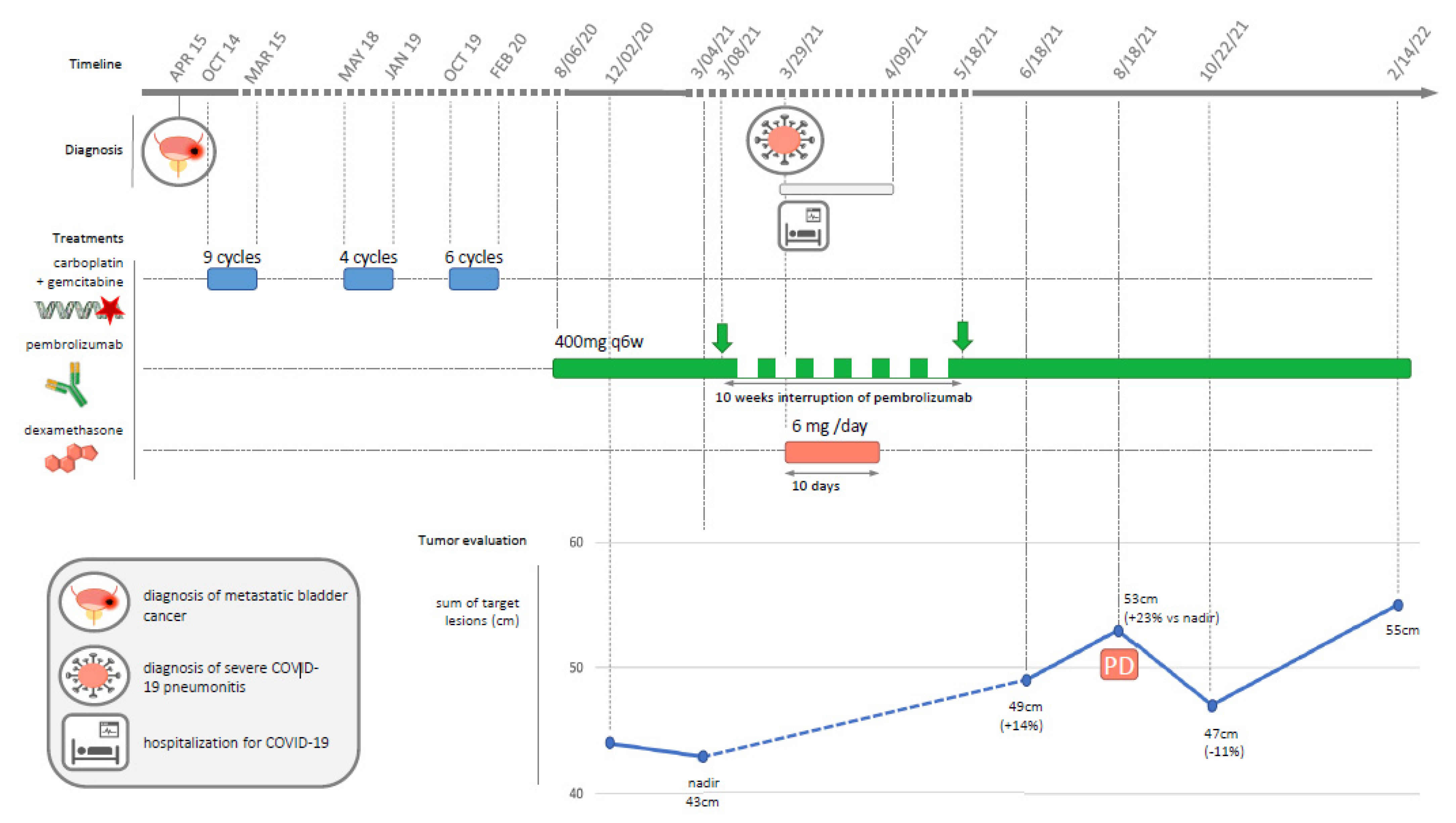
Reversible Tumor Progression Induced by a Dexamethasone Course for Severe COVID-19 during Immune Checkpoint Inhibitor Treatment
Abstract
:

Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The RECOVERY Collaborative Group. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Giles, A.J.; Hutchinson, M.-K.N.D.; Sonnemann, H.M.; Jung, J.; Fecci, P.E.; Ratnam, N.M.; Zhang, W.; Song, H.; Bailey, R.; Davis, D.; et al. Dexamethasone-Induced Immunosuppression: Mechanisms and Implications for Immunotherapy. J. Immunother. Cancer 2018, 6, 51. [Google Scholar] [CrossRef] [PubMed]
- Alfarouk, K.O.; AlHoufie, S.T.S.; Ahmed, S.B.M.; Shabana, M.; Ahmed, A.; Alqahtani, S.S.; Alqahtani, A.S.; Alqahtani, A.M.; Ramadan, A.M.; Ahmed, M.E.; et al. Pathogenesis and Management of COVID-19. J. Xenobiot. 2021, 11, 77–93. [Google Scholar] [CrossRef] [PubMed]
- Geraud, A.; Gougis, P.; Vozy, A.; Anquetil, C.; Allenbach, Y.; Romano, E.; Funck-Brentano, E.; Moslehi, J.J.; Johnson, D.B.; Salem, J.-E. Clinical Pharmacology and Interplay of Immune Checkpoint Agents: A Yin-Yang Balance. Annu. Rev. Pharmacol. Toxicol. 2021, 61, 85–112. [Google Scholar] [CrossRef] [PubMed]
- Libert, C.; Dejager, L. How Steroids Steer T Cells. Cell Rep. 2014, 7, 938–939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brahmer, J.R.; Lacchetti, C.; Schneider, B.J.; Atkins, M.B.; Brassil, K.J.; Caterino, J.M.; Chau, I.; Ernstoff, M.S.; Gardner, J.M.; Ginex, P.; et al. Management of Immune-Related Adverse Events in Patients Treated With Immune Checkpoint Inhibitor Therapy: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2018, 36, 1714–1768. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.C.; Pennell, N.A. Early Use of Systemic Corticosteroids in Patients with Advanced NSCLC Treated with Nivolumab. J. Thorac. Oncol. 2018, 13, 1771–1775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arbour, K.C.; Mezquita, L.; Long, N.; Rizvi, H.; Auclin, E.; Ni, A.; Martínez-Bernal, G.; Ferrara, R.; Lai, W.V.; Hendriks, L.E.L.; et al. Impact of Baseline Steroids on Efficacy of Programmed Cell Death-1 and Programmed Death-Ligand 1 Blockade in Patients with Non–Small-Cell Lung Cancer. JCO 2018, 36, 2872–2878. [Google Scholar] [CrossRef] [PubMed]
- De Giglio, A.; Mezquita, L.; Auclin, E.; Blanc-Durand, F.; Riudavets, M.; Caramella, C.; Martinez, G.; Benitez, J.C.; Martín-Romano, P.; El-Amarti, L.; et al. Impact of Intercurrent Introduction of Steroids on Clinical Outcomes in Advanced Non-Small-Cell Lung Cancer (NSCLC) Patients under Immune-Checkpoint Inhibitors (ICI). Cancers 2020, 12, 2827. [Google Scholar] [CrossRef] [PubMed]
- Buti, S.; Bersanelli, M.; Perrone, F.; Tiseo, M.; Tucci, M.; Adamo, V.; Stucci, L.S.; Russo, A.; Tanda, E.T.; Spagnolo, F.; et al. Effect of Concomitant Medications with Immune-Modulatory Properties on the Outcomes of Patients with Advanced Cancer Treated with Immune Checkpoint Inhibitors: Development and Validation of a Novel Prognostic Index. Eur. J. Cancer 2021, 142, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Petrelli, F.; Signorelli, D.; Ghidini, M.; Ghidini, A.; Pizzutilo, E.G.; Ruggieri, L.; Cabiddu, M.; Borgonovo, K.; Dognini, G.; Brighenti, M.; et al. Association of Steroids Use with Survival in Patients Treated with Immune Checkpoint Inhibitors: A Systematic Review and Meta-Analysis. Cancers 2020, 12, 546. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- EMA Keytruda—European Public Assessment Report. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/keytruda (accessed on 14 December 2021).
- Taves, M.D.; Ashwell, J.D. Glucocorticoids in T Cell Development, Differentiation and Function. Nat. Rev. Immunol. 2021, 21, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Soria, F.; Beleni, A.I.; D’Andrea, D.; Resch, I.; Gust, K.M.; Gontero, P.; Shariat, S.F. Pseudoprogression and Hyperprogression during Immune Checkpoint Inhibitor Therapy for Urothelial and Kidney Cancer. World J. Urol. 2018, 36, 1703–1709. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurra, V.; Sullivan, R.J.; Gainor, J.F.; Hodi, F.S.; Gandhi, L.; Sadow, C.A.; Harris, G.J.; Flaherty, K.; Lee, S. Pseudoprogression in Cancer Immunotherapy: Rates, Time Course and Patient Outcomes. JCO 2016, 34, 6580. [Google Scholar] [CrossRef]
- Hodi, F.S.; Ballinger, M.; Lyons, B.; Soria, J.-C.; Nishino, M.; Tabernero, J.; Powles, T.; Smith, D.; Hoos, A.; McKenna, C.; et al. Immune-Modified Response Evaluation Criteria In Solid Tumors (ImRECIST): Refining Guidelines to Assess the Clinical Benefit of Cancer Immunotherapy. J. Clin. Oncol. 2018, 36, 850–858. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gougis, P.; Abbar, B.; Benzimra, J.; Vozy, A.; Spano, J.-P.; Campedel, L. Reversible Tumor Progression Induced by a Dexamethasone Course for Severe COVID-19 during Immune Checkpoint Inhibitor Treatment. Diagnostics 2022, 12, 1933. https://doi.org/10.3390/diagnostics12081933
Gougis P, Abbar B, Benzimra J, Vozy A, Spano J-P, Campedel L. Reversible Tumor Progression Induced by a Dexamethasone Course for Severe COVID-19 during Immune Checkpoint Inhibitor Treatment. Diagnostics. 2022; 12(8):1933. https://doi.org/10.3390/diagnostics12081933
Chicago/Turabian StyleGougis, Paul, Baptiste Abbar, Julie Benzimra, Aurore Vozy, Jean-Philippe Spano, and Luca Campedel. 2022. "Reversible Tumor Progression Induced by a Dexamethasone Course for Severe COVID-19 during Immune Checkpoint Inhibitor Treatment" Diagnostics 12, no. 8: 1933. https://doi.org/10.3390/diagnostics12081933
APA StyleGougis, P., Abbar, B., Benzimra, J., Vozy, A., Spano, J.-P., & Campedel, L. (2022). Reversible Tumor Progression Induced by a Dexamethasone Course for Severe COVID-19 during Immune Checkpoint Inhibitor Treatment. Diagnostics, 12(8), 1933. https://doi.org/10.3390/diagnostics12081933






