Implementation of Objective Structured Clinical Examination on Diagnostic Musculoskeletal Ultrasonography Training in Undergraduate Traditional Korean Medicine Education: An Action Research
Abstract
1. Introduction
2. Materials and Methods
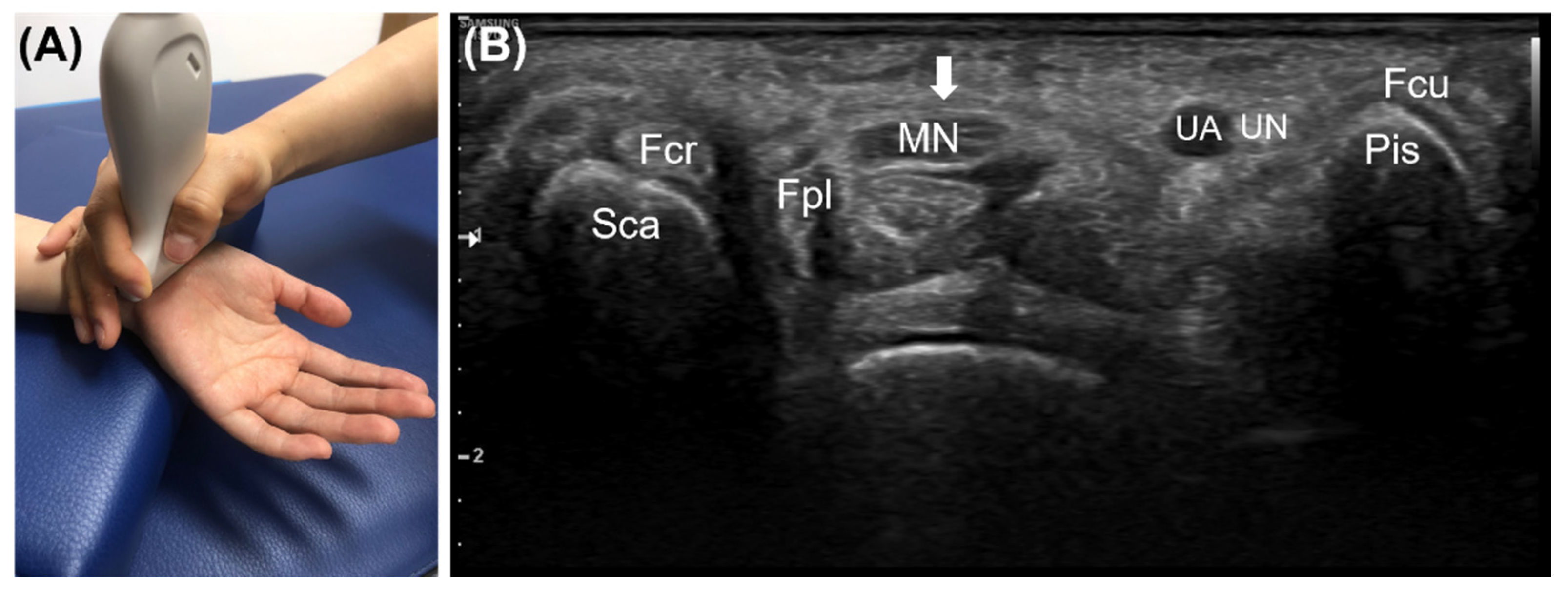
2.1. Course of Diagnostic Musculoskeletal Ultrasound Focused on Volar Wrist and Carpal Tunnel Syndrome
2.2. Study Design and Participants
2.3. Statistical Analysis
3. Results
3.1. Participants
3.2. Students’ Opinions toward Ultrasound Training and OSCE
3.3. Students’ Self-Assessment
3.4. Students’ OSCE Score
4. Discussion
4.1. Summary of Findings
4.2. Debates
4.3. Strengths and Limitations
4.4. Implications and Contributions for Further Education and Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Flexner, A. Medical Education in the United States and Canada; Hangilsa: Paju, Korea, 2005. [Google Scholar]
- Harden, R.M.; Laidlaw, J.M. Essential Skills for a Medical Teacher: An Introduction to Teaching and Learning in Medicine; Academypress: Paju, Korea, 2017. [Google Scholar]
- Harden, R.M.; Lilley, P.; Patricio, M. The Definitive Guide to the OSCE: The Objective Structured Clinical Examination as a Performance Assessment; Elsevier: Edinburgh, UK, 2016. [Google Scholar]
- Patrício, M.F.; Julião, M.; Fareleira, F.; Carneiro, A.V. Is the OSCE a Feasible Tool to Assess Competencies in Undergraduate Medical Education? Med. Teach. 2013, 35, 503–514. [Google Scholar] [CrossRef] [PubMed]
- Tarique, U.; Tang, B.; Singh, M.; Kulasegaram, K.M.; Ailon, J. Ultrasound curricula in undergraduate medical education: A scoping review. J. Ultrasound Med. 2018, 37, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-L.; Hou, M.C.; Lin, S.-C.; Tung, Y.-J. Educational efficacy of objective structured clinical examination on clinical training of traditional Chinese medicine—A qualitative study. Complement. Ther. Clin. Pract. 2015, 21, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.; Lee, J.-H.; Kwon, O.S.; Hong, J.; Cho, N.G. Assessment of acupuncture and moxibustion medicine clinical practice using the objective structured clinical examination. J. Acupunct. Res. 2021, 38, 219–226. [Google Scholar] [CrossRef]
- Cho, E.; Jeon, H.; Kwon, O.S.; Hong, J.; Lee, J.; Jung, E.; Park, J.; Seo, W.; Lim, K.S.; Cho, N.G. Training future Korean medicine doctors to perform bee venom acupuncture and obtain informed consent using an objective structured clinical examination. J. Korean Med. 2022, 43, 6–17. [Google Scholar] [CrossRef]
- Chu, H.; Kim, J.; Ha, W.; Cho, E.; Kang, G.; Park, S.; Jang, J.; Yang, S.B.; Kang, Y.; Lee, S.; et al. Change of safe needling depth at acupoint GB21 according to posture and breathing. Evid. Based Complement. Altern. Med. 2018, 2018, 2308102. [Google Scholar] [CrossRef]
- Chu, H.; Park, K.; Jang, J.; Shin, H.-R.; Yang, M.; Kim, D.R.; Ryu, W.H.; Ryu, H.; Yeom, S.-R.; Lee, S.; et al. Comparison of cervical hyeopcheok acupoint’s depth change with cervical rotation in a prone position: Protocol and pilot study result for accurate observation of cervical hyeopcheok acupoint by ultrasonography. J. Korean Med. Rehabil. 2019, 29, 81–88. [Google Scholar] [CrossRef]
- Go, H.I.; Cho, E.; Jung, H.-J.; Lee, S.; Kim, J.-H.; Kwon, O.S. What is the source of pressure pain during abdominal examination in Korean medicine? Integr. Med. Res. 2020, 9, 100406. [Google Scholar] [CrossRef]
- Park, M.; Kim, S.; Lee, S.; Lee, J.; Lim, J.; Kwon, S.; Jung, I.; Kim, S. The case report of posterior headache caused by traffic accident treated with musculoskeletal ultrasound-guided acupotomy therapy. J. Korean Acupunct. Moxibustion Soc. 2011, 28, 165–172. [Google Scholar]
- Gwak, Yu-Jin; Park, Sang-Hee; Jung, Myung-Ju; Park, Sung-Woo; Park, Ung; Jo, Hee-Guen A case report on 2 cases of patients with uterine fibroids observed an effective result on ultrasonography after Korean traditional medical treatment. J. Korean Obstet. Gynecol. 2015, 28, 147–157. [CrossRef][Green Version]
- Ahn, T.-S.; Moon, J.-H.; Park, C.-Y.; Oh, M.-J.; Choi, Y.-M. The effectiveness of ultrasound-guided essential bee venom pharmacopuncture combined with integrative Korean medical treatment for rib fracture: A case study. J. Korean Med. Rehabil. 2019, 29, 157–163. [Google Scholar] [CrossRef]
- Kim, Y.H.; Oh, T.Y.; Lee, E.J.; Oh, M.S. A comparative study on the pain and treatment satisfaction between Korean medical treatment combined with ultrasound guided soyeom pharmacopuncture therapy in thoracic paravertebral space and non-guided soyeom pharmacopuncture therapy on patients with ribs fracture: A retrospective study. J. Korean Med. Rehabil. 2019, 29, 103–112. [Google Scholar] [CrossRef]
- Wang, B.-R.; Choi, I.Y.; Kim, K.-J.; Kwon, Y.D. Use of traditional Korean medicine by patients with musculoskeletal disorders. PLoS ONE 2013, 8, e63209. [Google Scholar] [CrossRef]
- Kavadar, G.; DemiR, S.E.; AytekiN, E.; Akbal, Y. Use of traditional and complementary medicine for musculoskeletal diseases. Turk. J. Med. Sci. 2019, 49, 809–814. [Google Scholar] [CrossRef] [PubMed]
- Gheihman, G.; Callahan, D.G.; Onyango, J.; Gooding, H.C.; Hirsh, D.A. Coproducing clinical curricula in undergraduate medical education: Student and faculty experiences in longitudinal integrated clerkships. Med. Teach. 2021, 43, 1267–1277. [Google Scholar] [CrossRef]
- Braier-Lorimer, D.A.; Warren-Miell, H. A peer-led mock OSCE improves student confidence for summative OSCE assessments in a traditional medical course. Med. Teach. 2022, 44, 535–540. [Google Scholar] [CrossRef]
- Grover, S.; Pandya, M.; Ranasinghe, C.; Ramji, S.P.; Bola, H.; Raj, S. Assessing the utility of virtual OSCE sessions as an educational tool: A national pilot study. BMC Med. Educ. 2022, 22, 178. [Google Scholar] [CrossRef]
- Cho, E.; Han, Y.-M.; Kang, Y.; Kim, J.-H.; Shin, M.-S.; Oh, M.; Jung, H.-J.; Jeon, H.; Cho, N.G.; Leem, J. Development of objective structured clinical examination checklist and post-education questionnaire for diagnostic musculoskeletal ultrasound training focusing on volar wrist and carpal tunnel syndrome through expert consensus. J. Acupunct. Res. 2022, 39, 105–114. [Google Scholar] [CrossRef]
- Buchberger, W. Radiologic imaging of the carpal tunnel. Eur. Radiol. 1997, 25, 112–117. [Google Scholar] [CrossRef]
- Sarría, L.; Cabada, T.; Cozcolluela, R.; Martínez-Berganza, T.; García, S. Carpal tunnel syndrome: Usefulness of sonography. Eur. Radiol. 2000, 10, 1920–1925. [Google Scholar] [CrossRef]
- Ng, A.W.H.; Griffith, J.F.; Lee, R.K.L.; Tse, W.L.; Wong, C.W.Y.; Ho, P.C. Ultrasound carpal tunnel syndrome: Additional criteria for diagnosis. Clin. Radiol. 2018, 73, 214.e11–214.e18. [Google Scholar] [CrossRef]
- Wong, S.M.; Griffith, J.F.; Hui, A.C.F.; Lo, S.K.; Fu, M.; Wong, K.S. Carpal tunnel syndrome: Diagnostic usefulness of sonography. Radiology 2004, 232, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.H.; Lee, S.; Lee, Y.H. Musculoskeletal Ultrasound; Koonja Publish, Co.: Paju, Korea, 2017. [Google Scholar]
- Korean Orthopedics Ultrasound Society. Orthopaedic Ultrasound; Koonja Publish Co.: Paju, Korea, 2019. [Google Scholar]
- Musculoskeletal Sonography Examination—MSKS/ARDMS. Available online: https://www.ardms.org/get-certified/rmsks/musculoskeletal-sonographer-msks/ (accessed on 31 January 2022).
- George, J.H.; Doto, F.X. A simple five-step method for teaching clinical skills. Fam. Med. 2001, 33, 577–578. [Google Scholar] [PubMed]
- Moore, C.L.; Copel, J.A. Point-of-care ultrasonography. N. Engl. J. Med. 2011, 364, 749–757. [Google Scholar] [CrossRef] [PubMed]
- Hoppmann, R.A.; Rao, V.V.; Poston, M.B.; Howe, D.B.; Hunt, P.S.; Fowler, S.D.; Paulman, L.E.; Wells, J.R.; Richeson, N.A.; Catalana, P.V.; et al. An integrated ultrasound curriculum (IUSC) for medical students: 4-year experience. Crit. Ultrasound J. 2011, 3, 1–12. [Google Scholar] [CrossRef]
- Baltarowich, O.H.; Di Salvo, D.N.; Scoutt, L.M.; Brown, D.L.; Cox, C.W.; DiPietro, M.A.; Glazer, D.I.; Hamper, U.M.; Manning, M.A.; Nazarian, L.N.; et al. National ultrasound curriculum for medical students. Ultrasound Q. 2014, 30, 13–19. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Health Insurance Review & Assessment Service Frequent Disease Statistics. Available online: http://opendata.hira.or.kr/op/opc/olapHifrqSickInfo.do (accessed on 29 March 2022).
- Bianchi, S.; Martinoli, C. Ultrasound of the Musculoskeletal System; Springer Science & Business Media: Berlin, Germany, 2007. [Google Scholar]
- Griswold-Theodorson, S.; Hannan, H.; Handly, N.; Pugh, B.; Fojtik, J.; Saks, M.; Hamilton, R.J.; Wagner, D. Improving patient safety with ultrasonography guidance during internal jugular central venous catheter placement by novice practitioners. Simul. Healthc. 2009, 4, 212–216. [Google Scholar] [CrossRef]
- Osborn, S.R.; Borhart, J.; Antonis, M.S. Medical Students Benefit from the Use of Ultrasound When Learning Peripheral IV Techniques. Crit. Ultrasound J. 2012, 4, 2. [Google Scholar] [CrossRef]
- Favot, M.; Courage, C.; Mantouffel, J.; Amponsah, D. Ultrasound training in the emergency medicine clerkship. West. J. Emerg. Med. 2015, 16, 938–942. [Google Scholar] [CrossRef]
- Hofer, M.; Kamper, L.; Sadlo, M.; Sievers, K.; Heussen, N. Evaluation of an OSCE assessment tool for abdominal ultrasound courses. Ultraschall. Med. 2011, 32, 184–190. [Google Scholar] [CrossRef]
- Patrawalla, P.; Eisen, L.A.; Shiloh, A.; Shah, B.J.; Savenkov, O.; Wise, W.; Evans, L.; Mayo, P.; Szyld, D. Development and validation of an assessment tool for competency in critical care ultrasound. J. Grad. Med. Educ. 2015, 7, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Diep, D.; Chen, K.J.Q.; Kumbhare, D. Ultrasound-guided interventional procedures for myofascial trigger points: A systematic review. Reg. Anesth. Pain Med. 2021, 46, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, S.; Ha, W.-B.; Lee, J.-H.; Jung, H.-J.; Chu, H.-M.; Yang, S.-B.; Choi, S.; Son, M.J.; Kim, J.H.; et al. Development of an ultrasound-imaging procedure and acquisition of ultrasound images of acupuncture points for safety and accuracy of needle insertion. Integr. Med. Res. 2017, 6, 427–433. [Google Scholar] [CrossRef]
- Yoon, S.-H.; Kim, S.-A.; Lee, G.-Y.; Kim, H.; Lee, J.-H.; Leem, J. Using magnetic resonance imaging to measure the depth of acupotomy points in the lumbar spine: A retrospective study. Integr. Med. Res. 2021, 10, 100679. [Google Scholar] [CrossRef] [PubMed]
- Gharries, H. Is ultrasound guided spine injection safe? J. Anest. Crit. Care 2018, 10, 131–138. [Google Scholar]
- Kwon, C.-Y.; Yoon, S.-H.; Lee, B. Clinical effectiveness and safety of acupotomy: An overview of systematic reviews. Complement. Ther. Clin. Pract. 2019, 36, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Duanmu, Y.; Henwood, P.C.; Takhar, S.S.; Chan, W.; Rempell, J.S.; Liteplo, A.S.; Koskenoja, V.; Noble, V.E.; Kimberly, H.H. Correlation of OSCE performance and point-of-care ultrasound scan numbers among a cohort of emergency medicine residents. Ultrasound J. 2019, 11, 3. [Google Scholar] [CrossRef]
| Question (Answers Ranging from 1 (Not at All) to 5 (Entirely) | Total (n = 60) | 3-Week Group (n = 37) | 8-Week Group (n = 23) | p-Value | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | ||
| Were the learning objectives of the ultrasound training appropriate? | 4.52 ± 0.57 | 4.49 ± 0.56 | 5 (4–5) | 4.57 ± 0.59 | 5 (4–5) | 0.530 |
| Were the learning objectives and ultrasound training contents related well? | 4.52 ± 0.57 | 4.49 ± 0.56 | 5 (4–5) | 4.57 ± 0.59 | 5 (4–5) | 0.530 |
| Was it easy to understand the contents of the ultrasound training? | 4.6 ± 0.49 | 4.59 ± 0.50 | 5 (4–5) | 4.61 ± 0.50 | 5 (4–5) | 0.914 |
| Has ultrasound training improved your knowledge about the anatomy and physiology of carpal tunnels? | 4.75 ± 0.44 | 4.68 ± 0.47 | 5 (4–5) | 4.87 ± 0.34 | 5 (5–5) | 0.094 |
| Did the ultrasound practice help you develop ultrasound skills? | 4.5 ± 0.62 | 4.43 ± 0.60 | 4 (4–5) | 4.61 ± 0.66 | 5 (4–5) | 0.182 |
| Did the ultrasound OSCE help motivate independent practical training? | 4.45 ± 0.53 | 4.41 ± 0.55 | 4 (4–5) | 4.52 ± 0.51 | 5 (4–5) | 0.448 |
| Was the ultrasound OSCE difficult? | 2.98 ± 1.11 | 2.92 ± 1.06 | 3 (2–4) | 3.09 ± 1.20 | 3 (2–4) | 0.569 |
| Was the ultrasound OSCE time limit (5 min) enough for you? | 3.27 ± 1.22 | 2.97 ± 1.30 | 3 (2–4) | 3.74 ± 0.92 | 4 (3–4) | 0.019 * |
| Are you generally satisfied with this ultrasound training? | 4.5 ± 0.60 | 4.41 ± 0.60 | 4 (4–5) | 4.65 ± 0.57 | 5 (4–5) | 0.091 |
| Do you have any intentions of studying ultrasound more in the future? | 4.57 ± 0.56 | 4.57 ± 0.60 | 5 (4–5) | 4.57 ± 0.51 | 5 (4–5) | 0.804 |
| Are you willing to use ultrasound in clinical practice after graduation? | 4.10 ± 0.71 | 4.08 ± 0.76 | 4 (4–5) | 4.13 ± 0.63 | 4 (4–5) | 0.912 |
| Has your opinion about ultrasound usage changed positively through this education? | 4.33 ± 0.60 | 4.30 ± 0.66 | 4 (4–5) | 4.39 ± 0.50 | 4 (4–5) | 0.706 |
| Items of Self-Assessment (Answers Ranging from 1 = Strongly Disagree to 5 = Completely Agree) | Total (n = 60) | 3-Week Group (n = 37) | 8-Week Group (n = 23) | p-Value | ||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | ||
| I actively participated in ultrasound training. | 4.40 ± 0.74 | 4.27 ± 0.80 | 4 (4–5) | 4.61 ± 0.58 | 5 (4–5) | 0.089 |
| I was considerate of the subject during the ultrasound examination. | 4.35 ± 0.66 | 4.30 ± 0.70 | 4 (4–5) | 4.43 ± 0.59 | 4 (4–5) | 0.511 |
| I communicated appropriately with the subject during the ultrasound examination. | 4.45 ± 0.59 | 4.38 ± 0.64 | 4 (4–5) | 4.57 ± 0.51 | 5 (4–5) | 0.303 |
| I can use basic functions of ultrasound such as ultrasonic probe selection, depth and focus control, and freeze. | 4.52 ± 0.70 | 4.41 ± 0.80 | 5 (4–5) | 4.70 ± 0.47 | 5 (4–5) | 0.203 |
| I can identify the anterior structure of the wrist through ultrasound. | 4.35 ± 0.71 | 4.24 ± 0.80 | 4 (4–5) | 4.52 ± 0.51 | 5 (4–5) | 0.232 |
| I can do ultrasound scans according to the criteria for diagnosing carpal tunnel syndrome. | 4.40 ± 0.67 | 4.30 ± 0.74 | 4 (4–5) | 4.57 ± 0.51 | 5 (4–5) | 0.192 |
| Task | Score | Sub-Score | Mean ± SD |
|---|---|---|---|
| 1. Self-introduction | 1 | 0.99 ± 0.10 | |
| 2. Patient identification | 1 | 0.96 ± 0.19 | |
| 3. Explaining the ultrasound examination to the patient | 1 | 0.98 ± 0.13 | |
| 4. Hand hygiene before the examination | 2 | 1.46 ± 0.59 | |
| 5. Patient guidance | 2 | 1.86 ± 0.34 | |
| 6. Selecting the appropriate probe and setting the device | 3 | 1.43 ± 1.28 | |
| 6–1. Probe setting | 1 | 0.57 ± 0.50 | |
| 6–2. Selecting the area to be scanned | 1 | 0.57 ± 0.50 | |
| 6–3. Adjusting the depth to scan | 1 | 0.28 ± 0.45 | |
| 7. Applying the gel | 1 | 1.00 ± 0.00 | |
| 8. Probe tuning | 1 | 0.91 ± 0.29 | |
| 9. Probe handling | 1 | 0.83 ± 0.38 | |
| 10. Correct view of the (1) scaphoid, (2) pisiform, (3) median nerve, (4) ulnar artery, (5) flexor retinaculum, (6) flexor pollicis longus, (7) ulnar nerve, (8) flexor digitorum superficialis, flexor digitorum profundus, (9) flexor carpi radialis, (10) flexor carpi ulnaris | 3 | 2.33 ± 0.74 | |
| 10–1. 9–10 structures | 3 | ||
| 10–2. 4–8 structures | 2 | ||
| 10–3. 1–3 structures | 1 | ||
| 10–4. 0 structure | 0 | ||
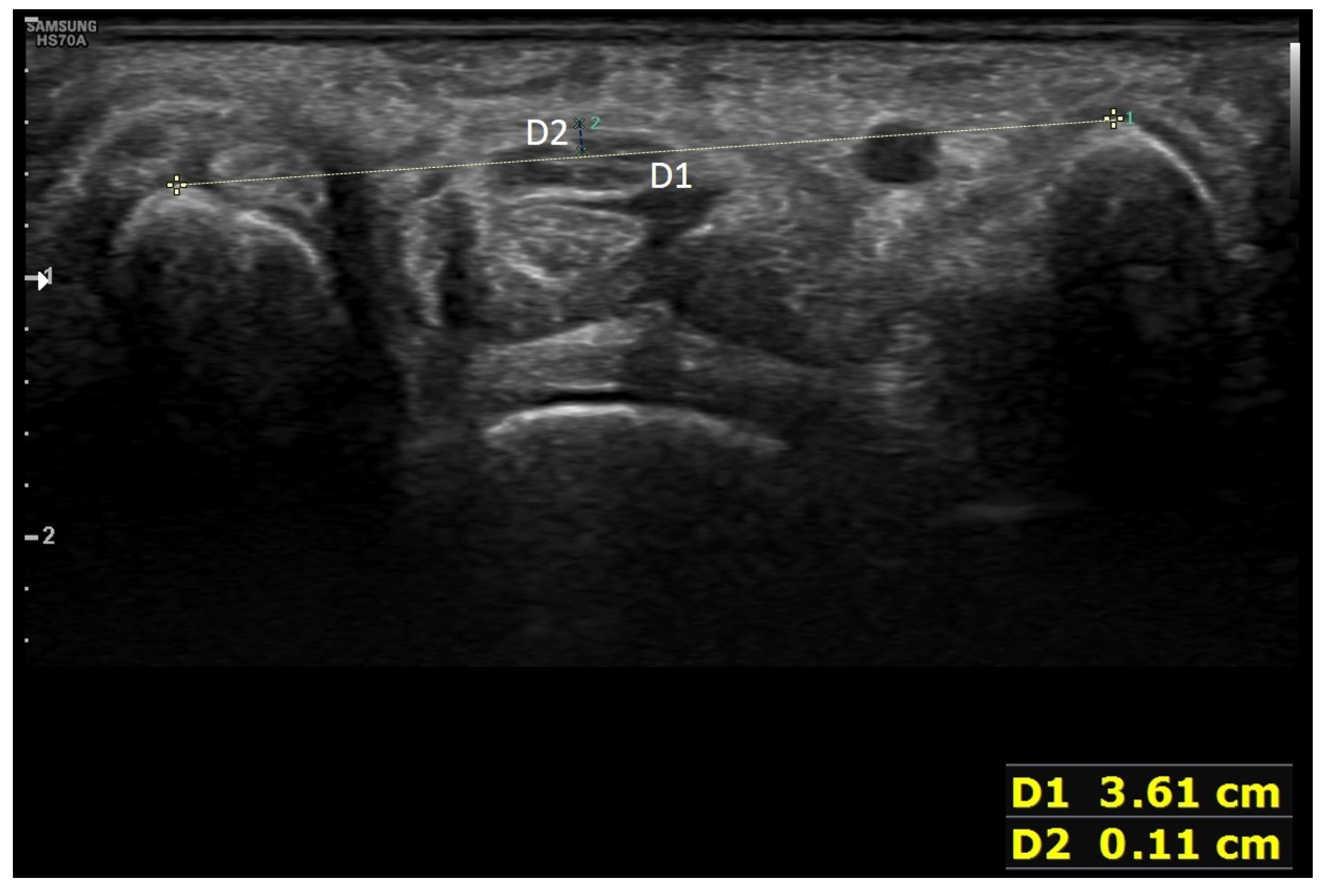
| 11. Correct measurement according to diagnostic criteria of carpal tunnel syndrome and explaining the results | 3 | 2.21 ± 0.97 | |
| 11–1. Connecting the top of the scaphoid and the pisiform with a line | 1 | 0.76 ± 0.43 | |
| 11–2. Measuring the vertical distance between the line connecting the top of the scaphoid and the pisiform and the flexor retinaculum | 1 | 0.64 ± 0.48 | |
| 11–3. Explaining the examination results | 1 | 0.81 ± 0.39 | |
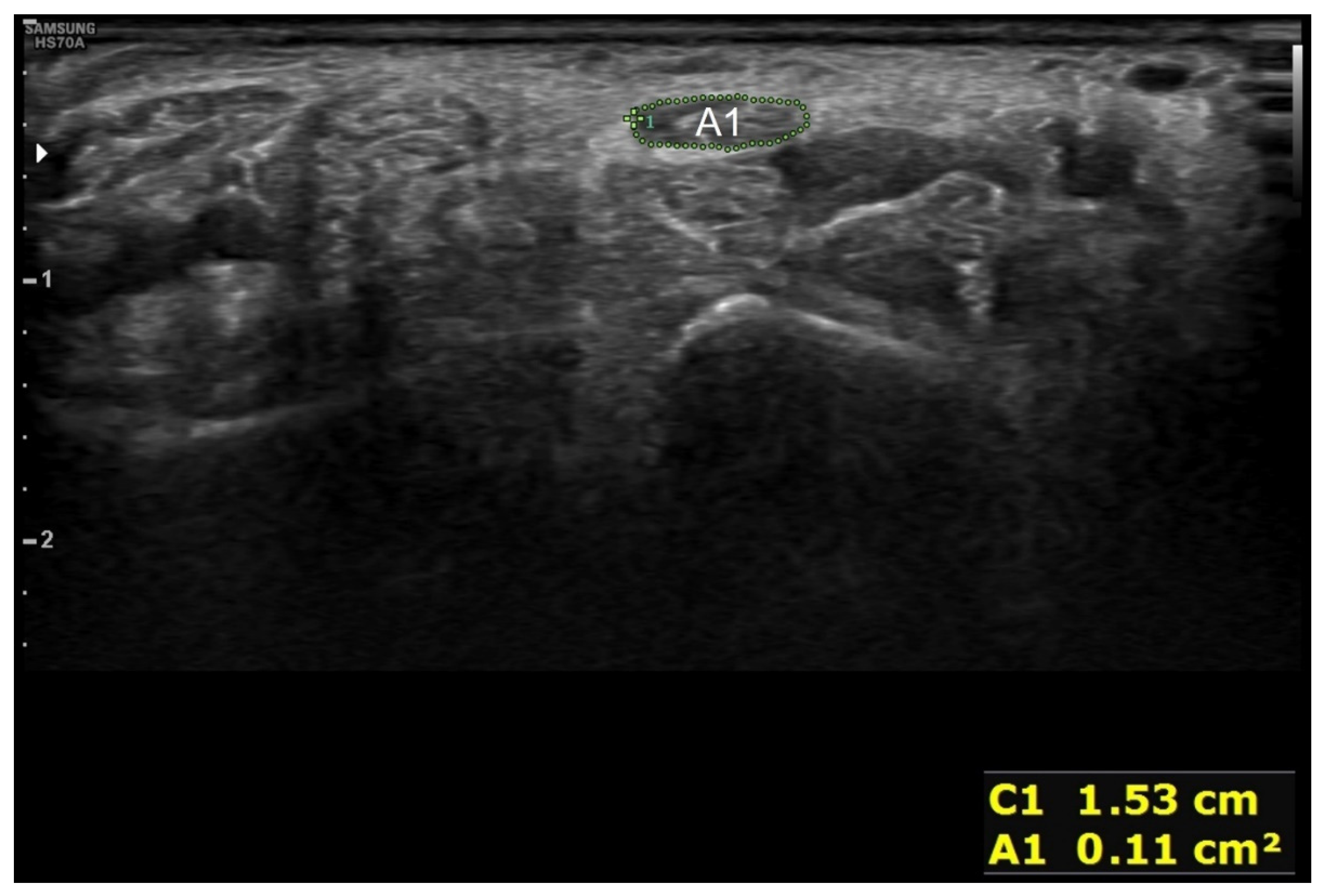
| 12. Correct measurement of the cross-sectional area of the median nerve and explaining the examination results | 3 | 1.65 ± 1.19 | |
| 12–1. Correct measurement of the cross-sectional area of the median nerve proximal to the flexor retinaculum | 2 | 1.07 ± 0.83 | |
| 12–2. Explaining the examination results | 1 | 0.58 ± 0.50 | |
| 13. Hand hygiene after the examination? | 2 | 0.30 ± 0.66 | |
| 14. Informing the patient about the examination’s completion and explaining the final findings after the examination | 2 | 1.05 ± 0.96 | |
| 15. Cleaning up the used devices and wiping off the gel | 2 | 1.04 ± 0.95 | |
| Total score | 28 | 19 ± 5.35 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cho, E.; Han, Y.-M.; Kang, Y.; Kim, J.-H.; Shin, M.-S.; Oh, M.; Cho, N.-G.; Jung, H.-J.; Leem, J. Implementation of Objective Structured Clinical Examination on Diagnostic Musculoskeletal Ultrasonography Training in Undergraduate Traditional Korean Medicine Education: An Action Research. Diagnostics 2022, 12, 1707. https://doi.org/10.3390/diagnostics12071707
Cho E, Han Y-M, Kang Y, Kim J-H, Shin M-S, Oh M, Cho N-G, Jung H-J, Leem J. Implementation of Objective Structured Clinical Examination on Diagnostic Musculoskeletal Ultrasonography Training in Undergraduate Traditional Korean Medicine Education: An Action Research. Diagnostics. 2022; 12(7):1707. https://doi.org/10.3390/diagnostics12071707
Chicago/Turabian StyleCho, Eunbyul, Young-Min Han, Yeonseok Kang, Jae-Hyo Kim, Min-Seop Shin, Myungjin Oh, Nam-Geun Cho, Hyun-Jong Jung, and Jungtae Leem. 2022. "Implementation of Objective Structured Clinical Examination on Diagnostic Musculoskeletal Ultrasonography Training in Undergraduate Traditional Korean Medicine Education: An Action Research" Diagnostics 12, no. 7: 1707. https://doi.org/10.3390/diagnostics12071707
APA StyleCho, E., Han, Y.-M., Kang, Y., Kim, J.-H., Shin, M.-S., Oh, M., Cho, N.-G., Jung, H.-J., & Leem, J. (2022). Implementation of Objective Structured Clinical Examination on Diagnostic Musculoskeletal Ultrasonography Training in Undergraduate Traditional Korean Medicine Education: An Action Research. Diagnostics, 12(7), 1707. https://doi.org/10.3390/diagnostics12071707






