Challenges for Artificial Intelligence in Recognizing Mental Disorders
Abstract
1. Introduction
2. The Rationale for Using Machine Learning to Identify Mental Disorders
3. Challenges from Diagnostic Criteria
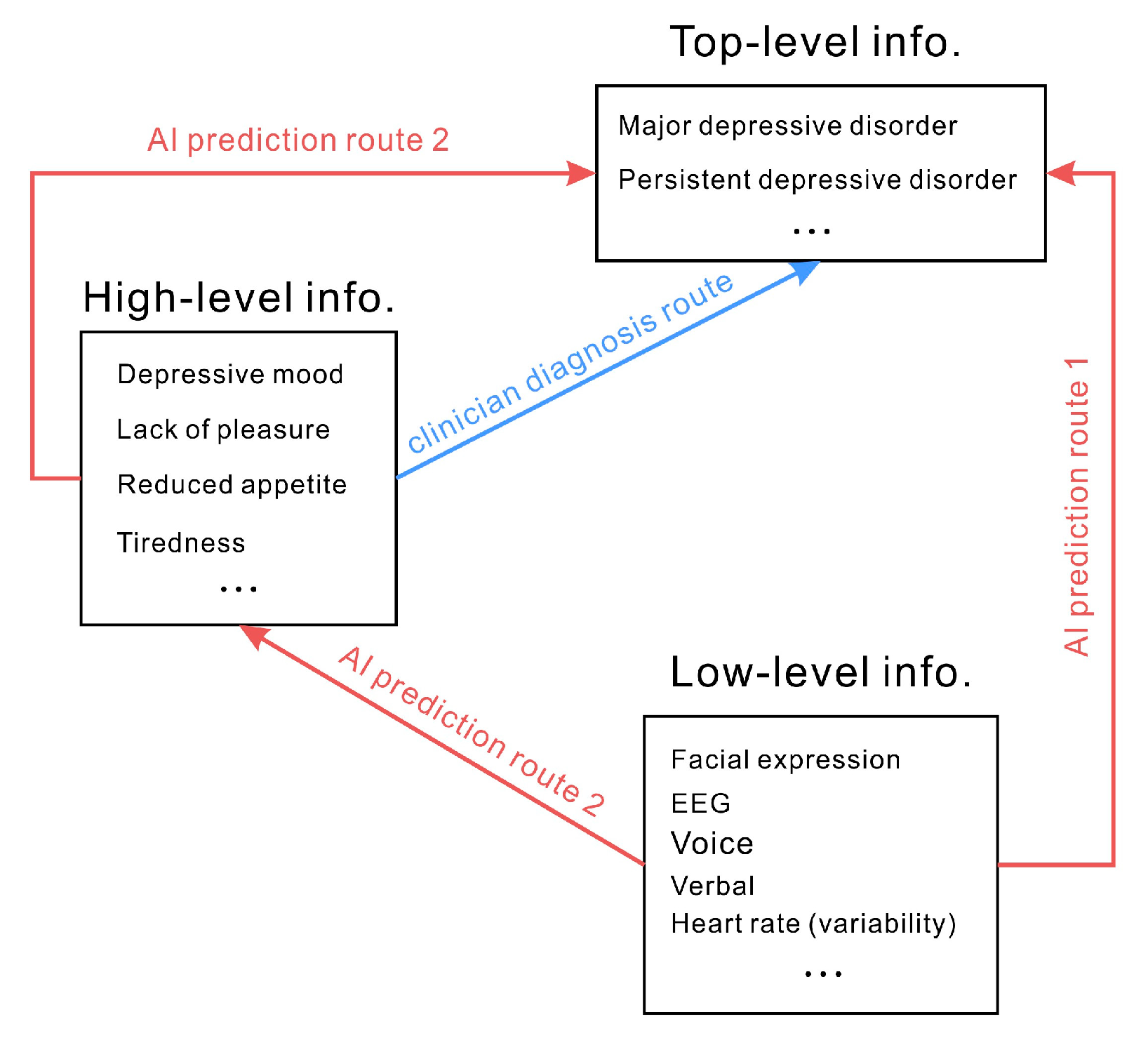
4. Challenges from Standard Diagnostic Approaches
5. Challenges from the Logical Fallacy of Mental Disorder Diagnosis
6. Challenges from Datasets
6.1. Example Datasets for Depression Recognition
6.2. Are the Recorded Data Sufficiently Valid and Ecological?
6.3. Small Sample Size
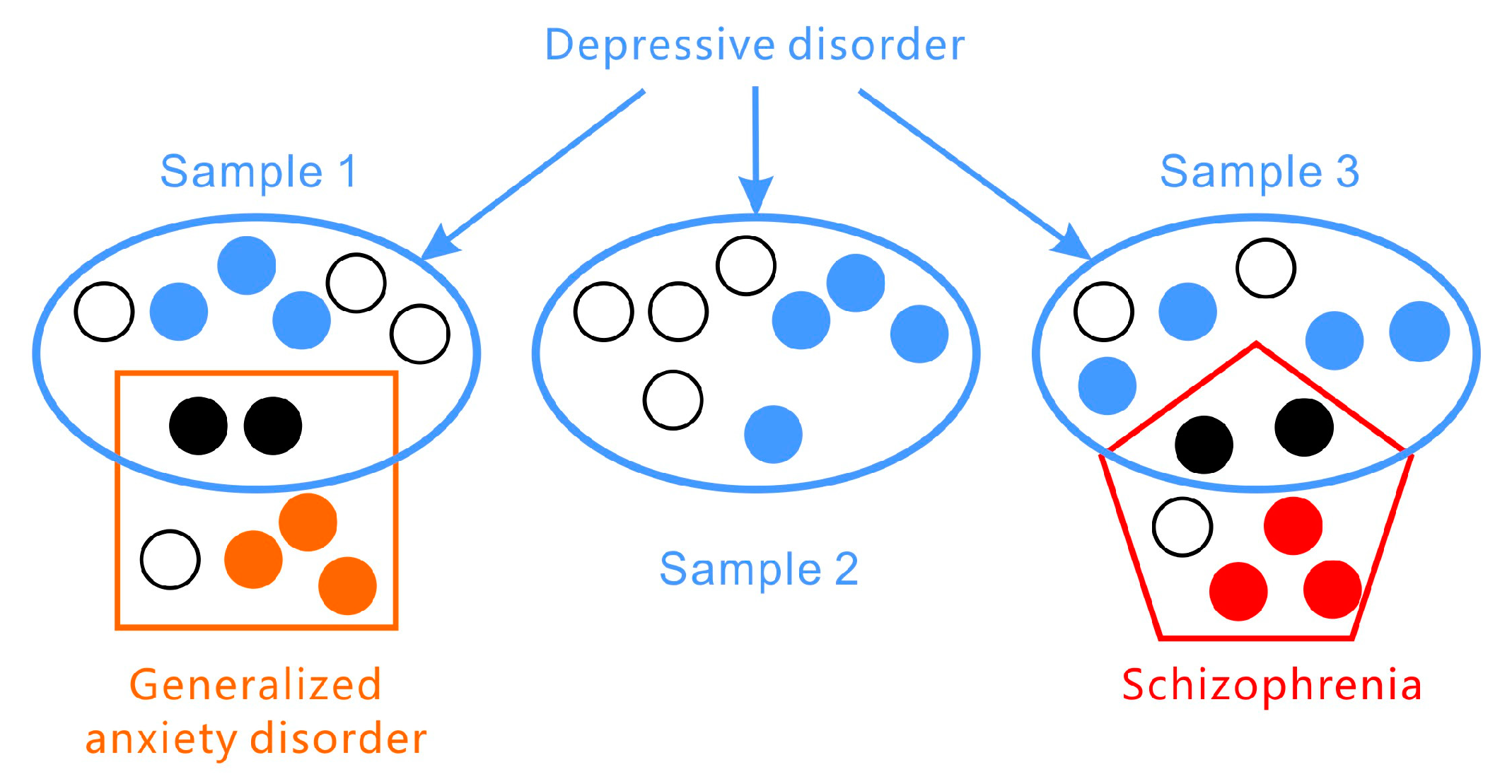
6.4. Simplified Limited Categories
7. Challenges from Annotations
7.1. Is the Annotation Valid?
7.2. Can Subjective Feelings Be Mapped from Objective Measures?
8. Can Multimodality Be a Solution to the Complexity?
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Zhou, M.; Scott, J.; Chaudhury, B.; Hall, L.; Goldgof, D.; Yeom, K.W.; Iv, M.; Ou, Y.; Kalpathy-Cramer, J.; Napel, S. Radiomics in brain tumor: Image assessment, quantitative feature descriptors, and machine-learning approaches. Am. J. Neuroradiol. 2018, 39, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, F.; Fidalgo, F.; Silva, A.; Metrôlho, J.; Santos, O.; Dionisio, R. Literature Review of Machine-Learning Algorithms for Pressure Ulcer Prevention: Challenges and Opportunities. Informatics 2021, 8, 76. [Google Scholar] [CrossRef]
- Bolton, D. What Is Mental Disorder? An Essay in Philosophy, Science, and Values; Oxford University Press: Oxford, UK, 2008. [Google Scholar]
- Gao, S.; Calhoun, V.D.; Sui, J. Machine learning in major depression: From classification to treatment outcome prediction. CNS Neurosci. Ther. 2018, 24, 1037–1052. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, X.; Zhu, J.; Mao, W.; Sun, S.; Wang, Z.; Xia, C.; Hu, B. Depression recognition using machine learning methods with different feature generation strategies. Artif. Intell. Med. 2019, 99, 101696. [Google Scholar] [CrossRef]
- Ayano, G.; Demelash, S.; Haile, K.; Tulu, M.; Assefa, D.; Tesfaye, A.; Haile, K.; Solomon, M.; Chaka, A.; Tsegay, L. Misdiagnosis, detection rate, and associated factors of severe psychiatric disorders in specialized psychiatry centers in Ethiopia. Ann. Gen. Psychiatry 2021, 20, 1–10. [Google Scholar] [CrossRef]
- Vermani, M.; Marcus, M.; Katzman, M.A. Rates of detection of mood and anxiety disorders in primary care: A descriptive, cross-sectional study. Prim. Care Companion CNS Disord. 2011, 13, 27211. [Google Scholar] [CrossRef]
- Wang, L.; Hermens, D.F.; Hickie, I.B.; Lagopoulos, J. A systematic review of resting-state functional-MRI studies in major depression. J. Affect. Disord. 2012, 142, 6–12. [Google Scholar] [CrossRef]
- Pan, J.-X.; Xia, J.-J.; Deng, F.-L.; Liang, W.-W.; Wu, J.; Yin, B.-M.; Dong, M.-X.; Chen, J.-J.; Ye, F.; Wang, H.-Y. Diagnosis of major depressive disorder based on changes in multiple plasma neurotransmitters: A targeted metabolomics study. Transl. Psychiatry 2018, 8, 1–10. [Google Scholar] [CrossRef]
- Lee, H.S.; Baik, S.Y.; Kim, Y.-W.; Kim, J.-Y.; Lee, S.-H. Prediction of antidepressant treatment outcome using event-related potential in patients with major depressive disorder. Diagnostics 2020, 10, 276. [Google Scholar] [CrossRef]
- Ellis, A.J.; Vanderlind, W.M.; Beevers, C.G. Enhanced anger reactivity and reduced distress tolerance in major depressive disorder. Cogn. Ther. Res. 2013, 37, 498–509. [Google Scholar] [CrossRef]
- Fiquer, J.T.; Moreno, R.A.; Brunoni, A.R.; Barros, V.B.; Fernandes, F.; Gorenstein, C. What is the nonverbal communication of depression? Assessing expressive differences between depressive patients and healthy volunteers during clinical interviews. J. Affect. Disord. 2018, 238, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Pampouchidou, A.; Simos, P.G.; Marias, K.; Meriaudeau, F.; Yang, F.; Pediaditis, M.; Tsiknakis, M. Automatic assessment of depression based on visual cues: A systematic review. IEEE Trans. Affect. Comput. 2017, 10, 445–470. [Google Scholar] [CrossRef]
- Lee, Y.-S.; Park, W.-H. Diagnosis of Depressive Disorder Model on Facial Expression Based on Fast R-CNN. Diagnostics 2022, 12, 317. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Wang, R.; Lin, H.; Zhang, F.; Tu, J.; Sun, M. Automatic depression recognition by intelligent speech signal processing: A systematic survey. CAAI Trans. Intell. Technol. 2022. [Google Scholar] [CrossRef]
- Jones, N.P.; Siegle, G.J.; Mandell, D. Motivational and emotional influences on cognitive control in depression: A pupillometry study. Cogn. Affect. Behav. Neurosci. 2015, 15, 263–275. [Google Scholar] [CrossRef]
- Gavrilescu, M.; Vizireanu, N. Predicting depression, anxiety, and stress levels from videos using the facial action coding system. Sensors 2019, 19, 3693. [Google Scholar] [CrossRef]
- Scherer, S.; Stratou, G.; Morency, L.-P. Audiovisual behavior descriptors for depression assessment. In Proceedings of the 15th ACM on International Conference on Multimodal Interaction, Sydney, Australia, 9–13 December 2013; pp. 135–140. [Google Scholar]
- Morency, L.-P.; Stratou, G.; DeVault, D.; Hartholt, A.; Lhommet, M.; Lucas, G.; Morbini, F.; Georgila, K.; Scherer, S.; Gratch, J. SimSensei demonstration: A perceptive virtual human interviewer for healthcare applications. In Proceedings of the AAAI Conference on Artificial Intelligence, Austin, TX, USA, 25–30 January 2015. [Google Scholar]
- Gupta, R.; Malandrakis, N.; Xiao, B.; Guha, T.; Van Segbroeck, M.; Black, M.; Potamianos, A.; Narayanan, S. Multimodal prediction of affective dimensions and depression in human-computer interactions. In Proceedings of the 4th International Workshop on Audio/Visual Emotion Challenge, Orlando, FL, USA, 7 November 2014; pp. 33–40. [Google Scholar]
- Ringeval, F.; Schuller, B.; Valstar, M.; Cummins, N.; Cowie, R.; Tavabi, L.; Pantic, M. AVEC 2019 workshop and challenge: State-of-mind, detecting depression with AI, and cross-cultural affect recognition. In Proceedings of the 9th International on Audio/Visual Emotion Challenge and Workshop, Nice, France, 21 October 2019; pp. 3–12. [Google Scholar]
- Siegle, G.J.; Steinhauer, S.R.; Friedman, E.S.; Thompson, W.S.; Thase, M.E. Remission prognosis for cognitive therapy for recurrent depression using the pupil: Utility and neural correlates. Biol. Psychiatry 2011, 69, 726–733. [Google Scholar] [CrossRef]
- Silk, J.S.; Dahl, R.E.; Ryan, N.D.; Forbes, E.E.; Axelson, D.A.; Birmaher, B.; Siegle, G.J. Pupillary reactivity to emotional information in child and adolescent depression: Links to clinical and ecological measures. Am. J. Psychiatry 2007, 164, 1873–1880. [Google Scholar] [CrossRef]
- Price, R.B.; Rosen, D.; Siegle, G.J.; Ladouceur, C.D.; Tang, K.; Allen, K.B.; Ryan, N.D.; Dahl, R.E.; Forbes, E.E.; Silk, J.S. From anxious youth to depressed adolescents: Prospective prediction of 2-year depression symptoms via attentional bias measures. J. Abnorm. Psychol. 2016, 125, 267. [Google Scholar] [CrossRef]
- Alghowinem, S.; Goecke, R.; Wagner, M.; Parker, G.; Breakspear, M. Eye movement analysis for depression detection. In Proceedings of the 2013 IEEE International Conference on Image Processing, Melbourne, Australia, 15–18 September 2013; pp. 4220–4224. [Google Scholar]
- Association, A.P. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub; 2013. J. Physiother. Res. Salvador 2019, 9, 155–158. [Google Scholar]
- World Health Organization. ICD-11 for Mortality and Morbidity Statistics. Version: 2019 April. Geneva. Available online: https://icd.who.int/browse11/l-m/en (accessed on 24 October 2022).
- Lochbaum, M.; Zanatta, T.; Kirschling, D.; May, E. The Profile of Moods States and athletic performance: A meta-analysis of published studies. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 50–70. [Google Scholar] [CrossRef] [PubMed]
- Østergaard, S.D.; Jensen, S.; Bech, P. The heterogeneity of the depressive syndrome: When numbers get serious. Acta Psychiatr. Scand. 2011, 124, 495–496. [Google Scholar] [CrossRef] [PubMed]
- Stein, D.J.; Phillips, K.A.; Bolton, D.; Fulford, K.; Sadler, J.Z.; Kendler, K.S. What is a mental/psychiatric disorder? From DSM-IV to DSM-V. Psychol. Med. 2010, 40, 1759–1765. [Google Scholar] [CrossRef]
- Oquendo, M.A.; Baca-García, E.; Mann, J.J.; Giner, J. Issues for DSM-V: Suicidal Behavior as a Separate Diagnosis on a Separate Axis; American Psychiatric Association: Washington, DC, USA, 2008; Volume 165, pp. 1383–1384. [Google Scholar]
- Lux, V.; Kendler, K. Deconstructing major depression: A validation study of the DSM-IV symptomatic criteria. Psychol. Med. 2010, 40, 1679–1690. [Google Scholar] [CrossRef]
- Kamphuis, J.H.; Noordhof, A. On categorical diagnoses in DSM-V: Cutting dimensions at useful points? Psychol. Assess. 2009, 21, 294. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.A.; Di Nardo, P.A.; Lehman, C.L.; Campbell, L.A. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. J. Abnorm. Psychol. 2001, 110, 49. [Google Scholar] [CrossRef]
- Nestler, E.J.; Barrot, M.; DiLeone, R.J.; Eisch, A.J.; Gold, S.J.; Monteggia, L.M. Neurobiology of depression. Neuron 2002, 34, 13–25. [Google Scholar] [CrossRef]
- Kessler, R.C.; Bromet, E.J. The epidemiology of depression across cultures. Annu. Rev. Public Health 2013, 34, 119. [Google Scholar] [CrossRef]
- Maj, M.; Stein, D.J.; Parker, G.; Zimmerman, M.; Fava, G.A.; De Hert, M.; Demyttenaere, K.; McIntyre, R.S.; Widiger, T.; Wittchen, H.U. The clinical characterization of the adult patient with depression aimed at personalization of management. World Psychiatry 2020, 19, 269–293. [Google Scholar] [CrossRef]
- Williams, L.S.; Brizendine, E.J.; Plue, L.; Bakas, T.; Tu, W.; Hendrie, H.; Kroenke, K. Performance of the PHQ-9 as a screening tool for depression after stroke. Stroke 2005, 36, 635–638. [Google Scholar] [CrossRef]
- Hamilton, M. The Hamilton Rating Scale for Depression. In Assessment of Depression; Springer: Berlin/Heidelberg, Germany, 1986; pp. 143–152. [Google Scholar]
- Mundt, J.C.; Snyder, P.J.; Cannizzaro, M.S.; Chappie, K.; Geralts, D.S. Voice acoustic measures of depression severity and treatment response collected via interactive voice response (IVR) technology. J. Neurolinguist. 2007, 20, 50–64. [Google Scholar] [CrossRef] [PubMed]
- Sharp, T.; Cowen, P.J. 5-HT and depression: Is the glass half-full? Curr. Opin. Pharmacol. 2011, 11, 45–51. [Google Scholar] [CrossRef]
- Luscher, B.; Shen, Q.; Sahir, N. The GABAergic deficit hypothesis of major depressive disorder. Mol. Psychiatry 2011, 16, 383–406. [Google Scholar] [CrossRef]
- Peterson, B.S.; Kaur, T.; Baez, M.A.; Whiteman, R.C.; Sawardekar, S.; Sanchez-Peña, J.; Hao, X.; Klahr, K.W.; Talati, A.; Wickramaratne, P. Morphological Biomarkers in the Amygdala and Hippocampus of Children and Adults at High Familial Risk for Depression. Diagnostics 2022, 12, 1218. [Google Scholar] [CrossRef] [PubMed]
- Valstar, M.; Schuller, B.; Smith, K.; Eyben, F.; Jiang, B.; Bilakhia, S.; Schnieder, S.; Cowie, R.; Pantic, M. Avec 2013: The continuous audio/visual emotion and depression recognition challenge. In Proceedings of the 3rd ACM International Workshop on Audio/Visual Emotion Challenge, Barcelona, Spain, 21 October 2013; pp. 3–10. [Google Scholar]
- Beck, A.T.; Steer, R.A.; Brown, G. Beck depression inventory–II. Psychol. Assess. 1996. [Google Scholar] [CrossRef]
- Valstar, M.; Schuller, B.; Smith, K.; Almaev, T.; Eyben, F.; Krajewski, J.; Cowie, R.; Pantic, M. Avec 2014: 3d dimensional affect and depression recognition challenge. In Proceedings of the 4th International Workshop on Audio/Visual Emotion Challenge, Orlando, FL, USA, 7 November 2014; pp. 3–10. [Google Scholar]
- Gratch, J.; Artstein, R.; Lucas, G.; Stratou, G.; Scherer, S.; Nazarian, A.; Wood, R.; Boberg, J.; DeVault, D.; Marsella, S. The Distress Analysis Interview Corpus of human and computer interviews. In Proceedings of the Ninth International Conference on Language Resources and Evaluation (LREC’14), Reykjavik, Iceland, 26–31 May 2014; pp. 3123–3128. [Google Scholar]
- Kroenke, K.; Strine, T.W.; Spitzer, R.L.; Williams, J.B.; Berry, J.T.; Mokdad, A.H. The PHQ-8 as a measure of current depression in the general population. J. Affect. Disord. 2009, 114, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Barrett, L.F.; Adolphs, R.; Marsella, S.; Martinez, A.M.; Pollak, S.D. Emotional expressions reconsidered: Challenges to inferring emotion from human facial movements. Psychol. Sci. Public Interest 2019, 20, 1–68. [Google Scholar] [CrossRef]
| Logical Format | Diagnosis | Logical Value |
|---|---|---|
| DD *→DS ** Modus Pollens | If depressive disorder then depressive symptom | Valid |
| Non-DD→non-DS Denying the antecedents | If no depressive disorder then no depressive symptom | Invalid |
| DS→DD Affirming the Consequent | If depressive symptom then depressive disorder | Invalid |
| Non-DS→non-DD Modus Tollens | If no depressive symptom then no depressive disorder | Valid |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yan, W.-J.; Ruan, Q.-N.; Jiang, K. Challenges for Artificial Intelligence in Recognizing Mental Disorders. Diagnostics 2023, 13, 2. https://doi.org/10.3390/diagnostics13010002
Yan W-J, Ruan Q-N, Jiang K. Challenges for Artificial Intelligence in Recognizing Mental Disorders. Diagnostics. 2023; 13(1):2. https://doi.org/10.3390/diagnostics13010002
Chicago/Turabian StyleYan, Wen-Jing, Qian-Nan Ruan, and Ke Jiang. 2023. "Challenges for Artificial Intelligence in Recognizing Mental Disorders" Diagnostics 13, no. 1: 2. https://doi.org/10.3390/diagnostics13010002
APA StyleYan, W.-J., Ruan, Q.-N., & Jiang, K. (2023). Challenges for Artificial Intelligence in Recognizing Mental Disorders. Diagnostics, 13(1), 2. https://doi.org/10.3390/diagnostics13010002






