Effective Prevention and Management Tools for Metabolic Syndrome Based on Digital Health-Based Lifestyle Interventions Using Healthcare Devices
Abstract
:1. Introduction
1.1. Background
1.2. Lifestyle Interventions and Self-Care
1.3. Objective
2. Materials and Methods
2.1. Definition of Metabolic Syndrome
2.2. Design
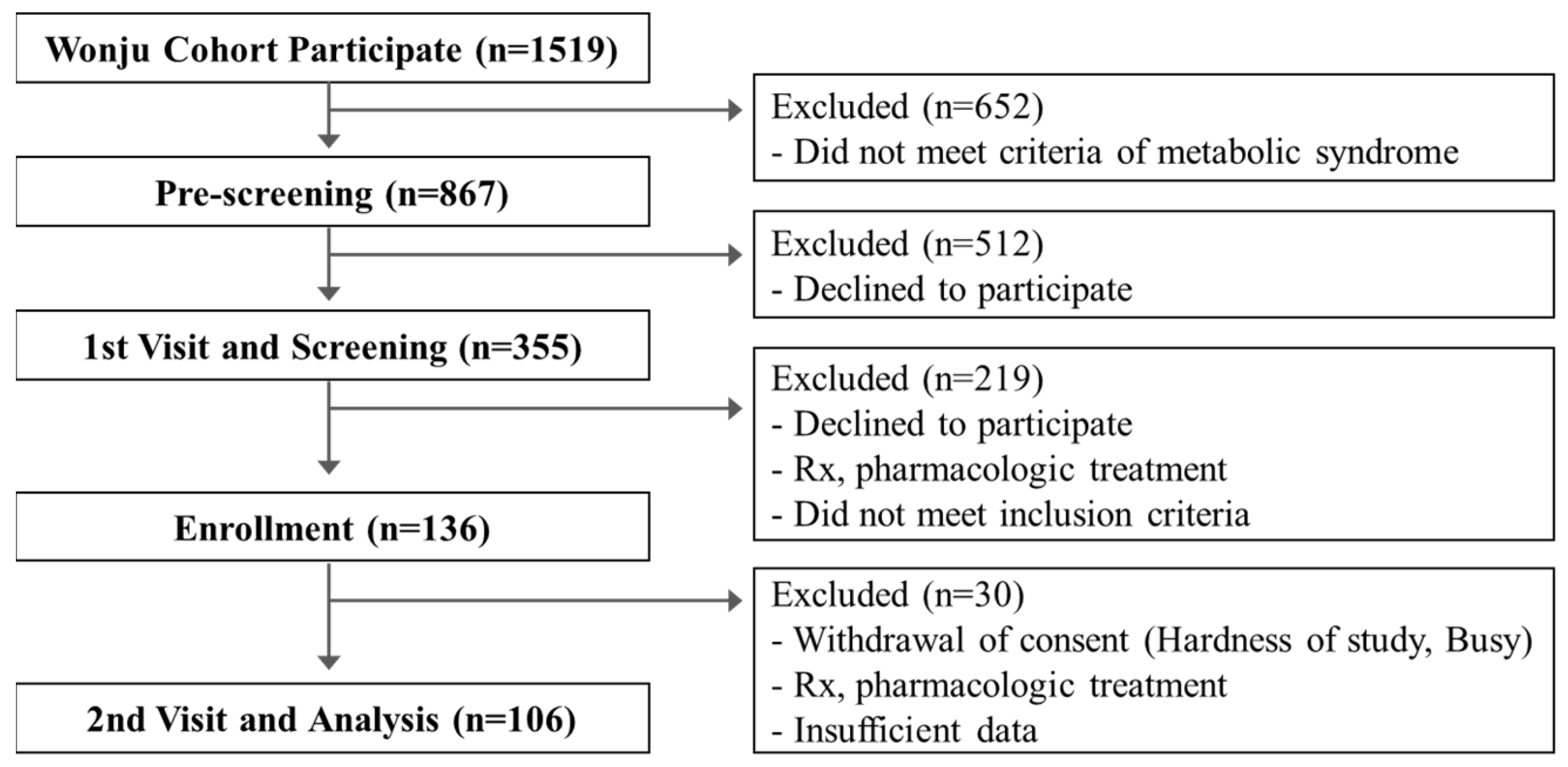
2.3. Participants
2.4. Collection of Lifelog Data Using Healthcare Devices
2.5. Group Classification
2.6. Engagement, Persistence, and Physical Activity
2.7. Prevention and Management of Metabolic Syndrome
2.8. Statistical Analysis
3. Results
3.1. Participant’s Characteristics between the Baseline and Follow-Up
3.2. Effectiveness of Digital Health-Based Lifestyle Interventions
3.3. Characteristic of Self-Care Using Healthcare Devices
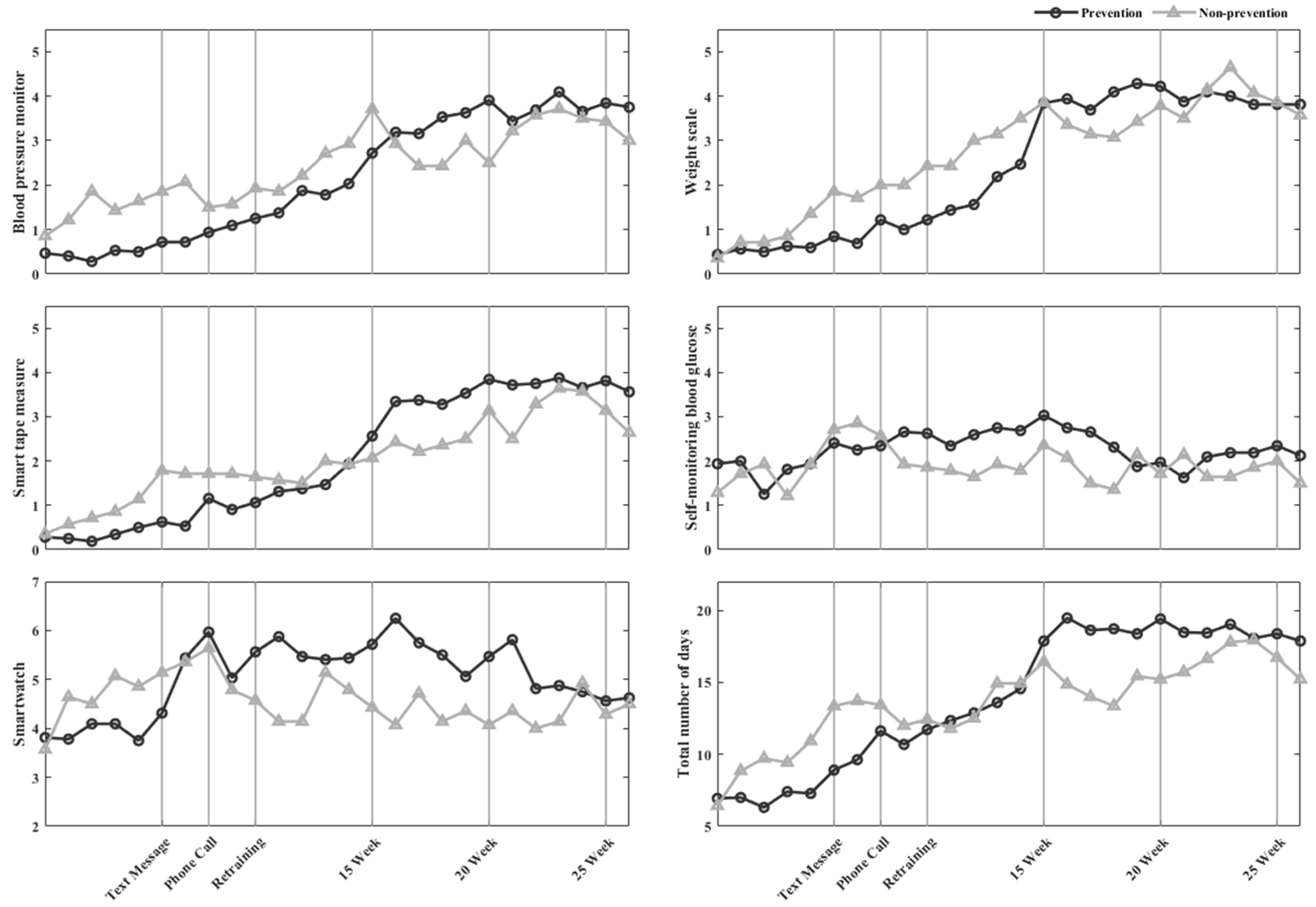
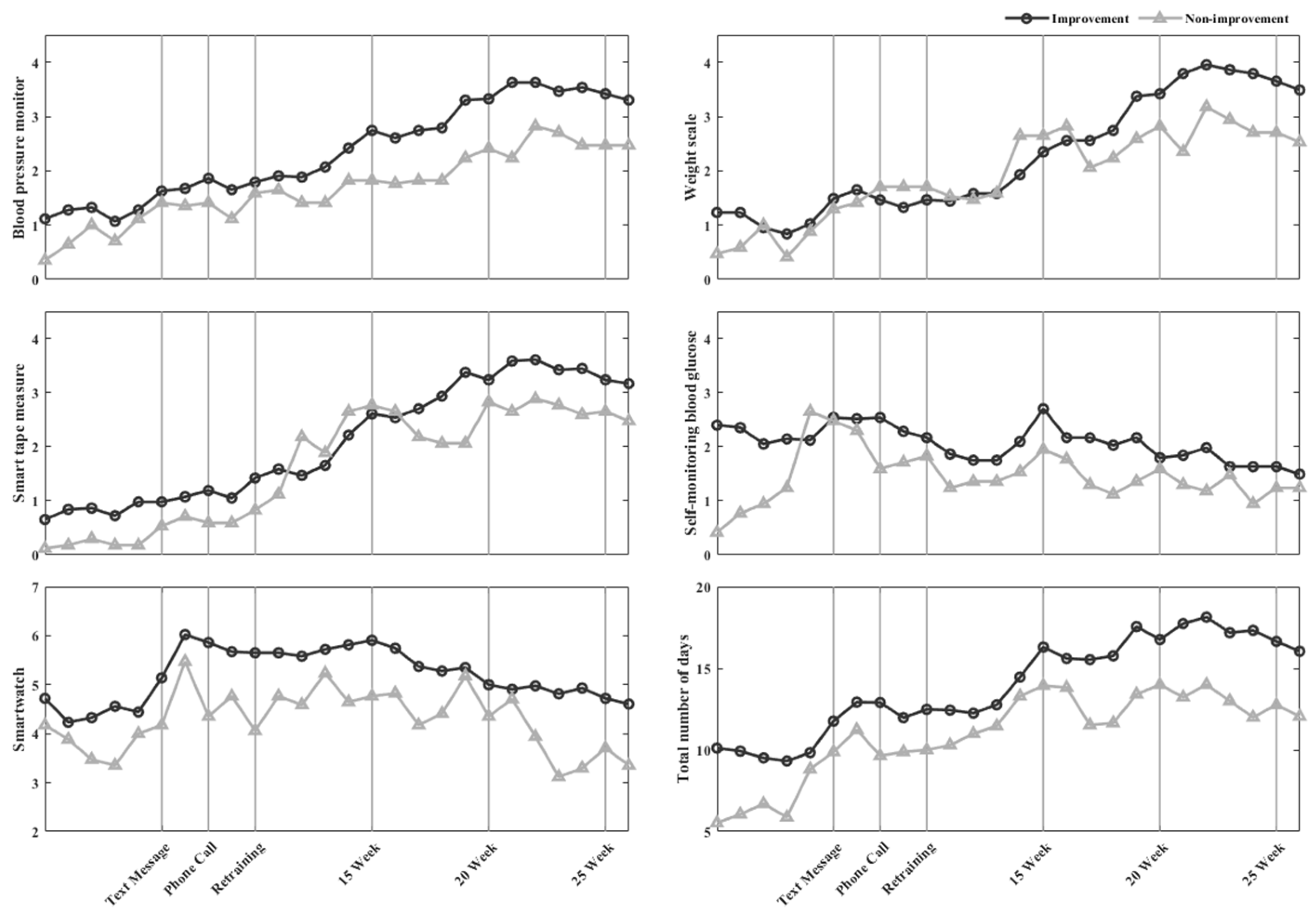
3.3.1. The Frequency of Healthcare Device Use
3.3.2. Engagement and Persistence
3.3.3. Physical Activity
3.4. Prevention and Management of Metabolic Syndrome
4. Discussion
4.1. Management Tool of MetS Using Healthcare Devices
4.2. Digital Health-Based Lifestyle Intervention
4.3. Engagement, Persistence, and Physical Activity
4.4. Change in Risk Factors
4.5. Drop-Out
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alberti, K.G.M.; Zimmet, P.; Shaw, J. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef]
- Noubiap, J.J.; Nansseu, J.R.; Lontchi-Yimagou, E.; Nkeck, J.R.; Nyaga, U.F.; Ngouo, A.T.; Tounouga, D.N.; Tianyi, F.L.; Foka, A.J.; Ndoadoumgue, A.L. Geographic distribution of metabolic syndrome and its components in the general adult population: A meta-analysis of global data from 28 million individuals. Diabetes Res. Clin. Pract. 2022, 188, 109924. [Google Scholar] [CrossRef] [PubMed]
- Papaioannou, K.-G.; Kadi, F.; Nilsson, A. Benefits of fruit and vegetable consumption on prevalence of metabolic syndrome are independent of physical activity behaviors in older adults. Nutrients 2022, 14, 263. [Google Scholar] [CrossRef]
- Liang, X.; Or, B.; Tsoi, M.F.; Cheung, C.L.; Cheung, B.M. Prevalence of Metabolic Syndrome in the United States National Health and Nutrition Examination Survey (NHANES) 2011–2018. Eur. Heart J. 2021, 42, 2420. [Google Scholar] [CrossRef]
- Kim, M.-h.; Lee, S.-h.; Shin, K.-S.; Son, D.-Y.; Kim, S.-H.; Joe, H.; Yoo, B.-W.; Hong, S.-H.; Cho, C.-Y.; Shin, H.-S. The change of metabolic syndrome prevalence and its risk factors in Korean adults for decade: Korea National Health and Nutrition Examination Survey for 2008–2017. Korean J. Fam. Pract. 2020, 10, 44–52. [Google Scholar] [CrossRef]
- Huang, J.-H.; Li, R.-H.; Huang, S.-L.; Sia, H.-K.; Chen, Y.-L.; Tang, F.-C. Lifestyle factors and metabolic syndrome among workers: The role of interactions between smoking and alcohol to nutrition and exercise. Int. J. Environ. Res. Public Health 2015, 12, 15967–15978. [Google Scholar] [CrossRef] [Green Version]
- Cho, D.Y.; Koo, J.-W. Differences in metabolic syndrome prevalence by employment type and sex. Int. J. Environ. Res. Public Health 2018, 15, 1798. [Google Scholar] [CrossRef] [Green Version]
- Kassi, E.; Pervanidou, P.; Kaltsas, G.; Chrousos, G. Metabolic syndrome: Definitions and controversies. BMC Med. 2011, 9, 48. [Google Scholar] [CrossRef] [Green Version]
- Gheorghe, G.; Toth, P.P.; Bungau, S.; Behl, T.; Ilie, M.; Pantea Stoian, A.; Bratu, O.G.; Bacalbasa, N.; Rus, M.; Diaconu, C.C. Cardiovascular risk and statin therapy considerations in women. Diagnostics 2020, 10, 483. [Google Scholar] [CrossRef]
- Vesa, C.M.; Popa, L.; Popa, A.R.; Rus, M.; Zaha, A.A.; Bungau, S.; Tit, D.M.; Corb Aron, R.A.; Zaha, D.C. Current data regarding the relationship between type 2 diabetes mellitus and cardiovascular risk factors. Diagnostics 2020, 10, 314. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magkos, F.; Yannakoulia, M.; Chan, J.L.; Mantzoros, C.S. Management of the metabolic syndrome and type 2 diabetes through lifestyle modification. Annu. Rev. Nutr. 2009, 29, 223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dalle Grave, R.; Calugi, S.; Centis, E.; Marzocchi, R.; El Ghoch, M.; Marchesini, G. Lifestyle modification in the management of the metabolic syndrome: Achievements and challenges. Diabetes Metab. Syndr. Obes. Targets Ther. 2010, 3, 373. [Google Scholar] [CrossRef] [Green Version]
- Yamaoka, K.; Tango, T. Effects of lifestyle modification on metabolic syndrome: A systematic review and meta-analysis. BMC Med. 2012, 10, 138. [Google Scholar] [CrossRef]
- Sequi-Dominguez, I.; Alvarez-Bueno, C.; Martinez-Vizcaino, V.; Fernandez-Rodriguez, R.; del Saz Lara, A.; Cavero-Redondo, I. Effectiveness of mobile health interventions promoting physical activity and lifestyle interventions to reduce cardiovascular risk among individuals with metabolic syndrome: Systematic review and meta-analysis. J. Med. Internet Res. 2020, 22, e17790. [Google Scholar] [CrossRef]
- Park, J.-M.; Choi, J.-E.; Lee, H.S.; Jeon, S.; Lee, J.-W.; Hong, K.-W. Effect of Walking Steps Measured by a Wearable Activity Tracker on Improving Components of Metabolic Syndrome: A Prospective Study. Int. J. Environ. Res. Public Health 2022, 19, 5433. [Google Scholar] [CrossRef]
- Bassi, N.; Karagodin, I.; Wang, S.; Vassallo, P.; Priyanath, A.; Massaro, E.; Stone, N.J. Lifestyle modification for metabolic syndrome: A systematic review. Am. J. Med. 2014, 127, 1242.e1–1242.e10. [Google Scholar] [CrossRef]
- Michie, S.; Yardley, L.; West, R.; Patrick, K.; Greaves, F. Developing and evaluating digital interventions to promote behavior change in health and health care: Recommendations resulting from an international workshop. J. Med. Internet Res. 2017, 19, e7126. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Widmer, R.J.; Collins, N.M.; Collins, C.S.; West, C.P.; Lerman, L.O.; Lerman, A. Digital health interventions for the prevention of cardiovascular disease: A systematic review and meta-analysis. Mayo Clin. Proc. 2015, 90, 469–480. [Google Scholar] [CrossRef] [Green Version]
- Andersson, G. Internet interventions: Past, present and future. Internet Interv. 2018, 12, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, H.; Ebert, D.D.; Snoek, F. Special issue on digital health interventions in chronic medical conditions. Internet Interv. 2021, 28, 100457. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.; Lee, J.-S.; Lee, S.-K. A technology-mediated interventional approach to the prevention of metabolic syndrome: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 512. [Google Scholar] [CrossRef] [PubMed]
- Huh, U.; Tak, Y.J.; Song, S.; Chung, S.W.; Sung, S.M.; Lee, C.W.; Bae, M.; Ahn, H.Y. Feedback on physical activity through a wearable device connected to a mobile phone app in patients with metabolic syndrome: Pilot study. JMIR mHealth uHealth 2019, 7, e13381. [Google Scholar] [CrossRef]
- Oh, B.; Cho, B.; Han, M.K.; Choi, H.; Lee, M.N.; Kang, H.-C.; Lee, C.H.; Yun, H.; Kim, Y. The effectiveness of mobile phone-based care for weight control in metabolic syndrome patients: Randomized controlled trial. JMIR mHealth uHealth 2015, 3, e4222. [Google Scholar] [CrossRef]
- Mao, A.Y.; Chen, C.; Magana, C.; Barajas, K.C.; Olayiwola, J.N. A mobile phone-based health coaching intervention for weight loss and blood pressure reduction in a national payer population: A retrospective study. JMIR mHealth uHealth 2017, 5, e7591. [Google Scholar] [CrossRef]
- Toro-Ramos, T.; Lee, D.-H.; Kim, Y.; Michaelides, A.; Oh, T.J.; Kim, K.M.; Jang, H.C.; Lim, S. Effectiveness of a smartphone application for the management of metabolic syndrome components focusing on weight loss: A preliminary study. Metab. Syndr. Relat. Disord. 2017, 15, 465–473. [Google Scholar] [CrossRef]
- Kowatsch, T.; Otto, L.; Harperink, S.; Cotti, A.; Schlieter, H. A design and evaluation framework for digital health interventions. IT-Inf. Technol. 2019, 61, 253–263. [Google Scholar] [CrossRef]
- Fappa, E.; Yannakoulia, M.; Pitsavos, C.; Skoumas, I.; Valourdou, S.; Stefanadis, C. Lifestyle intervention in the management of metabolic syndrome: Could we improve adherence issues? Nutrition 2008, 24, 286–291. [Google Scholar] [CrossRef]
- Kim, M.Y.; Lee, E.J. Factors affecting self-care behavior levels among elderly patients with type 2 diabetes: A quantile regression approach. Medicina 2019, 55, 340. [Google Scholar] [CrossRef] [Green Version]
- Jeong, S.; Kim, J.-Y.; Cho, Y.; Koh, S.B.; Kim, N.; Choi, J.R. Genetically, dietary sodium intake is causally associated with salt-sensitive hypertension risk in a community-based cohort study: A mendelian randomization approach. Curr. Hypertens. Rep. 2020, 22, 45. [Google Scholar] [CrossRef] [PubMed]
- Netea, R.; Lenders, J.; Smits, P.; Thien, T. Both body and arm position significantly influence blood pressure measurement. J. Hum. Hypertens. 2003, 17, 459–462. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Lee, D. Healthcare wearable devices: An analysis of key factors for continuous use intention. Serv. Bus. 2020, 14, 503–531. [Google Scholar] [CrossRef]
- Gomez-Delgado, F.; Katsiki, N.; Lopez-Miranda, J.; Perez-Martinez, P. Dietary habits, lipoprotein metabolism and cardiovascular disease: From individual foods to dietary patterns. Crit. Rev. Food Sci. Nutr. 2021, 61, 1651–1669. [Google Scholar] [CrossRef]
- Sarebanhassanabadi, M.; Mirhosseini, S.J.; Mirzaei, M.; Namayandeh, S.M.; Soltani, M.H.; Salehi-Abargouei, A. The association between a dietary habits score and the risk of metabolic syndrome: A cohort study. Clin. Nutr. 2020, 39, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Steinert, A.; Haesner, M.; Steinhagen-Thiessen, E. Activity-tracking devices for older adults: Comparison and preferences. Univers. Access Inf. Soc. 2018, 17, 411–419. [Google Scholar] [CrossRef]
- Tacken, M.; Marcellini, F.; Mollenkopf, H.; Ruoppila, I.; Szeman, Z. Use and acceptance of new technology by older people. Findings of the international MOBILATE survey: ‘Enhancing mobility in later life’. Gerontechnology 2005, 3, 126–137. [Google Scholar] [CrossRef]
| Characteristics | Pre-MetS (n = 46) | MetS (n = 60) | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | p-Value | Baseline | Follow-Up | p-Value | |
| General Characteristics, mean (SD) | ||||||
| Sex (male/female) (n) | 17/29 | - | - | 25/35 | ||
| Age (years) | 63.9 (6.8) | - | - | 65.2 (5.9) | ||
| Height (cm) | 160.1 (8.0) | 159.9 (8.1) | 0.11 | 160.0 (9.3) | 160.0 (9.2) | 0.93 |
| Weight (kg) | 62.1 (9.1) | 61.8 (8.9) | 0.29 | 67.9 (11.4) | 67.1 (11.3) | <0.01 |
| BMI (kg/m2) | 24.2 (2.9) | 24.2 (2.9) | 0.75 | 26.4 (2.7) | 26.0 (2.7) | <0.01 |
| Risk factors | 1.7 (0.5) | 1.6 (1.1) | 0.57 | 3.6 (0.6) | 2.4 (1.1) | <0.01 |
| Risk factors of metabolic syndromes, mean (SD) | ||||||
| WC (cm) | 87.9 (7.5) | 84.4 (7.2) | <0.01 | 93.3 (7.1) | 88.7 (8.4) | <0.01 |
| SBP (mmHg) | 138.0 (15.7) | 125.5 (15.2) | <0.01 | 140.1 (15.7) | 127.0 (13.0) | <0.01 |
| DBP (mmHg) | 90.1 (9.1) | 79.9 (9.2) | <0.01 | 89.6 (8.1) | 80.3 (9.0) | <0.01 |
| FBS (mg/dL) | 92.4 (9.2) | 91.5 (10.9) | 0.56 | 101.7 (10.8) | 96.9 (9.1) | <0.01 |
| HDL-C (mg/dL) | 55.1 (9.0) | 52.9 (10.0) | <0.05 | 46.6 (9.1) | 46.5 (10.0) | 0.97 |
| TG (mg/dL) | 118.6 (55.2) | 136.1 (73.2) | 0.05 | 166.7 (103.1) | 170.7 (114.0) | 0.63 |
| Group Classification (n) | ||||||
| Reduced risk factors | - | 18 | - | 43 | ||
| Consistent risk factors | - | 14 | - | 16 | ||
| Increased risk factors | - | 14 | - | 1 | ||
| Variables | Pre-MetS | MetS | ||||
|---|---|---|---|---|---|---|
| Prevention (n = 32) | Non-Prevention (n = 14) | p-Value | Improvement (n = 43) | Non-Improvement (n = 17) | p-Value | |
| The frequency of healthcare device after 14 weeks, mean (SD) per week | ||||||
| Weight Scale | 3.8 (2.8) | 3.7 (2.3) | 0.47 | 3.2 (2.7) | 2.6 (2.5) | <0.01 |
| Smart tape measure | 3.4 (2.9) | 2.7 (2.5) | <0.01 | 3.1 (2.7) | 2.6 (2.7) | <0.05 |
| Blood pressure monitor | 3.4 (2.8) | 3.1 (2.4) | 0.14 | 3.1 (2.6) | 2.2 (2.5) | <0.01 |
| SMBG | 2.3 (2.1) | 1.8 (1.7) | <0.01 | 1.9 (1.9) | 1.4 (1.6) | <0.01 |
| Smartwatch | 5.3 (2.8) | 4.4 (3.2) | <0.01 | 5.2 (2.9) | 4.2 (3.1) | <0.01 |
| Total number of use days | 18.3 (10.1) | 15.7 (9.2) | <0.01 | 16.5 (9.7) | 13.0 (9.6) | <0.01 |
| Physical activity | 7162.4 (4714.0) | 5837.1 (5034.0) | <0.01 | 7444.3 (5337.3) | 4878.6 (4543.1) | <0.01 |
| Criteria for achievement, mean (SD) per 26 weeks | ||||||
| Engagement | 10.6 (6.1) | 9.9 (6.3) | 0.71 | 10.2 (5.8) | 7.1 (6.1) | 0.07 |
| Persistence | 8.9 (5.7) | 6.8 (4.7) | 0.23 | 7.5 (4.8) | 5.4 (4.9) | 0.13 |
| Change of risk factors (n, %) | ||||||
| Baseline * | 1.6 (0.5) | 1.7 (0.5) | 0.56 | 3.7 (0.7) | 3.3 (0.5) | <0.05 |
| WC | 14 (43.8) | 6 (42.9) | 41 (95.3) | 13 (76.5) | ||
| Blood pressure | 30 (93.8) | 10 (71.4) | 38 (88.4) | 15 (88.2) | ||
| FBS | 3 (9.4) | 2 (14.3) | 26 (60.5) | 12 (70.6) | ||
| HDL-C | 2 (6.3) | 3 (21.4) | 27 (62.8) | 7 (41.2) | ||
| TG | 3 (9.4) | 3 (21.4) | 25 (58.1) | 9 (52.9) | ||
| Follow-up * | 1.0 (1.0) | 2.92 (0.3) | <0.01 | 2.0 (1.0) | 3.4 (0.5) | <0.01 |
| WC | 8 (25.00) | 8 (57.1) | 22 (51.2) | 13 (76.5) | ||
| Blood pressure | 13 (40.62) | 10 (71.4) | 17 (39.5) | 16 (94.1) | ||
| FBS | 2 (6.25) | 4 (28.6) | 9 (20.9) | 9 (52.9) | ||
| HDL-C | 3 (9.37) | 10 (71.4) | 19 (44.2) | 9 (52.9) | ||
| TG | 5 (15.6) | 9 (64.3) | 17 (39.5) | 10 (58.8) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-H.; Lee, K.-H.; Kim, H.-J.; Youk, H.; Lee, H.-Y. Effective Prevention and Management Tools for Metabolic Syndrome Based on Digital Health-Based Lifestyle Interventions Using Healthcare Devices. Diagnostics 2022, 12, 1730. https://doi.org/10.3390/diagnostics12071730
Lee J-H, Lee K-H, Kim H-J, Youk H, Lee H-Y. Effective Prevention and Management Tools for Metabolic Syndrome Based on Digital Health-Based Lifestyle Interventions Using Healthcare Devices. Diagnostics. 2022; 12(7):1730. https://doi.org/10.3390/diagnostics12071730
Chicago/Turabian StyleLee, Jung-Hun, Kang-Hyun Lee, Hee-Jin Kim, Hyun Youk, and Hee-Young Lee. 2022. "Effective Prevention and Management Tools for Metabolic Syndrome Based on Digital Health-Based Lifestyle Interventions Using Healthcare Devices" Diagnostics 12, no. 7: 1730. https://doi.org/10.3390/diagnostics12071730
APA StyleLee, J.-H., Lee, K.-H., Kim, H.-J., Youk, H., & Lee, H.-Y. (2022). Effective Prevention and Management Tools for Metabolic Syndrome Based on Digital Health-Based Lifestyle Interventions Using Healthcare Devices. Diagnostics, 12(7), 1730. https://doi.org/10.3390/diagnostics12071730







