Maternal and Neonatal Outcomes of Elective Induction of Labor at 39 or More Weeks: A Prospective, Observational Study
Abstract
1. Introduction
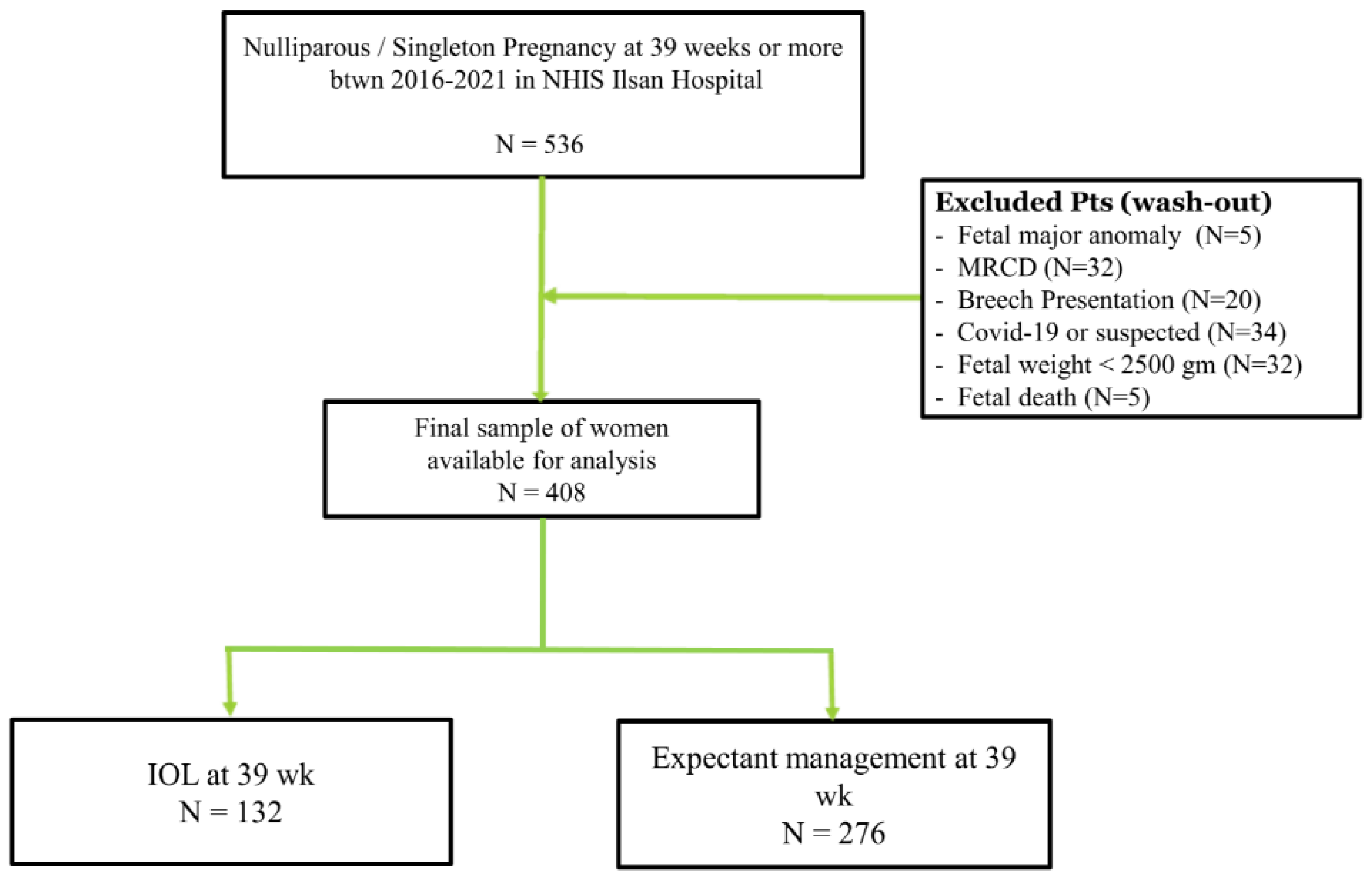
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wen, T.; Turitz, A.L. Optimizing Term Delivery and Mode of Delivery. Clin. Perinatol. 2020, 47, 799–815. [Google Scholar] [CrossRef]
- Papalia, N.; D’Souza, R.D.; Hobson, S.R. Optimal timing of labour induction in contemporary clinical practice. Best Pract. Res. Clin. Obstet. Gynaecol. 2022, 79, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Caughey, A.B.; Stotland, N.E.; Washington, A.E.; Escobar, G.J. Maternal and obstetric complications of pregnancy are associated with increasing gestational age at term. Am. J. Obstet. Gynecol. 2007, 196, 155.e1–155.e6. [Google Scholar] [CrossRef]
- Rydahl, E.; Eriksen, L.; Juhl, M. Effects of induction of labor prior to post-term in low-risk pregnancies: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 170–208. [Google Scholar] [CrossRef] [PubMed]
- Alkmark, M.; Keulen, J.K.J.; Kortekaas, J.C.; Bergh, C.; van Dillen, J.; Duijnhoven, R.G.; Hagberg, H.; Mol, B.W.; Molin, M.; van der Post, J.A.M.; et al. Induction of labour at 41 weeks or expectant management until 42 weeks: A systematic review and an individual participant data meta-analysis of randomised trials. PLoS Med. 2020, 17, e1003436. [Google Scholar] [CrossRef] [PubMed]
- Ehrenthal, D.B.; Jiang, X.; Strobino, D.M. Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstet. Gynecol. 2010, 116, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Kiesewetter, B.; Lehner, R. Maternal outcome monitoring: Induction of labor versus spontaneous onset of labor-a retrospective data analysis. Arch. Gynecol. Obstet. 2012, 286, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Visconti, F.; Quaresima, P.; Rania, E.; Palumbo, A.R.; Micieli, M.; Zullo, F.; Venturella, R.; Di Carlo, C. Difficult caesarean section: A literature review. Eur J. Obstet. Gynecol. Reprod. Biol. 2020, 246, 72–78. [Google Scholar] [CrossRef]
- ACOG. Practice Bulletin No. 107: Induction of Labor. Obstet. Gynecol. 2009, 114, 386–397. [Google Scholar] [CrossRef]
- Grobman, W.A. Labor Induction vs. Expectant Management of Low-Risk Pregnancy. N. Engl. J. Med. 2018, 379, 2278–2279. [Google Scholar] [CrossRef]
- ACOG. Clinical Guidance for Integration of the Findings of The ARRIVE Trial: Labor Induction Versus Expectant Management in Low-Risk Nulliparous Women. Available online: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2018/08/clinical-guidance-for-integration-of-the-findings-of-the-arrive-trial (accessed on 15 October 2022).
- SMFM Statement on Elective Induction of Labor in Low-Risk Nulliparous Women at Term: The ARRIVE Trial. Am. J. Obstet. Gynecol. 2019, 221, B2–B4. [CrossRef] [PubMed]
- Statistics Korea. Birth Statistics in 2021. Available online: http://kostat.go.kr/portal/eng/pressReleases/8/1/index.board?bmode=read&bSeq=&aSeq=420358&pageNo=1&rowNum=10&navCount=10&currPg=&searchInfo=&sTarget=title&sTxt= (accessed on 15 October 2022).
- Song, J.E.; Ahn, J.A.; Lee, S.K.; Roh, E.H. Factors related to low birth rate among married women in Korea. PLoS ONE 2018, 13, e0194597. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.H.; Lee, J.; Lee, S.A.; Jung, Y.W. Impact of Maternal Age on Singleton Pregnancy Outcomes in Primiparous Women in South Korea. J. Clin. Med. 2022, 11, 969. [Google Scholar] [CrossRef] [PubMed]
- OECD. Health at a Glance 2013. Available online: https://www.oecd-ilibrary.org/social-issues-migration-health/health-at-a-glance-2013_health_glance-2013-en (accessed on 31 October 2022).
- Reis, F.M.; Gervasi, M.T.; Florio, P.; Bracalente, G.; Fadalti, M.; Severi, F.M.; Petraglia, F. Prediction of successful induction of labor at term: Role of clinical history, digital examination, ultrasound assessment of the cervix, and fetal fibronectin assay. Am. J. Obstet. Gynecol. 2003, 189, 1361–1367. [Google Scholar] [CrossRef]
- Jung, Y.W.; Pak, H.; Lee, I.; Kim, E.H. The Effect of Diagnosis-Related Group Payment System on Quality of Care in the Field of Obstetrics and Gynecology among Korean Tertiary Hospitals. Yonsei Med. J. 2018, 59, 539–545. [Google Scholar] [CrossRef]
- Tsai, T.C.; Joynt, K.E.; Orav, E.J.; Gawande, A.A.; Jha, A.K. Variation in surgical-readmission rates and quality of hospital care. N. Engl. J. Med. 2013, 369, 1134–1142. [Google Scholar] [CrossRef]
- Saccone, G.; Della Corte, L.; Maruotti, G.M.; Quist-Nelson, J.; Raffone, A.; De Vivo, V.; Esposito, G.; Zullo, F.; Berghella, V. Induction of labor at full-term in pregnant women with uncomplicated singleton pregnancy: A systematic review and meta-analysis of randomized trials. Acta Obstet. Gynecol. Scand. 2019, 98, 958–966. [Google Scholar] [CrossRef]
- Freret, T.S.; Woods, G.T.; James, K.E.; Kaimal, A.J.; Clapp, M.A. Incidence of and Risk Factors for Failed Induction of Labor Using a Contemporary Definition. Obstet. Gynecol. 2021, 137, 497–504. [Google Scholar] [CrossRef]
- Grobman, W.A.; Caughey, A.B. Elective induction of labor at 39 weeks compared with expectant management: A meta-analysis of cohort studies. Am. J. Obstet. Gynecol. 2019, 221, 304–310. [Google Scholar] [CrossRef]
- Souter, V.; Painter, I.; Sitcov, K.; Caughey, A.B. Maternal and newborn outcomes with elective induction of labor at term. Am. J. Obstet. Gynecol. 2019, 220, 273.e1–273.e11. [Google Scholar] [CrossRef]
- Zhu, J.; Xue, L.; Shen, H.; Zhang, L.; Lu, D.; Wang, Y.; Zhang, Y.; Zhang, J. Labor induction in China: A nationwide survey. BMC Pregnancy Childbirth 2022, 22, 463. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Induction of Labor (n = 132) | Expectant Management (n = 276) | p-Value |
|---|---|---|---|
| Age (year) | 32.6 ± 4.7 | 31.7 ± 4.2 | 0.060 |
| Gestational age (weeks) | 39.0 | 39.6 ± 0.5 | <0.001 * |
| Weight gain in pregnancy | 12.1 ± 6.0 | 12.9 ± 5.5 | 0.194 |
| BMI | |||
| BMI in pre-pregnancy | 22.0 ± 3.9 | 21.1 ± 2.7 | 0.004 * |
| BMI in term | 27.1 ± 4.2 | 26.2 ± 3.3 | 0.021 * |
| Bishop Score ** at admission | 3.8 ± 1.6 | 4.1 ± 1.8 | 0.170 |
| Cervix length (mm) at admission | 20.1 ± 0.88 | 18.6 ± 8.6 | 0.132 |
| Variables | Induction of Labor (n = 132) | Expectant Management (n = 276) | p-Value |
|---|---|---|---|
| Cesarean section | 24 (18.2) | 44 (15.9) | 0.570 |
| Operative vaginal delivery | 21 (18.9) | 41 (17.2) | 0.700 |
| Length of hospital stay (day) | 4.1 ± 1.3 | 4.0 ± 1.3 | 0.244 |
| Time from admission to delivery (min) | 835 ± 527 | 717 ± 469 | 0.040 * |
| Time for second stage labor (min) | 69 ± 54 | 76 ± 51 | 0.276 |
| Delivery within 12 h | 58 (53.7) | 142 (61.2) | 0.191 |
| Decrease in Hgb after delivery (g/dL) | 1.7 ± 2.1 | 1.8 ± 1.7 | 0.526 |
| Transfusion | 3 (2.3) | 13 (4.7) | 0.235 |
| Embolization | 2 (1.5) | 1 (0.4) | 0.202 |
| Readmission ** | 4 (3.0) | 17 (6.2) | 0.181 |
| Outpatient visits *** > 2 | 73 (55.3) | 154 (55.8) | 0.925 |
| Variables | Induction of Labor (n = 132) | Expectant Management (n = 276) | p-Value |
|---|---|---|---|
| Fetal body weight (gm) | 3233 ± 376 | 3304 ± 341 | 0.057 |
| FBW > 3500 gm | 34 (25.8) | 75 (27.2) | 0.762 |
| Apgar score | |||
| AS at 5 min | 8.2 ± 1.1 | 8.1 ± 1.4 | 0.421 |
| AS at 5 min < 7 | 1 (0.8) | 15 (5.4) | 0.023 * |
| NICU admission | 65 (49.2) | 101 (36.6) | 0.015 * |
| Intubation | 3 (2.3) | 9 (3.3) | 0.581 |
| Meconium-stained amniotic fluid | 18 (13.6) | 51 (18.5) | 0.222 |
| Odds Ratio (95% CI) | ||||
|---|---|---|---|---|
| Unadjusted OR | p-Value | Adjusted OR | p-Value | |
| Induction of labor at 39 weeks | 0.83 (0.48–1.44) | 0.507 | 0.64 (0.28–1.45) | 0.280 |
| Induction of Labor | Expectant Management | |
|---|---|---|
| Maternal outcome | ||
| Cesarean section | Similar | Similar |
| Time from admission to delivery | Shorter | Longer |
| Time for second stage labor | Similar | Similar |
| Postpartum hemorrhage | Similar | Similar |
| Readmission * | Similar | Similar |
| Neonatal outcome | ||
| AS at 5 min <7 | Lower | Higher |
| NICU admission | Higher | Lower |
| Intubation | Similar | Similar |
| Meconium-stained amniotic fluid | Similar | Similar |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.; Cha, D.H.; Park, C.W.; Kim, E.H. Maternal and Neonatal Outcomes of Elective Induction of Labor at 39 or More Weeks: A Prospective, Observational Study. Diagnostics 2023, 13, 38. https://doi.org/10.3390/diagnostics13010038
Lee S, Cha DH, Park CW, Kim EH. Maternal and Neonatal Outcomes of Elective Induction of Labor at 39 or More Weeks: A Prospective, Observational Study. Diagnostics. 2023; 13(1):38. https://doi.org/10.3390/diagnostics13010038
Chicago/Turabian StyleLee, Soobin, Dong Hyun Cha, Cho Won Park, and Eui Hyeok Kim. 2023. "Maternal and Neonatal Outcomes of Elective Induction of Labor at 39 or More Weeks: A Prospective, Observational Study" Diagnostics 13, no. 1: 38. https://doi.org/10.3390/diagnostics13010038
APA StyleLee, S., Cha, D. H., Park, C. W., & Kim, E. H. (2023). Maternal and Neonatal Outcomes of Elective Induction of Labor at 39 or More Weeks: A Prospective, Observational Study. Diagnostics, 13(1), 38. https://doi.org/10.3390/diagnostics13010038






