Inter-Rater Agreement for Diagnosing Adenomyosis Using Magnetic Resonance Imaging and Transvaginal Ultrasonography
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Eligibility Criteria
2.2. MRI Examination and Assessment
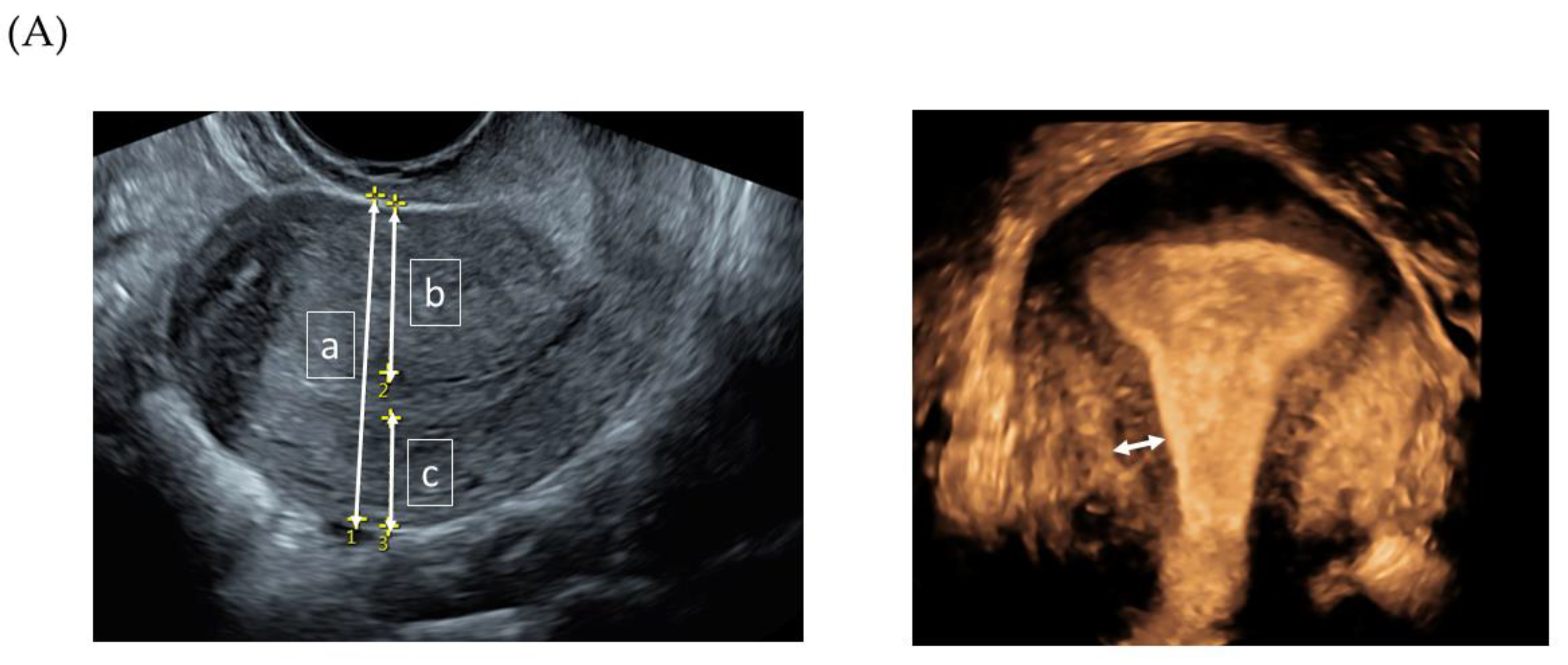
2.3. TVS Examination and Assessment
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bird, C.C.; McElin, T.W.; Manalo-Estrella, P. The elusive adenomyosis of the uterus—Revisited. Am. J. Obstet. Gynecol. 1972, 112, 583–593. [Google Scholar] [PubMed]
- Cockerham, A.Z. Adenomyosis: A Challenge in Clinical Gynecology. J. Midwifery Womens Health 2012, 57, 212–220. [Google Scholar] [PubMed]
- Pinzauti, S.; Lazzeri, L.; Tosti, C.; Centini, G.; Orlandini, C.; Luisi, S.; Zupi, E.; Exacoustos, C.; Petraglia, F. Transvaginal sonographic features of diffuse adenomyosis in 18–30-year-old nulligravid women without endometriosis: Association with symptoms. Ultrasound Obstet. Gynecol. 2015, 46, 730–736. [Google Scholar]
- Sammour, A.; Pirwany, I.; Usubutun, A.; Arseneau, J.; Tulandi, T. Correlations between extent and spread of adenomyosis and clinical symptoms. Gynecol. Obstet. Investig. 2002, 54, 213–216. [Google Scholar] [CrossRef]
- Bazot, M.; Darai, E. Role of transvaginal sonography and magnetic resonance imaging in the diagnosis of uterine adenomyosis. Fertil. Steril. 2018, 109, 389–397. [Google Scholar] [PubMed] [Green Version]
- Reinhold, C.; McCarthy, S.; Bret, P.M.; Mehio, A.; Atri, M.; Zakarian, R.; Glaude, Y.; Liang, L.; Seymour, R.J. Diffuse adenomyosis: Comparison of endovaginal US and MR imaging with histopathologic correlation. Radiology 1996, 199, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Bazot, M.; Cortez, A.; Darai, E.; Rouger, J.; Chopier, J.; Antoine, J.M.; Uzan, S. Ultrasonography compared with magnetic resonance imaging for the diagnosis of adenomyosis: Correlation with histopathology. Hum. Reprod. 2001, 16, 2427–2433. [Google Scholar] [CrossRef] [Green Version]
- Dueholm, M.; Lundorf, E.; Hansen, E.S.; Sorensen, J.S.; Ledertoug, S.; Olesen, F. Magnetic resonance imaging and transvaginal ultrasonography for the diagnosis of adenomyosis. Fertil. Steril. 2001, 76, 588–594. [Google Scholar]
- Tellum, T.; Matic, G.V.; Dormagen, J.B.; Nygaard, S.; Viktil, E.; Qvigstad, E.; Lieng, M. Diagnosing adenomyosis with MRI: A prospective study revisiting the junctional zone thickness cutoff of 12 mm as a diagnostic marker. Eur. Radiol. 2019, 29, 6971–6981. [Google Scholar]
- Dueholm, M.; Lundorf, E. Transvaginal ultrasound or MRI for diagnosis of adenornyosis. Curr. Opin. Obstet. Gynecol. 2007, 19, 505–512. [Google Scholar] [CrossRef]
- Reinhold, C.; Tafazoli, F.; Mehio, A.; Wang, L.; Atri, M.; Siegelman, E.S.; Rohoman, L. Uterine adenomyosis: Endovaginal US and MR imaging features with histopathologic correlation. Radiographics 1999, 19, S147–S160. [Google Scholar] [CrossRef]
- Dueholm, M.; Lundorf, E.; Sorensen, J.S.; Ledertoug, S.; Olesen, F.; Laursen, H. Reproducibility of evaluation of the uterus by transvaginal sonography, hysterosonographic examination, hysteroscopy and magnetic resonance imaging. Hum. Reprod. 2002, 17, 195–200. [Google Scholar] [CrossRef]
- Exacoustos, C.; Brienza, L.; Di Giovanni, A.; Szabolcs, B.; Romanini, M.E.; Zupi, E.; Arduini, D. Adenomyosis: Three-dimensional sonographic findings of the junctional zone and correlation with histology. Ultrasound Obstet. Gynecol. 2011, 37, 471–479. [Google Scholar] [CrossRef] [Green Version]
- van den Bosch, T.; Dueholm, M.; Leone, F.P.G.; Valentin, L.; Rasmussen, C.K.; Votino, A.; Van Schoubroeck, D.; Landolfo, C.; Installé, A.J.F.; Guerriero, S.; et al. Terms, definitions and measurements to describe sonographic features of myometrium and uterine masses: A consensus opinion from the Morphological Uterus Sonographic Assessment (MUSA) group. Ultrasound Obstet. Gynecol. 2015, 46, 284–298. [Google Scholar]
- Van den Bosch, T.; Van Schoubroeck, D. Ultrasound diagnosis of endometriosis and adenomyosis: State of the art. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 51, 16–24. [Google Scholar] [PubMed]
- Lazzeri, L.; Morosetti, G.; Centini, G.; Monti, G.; Zupi, E.; Piccione, E.; Exacoustos, C. A sonographic classification of adenomyosis: Interobserver reproducibility in the evaluation of type and degree of the myometrial involvement. Fertil. Steril. 2018, 110, 1154–1161.e3. [Google Scholar] [PubMed] [Green Version]
- Harmsen, M.J.; Van den Bosch, T.; de Leeuw, R.A.; Dueholm, M.; Exacoustos, C.; Valentin, L.; Hehenkamp, W.J.K.; Groenman, F.; De Bruyn, C.; Rasmussen, C.; et al. Consensus on revised definitions of Morphological Uterus Sonographic Assessment (MUSA) features of adenomyosis: Results of modified Delphi procedure. Ultrasound Obstet. Gynecol. 2022, 60, 118–131. [Google Scholar]
- Naftalin, J.; Hoo, W.; Nunes, N.; Mavrelos, D.; Nicks, H.; Jurkovic, D. Inter- and intraobserver variability in three-dimensional ultrasound assessment of the endometrial-myometrial junction and factors affecting its visualization. Ultrasound Obstet. Gynecol. 2012, 39, 587–591. [Google Scholar] [PubMed]
- Luciano, D.E.; Exacoustos, C.; Albrecht, L.; LaMonica, R.; Proffer, A.; Zupi, E.; Luciano, A.A. Three-Dimensional Ultrasound in Diagnosis of Adenomyosis: Histologic Correlation With Ultrasound Targeted Biopsies of the Uterus. J. Minim. Invasive Gynecol. 2013, 20, 803–810. [Google Scholar] [CrossRef] [PubMed]
- Puente, J.M.; Alcazar, J.L.; Martinez-Ten, P.; Bermejo, C.; Troncoso, M.T.; Garcia-Velasco, J.A. Interobserver agreement in the study of 2D and 3D sonographic criteria for adenomyosis. J. Endometr. Pelvic. Pain Disord. 2017, 9, 211–215. [Google Scholar] [CrossRef]
- Rasmussen, C.K.; Hansen, E.S.; Dueholm, M. Inter-rater agreement in the diagnosis of adenomyosis by 2- and 3-dimensional transvaginal ultrasonography. J. Ultrasound Med. 2019, 38, 657–666. [Google Scholar] [CrossRef]
- Rasmussen, C.K.; Van den Bosch, T.; Exacoustos, C.; Manegold-Brauer, G.; Benacerraf, B.R.; Froyman, W.; Landolfo, C.; Condorelli, M.; Egekvist, A.G.; Josefsson, H.; et al. Intra- and Inter-Rater Agreement Describing Myometrial Lesions Using Morphologic Uterus Sonographic Assessment: A Pilot Study. J. Ultrasound Med. 2019, 38, 2673–2683. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar]
- Brennan, P.; Silman, A. Statistical methods for assessing observer variability in clinical measures. BMJ 1992, 304, 1491–1494. [Google Scholar] [CrossRef] [Green Version]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420–428. [Google Scholar] [CrossRef]
- Rees, C.O.; Nederend, J.; Mischi, M.; van Vliet, H.; Schoot, B.C. Objective measures of adenomyosis on MRI and their diagnostic accuracy—A systematic review & meta-analysis. Acta Obstet. Gynecol. Scand. 2021, 100, 1377–1391. [Google Scholar]
- Tellum, T.; Nygaard, S.; Lieng, M. Noninvasive Diagnosis of Adenomyosis: A Structured Review and Meta-analysis of Diagnostic Accuracy in Imaging. J. Minim. Invasive Gynecol. 2020, 27, 408–418 e3. [Google Scholar] [CrossRef]
- Alcazar, J.L.; Vara, J.; Usandizaga, C.; Ajossa, S.; Pascual, M.A.; Guerriero, S. Transvaginal ultrasound versus magnetic resonance imaging for diagnosing adenomyosis: A systematic review and head-to-head meta-analysis. Int. J. Gynaecol. Obstet. 2023, 161, 397–405. [Google Scholar] [CrossRef]
- Bazot, M.; Bharwani, N.; Huchon, C.; Kinkel, K.; Cunha, T.M.; Guerra, A.; Manganaro, L.; Bunesch, L.; Kido, A.; Togashi, K.; et al. European society of urogenital radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur. Radiol. 2017, 27, 2765–2775. [Google Scholar] [PubMed] [Green Version]
- Tong, A.; VanBuren, W.M.; Chamié, L.; Feldman, M.; Hindman, N.; Huang, C.; Jha, P.; Kilcoyne, A.; Laifer-Narin, S.; Nicola, R.; et al. Recommendations for MRI technique in the evaluation of pelvic endometriosis: Consensus statement from the Society of Abdominal Radiology endometriosis disease-focused panel. Abdom. Radiol. 2020, 45, 1569–1586. [Google Scholar]
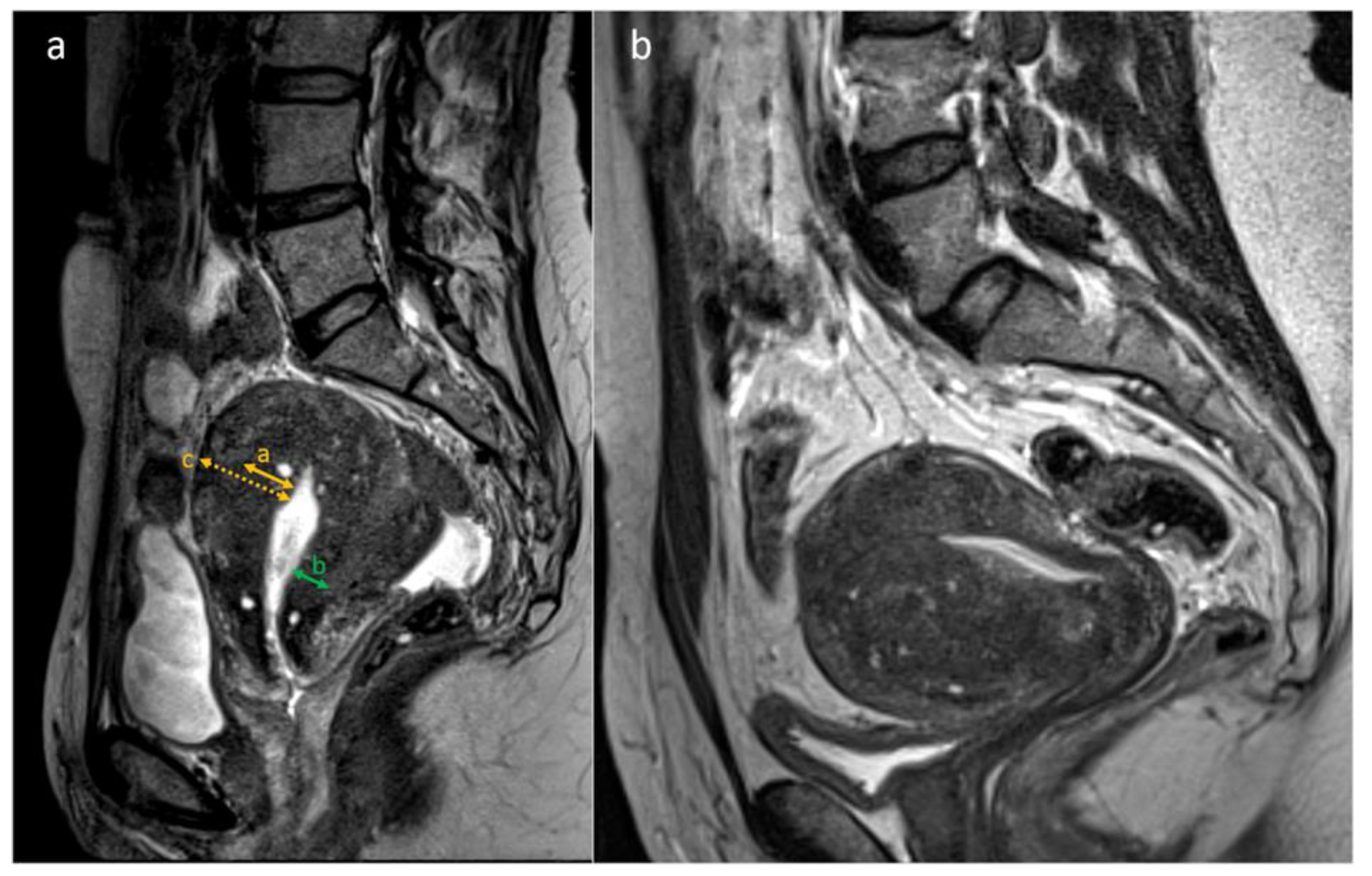

| JZ 1 max | Maximal JZ thickness (mm). Thickest part of the JZ in the midsagittal plane. |
| JZmin | Minimal JZ thickness (mm). Thinnest part of the JZ in the midsagittal plane. |
| Myometrial thickness | The thickness (mm) of the uterine wall at the same level as JZmax. |
| JZdiff | JZ differential (mm). Difference between the JZmax and JZmin. |
| JZmax/Myometrial thickness | The extent of the uterine wall that is affected by adenomyosis (%), JZmax divided by myometrial thickness measured at the same level |
| Appearance of JZ | (a) Not visible or not assessable. (b) Regular JZ: the inner and outer borders of the JZ are well defined. (c) Irregular JZ; the presence of focal thickening of the JZ and/or presence of cystic foci of high signal intensity. |
| Cysts | Cystic changes in the JZ (defined as foci of high signal intensity on T2-weighted images). Absent/Present. |
| Globular uterine shape | Subjective evaluation of the uterine corpus being globular shaped and not due to fibroids. Globular yes/no. |
| Wall asymmetry | Subjective evaluation of the anterior and posterior wall thickness. Yes/no. |
| Diagnosis | Assessment of the images. Does the subject have adenomyosis? Yes/No |
| Image Quality | Evaluation of the quality of the images. Low/Moderate/High |
| Diagnostic confidence | Examiner confidence in their assessment. Low/Medium/High |
| JZ 1 max | Maximal JZ thickness (mm), measured in the reconstructed coronal plan from the 3D 2 volume. |
| JZmin | Minimal JZ thickness (mm), measured in the reconstructed coronal plane from 3D 2 volume. |
| Globular uterine shape | Subjective evaluation of the uterine corpus being globular-shaped and not due to fibroids. Yes/No. |
| Wall asymmetry | Subjective evaluation of the anterior and posterior wall thickness. Are the walls asymmetric? Yes/No |
| Appearance of JZ | Assessment of the JZ irregularity. Regular/Irregular |
| Fan-shaped shadows | Is fan-shaped shadowing present in the myometrium? Yes/No. |
| Buds/Striations | Are endometrial buds/striations present in the myometrium? Yes/No |
| Hyperechogenic Islands | Are hyperechogenic islands present in the myometrium? Yes/No |
| Cysts | Presence of myometrial cysts? Yes/No |
| Diagnosis | Assessment of the images. Does the subject have adenomyosis? Yes/No. |
| Quality | Evaluation of the quality of the images. Low/Moderate /High |
| Confidence | Examiner confidence in the assessment. Low/Medium/High |
| Variable | MRI | TVS | ||
|---|---|---|---|---|
| Kappa | 95% CI | Kappa | 95% CI | |
| Globular uterus shape | 0.199 | 0.195–0.202 | 0.482 | 0.48–0.485 |
| Wall asymmetry | 0.552 | 0.548–0.556 | 0.414 | 0.411–0.417 |
| Irregular JZ 1 | 0.527 | 0.522–0.531 | 0.309 | 0.307–0.312 |
| Cysts in the JZ/Myometrium | 0.327 | 0.324–0.331 | 0.192 | 0.190–0.195 |
| Fan-shaped shadowing | - | - | 0.357 | 0.354–0.359 |
| Buds or Striations | - | - | 0.209 | 0.206–0.211 |
| Hyperechogenic Islands | - | - | 0.289 | 0.286–0.292 |
| Diagnosis | 0.283 | 0.280–0.287 | 0.420 | 0.417–0.422 |
| Variable | MRI | TVS | ||
|---|---|---|---|---|
| ICC | 95% CI | ICC | 95% CI | |
| JZ 1 max | 0.821 2 | 0.709–0.898 | 0.082 3 | −0.11–0.252 |
| JZmin | 0.572 2 | 0.408–0.724 | −0.31 4 | −0.67–−0.104 |
| JZmax/Myometrial thickness | 0.830 2 | 0.739–0.900 | - | - |
| RatioJZmax/Myometrium | 0.570 2 | 0.382–0.731 | - | - |
| JZmax-JZmin (JZdiff) | 0.713 2 | 0.583–0.823 | - | - |
| Rater 1 | Rater 2 | Rater 3 | Rater 4 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality | Confidence | Quality | Confidence | Quality | Confidence | Quality | Confidence | |||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Low | 27 | 52.9 | 15 | 29.4 | 5 | 9.8 | 3 | 5.9 | 6 | 11.8 | 1 | 2.0 | 16 | 31.4 | 10 | 19.6 |
| Medium | 18 | 35.3 | 19 | 37.3 | 18 | 35.3 | 17 | 33.3 | 21 | 41.2 | 10 | 19.6 | 30 | 58.8 | 27 | 52.9 |
| High | 6 | 11.8 | 17 | 33.3 | 28 | 54.9 | 31 | 60.8 | 24 | 47.1 | 40 | 78.4 | 5 | 9.8 | 14 | 27.5 |
| Rater 1 | Rater 2 | Rater 3 | Rater 4 | Rater 5 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality | Confidence | Quality | Confidence | Quality | Confidence | Quality | Confidence | Quality | Confidence | |||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| Low | 9 | 17.6 | 2 | 3.9 | 7 | 13.7 | 3 | 5.9 | 17 | 33.3 | 13 | 25.5 | 12 | 23.5 | 9 | 17.6 | 6 | 11.8 | 11 | 21.6 |
| Medium | 35 | 68.6 | 7 | 13.7 | 35 | 68.6 | 33 | 64.7 | 21 | 41.2 | 12 | 23.5 | 17 | 33.3 | 9 | 17.6 | 37 | 72.5 | 24 | 47.1 |
| High | 7 | 13.7 | 42 | 82.4 | 9 | 17.6 | 15 | 29.4 | 13 | 25.5 | 26 | 51.0 | 22 | 43.1 | 32 | 62.7 | 8 | 15.7 | 16 | 31.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andersson, J.K.; Mucelli, R.P.; Dueholm, M.; Fridsten, S.; Grigoriadis, A.; Guerriero, S.; Leone, F.P.; Valentin, L.; Van Den Bosch, T.; Voulgarakis, N.; et al. Inter-Rater Agreement for Diagnosing Adenomyosis Using Magnetic Resonance Imaging and Transvaginal Ultrasonography. Diagnostics 2023, 13, 2193. https://doi.org/10.3390/diagnostics13132193
Andersson JK, Mucelli RP, Dueholm M, Fridsten S, Grigoriadis A, Guerriero S, Leone FP, Valentin L, Van Den Bosch T, Voulgarakis N, et al. Inter-Rater Agreement for Diagnosing Adenomyosis Using Magnetic Resonance Imaging and Transvaginal Ultrasonography. Diagnostics. 2023; 13(13):2193. https://doi.org/10.3390/diagnostics13132193
Chicago/Turabian StyleAndersson, Johanna K., Raffaella Pozzi Mucelli, Margit Dueholm, Susanne Fridsten, Aristeidis Grigoriadis, Stefano Guerriero, Francesco Paolo Leone, Lil Valentin, Thierry Van Den Bosch, Nikolaos Voulgarakis, and et al. 2023. "Inter-Rater Agreement for Diagnosing Adenomyosis Using Magnetic Resonance Imaging and Transvaginal Ultrasonography" Diagnostics 13, no. 13: 2193. https://doi.org/10.3390/diagnostics13132193
APA StyleAndersson, J. K., Mucelli, R. P., Dueholm, M., Fridsten, S., Grigoriadis, A., Guerriero, S., Leone, F. P., Valentin, L., Van Den Bosch, T., Voulgarakis, N., Gemzell-Danielsson, K., & Epstein, E. (2023). Inter-Rater Agreement for Diagnosing Adenomyosis Using Magnetic Resonance Imaging and Transvaginal Ultrasonography. Diagnostics, 13(13), 2193. https://doi.org/10.3390/diagnostics13132193






