Heart Rate Recovery as a Predictor of Long-Term Adverse Events after Negative Exercise Testing in Patients with Chest Pain and Pre-Test Probability of Coronary Artery Disease from 15% to 65%
Abstract
:1. Introduction
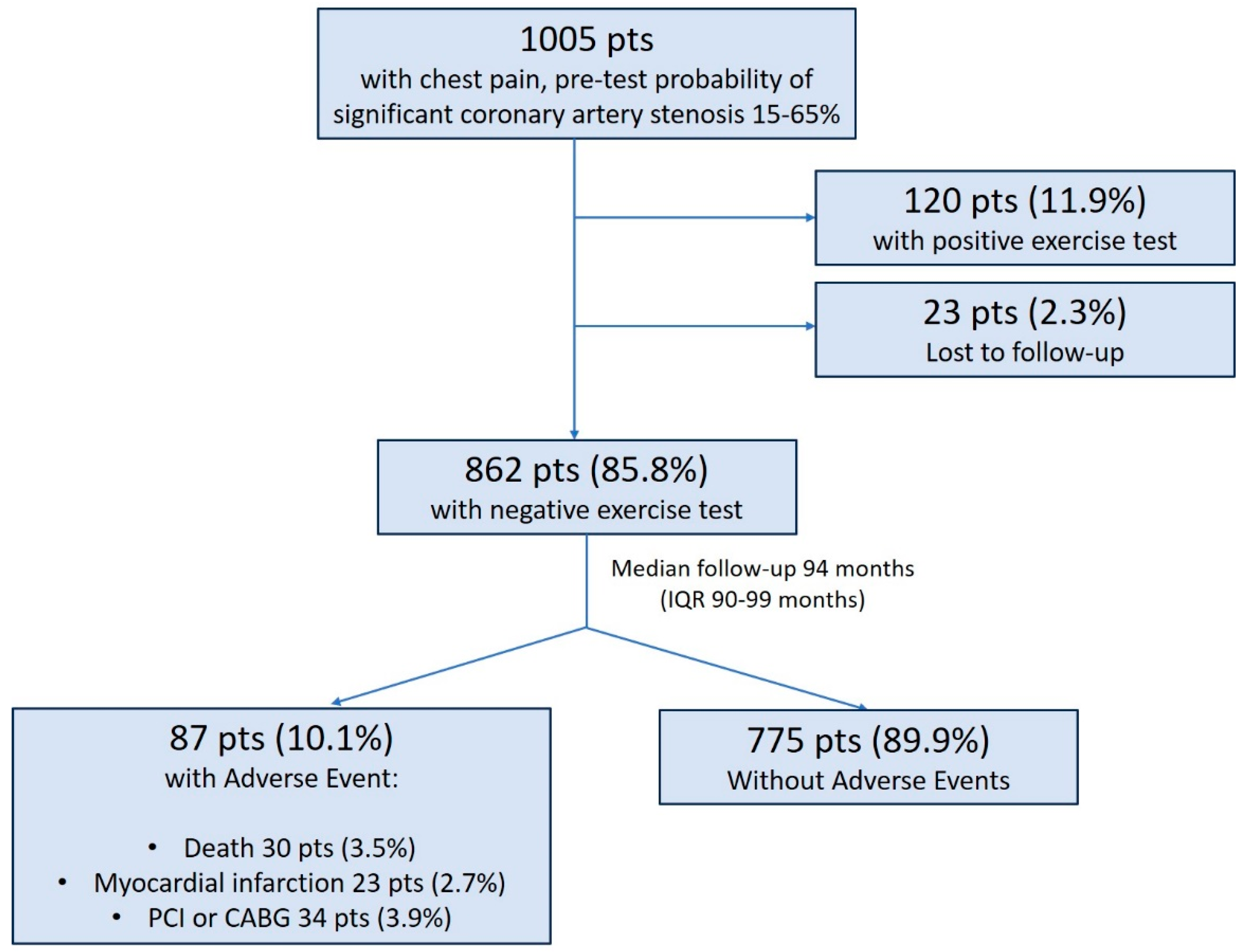
2. Materials and Methods
2.1. Patient Population
2.2. Exercise Testing
2.3. Statistical Analysis
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hachamovitch, R.; Berman, D.S.; Shaw, L.J.; Kiat, H.; Cohen, I.; Cabico, J.A.; Friedman, J.; Diamond, G.A. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: Differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998, 97, 535–543. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marwick, T.H.; Case, C.; Vasey, C.; Allen, S.; Short, L.; Thomas, J.D. Prediction of mortality by exercise echocardiography: A strategy for combination with the Duke treadmill score. Circulation 2001, 103, 2566–2571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, S.S.; Qureshi, E.; Sherrid, M.V.; Chaudhry, F.A. Practical applications in stress echocardiography: Risk stratification and prognosis in patients with known or suspectedischemic heart disease. J. Am. Coll. Cardiol. 2003, 42, 1084–1090. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rozanski, A.; Gransar, H.; Hayes, S.W.; Min, J.; Friedman, J.D.; Thomson, L.E.; Berman, D.S. Temporal Trends in the Frequency of Inducible Myocardial Ischemia During Cardiac Stress Testing: 1991 to 2009. J. Am. Coll. Cardiol. 2013, 61, 1054–1065. [Google Scholar] [CrossRef] [Green Version]
- Metz, L.D.; Beattie, M.; Hom, R.; Redberg, R.F.; Grady, D.; Fleischmann, K.E. The Prognostic Value of Normal Exercise Myocardial Perfusion Imaging and Exercise Echocardiography: A Meta-Analysis. J. Am. Coll. Cardiol. 2007, 49, 227–237. [Google Scholar] [CrossRef] [Green Version]
- Smulders, M.W.; Jaarsma, C.; Nelemans, J.P.; Bekkers, S.C.A.M.; Bucerius, J.; Leiner, T.; Crijns, H.J.G.M.; Wildberger, J.E.; Schalla, S. Comparison of the prognostic value of negative non-invasive cardiac investigations in patients with suspected or known coronary arterydisease–a meta-analysis. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 980–987. [Google Scholar] [CrossRef] [Green Version]
- Hoffmann, U.; Ferencik, M.; Udelson, J.E.; Picard, M.H.; Truong, Q.A.; Patel, M.R.; Huang, M.; Pencina, M.; Mark, D.B.; Heitner, J.F.; et al. PROMISE Investigators. Prognostic Value of Noninvasive Cardiovascular Testing in Patients With Stable Chest Pain: Insights From the PROMISE Trial (Prospective Multicenter Imaging Study for Evaluation of Chest Pain). Circulation 2017, 135, 2320–2332. [Google Scholar] [CrossRef]
- Aguire, A.D.; Arbab-Zadeh, A.; Soeda, T.; Fuster, V.; Jang, I.K. Optical Coherence Tomography of Plaque Vulnerability and Rupture: JACC Focus Seminar Part 1/3. J. Am. Coll. Cardiol. 2021, 78, 1257–1265. [Google Scholar] [CrossRef]
- Kubo, T.; Ino, Y.; Mintz, G.S.; Shiono, Y.; Shimamura, K.; Takahata, M.; Terada, K.; Higashioka, D.; Emori, H.; Wada, T.; et al. Optical coherence tomography detection of vulnerable plaques at high risk of developing acute coronary syndrome. Eur. Heart J. Cardiovasc. Imaging 2021, 22, 1376–1384. [Google Scholar] [CrossRef]
- Fabris, E.; Berta, B.; Roleder, T.; Hermanides, R.S.; Ijsselmuiden, A.J.; Kauer, F.; Alfonso, F.; von Birgelen, C.; Escaned, J.; Camaro, C.; et al. Thin-Cap Fibroatheroma Rather Than Any Lipid Plaques Increases the Risk of Cardiovascular Events in Diabetic Patients: Insights From the COMBINE OCT–FFR Trial. Circ. Cardiovasc. Interv. 2022, 15, 011728. [Google Scholar] [CrossRef]
- Lauer, M.S.; Okin, P.M.; Larson, M.G.; Evans, J.C.; Levy, D. Impaired heart rate response to graded exercise. Prognostic implications of chronotropic incompetence in the Framingham Heart Study. Circulation 1996, 93, 1520–1526. [Google Scholar] [CrossRef] [PubMed]
- Lauer, M.S.; Mehta, R.; Pashkow, F.J.; Okin, P.M.; Lee, K.; Marwick, T.H. Association of chronotropic incompetence with echocardiographic ischemia and prognosis. J. Am. Coll. Cardiol. 1998, 32, 1280–1286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mora, S.; Redberg, R.F.; Cui, Y.; Whiteman, M.K.; Flaws, J.A.; Sharrett, A.R.; Blumenthal, R.S. Ability of exercise testing to predict cardiovascular and all-cause death in asymptomatic women: A 20-year follow-up of the lipid research clinics prevalence study. JAMA 2003, 290, 1600–1607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morshedi-Meibodi, A.; Larson, M.G.; Levy, D.; O’donnell, C.J.; Vasan, R.S. Heart rate recovery after treadmill exercise testing and risk of cardiovascular disease events (The Framingham Heart Study). Am. J. Cardiol. 2002, 90, 848–852. [Google Scholar] [CrossRef]
- Genders, T.S.; Steyerberg, E.W.; Alkadhi, H.; Leschka, S.; Desbiolles, L.; Nieman, K.; Galema, T.W.; Meijboom, W.B.; Mollet, N.R.; de Feyter, P.J.; et al. A clinical prediction rule for the diagnosis of coronary artery disease: Validation, updating, and extension. Eur. Heart J. 2011, 32, 1316–1330. [Google Scholar] [CrossRef]
- Handelsman, Y.; Bloomgarden, Z.; Grunberger, G.; Umpierrez, G.; Zimmerman, R.S.; Bailey, T.S.; Blonde, L.; Bray, G.A.; Cohen, A.J.; Dagogo-Jack, S.; et al. American Association of Clinical Endocrinologist and American College of Endocrinology-a clinical practical guideline for developing a diabetes melitus comprehensive care plan-2015. AACE/ACE Diabetes Guidel. Endocr. Pract. 2015, 21 (Suppl. 1), 1–87. [Google Scholar] [CrossRef] [Green Version]
- Mancia, G.; De Backer, G.; Dominiczak, A.; Cifkova, R.; Fagard, R.; Germano, G.; Grassi, G.; Heagerty, A.M.; Kjeldsen, S.E.; Laurent, S.; et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 2007, 28, 1462–1536. [Google Scholar] [CrossRef]
- Catapano, A.L.; Graham, I.; De Backer, G.; Wiklund, O.; Chapman, M.J.; Drexel, H.; Hoes, A.W.; Jennings, C.S.; Landmesser, U.; Pedersen, T.R.; et al. ESC Scientific Document Group. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Eur. Heart J. 2016, 37, 2999–3058. [Google Scholar] [CrossRef] [Green Version]
- Lauer, M.S.; Blackstone, E.H.; Young, J.B.; Topol, E.J. Cause of death in clinical research: Time for a reassessment? J. Am.Coll. Cardiol. 1999, 34, 618–620. [Google Scholar] [CrossRef] [Green Version]
- Gottlieb, S.S. Dead is dead—Artificial definitions are no substitute. Lancet 1997, 349, 662–663. [Google Scholar] [CrossRef]
- Watanabe, J.; Thamilarasan, M.; Blackstone, E.H.; Thomas, J.D.; Lauer, M.S. Heart rate recovery immediately after treadmill exercise and left ventricular systolic dysfunction as predictors of mortality: The case of stress echocardiography. Circulation 2001, 104, 1911–1916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vivekananthan, D.P.; Blackstone, E.H.; Pothier, C.E.; Lauer, M.S. Heart rate recovery after exercise is a predictor of mortality, independent of the angiographic severity of coronary disease. J. Am. Coll. Cardiol. 2003, 42, 831–838. [Google Scholar] [CrossRef] [PubMed]
- Wilkoff, B.L.; E Miller, R. Exercise testing for chronotropic assessment. Cardiol. Clin. 1992, 10, 705–717. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Bierig, M.; Devereux, R.B.; Flachskampf, F.A.; Foster, E.; Pellikka, P.A.; Picard, M.H.; Roman, M.J.; Seward, J.; Shanewise, J.S.; et al. American Society of Echocardiography’s Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: A report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J. Am. Soc. Echocardiogr. 2005, 18, 1440–1463. [Google Scholar]
- Cortigiani, L.; Urluescu, M.-L.; Coltelli, M.; Carpeggiani, C.; Bovenzi, F.; Picano, E. Apparent Declining Prognostic Value of a Negative Stress Echocardiography Based on Regional Wall Motion Abnormalities in Patients With Normal Resting Left Ventricular Function Due to the Changing Referral Profile of the Population Under Study. Circ. Cardiovasc. Imaging 2019, 12, e008564. [Google Scholar] [CrossRef]
- Bangalore, S.; Gopinath, D.; Yao, S.S.; Chaudhry, F.A. Risk Stratification Using Stress Echocardiography: Incremental Prognostic Value over Historic, Clinical, and Stress Electrocardiographic Variables Across a Wide Spectrum of Bayesian Pretest Probabilities for Coronary Artery Disease. J. Am. Soc. Echocardiogr. 2007, 20, 244–252. [Google Scholar] [CrossRef]
- Mudrick, D.W.; Cowper, P.A.; Shah, B.R.; Patel, M.R.; Jensen, N.C.; Peterson, E.D.; Douglas, P.S. Downstream procedures and outcomes after stress testing for chest pain without known coronary artery disease in the United States. Am. Heart J. 2012, 163, 454–461. [Google Scholar] [CrossRef] [Green Version]
- Schnur, S.S.K.; Achim, A.; Toth, G.G. Clinical application of results of the ISCHEMIA trial. Trends Cardiovasc. Med. 2023, 33, 125–130. [Google Scholar] [CrossRef]
- Cortigiani, L.; Borelli, L.; Raciti, M.; Bovenzi, F.; Picano, E.; Molinaro, S.; Sicari, R. Prediction of Mortality by Stress Echocardiography in 2835 Diabetic and 11 305 Nondiabetic Patients. Circ. Cardiovasc. Imaging 2015, 8, e002757. [Google Scholar] [CrossRef] [Green Version]
- Pecanha, T.; Silva-Junior, N.D.; Forjaz, C.L. Heart rate recovery: Autonomic determinants, methods of assessment and association with mortality and cardiovascular diseases. Clin. Physiol. Funct. Imaging 2014, 34, 327–339. [Google Scholar] [CrossRef]
- Pierpont, G.L.; Stolpman, D.R.; Gornick, C.C. Heart rate recovery post-exercise as an index of parasympathetic activity. J. Auton. Nerv. Syst. 2000, 80, 169–174. [Google Scholar] [CrossRef] [PubMed]
- La Rovere, M.T.; Pinna, G.D.; Hohnloser, S.H. Baroreflex sensitivity and heart rate variability in the identification of patients at risk for life-threatening arrhythmias: Implications for clinical trials. Circulation 2001, 103, 2072–2077. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Snader, C.E.; Lauer, M.S. Heart-Rate Recovery Immediately after Exercise as a Predictor of Mortality. N. Engl. J. Med. 1999, 341, 1351–1357. [Google Scholar] [CrossRef] [PubMed]
- Nishime, E.O.; Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Lauer, M.S. Heart Rate Recovery and Treadmill Exercise Score as Predictors of Mortality in Patients Referred for Exercise ECG. JAMA 2000, 284, 1392–1398. [Google Scholar] [CrossRef]
- Cole, C.R.; Foody, J.M.; Blackstone, E.H.; Lauer, M.S. Heart Rate Recovery after Submaximal Exercise Testing as a Predictor of Mortality in a Cardiovascularly Healthy Cohort. Ann. Intern. Med. 2000, 132, 552–555. [Google Scholar] [CrossRef]
- Diaz, L.A.; Brunken, R.C.; Blackstone, E.H.; Snader, C.E.; Lauer, M.S. Independent contribution of myocardial perfusion defects to exercise capacity and heart rate recovery for prediction of all-cause mortality in patients with known or suspected coronary heart disease. J. Am. Coll. Cardiol. 2001, 37, 1558–1564. [Google Scholar] [CrossRef] [Green Version]
- Gayda, M.; Bourassa, M.G.; Tardif, J.-C.; Fortier, A.; Juneau, M.; Nigam, A. Heart Rate Recovery After Exercise and Long-term Prognosis in Patients with Coronary Artery Disease. Can. J. Cardiol. 2012, 28, 201–207. [Google Scholar] [CrossRef]
- Qiu, S.; Cai, X.; Sun, Z.; Li, L.; Zuegel, M.; Steinacker, J.M.; Schumann, U. Heart Rate Recovery and Risk of Cardiovascular Events and All-Cause Mortality: A Meta-Analysis of Prospective Cohort Studies. J. Am. Heart Assoc. 2017, 6, e005505. [Google Scholar] [CrossRef] [Green Version]
- Park, J.-I.; Shin, S.-Y.; Park, S.K.; Barrett-Connor, E. Usefulness of the Integrated Scoring Model of Treadmill Tests to Predict Myocardial Ischemia and Silent Myocardial Ischemia in Community-Dwelling Adults (from the Rancho Bernardo Study). Am. J. Cardiol. 2015, 115, 1049–1055. [Google Scholar] [CrossRef] [Green Version]
- Huang, P.-H.; Leu, H.-B.; Chen, J.-W.; Cheng, C.-M.; Huang, C.-Y.; Tuan, T.-C.; Ding, P.Y.-A.; Lin, S.-J. Usefulness of attenuated heart rate recovery immediately after exercise to predict endothelial dysfunction in patients with suspected coronary artery disease. Am. J. Cardiol. 2004, 93, 10–13. [Google Scholar] [CrossRef]
- Jae, S.Y.; Ahn, E.S.; Heffernan, K.S.; Woods, J.A.; Lee, M.-K.; Park, W.H.; Fernhall, B. Relation of Heart Rate Recovery After Exercise to C-Reactive Protein and White Blood Cell Count. Am. J. Cardiol. 2007, 99, 707–710. [Google Scholar] [CrossRef]
- Fei, D.-Y.; Arena, R.; Arrowood, J.A.; Kraft, K.A. Relationship between arterial stiffness and heart rate recovery in apparently healthy adults. Vasc. Health Risk Manag. 2005, 1, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Kuo, H.-K.; Gore, J.M. Relation of heart rate recovery after exercise to insulin resistance and chronic inflammation in otherwise healthy adolescents and adults: Results from the National Health and Nutrition Examination Survey (NHANES) 1999–2004. Clin. Res. Cardiol. 2015, 104, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Jae, S.Y.; Kurl, S.; Laukkanen, J.; Yoon, E.S.; Choi, Y.-H.; Fernhall, B.; Franklin, B.A. Relation of heart rate recovery after exercise testing to coronary artery calcification. Ann. Med. 2017, 49, 404–410. [Google Scholar] [CrossRef]
- Jae, S.Y.; Carnethon, M.R.; Ahn, E.S.; Heffernan, K.S.; Choi, Y.-H.; Lee, M.-K.; Fernhall, B. Association between heart rate recovery after exercise testing and plasminogen activator inhibitor 1, tissue plasminogen activator, and fibrinogen in apparently healthy men. Atherosclerosis 2008, 197, 415–419. [Google Scholar] [CrossRef]
- Knuuti, J.; Wijns, W.; Saraste, A.; Capodanno, D.; Barbato, E.; Funck-Brentano, C.; Prescott, E.; Storey, R.F.; Deaton, C.; Cuisset, T.; et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 2020, 41, 407–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morrone, D.; Gentile, F.; Aimo, A.; Cameli, M.; Barison, A.; Picoi, M.E.; Guglielmo, M.; Villano, A.; DeVita, A.; Mandoli, G.E.; et al. Perspectives in noninvasive imaging for chronic coronary syndromes. Int. J. Cardiol. 2022, 365, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Shaw, L.J.; Veledar, E.; Wenger, N.K.; Mieres, J.H.; Hendel, R.H.; Boden, W.E.; Gulati, M.; Hachamovitch, R.; Arrighi, J.A.; Merz, C.N.B.; et al. Comparative effectiveness of exercise electrocardiography with or without myocardial perfusion single photon emission computed tomography in women with suspected coronary artery disease: Results from the What Is the Optimal Method for Ischemia Evaluation in Women (WOMEN) Trial. Circulation 2012, 125, e934–e935. [Google Scholar] [CrossRef] [Green Version]
- Elhendy, A.; Shub, C.; McCully, R.B.; Mahoney, D.W.; Burger, K.N.; A Pellikka, P.A. Exercise echocardiography for the prognostic stratification of patients with low pretest probability of coronary artery disease. Am. J. Med. 2001, 111, 18–23. [Google Scholar] [CrossRef]
- Ciampi, Q.; Zagatina, A.; Cortigiani, L.; Wierzbowska-Drabik, K.; Kasprzak, J.D.; Haberka, M.; Djordjevic-Dikic, A.; Beleslin, B.; Boshchenko, A.; Ryabova, T.; et al. Prognostic value of stressechocardiography assessed by ABCDE protocol. Eur. Heart J. 2021, 42, 3869–3878. [Google Scholar] [CrossRef]
- Gaibazzi, N.; Bergamaschi, L.; Pizzi, C.; Tuttolomondo, D. Resting global longitudinal strain and stress echocardiography to detect coronary artery disease burden. Eur. Heart J. Cardiovasc. Imaging 2023, 24, e86–e88. [Google Scholar] [CrossRef] [PubMed]
- Pletscher, M.; Walker, S.; Moschetti, K.; Pinget, C.; Wasserfallen, J.-B.; Greenwood, J.P.; Schwitter, J.; Girardin, F.R. Cost-effectiveness of functional cardiac imaging in the diagnostic work-up of coronary heart disease. Eur. Heart J. Qual. Care Clin. Outcomes 2016, 2, 201–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bedetti, G.; Pasanisi, E.M.; Pizzi, C.; Turchetti, G.; Lore, C. Economic analysis including long-term risks and costs of alternative diagnostic strategies to evaluate patients with chest pain. Cardiovasc. Ultrasound 2008, 6, 21. [Google Scholar] [CrossRef] [Green Version]
- Picano, E.; Ciampi, Q.; Citro, R.; D’andrea, A.; Scali, M.C.; Cortigiani, L.; Olivotto, I.; Mori, F.; Galderisi, M.; Costantino, M.F.; et al. Stress echo 2020: The international stress echo study in ischemic and non-ischemic heart disease. Cardiovasc. Ultrasound 2017, 15, 3. [Google Scholar] [CrossRef] [Green Version]
- Lanza, G.A.; Morrone, D.; Pizzi, C.; Tritto, I.; Bergamaschi, L.; De Vita, A.; Villano, A.; Crea, F. Diagnostic approach for coronary microvascular dysfunction in patients with chest pain and no obstructive coronary artery disease. Trends Cardiovasc. Med. 2022, 32, 448–453. [Google Scholar] [CrossRef] [PubMed]
- Kenkre, T.S.; Malhotra, P.; Johnson, B.D.; Handberg, E.M.; Thompson, D.V.; Marroquin, O.C.; Rogers, W.J.; Pepine, C.J.; Merz, C.N.B.; Kelsey, S.F.; et al. Ten-Year Mortality in the WISE Study (Women’s Ischemia Syndrome Evaluation). Circ. Cardiovasc. Qual. Outcomes 2017, 10, e003863. [Google Scholar] [CrossRef]
- Woudstra, J.; Vink, C.E.M.; Schipaanboord, D.J.M.; Eringa, E.C.; Ruijter, H.M.D.; Feenstra, R.G.T.; Boerhout, C.K.M.; Beijk, M.A.M.; de Waard, G.A.; Ong, P.; et al. Meta-analysis and systematic review of coronary vasospasm in ANOCA patients: Prevalence, clinical features and prognosis. Front. Cardiovasc. Med. 2023, 10, 1129159. [Google Scholar] [CrossRef]
- Pasupathy, S.; Air, T.; Dreyer, R.P.; Tavella, R.; Beltrame, J.F. Systematic Review of Patients Presenting With Suspected Myocardial Infarction and Nonobstructive Coronary Arteries. Circulation 2015, 131, 861–870. [Google Scholar] [CrossRef] [Green Version]
- Achim, A.; Stanek, A.; Homorodean, C.; Spinu, M.; Onea, H.L.; Lazăr, L.; Marc, M.; Ruzsa, Z.; Olinic, D.M. Approaches to Peripheral Artery Disease in Diabetes: Are There Any Differences? Int. J. Environ. Res. Public Health 2022, 19, 9801. [Google Scholar] [CrossRef]

| Variable | All Patients (n = 862) | Patients with AE a (n = 87, 10.1%) | Patients without AE a (n = 775, 89.9%) | p Value |
|---|---|---|---|---|
| Male gender | 364 (42.2%) | 56 (64.4%) | 308 (39.7%) | <0.001 |
| Age (years) | 56 ± 10 | 60 ± 10 | 55 ± 10 | <0.001 |
| Hypertension | 603 (70%) | 67 (77%) | 536 (69.2%) | 0.130 |
| Hyperlypoproteinemia | 488 (56.6%) | 50 (57.5%) | 438 (56.5%) | 0.865 |
| Smoker | 326 (37.9%) | 38 (44.2%) | 288 (37.2%) | 0.203 |
| Diabetes | 118 (13.7%) | 24 (27.6%) | 94 (12.1%) | <0.001 |
| Family history of CAD b | 509 (59%) | 49 (56.3%) | 460 (59.4%) | 0.585 |
| Typical chest pain | 403 (48.4%) | 71 (81.6%) | 498 (64.3%) | 0.001 |
| Duration of the test (minutes) | 7.4 ± 2.7 | 7.0 ± 2.7 | 7.5 ± 2.8 | 0.132 |
| Chronotropic index < 0.8 | 411 (47.7%) | 54 (62.1%) | 364 (47%) | 0.008 |
| Achieved target heart rate | 674 (78.2%) | 62 (71.3%) | 612 (79%) | 0.099 |
| Maximum achieved SBP c (mmHg) | 180 ± 21 | 183 ± 21 | 179 ± 22 | 0.126 |
| Maximum achieved DBP d (mmHg) | 100 ± 11 | 100 ± 11 | 100 ± 11 | 0.946 |
| Slow HRR e | 45 (5.2%) | 11 (12.6%) | 34 (4.4%) | 0.001 |
| Variable | HR h | Univariate Analysis | B | p Value | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|---|---|
| 95% CI i | HR h | 95% CI i | p Value | ||||||
| Lower Level | Upper Level | Lower Level | Upper Level | ||||||
| Male gender | 2.600 | 1.676 | 4.032 | 0.955 | <0.001 | 2.525 | 1.441 | 4.425 | 0.001 |
| Age (years) | 1.045 | 1.021 | 1.070 | 0.044 | <0.001 | 1.042 | 1.017 | 1.067 | 0.001 |
| Hypertension | 1.542 | 0.935 | 2.543 | 0.433 | 0.089 | ||||
| Hyperlipoproteinemia | 1.086 | 0.698 | 1.634 | 0.066 | 0.762 | ||||
| Smoking | 1.395 | 0.910 | 2.139 | 0.333 | 0.126 | ||||
| Diabetes | 2.523 | 1.576 | 4.038 | 0.925 | <0.001 | 1.891 | 1.171 | 3.055 | 0.009 |
| Family history of CAD b | 0.894 | 0.585 | 1.365 | −0.113 | 0.603 | ||||
| Typical chest pain | 2.495 | 1.449 | 4.296 | 0.914 | 0.001 | 0.838 | 0.420 | 1.670 | 0.615 |
| SECHO c/SECG d | 0.989 | 0.641 | 1.525 | −0.011 | 0.959 | ||||
| Duration of the test (minutes) | 0.945 | 0.875 | 1.021 | −0.056 | 0.151 | ||||
| Achieved target heart rate | 0.682 | 0.429 | 1.086 | −0.382 | 0.107 | ||||
| Maximum achieved SBP e | 1.007 | 0.997 | 1.017 | 0.007 | 0.157 | ||||
| Maximum achieved DBP f | 1.000 | 0.982 | 1.019 | 0.000 | 0.976 | ||||
| Chronotropic index < 0.8 | 1.765 | 1.144 | 2.724 | −0.568 | 0.010 | 1.493 | 0.955 | 2.332 | 0.079 |
| Slow HRR g | 3.084 | 1.638 | 5.808 | 1.126 | <0.001 | 2.024 | 1.041 | 3.939 | 0.038 |
| Variable | All Patients (n = 862) | SECHO a (n = 321, 37.2%) | Stress ECG b (n = 541, 62.8%) | p Value |
|---|---|---|---|---|
| Male gender | 364 (42.2%) | 137 (42.7%) | 227 (42%) | 0.836 |
| Age | 56 ± 10 | 56 ± 9 | 56 ± 10 | 0.245 |
| Hypertension | 603 (70%) | 227 (70.7%) | 376 (69.5%) | 0.707 |
| Hyperlypoproteinemia | 488 (56.6%) | 190 (59.2%) | 298 (55.1%) | 0.240 |
| Smoker | 326 (37.9%) | 111 (34.7%) | 215 (39.7%) | 0.140 |
| Diabetes | 118 (13.7%) | 45 (14%) | 73 (13.5%) | 0.828 |
| Family history of CAD c | 509 (59%) | 190 (59.2%) | 319 (59%) | 0.948 |
| Typical chest pain | 293 (34%) | 119 (37.1%) | 174 (32.2%) | 0.141 |
| PTP d (%) | 40.7 ± 13.9 | 42.3 ± 14 | 39.7 ± 13.8 | 0.009 l |
| Duration of the test (minutes) | 7.4 ± 2.7 | 7.4 ± 2.9 | 7.5 ± 2.7 | 0.764 |
| Chronotropic index < 0.8 | 418 (48.5%) | 158 (49.2%) | 260 (48.1%) | 0.761 |
| Achieved target heart rate | 674 (78.2%) | 255 (79.4%) | 419 (77.4%) | 0.494 |
| Maximum achieved SBP e (mmHg) | 180 ± 21.1 | 180 ± 21.2 | 180.1 ± 21.1 | 0.814 |
| Maximum achieved DBP f (mmHg) | 100.4 ± 11.3 | 99.9 ± 12 | 100.5 ± 10.8 | 0.509 |
| Slow HRR g | 45 (5.2%) | 16 (5%) | 29 (5.4%) | 0.810 |
| AE h | 87 (10.1%) | 33 (10.3%) | 54 (10.0%) | 0.888 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giga, V.; Boskovic, N.; Djordjevic-Dikic, A.; Beleslin, B.; Nedeljkovic, I.; Stankovic, G.; Tesic, M.; Jovanovic, I.; Paunovic, I.; Aleksandric, S. Heart Rate Recovery as a Predictor of Long-Term Adverse Events after Negative Exercise Testing in Patients with Chest Pain and Pre-Test Probability of Coronary Artery Disease from 15% to 65%. Diagnostics 2023, 13, 2229. https://doi.org/10.3390/diagnostics13132229
Giga V, Boskovic N, Djordjevic-Dikic A, Beleslin B, Nedeljkovic I, Stankovic G, Tesic M, Jovanovic I, Paunovic I, Aleksandric S. Heart Rate Recovery as a Predictor of Long-Term Adverse Events after Negative Exercise Testing in Patients with Chest Pain and Pre-Test Probability of Coronary Artery Disease from 15% to 65%. Diagnostics. 2023; 13(13):2229. https://doi.org/10.3390/diagnostics13132229
Chicago/Turabian StyleGiga, Vojislav, Nikola Boskovic, Ana Djordjevic-Dikic, Branko Beleslin, Ivana Nedeljkovic, Goran Stankovic, Milorad Tesic, Ivana Jovanovic, Ivana Paunovic, and Srdjan Aleksandric. 2023. "Heart Rate Recovery as a Predictor of Long-Term Adverse Events after Negative Exercise Testing in Patients with Chest Pain and Pre-Test Probability of Coronary Artery Disease from 15% to 65%" Diagnostics 13, no. 13: 2229. https://doi.org/10.3390/diagnostics13132229
APA StyleGiga, V., Boskovic, N., Djordjevic-Dikic, A., Beleslin, B., Nedeljkovic, I., Stankovic, G., Tesic, M., Jovanovic, I., Paunovic, I., & Aleksandric, S. (2023). Heart Rate Recovery as a Predictor of Long-Term Adverse Events after Negative Exercise Testing in Patients with Chest Pain and Pre-Test Probability of Coronary Artery Disease from 15% to 65%. Diagnostics, 13(13), 2229. https://doi.org/10.3390/diagnostics13132229





