1. Introduction
Vulto-van Silfhout-de Vries syndrome (VSVS; OMIM# 615828) is an orphan disease with an autosomal dominant type of inheritance, associated with impaired speech and intellectual development, delayed psychomotor development, and behavioral anomalies, including autistic behavioral traits and poor eye contact.
VSVS was first described by Vulto-van Silfhout (The Netherlands) in 2014 for four patients with delayed psychomotor and intellectual development with totally absent or impaired speech [
1]. Currently, 27 cases of VSVS have been reviewed in the world literature. In addition to psychomotor abnormalities, most patients have additional nonspecific signs, such as hypotonia, gait disorders, seizures (that may be refractory), a high pain threshold, and sleep disorders [
2].
VSVS occurs as a result of pathogenic germline mutations in the
DEAF1 gene, which encodes deformed epidermal autoregulatory factor-1 (
DEAF1).
DEAF1 is involved in the regulation of multiple genes, showing high expressive activity in brain tissues, which explains its key role in the early development of the fetal central nervous system [
3].
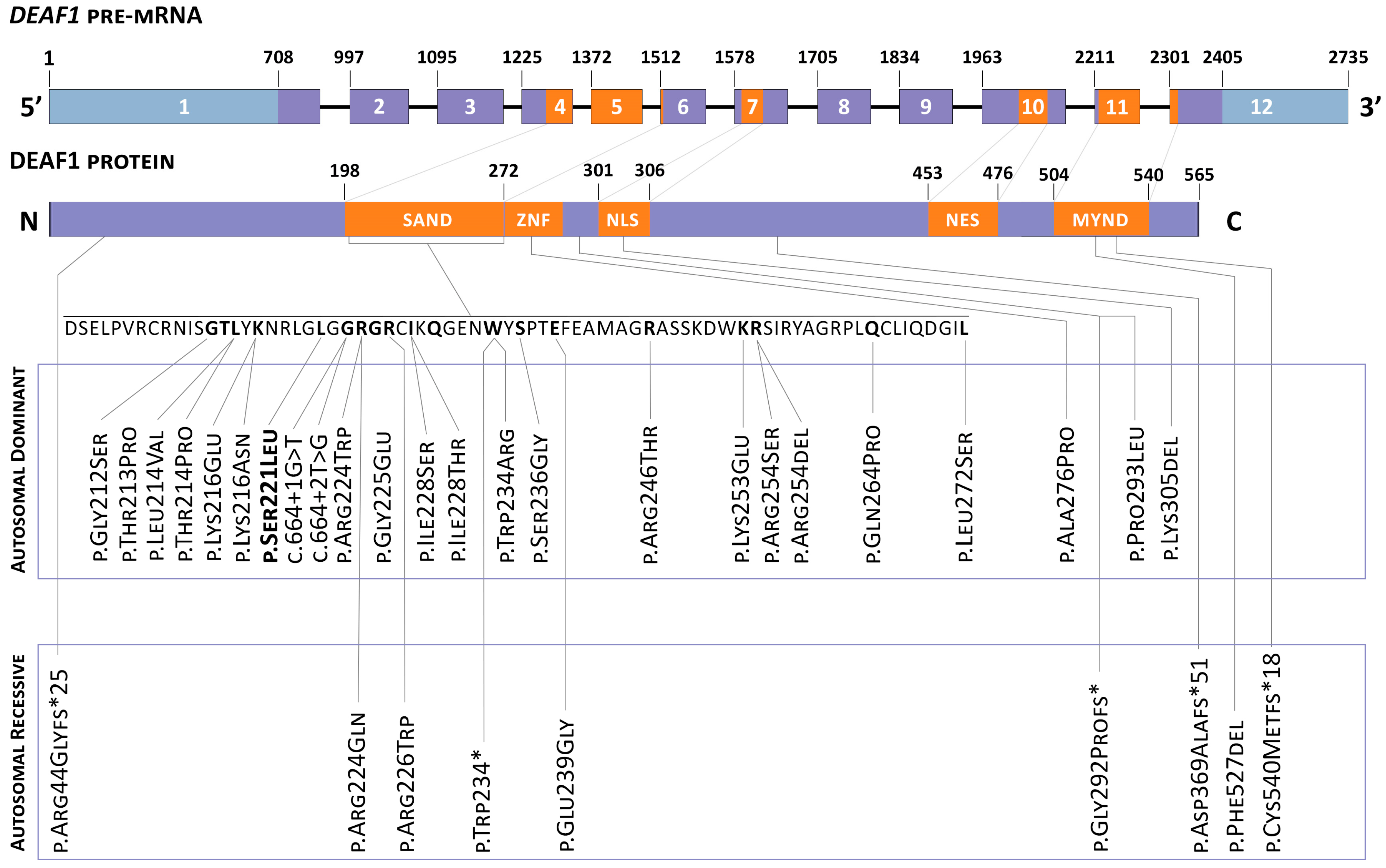
In most cases, mutations in the
DEAF1 gene are represented by “de novo” missense variants. The assessment of phenotypic–genotypic correlation showed no significant differences between heterozygous or homo- and compound-heterozygous mutation carriers, except for the presence of microcephaly in carriers of biallelic pathogenic variants in the
DEAF1 gene. The overall spectrum of detected variants of the
DEAF1 gene is described in
Figure 1 (adapted from ‘De novo and biallelic
DEAF1 variants cause a phenotypic spectrum’/Maria J. Nabais Sá, MD, PhD. Genetics in medicine) [
4].
The article describes a clinical case of a patient who had a heterozygous carrier of variant c.662C > T in the DEAF1 gene responsible for the development of Vulto-van Sylfhout-de Vries syndrome. The mentioned variant of the DEAF1 gene was not previously described either in the scientific literature or in any genomic database.
2. Clinical Case
The proband is a male patient (Russian/Ukrainian origin), 23-years-old, hospitalized to the State Budgetary Healthcare Institution—The Loginov Moscow Clinical Scientific Center—of Moscow Healthcare Department complaining of prominent fatigue, muscle weakness, weight loss, diarrhea (stool up to 2–3 times a day of mushy consistency and small amount, without pathological impurities), and edema of the lower extremities. The patient was accompanied by his mother, and could not establish personal or visual contact with the physician upon examination. According to his mother, the mentioned complaints appeared two months ago after receiving antibacterial therapy.
In terms of anamnesis vitae, the proband was born at 39 weeks of gestation from the first pregnancy complicated by development of the first trimester toxicosis. His weight and height at birth were 3200 g and 53 cm, respectively. The early motor development of the patient was normal.
In terms of anamnesis morbi, at the age of 2.5 years, mental developmental regression became evident, phrasal speech was missing, and the proband could say only individual sounds and syllables. According to the complaints mentioned, an autism spectrum disorder (ASD) was diagnosed. Epileptic seizures started at 5 years of age. Since then, seizures developed every 2–3 months. The proband received symptomatic treatment with anticonvulsants (valproic acid).
Growth retardation in the patient was first noted at 12 years of age. At 14 years old, due to severe stress and prominent appetite decrease, the patient started losing weight progressively. At 16 years old, the boy was hospitalized to the clinic to exclude an endocrine nature of his weight loss and growth retardation (weight 26.5 kg, SDS 6.68, height 143.5 sm, SDS-4.45). X-ray examination (and TW 20) showed that his bone age was 12.7 years old. The diagnosis on discharge was delayed physical and sexual development, i.e., cachexia (BMI 12.87 kg/m2 SDS 5.55). Brain MRI revealed no structural abnormality.
At 22 years old, the patient was first diagnosed with primary hypothyroidism, and therefore levothyroxine therapy was started. Adrenal as well as somatotropin insufficiency was excluded. There was an increase of the alkaline phosphatase level up to 147 IU/L (30–120), moderate hypoglycemia up to 3.7 mmol/L (4.9–5.1), and an increase of vitamin B12 up to 2179 pg/mL (189–833).
Throughout his life, numerous different genetic tests were conducted to identify the cause of the ASD in the proband. Numerical and large chromosomal aberrations such as micro-deletion and micro-duplication syndromes were excluded by karyotyping and DNA-microarray analysis (karyotype 46,XY; molecular karyotype arr(1–22)x2,(X,Y)x1). Molecular analysis of the abnormal methylation of the FMR1 gene promoter region did not reveal any changes typical for Fragile X syndrome. Aminoacidopathies and aminoaciduria associated with ASD were also excluded by the tandem mass spectrometry of amino acids and organic acids in the blood.
The deterioration that led to the patient’s current hospitalization occurred 6 months prior to the admission, after the antibiotic therapy of a urinary tract infection followed by an increase in stool frequency up to 5–6 times a day. An abdominal CT showed a small bilateral hydrothorax, pronounced ascites, and an increased amount of gas in the intestinal loops. Upon a consultation with a gastroenterologist of the State B H I—The Loginov Moscow Clinical Scientific Center—of Moscow Healthcare Department, it was decided to hospitalize the patient for further investigation and treatment.
Upon admission, the patient’s condition was severe. The somatic status highlighted his short stature (143 cm), signs of hypogonadism, and cachexia (weight 31 kg). Consciousness was clear. The patient was sluggish, retarded, and demonstrated aggressive behavior and the active rejection of examination and medical interventions. No verbal contact was possible. The patient did not follow commands even to perform simple motor actions. According to the mother, the patient can write, but did not demonstrate any writing skills during the examination. Upon cranial nerve examination, the sense of smell was not evaluated, fields of vision were not limited, and there was full movement of the eyeballs: convergent strabismus due to the right eye, medium-sized pupils, S = D, normal eye slits, S = D, direct and cross photoreaction of the pupils preserved, satisfactory convergence, and no nystagmus was noted. Face surface sensitivity was normal. Masticatory muscle strength was 5/5 Medical Research Council Weakness Scale (MRC) points on both sides. The face was symmetrical and mobile. Hearing was not reduced. Swallowing was not impaired. Sternocleidomastoid and trapezius muscle strength was 5/5 MRC points on both sides. Muscle tone was slightly reduced. The upper and lower extremities’ strength was 4/5 MRC points on both sides. Tendon reflexes were of medium agility, S = D. No pathological symptoms were noted. The patient was not able to perform coordination tests, but did perform purposeful movements without an action tremor or discoordination. His mother moved him around in a wheelchair. The patient underwent routine electroencephalography (EEG), which did not record any typical epileptiform activity.
The patient was consulted by a gastroenterologist, a nutritionist and a neurologist. CT revealed hydrothorax on the left with the formation of compression atelectasis, signs of gastrostasis, a picture of inflammatory changes in the walls of the colon, total lesion in the active stage, and pronounced ascites. According to the laboratory data, there was a decrease in total protein down to 53 g/L (64–83), creatinine to 39 μmol/L (80–115), and hemoglobin to 8.2 g/dL (13.0–16.0); there was an increase in presepsin to 247 pg/mL (0–155). Clostridium Difficile was revealed (Toxin A and B positive).
Considering the presence of systemic pathology and ASD signs, consultation of clinical geneticist was performed. The patient’s phenotype was characterized by a short stature (143 cm), being underweight (31 kg), an impaired posture with kyphosis, a superficial location of the saphenous veins and marbling of the skin, multiple diffusely located nevi, freckles and small hyperpigmentation spots on the neck, an elongated face, hypertelorism of the eyes, a short nose, bilateral epicanthic folds, strabismus, an opened mouth, dry lips, attached earlobes, and impaired dermatoglyphics on the palms (
Figure 2).
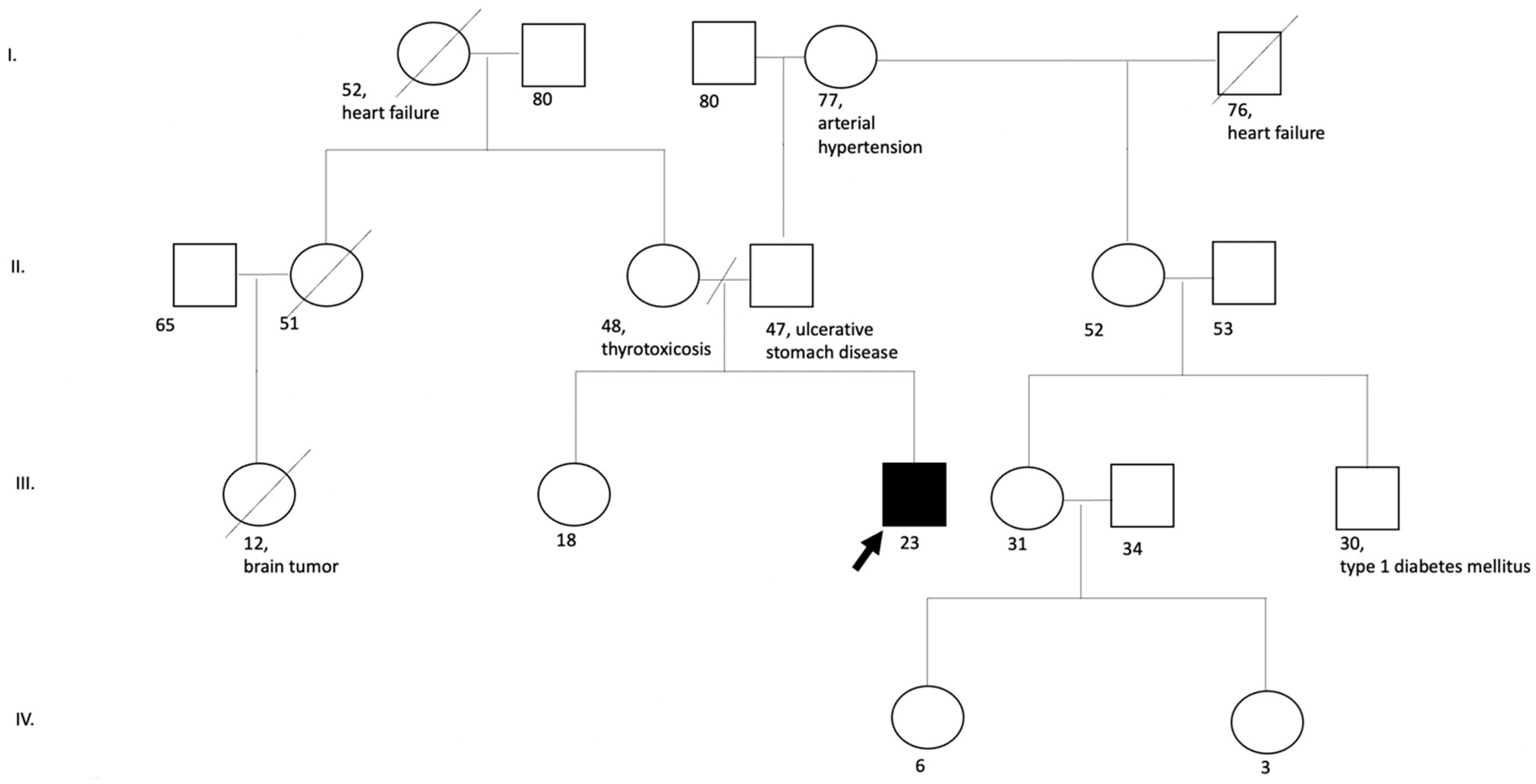
No clinical disorders similar to the disease of the proband were revealed in the family history (the patient has a healthy sibling, and the parents are not relatives to each other) (
Figure 3).
Taking into account the negative results of the genetic tests performed, the geneticist recommended whole-genome sequencing.
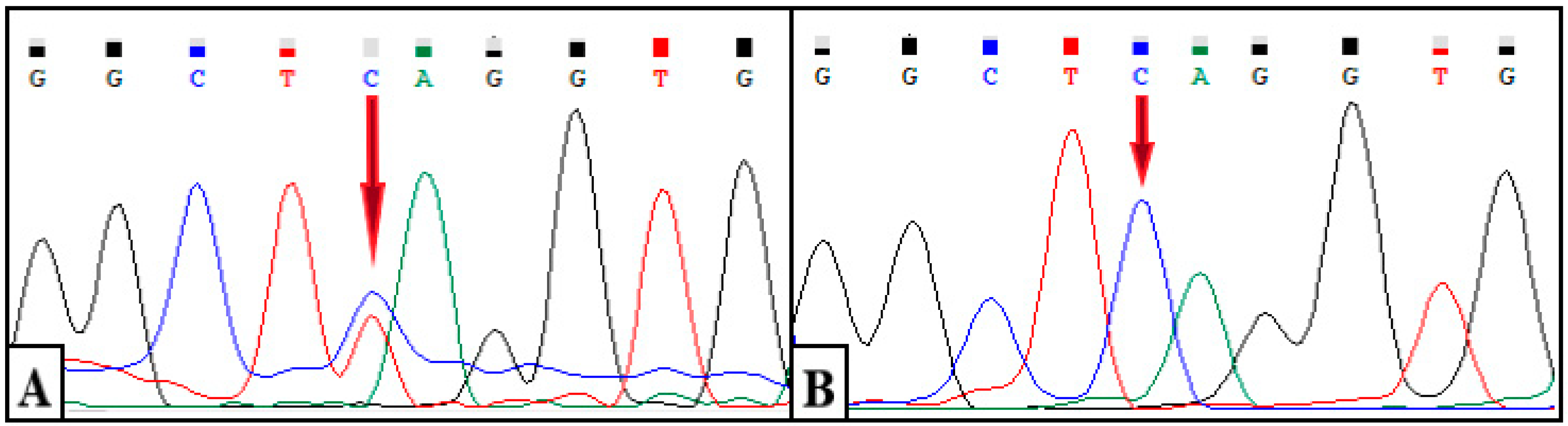
The results showed a heterozygous variant chr11: 687913G > A (c.662C > T, p.S221L) in exon 4 of the
DEAF1 gene (NM_001293634.1). The identified variant is represented by a missense variant and leads to a substitution of serine for leucine at position 221 of the protein
DEAF1 (
Figure 4A). A segregation analysis was carried out for the identified variant c.662C > T of the
DEAF1 gene in his mother, father, and sister. As a result of Sanger sequencing, the wild-type genotype (c.662C/C) was revealed in all of the relatives studied. (
Figure 4B).
This variant had not been previously described in the gnomAD, 1000 G, ClinVar, ExAC, or Human Genome Mutation and Human Genome Variation. The substitution c.662C > T is localized in the highly conserved gene region (PM2), and the results of ten algorithms for the in silico prediction of pathogenicity (BayesDel_addAF, DANN, DEOGEN2, EIGEN, FATHMM-MKL, LIST-S2, M-CAP, MutationAssessor, MutationTaster and SIFT) confirm the pathogenic effect of the variant on the gene and its effect on protein splicing and functionality (PP3); additionally, more than 59.4% of variants (including missense mutations) in the SAND domain of the DEAF1 gene are pathogenic (PM1). This codon previously described the missense variant chr11: 687914A > G (c.661T > C, p.Ser221Pro), annotated as likely pathogenic (PM5). Considering that the phenotype of the proband is highly specific for VSVS (PP4), and as a result of segregation analysis in the family, a “de novo” character of alteration in the patient (PP4) was established; according to the criteria of the American College of Medical Genetics, this nucleotide substitution can be considered as a pathogenic, clinically significant variant.
The final clinical diagnosis was: VSVS syndrome, epileptic encephalopathy, pseudomembranous colitis associated with ClDifficile (Toxin A and B positive), and metabolic disorders—hypoproteinemia, anasarca, ascites, and cachexia.
The patient’s treatment included antibacterial and symptomatic therapy to correct water-electrolyte disturbances due to long-term persistent pseudomembranous colitis.
The patient was discharged with some improvement in his condition under the supervision of specialists. Given the history of cachexia, with the identified genetic syndrome, and the associated long-term persistent infection (Cl. Difficile), the prognosis of the patient appears to be poor.
5. Materials and Methods
All of the participants signed informed consent prior to genetic testing.
WGS was performed NGS on the MiSeq (Argonne, IL USA). The sequencing data results were analyzed using an automated algorithm, including the alignment of the reads to the reference sequence of the human genome (hg19), post-processing alignment, the identification of variants and the filtering of variants by sequencing quality, as well as the annotation of the identified variants according to all of the transcripts of each gene from the RefSeq database and using the predictive programs SIFT, PolyPhen2-HDIV, PolyPhen2-HVAR, MutationTaster, LRTPhyloP, and PhastCons.
The ACMG recommendations were used to annotate the identified variants. Samples from the 1000 Genomes, ESP6500, Exome Aggregation Consortium, and gnomAD projects were used to estimate the population frequencies of the identified variants. The OMIM database and worldwide literature data were used to assess the clinical relevance of the identified variants.
Genomic DNA was isolated from peripheral venous blood samples by the sorbent method (Sample-GS-Genetics, LLC DNA-Technology Research &Production, Moscow, Russia) according to the manufacturer’s protocol. DNA concentrations were measured with a Qubit 2.0 Fluorometer (Thermo Fisher Scientific, Waltham, MA, USA) using a Qubit ™ dsDNA High Sensitivity Assay Kit (Thermo Fisher Scientific). The isolated DNA was then amplified with a polymerase chain reaction (PCR) using oligonucleotide primers.
Table 2 shows the Senger sequencing performed using the BigDyeTM Terminator v3.1 Cycle Sequencing Kit (Thermo Fister Scientific, Waltham, MA, USA) according to the manufacturer’s protocol. The detection of sequencing products was performed by Applied Biosystems 3500 (Thermofister Scientific, Waltham, MA, USA).