Modality | Study Population (No. of Patients) | Mean Age (y) and Range | Classification | Diagnosis/Type of Injury | Duration of Study | Reference Standard |
|---|---|---|---|---|---|---|---|---|---|---|
| Lee et al. [11] | 2016 | Korea | R | MRI (3T) | 34 | 29 (13–53) | Normal (1) Partial tear (22) Complete tear (11) | / | 11 months | Arthroscopy |
| Kim et al. [29] | 2015 | Korea | R | MRI (1.5T) | 79 | 34.6 (21–67) | / | Various ankle disorder | 10 months | Arthroscopy |
| Park et al. [28] | 2016 | Korea | R | MRI (3T/3D FSE) | 101 | 38.3 (10–80) | / | Chronic ankle pain Swelling Acute pain after a sprain | 5 months | Arthroscopy |
| Basha et al. [30] | 2021 | Egypt | R | MRI (1.5T) | 62 | 36.9 (17–52) | / | Acute sprain (28) Chronic ankle instability (18) Recurrent ankle sprain (15) | 8 months | Arthroscopy |
| Xu et al. [26] | 2021 | China | P | MRI (3T) | 45 | 32.1 (18–58) | / | Chronic ankle instability | 14 months | Arthroscopy |
| Oae et al. [15] | 2010 | Japan | R | US (9 MHz) | 34 | 29 (13–55) | Top (fibula) Middle Below (talus) | 19 acute causes 15 chronic cause | 2 years and 8 months | Arthroscopy |
| Hua et al. [31] | 2012 | China | R | US (5–17 MHz) | 83 | 32.2 (17–57) | Tear: partial or total | Chronic ankle instability, impingement syndrome, osteochondral lesions, arthritis, and others | 12 months | Arthroscopy |
| Gün et al. [25] | 2013 | Turkey | P | US (7.5 MHz) | 65 | 34 (18–72) | Normal Abnormal | Inversion-type ankle injury | 12 months | MRI |
| Singh et al. [27] | 2016 | Malaysia | R | US (5–13 MHz) | 25 | 34 (18–60) | Healthy Tear injury Thickened injury | High ankle sprain | / | US |
| Patient Selection | Index Test (MRI or US) | Reference Standard | Flow and Timing | ||
|---|---|---|---|---|---|
| Lee et al. [11] | 2016 | + | + | + | + |
| Kim et al. [29] | 2015 | + | + | + | + |
| Park et al. [28] | 2016 | + | + | + | + |
| Basha et al. [30] | 2021 | + | + | + | + |
| Xu et al. [26] | 2021 | + | + | + | + |
| Oae et al. [15] | 2010 | + | + | + | + |
| Hua et al. [31] | 2012 | + | + | + | + |
| Gün et al. [25] | 2013 | + | + | ? | ? |
| Singh et al. [27] | 2016 | + | + | - | - |
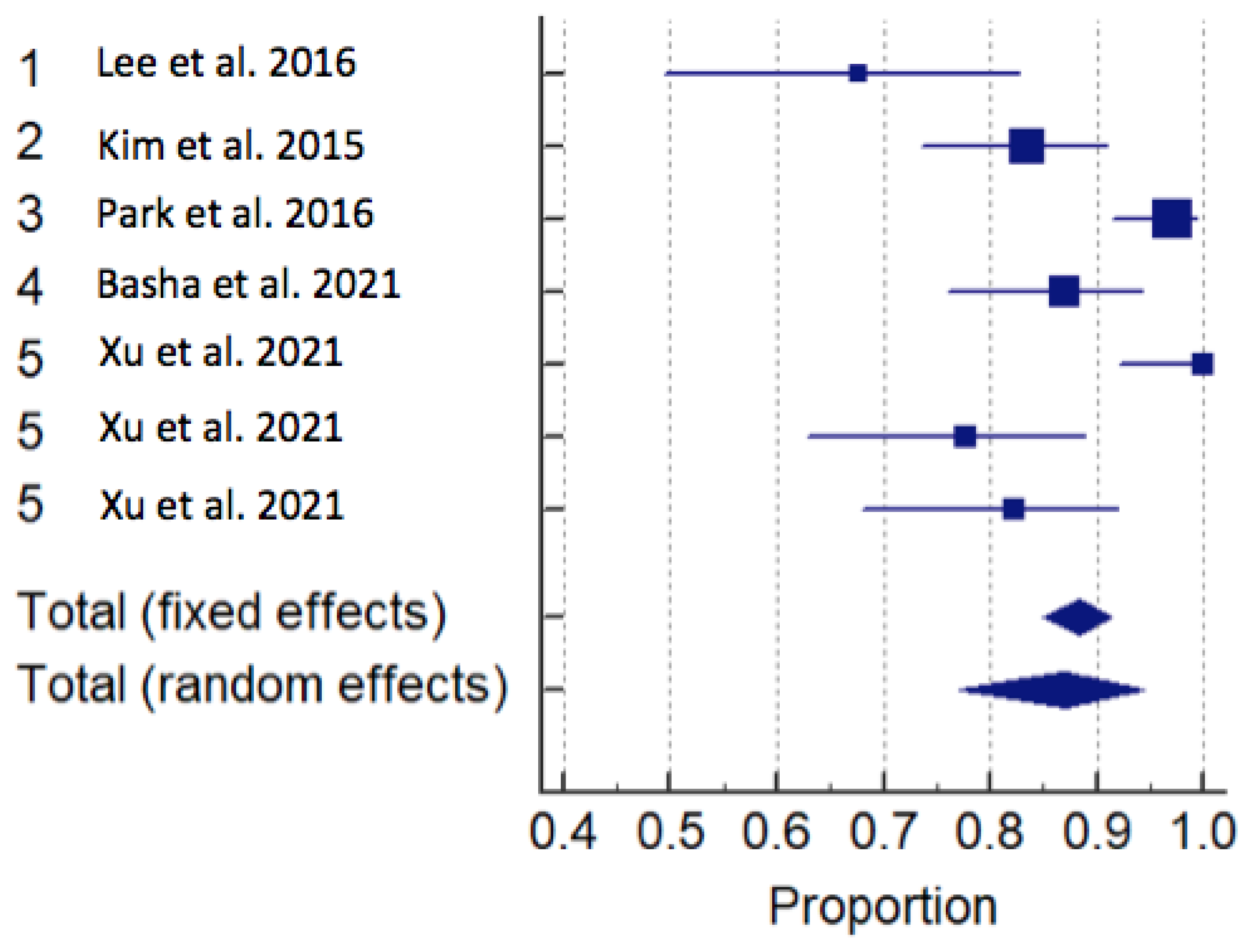
| Study | Sample Size | Proportion (%) (Sensitivity) | 95% CI |
|---|---|---|---|
| US SENSITIVITY | |||
| Total (fixed effects) | 207 | 96,884 | 93,551 to 98,783 |
| Total (random effects) | 207 | 97,018 | 93,802 to 99,090 |
| MRI SENSITIVITY | |||
| Total (fixed effects) | 411 | 88,501 | 85,047 to 91,397 |
| Total (random effects) | 411 | 86,978 | 77,162 to 94,344 |
| US SPECIFICITY | |||
| Total (fixed effects) | 207 | 88,396 | 83,287 to 92,386 |
| Total (random effects) | 207 | 84,447 | 55,235 to 99,396 |
| MRI SPECIFICITY | |||
| Total (fixed effects) | 411 | 81,375 | 76,717 to 85,452 |
| Total (random effects) | 411 | 82,547 | 66,808 to 93,975 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colò, G.; Bignotti, B.; Costa, G.; Signori, A.; Tagliafico, A.S. Ultrasound or MRI in the Evaluation of Anterior Talofibular Ligament (ATFL) Injuries: Systematic Review and Meta-Analysis. Diagnostics 2023, 13, 2324. https://doi.org/10.3390/diagnostics13142324
Colò G, Bignotti B, Costa G, Signori A, Tagliafico AS. Ultrasound or MRI in the Evaluation of Anterior Talofibular Ligament (ATFL) Injuries: Systematic Review and Meta-Analysis. Diagnostics. 2023; 13(14):2324. https://doi.org/10.3390/diagnostics13142324
Chicago/Turabian StyleColò, Gabriele, Bianca Bignotti, Giacomo Costa, Alessio Signori, and Alberto Stefano Tagliafico. 2023. "Ultrasound or MRI in the Evaluation of Anterior Talofibular Ligament (ATFL) Injuries: Systematic Review and Meta-Analysis" Diagnostics 13, no. 14: 2324. https://doi.org/10.3390/diagnostics13142324
APA StyleColò, G., Bignotti, B., Costa, G., Signori, A., & Tagliafico, A. S. (2023). Ultrasound or MRI in the Evaluation of Anterior Talofibular Ligament (ATFL) Injuries: Systematic Review and Meta-Analysis. Diagnostics, 13(14), 2324. https://doi.org/10.3390/diagnostics13142324