Chronic Kidney Disease in Balkan Countries—A Call to Action for Timely Diagnosis and Monitoring
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Epidemiology
3.1.1. Current Status
3.1.2. Call to Action
- Design and implement an epidemiology study across the Balkan region to collect standardized data on the incidence and prevalence of early stages and causes of CKD. A unique research protocol and uniform data collection and reporting would allow building real-world evidence across the Balkan region, further exploring the variability across countries and informing management strategies based on reliable data.
- Expand existing reporting protocols and registries to include all CKD patients, irrespective of stage of the disease.
- Discuss possibilities to extract retrospective data (serum creatinine and albuminuria) from electronic files and use them as benchmark for epidemiology studies.
3.2. Risk Factors and Disease Awareness
3.2.1. Current Status
3.2.2. Call to Action
- Advocate for development and implementation of professional awareness campaigns for patients and medical professional communities.
- Increase media presence of national key opinion leaders to enhance education regarding primary and secondary prevention of CKD.
- Address specifically high-risk populations and collaborate with patient organizations and medical societies to improve recognition of chronic conditions that are risk factors for CKD.
- Promote a unitary and coherent communication strategy to European and national professional societies to streamline education of their members during regular scientific meetings and webinars.
3.3. Diagnosis and Treatment
3.3.1. Current Status
3.3.2. Call to Action
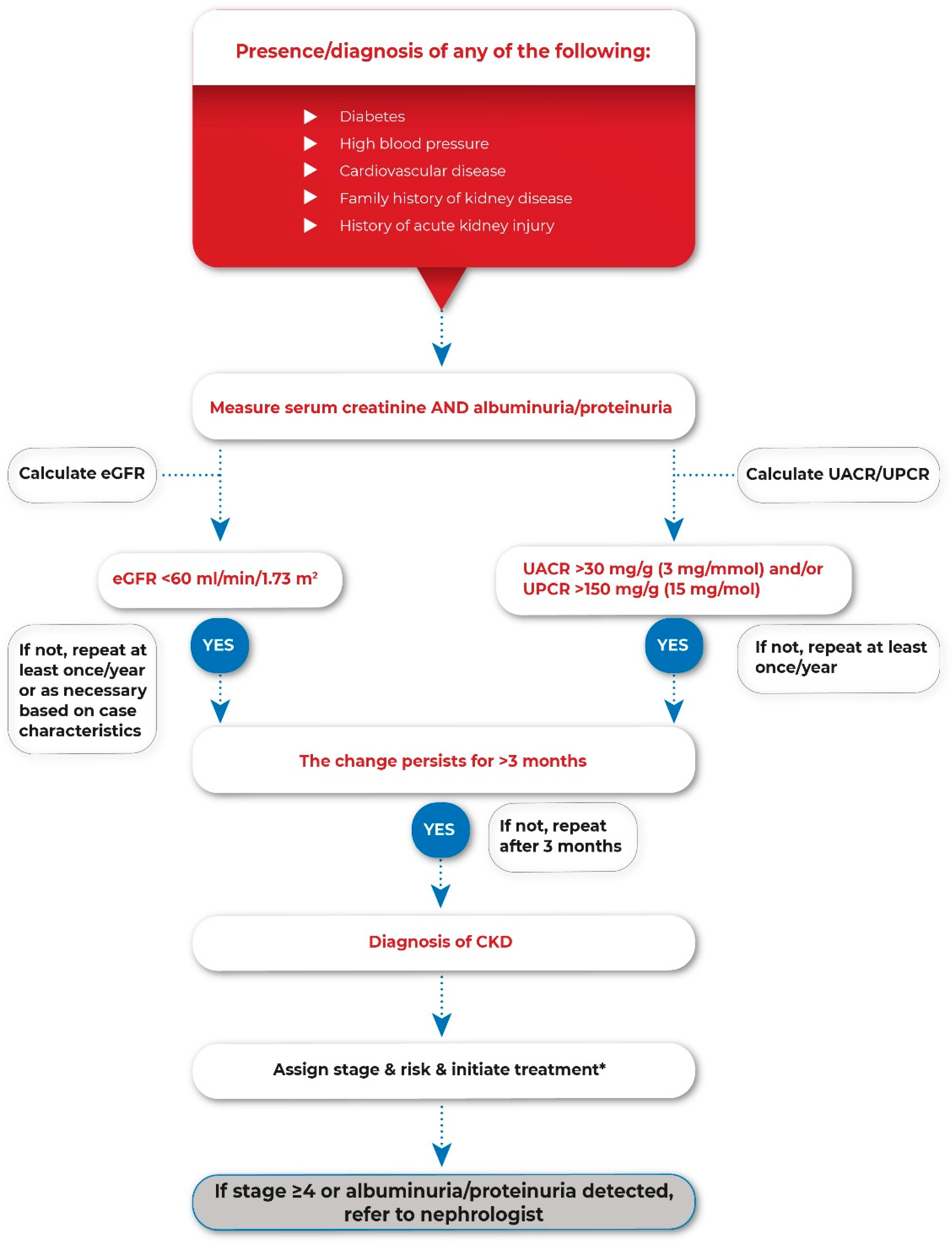
- Develop and implement screening programs in high-risk populations to allow diagnosis in early stages and adequate management to slow the decline of renal function (Figure 1).
- Develop simple algorithms for risk assessment, diagnosis, and referral to nephrologists.
- Include CKD risk assessment and diagnostic criteria in all relevant communications, and scientific meetings and webinars.
- Promote reporting on laboratory results of eGFR and UACR/UPCR in all patients with serum creatinine and albuminuria or proteinuria assessment.
- Create multidisciplinary working groups (nephrologist, endocrinologist, cardiologist, PCP) to coordinate implementation of CKD-related activities and lead high-level discussions to include CKD on the agenda of decision makers.
- ○
- Create the framework for structured collaboration of multidisciplinary team in national and regional kidney networks
- ○
- Empower PCPs to initiate and monitor treatment in CKD
- ○
- Increase number of nephrologists to treat CKD in all stages
- ○
- Provide reimbursement of treatments with strong and reliable results on mortality and renal function
- ○
- Share best practices of diagnosis and treatment between countries and institutions
- ○
- Collaborate with specialists in pharmaco-economics to assess the cost-effectiveness of early diagnosis and timely treatment in CKD
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Global Health Kidney Atlas, 2nd Edition. 2019. Available online: https://www.theisn.org/initiatives/global-kidney-health-atlas/ (accessed on 25 March 2022).
- European Kidney Health Alliance Call to Action. Available online: https://ekha.eu/blog/ekha-launches-a-call-to-action-to-improve-ckd-prevention-treatment-and-care-in-the-aftermath-of-covid-19/ (accessed on 25 March 2022).
- GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- Vanholder, R.; Annemans, L.; Bello, A.K.; Bikbov, B.; Gallego, D.; Gansevoort, R.T.; Lameire, N.; Luyckx, V.A.; Noruisiene, E.; Oostrom, T.; et al. Fighting the unbearable lightness of neglecting kidney health: The decade of the kidney. Clin. Kidney J. 2021, 14, 1719–1730. [Google Scholar] [CrossRef] [PubMed]
- Bennett, L. Changing European CKD trends: A call to action. J. Ren. Care 2007, 33, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Chronic Kidney Disease Prognosis Consortium; Matsushita, K.; van der Velde, M.; Astor, B.C.; Woodward, M.; Levey, A.S.; de Jong, P.E.; Coresh, J.; Gansevoort, R.T. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: A collaborative meta-analysis. Lancet 2010, 375, 2073–2081. [Google Scholar] [CrossRef]
- Vanholder, R.; Massy, Z.; Argiles, A.; Spasovski, G.; Verbeke, F.; Lameire, N. European Uremic Toxin Work Group. Chronic kidney disease as cause of cardiovascular morbidity and mortality. Nephrol. Dial. Transpl. 2005, 20, 1048–1056. [Google Scholar] [CrossRef]
- Stolpe, S.; Kowall, B.; Scholz, C.; Stang, A.; Blume, C. High unawareness of Chronic Kidney Disease in Germany. Int. J. Environ. Res. Public Health 2021, 18, 1752. [Google Scholar] [CrossRef]
- Chudek, J.; Wieczorowska-Tobis, K.; Zejda, J.; Broczek, K.; Skalska, A.; Zdrojewski, T.; Wiecek, A. The prevalence of chronic kidney disease and its relation to socioeconomic conditions in an elderly Polish population: Results from the national population-based study PolSenior. Nephrol. Dial. Transpl. 2014, 29, 1073–1082. [Google Scholar] [CrossRef]
- Chronic Kidney Disease in the United States, 2021. Centers for Disease Control and Prevention, US Department of Health and Human Services. 2021. Available online: https://www.cdc.gov/kidneydisease/publications-resources/ckd-national-facts.html (accessed on 5 April 2022).
- Komenda, P.; Rigatto, C.; Tangri, N. Screening strategies for unrecognized CKD. Clin. J. Am. Soc. Nephrol. 2016, 11, 925–927. [Google Scholar] [CrossRef]
- Vanholder, R.; Annemans, L.; Brown, E.; Gansevoort, R.; Gout-Zwart, J.J.; Lameire, N.; Morton, R.L.; Oberbauer, R.; Postma, M.J.; Tonelli, M.; et al. European Kidney Health Alliance. Reducing the costs of chronic kidney disease while delivering quality health care: A call to action. Nat. Rev. Nephrol. 2017, 13, 393–409. [Google Scholar] [CrossRef]
- Sever, M.Ş.; Jager, K.J.; Vanholder, R.; Stengel, B.; Harambat, J.; Finne, P.; Tesař, V.; Barbullushi, M.; Bumblytė, I.A.; Zakharova, E.; et al. A roadmap for optimizing chronic kidney disease patient care and patient-oriented research in the Eastern European nephrology community. Clin. Kidney J. 2020, 14, 23–35. [Google Scholar] [CrossRef]
- Zaletel, M.; Vardič, D.; Hladnik, M. (Eds.) Zdravstveni Statistični Letopis 2013; Nacionalni Inštitut za Javno Zdravje: Ljubljana, Slovenia, 2016; Available online: https://www.nijz.si/sl/publikacije/zdravstveni-statisticni-letopis-2013 (accessed on 5 April 2022).
- Zaletel, M.; Vardič, D.; Hladnik, M. (Eds.) Zdravstveni Statistični Letopis Slovenije 2019; Nacionalni Inštitut za Javno Zdravje: Ljubljana, Slovenia, 2021; Available online: https://www.nijz.si/sl/publikacije/zdravstveni-statisticni-letopis-2019 (accessed on 5 April 2022).
- Carriazo, S.; Ortiz, A. European East-West divide in kidney disease: The need to understand the drivers of chronic kidney disease outcomes. Clin. Kidney J. 2020, 14, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Impact Report of WKD 2021. Available online: https://www.worldkidneyday.org/impact-report-2021/ (accessed on 11 April 2022).
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Forxiga (Dapagliflozin) Summary of Product Characteristics. 2022. Available online: https://www.ema.europa.eu/en/documents/product-information/forxiga-epar-product-information_en.pdf (accessed on 11 April 2022).
- Rysz, J.; Gluba-Brzózka, A.; Franczyk, B.; Jabłonowski, Z.; Ciałkowska-Rysz, A. Novel Biomarkers in the Diagnosis of Chronic Kidney Disease and the Prediction of Its Outcome. Int. J. Mol. Sci. 2017, 18, 1702. [Google Scholar] [CrossRef] [PubMed]
- Mizdrak, M.; Kumrić, M.; Tičinović Kurir, T.; Božić, J. Emerging Biomarkers for Early Detection of Chronic Kidney Disease. J. Pers. Med. 2022, 12, 548. [Google Scholar] [CrossRef]
- Aziz Eftekhari, A.; Dizaj, S.M.; Ahmadian, E.; Przekora, A.; Khatibi, S.M.H.; Ardalan, M.; Vahed, S.Z.; Valiyeva, M.; Mehraliyeva, S.; Khalilov, R.; et al. Application of Advanced Nanomaterials for Kidney Failure Treatment and Regeneration. Materials 2021, 14, 2939. [Google Scholar] [CrossRef]
- Dizaj, S.M.; Eftekhari, A.; Mammadova, S.; Ahmadian, E.; Ardalan, M.; Davaran, S.; Nasibova, A.; Khalilov, R.; Valiyeva, M.; Mehraliyeva, S.; et al. Nanomaterials for Chronic Kidney Disease Detection. Appl. Sci. 2021, 11, 9656. [Google Scholar] [CrossRef]
- Jelaković, B.; Dika, Ž.; Arlt, V.M.; Stiborova, M.; Pavlović, N.M.; Nikolić, J.; Colet, J.M.; Vanherweghem, J.L.; Nortier, J.L. Balkan Endemic Nephropathy and the Causative Role of Aristolochic Acid. Semin. Nephrol. 2019, 39, 284–296. [Google Scholar] [CrossRef]
- Groopman, E.E.; Rasouly, H.M.; Gharavi, A.G. Genomic medicine for kidney disease. Nat. Rev. Nephrol. 2018, 14, 83–104. [Google Scholar] [CrossRef]
- Willows, J.; Brown, M.; Sheerin, N.S. The role of complement in kidney disease. Clin. Med. 2020, 20, 156–160. [Google Scholar] [CrossRef]
- Granata, S.; Dalla Gassa, A.; Tomei, P.; Lupo, A.; Zaza, G. Mitochondria: A new therapeutic target in chronic kidney disease. Nut. Metab. 2015, 12, 49. [Google Scholar] [CrossRef]
- Eirin, A.; Lerman, A.; Lerman, L.O. The Emerging Role of Mitochondrial Targeting in Kidney Disease. Handb. Exp. Pharmacol. 2017, 240, 229–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, P.K.-T.; Garcia-Garcia, G.; Lui, S.-F.; Andreoli, S.; Fung, W.W.-S.; Hradsky, A.; Kumaraswami, L.; Liakopoulos, V.; Rakhimova, Z.; Saadi, G.; et al. Kidney health for everyone everywhere-from prevention to detection and equitable access to care. Blood Purif. 2021, 50, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Country/Region | |||
|---|---|---|---|
| Bulgaria | Count | Age-Standardized Rate per 100,000 | Percentage Change in Age-Standardized Rates between 1990 and 2017 |
| Prevalence (95% UI) | |||
| 981,339 (909,610 to 1,061,687) | 8000 (7420 to 8630) | 2.6% (−0.7 to 5.9) | |
| Croatia | 562,778 (520,865 to 610,153) | 7779 (7206 to 8390) | 1.2% (−3.1 to 6.2) |
| Serbia | 1,142,513 (1,063,208 to 1,237,929) | 8421 (7846 to 9069) | −0.5% (−4.1 to 3.3) |
| Slovenia | 266,527 (247,205 to 289,578) | 7581 (7056 to 8179) | −1.1% (−5.7 to 3.2) |
| Central Europe | 13,951,402 (12,930,450 to 15,136,020) | 7659 (7115 to 8282) | −2.7% (−6.2 to 1.4) |
| Mortality (95% UI) | |||
| Bulgaria | 1447 (1346 to 1557) | 10.1 (9.4 to 10.8) | 45.7% (35.3 to 57.2) |
| Croatia | 829 (776 to 888) | 8.8 (8.2 to 9.4) | 35.3% (25.6 to 46.0) |
| Serbia | 2386 (1982 to 2607) | 14.8 (12.4 to 16.1) | 18.8% (7.3 to 32.0) |
| Slovenia | 213 (195 to 232) | 4.4 (4.0 to 4.8) | −30.2% (−36.7 to −23.1) |
| Central Europe | 16,284 (15,806 to 16,706) | 7.5 (7.3 to 7.7) | −21.2% (−23.6 to −18.9) |
| A. Diagnosis of CKD | |
| One or more markers of kidney damage present for >3 months |
|
| OR | |
| eGFR <60 mL/min/1.73 m2 persistently present >3 months | |
| B. Staging of CKD | |
| Stage | eGFR values (mL/min/1.73 m2) |
| G1 | ≥90 |
| G2 | 60–89 |
| G3a | 45–59 |
| G3b | 30–44 |
| G4 | 15–29 |
| G5 | <15 |
| Challenges in Diagnosis |
|---|
|
| Challenges in Treatment |
|
| Gaps in the Referral Pathway |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitić, I.; Laganović, M.; Marinova, I.; Gancheva, N.; Nakić, V.; Melentijevic, D.; Paskalev, E.; Vajd, R.; Škoberne, A. Chronic Kidney Disease in Balkan Countries—A Call to Action for Timely Diagnosis and Monitoring. Diagnostics 2022, 12, 2162. https://doi.org/10.3390/diagnostics12092162
Mitić I, Laganović M, Marinova I, Gancheva N, Nakić V, Melentijevic D, Paskalev E, Vajd R, Škoberne A. Chronic Kidney Disease in Balkan Countries—A Call to Action for Timely Diagnosis and Monitoring. Diagnostics. 2022; 12(9):2162. https://doi.org/10.3390/diagnostics12092162
Chicago/Turabian StyleMitić, Igor, Mario Laganović, Ivelina Marinova, Nina Gancheva, Valentina Nakić, Dragana Melentijevic, Emil Paskalev, Rajko Vajd, and Andrej Škoberne. 2022. "Chronic Kidney Disease in Balkan Countries—A Call to Action for Timely Diagnosis and Monitoring" Diagnostics 12, no. 9: 2162. https://doi.org/10.3390/diagnostics12092162
APA StyleMitić, I., Laganović, M., Marinova, I., Gancheva, N., Nakić, V., Melentijevic, D., Paskalev, E., Vajd, R., & Škoberne, A. (2022). Chronic Kidney Disease in Balkan Countries—A Call to Action for Timely Diagnosis and Monitoring. Diagnostics, 12(9), 2162. https://doi.org/10.3390/diagnostics12092162






