A Race against the Clock: A Case Report and Literature Review Concerning the Importance of ADAMTS13 Testing in Diagnosis and Management of Thrombotic Thrombocytopenic Purpura during Pregnancy
Abstract
1. Introduction
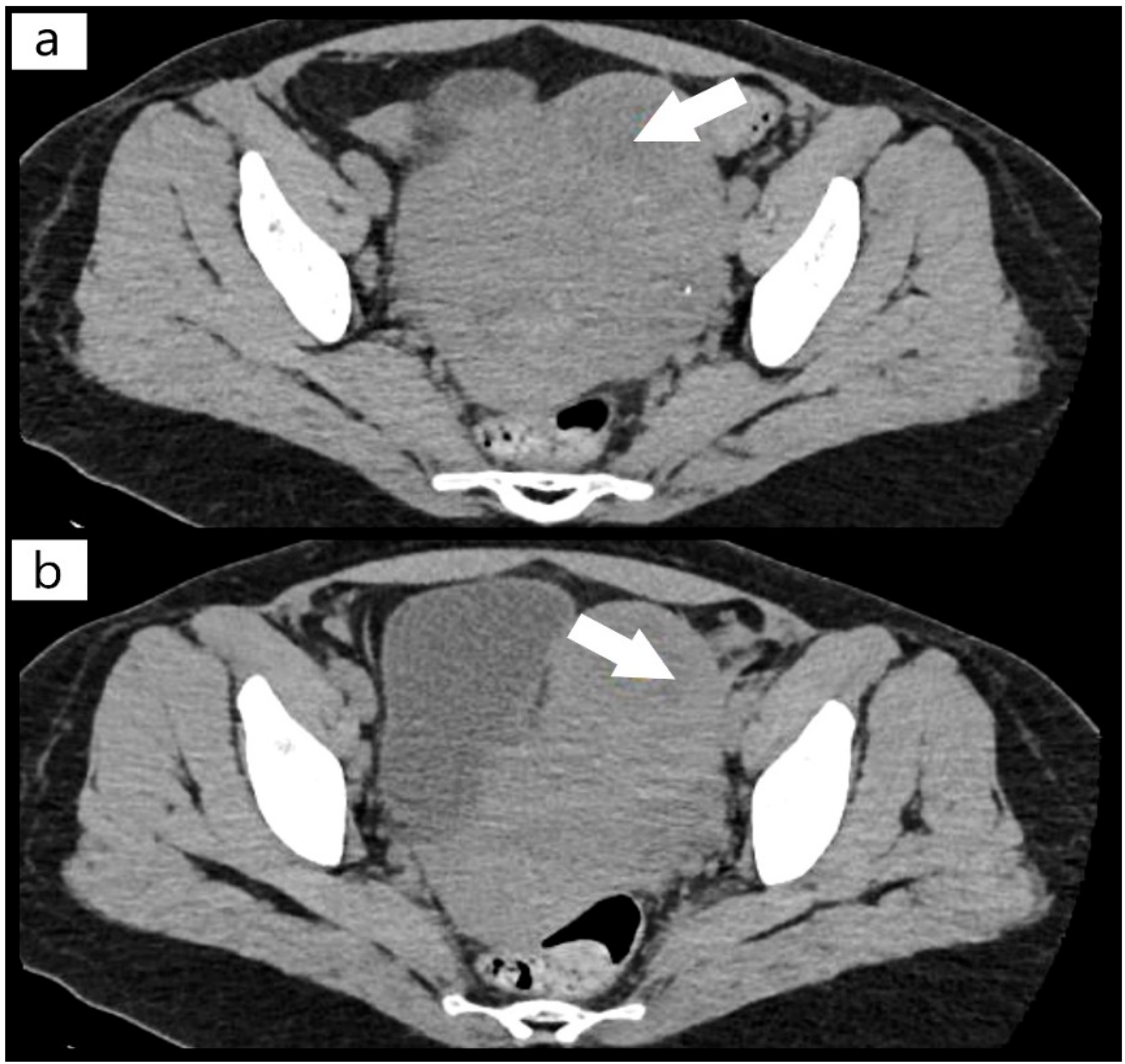
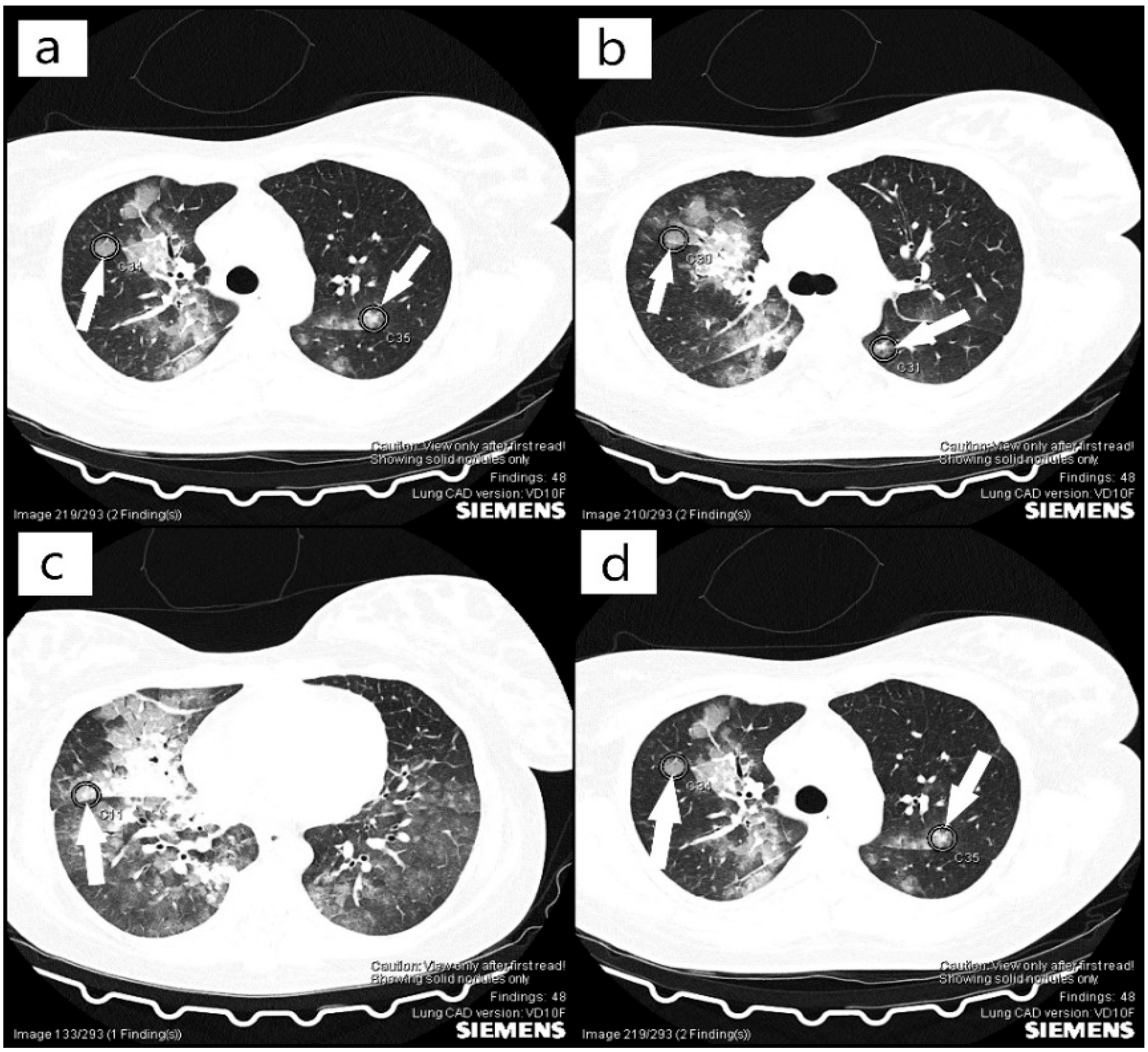
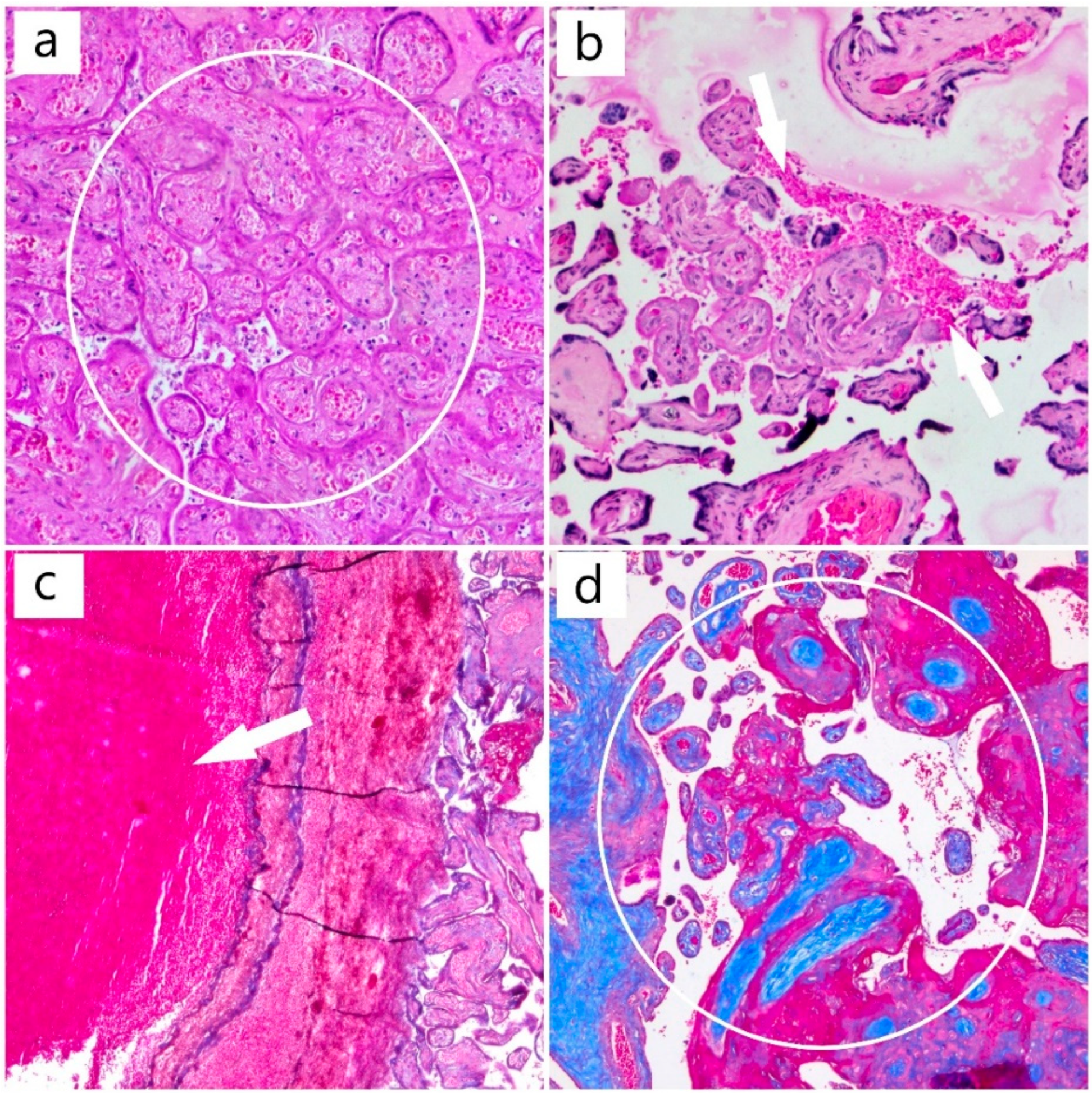
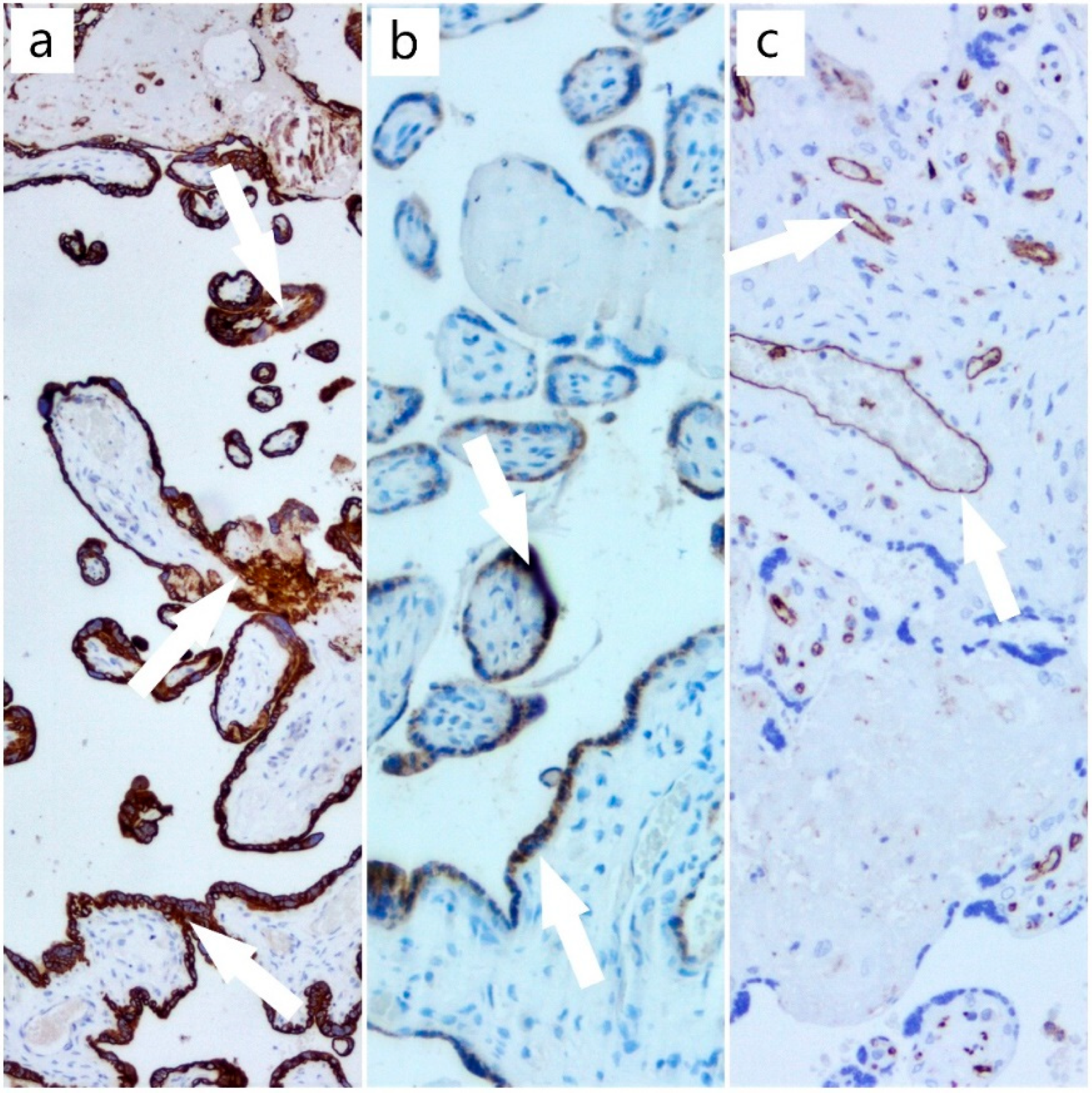
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Sakai, K.; Fujimura, Y.; Nagata, Y.; Higasa, S.; Moriyama, M.; Isonishi, A.; Konno, M.; Kajiwara, M.; Ogawa, Y.; Kaburagi, S.; et al. Success and limitations of plasma treatment in pregnant women with congenital thrombotic thrombocytopenic purpura. J. Thromb. Haemost. 2020, 18, 2929–2941. [Google Scholar] [CrossRef] [PubMed]
- Al-Husban, N.; Al-Kuran, O. Post-Partum Thrombotic Thrombocytopenic Purpura (TTP) in a Patient with known Idiopathic (Immune) Thrombocytopenic Purpura: A case report and review of the literature. J. Med. Case Rep. 2018, 12, 147. [Google Scholar] [CrossRef]
- Romão de Souza, V.; Beatriz Cavalcante de Oliveira, A.; Maria Vanderlei, A.; Queiroz da Mota Silveira Aroucha, A.; Pontes Duarte, B.; Nunes Machado, A.; Netto Chaer, L.; Wanderley de Barros Correia, C.; da Conceição de Barros Correia, M.; Freire Hazin Costa, M. Inherited thrombotic thrombocytopenic purpura mimicking immune thrombocytopenic purpura during pregnancy: A case report. J. Med. Case Rep. 2018, 12, 15. [Google Scholar] [CrossRef] [PubMed]
- Roose, E.; Tersteeg, C.; Demeersseman, R.; Schelpe, A.S.; Deforche, L.; Pareyn, I.; Vandenbulcke, A.; Vandeputte, N.; Dierickx, D.; Voorberg, J.; et al. Anti-ADAMTS13 Antibodies and a Novel Heterozygous p.R1177Q Mutation in a Case of Pregnancy-Onset Immune-Mediated Thrombotic Thrombocytopenic Purpura. TH Open 2018, 2, e8–e15. [Google Scholar] [CrossRef] [PubMed]
- Nonaka, T.; Yamaguchi, M.; Nishijima, K.; Moriyama, M.; Takakuwa, K.; Enomoto, T. A successfully treated case of an acute presentation of congenital thrombotic thrombocytopenic purpura (Upshaw-Schulman syndrome) with decreased ADAMTS13 during late stage of pregnancy. J. Obstet. Gynaecol. Res. 2021, 47, 1892–1897. [Google Scholar] [CrossRef]
- Perez Botero, J.; Reese, J.A.; George, J.N.; McIntosh, J.J. Severe thrombocytopenia and microangiopathic hemolytic anemia in pregnancy: A guide for the consulting hematologist. Am. J. Hematol. 2021, 96, 1655–1665. [Google Scholar] [CrossRef]
- Scully, M. Thrombotic Thrombocytopenic Purpura and Atypical Hemolytic Uremic Syndrome Microangiopathy in Pregnancy. Semin. Thromb. Hemost. 2016, 42, 774–779. [Google Scholar] [CrossRef]
- Ramadan, M.K.; Badr, D.A.; Hubeish, M.; Itani, S.; Hijazi, H.; Mogharbil, A. HELLP Syndrome, Thrombotic Thrombocytopenic Purpura or Both: Appraising the Complex Association and Proposing a Stepwise Practical Plan for Differential Diagnosis. J. Hematol. 2018, 7, 32–37. [Google Scholar] [CrossRef]
- Marins, L.R.; da Rocha Oppermann, M.L. Thrombotic thrombocytopenic purpura and acquired immunodeficiency syndrome diagnosed in pregnancy: Case report. J. Obstet. Gynaecol. Res. 2021, 47, 1898–1902. [Google Scholar] [CrossRef]
- Umemura, A.; Sasaki, A.; Nitta, H.; Obuchi, T.; Baba, S.; Wakabayashi, G. Laparoscopic splenectomy for the treatment of refractory thrombotic thrombocytopenic purpura. Clin. J. Gastroenterol. 2013, 6, 420–423. [Google Scholar] [CrossRef]
- Ferrari, B.; Maino, A.; Lotta, L.A.; Artoni, A.; Pontiggia, S.; Trisolini, S.M.; Malato, A.; Rosendaal, F.R.; Peyvandi, F. Pregnancy complications in acquired thrombotic thrombocytopenic purpura: A case-control study. Orphanet J. Rare Dis. 2014, 9, 193. [Google Scholar] [CrossRef]
- Zhao, C.; Qu, Y.; Sui, R.; Feng, J.; Gao, J.; Ma, J.; Jiang, R.; Li, H. Delayed visual recovery in pregnancy-associated thrombotic thrombocytopenic purpura with bilateral serous retinal detachment. Doc. Ophthalmol. 2013, 126, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Mariotte, E.; Azoulay, E.; Galicier, L.; Rondeau, E.; Zouiti, F.; Boisseau, P.; Poullin, P.; de Maistre, E.; Provôt, F.; Delmas, Y.; et al. Epidemiology and pathophysiology of adulthood-onset thrombotic microangiopathy with severe ADAMTS13 deficiency (thrombotic thrombocytopenic purpura): A cross-sectional analysis of the French national registry for thrombotic microangiopathy. Lancet Haematol 2016, 3, e237–e245. [Google Scholar] [CrossRef]
- Ferrari, B.; Peyvandi, F. How I treat thrombotic thrombocytopenic purpura in pregnancy. Blood 2020, 136, 2125–2132. [Google Scholar] [CrossRef] [PubMed]
- Lucania, G.; Camiolo, E.; Carmina, M.G.; Fiandaca, T.; Indovina, A.; Malato, A.; Messina, R.; Fabbiano, F.; Marcenò, R. Multidisciplinary approach in pregnancy-associated thrombotic thrombocytopenic purpura: A case report. Blood Transfus. 2014, 12 (Suppl. 1), s137–s140. [Google Scholar] [CrossRef] [PubMed]
- Kaneda, Y.; Kitagawa, J.; Yamaguchi, K.; Matsumoto, T.; Nakamura, N.; Nakamura, H.; Ninomiya, S.; Kanemura, N.; Kasahara, S.; Hara, T.; et al. Thrombotic thrombocytopenic purpura during pregnancy refractory to plasma exchange and rituximab. Rinsho Ketsueki 2019, 60, 209–212. [Google Scholar] [CrossRef]
- González-Mesa, E.; Narbona, I.; Blasco, M.; Cohen, I. Unfavorable course in pregnancy-associated thrombotic thrombocytopenic purpura necessitating a perimortem Cesarean section: A case report. J. Med. Case Rep. 2013, 7, 119. [Google Scholar] [CrossRef]
- Sukumar, S.; Lämmle, B.; Cataland, S.R. Thrombotic Thrombocytopenic Purpura: Pathophysiology, Diagnosis, and Management. J. Clin. Med. 2021, 10, 536. [Google Scholar] [CrossRef]
- Von Krogh, A.S.; Kremer Hovinga, J.A.; Tjønnfjord, G.E.; Ringen, I.M.; Lämmle, B.; Waage, A.; Quist-Paulsen, P. The impact of congenital thrombotic thrombocytopenic purpura on pregnancy complications. Thromb. Haemost. 2014, 111, 1180–1183. [Google Scholar] [CrossRef]
- Maayan, H.; Kirgner, I.; Gutwein, O.; Herzog-Tzarfati, K.; Rahimi-Levene, N.; Koren-Michowitz, M.; Blickstein, D. Acquired thrombotic thrombocytopenic purpura: A rare disease associated with BNT162b2 vaccine. J. Thromb. Haemost. 2021, 19, 2314–2317. [Google Scholar] [CrossRef]
- Aminimoghaddam, S.; Afrooz, N.; Nasiri, S.; Motaghi Nejad, O.; Mahmoudzadeh, F. A COVID-19 pregnant patient with thrombotic thrombocytopenic purpura: A case report. J. Med. Case Rep. 2021, 15, 104. [Google Scholar] [CrossRef] [PubMed]
- Nikolaou, M.; Karakantza, M.; Adonakis, G.; Theodorou, G.; Zoumbos, N.; Decavalas, G. A case of severe ADAMTS13 deficiency presenting as thrombotic thrombocytopenic purpura in pregnancy. Med. Pregl. 2012, 65, 436–439. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Williams, L.A.; Marques, M.B. Pathology Consultation on the Diagnosis and Treatment of Thrombotic Microangiopathies (TMAs). Am. J. Clin. Pathol. 2016, 145, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Moatti-Cohen, M.; Garrec, C.; Wolf, M.; Boisseau, P.; Galicier, L.; Azoulay, E.; Stepanian, A.; Delmas, Y.; Rondeau, E.; Bezieau, S.; et al. Unexpected frequency of Upshaw-Schulman syndrome in pregnancy-onset thrombotic thrombocytopenic purpura. Blood 2012, 119, 5888–5897. [Google Scholar] [CrossRef]
- Xu, J.; Yu, S.; Zhang, F. Frequent recurrence of pregnancy-triggered congenital thrombotic thrombocytopenic purpura: A rare case report. Clin. Hemorheol. Microcirc. 2021, 77, 195–200. [Google Scholar] [CrossRef]
- Fakhouri, F.; Scully, M.; Provôt, F.; Blasco, M.; Coppo, P.; Noris, M.; Paizis, K.; Kavanagh, D.; Pène, F.; Quezada, S.; et al. Management of thrombotic microangiopathy in pregnancy and postpartum: Report from an international working group. Blood 2020, 136, 2103–2117. [Google Scholar] [CrossRef]
- George, J.N. The remarkable diversity of thrombotic thrombocytopenic purpura: A perspective. Blood Adv. 2018, 2, 1510–1516. [Google Scholar] [CrossRef]
- Cines, D.B.; Levine, L.D. Thrombocytopenia in pregnancy. Blood 2017, 130, 2271–2277. [Google Scholar] [CrossRef]
- Gasparri, M.L.; Bellati, F.; Brunelli, R.; Perrone, G.; Pecorini, F.; Papadia, A.; Meloni, G.; Trisolini, S.M.; Gozzer, M.; Domenici, L.; et al. Thrombotic thrombocytopenic purpura during pregnancy versus imitator of preeclampsia. Transfusion 2015, 55, 2516–2518. [Google Scholar] [CrossRef]
- Zheng, X.L.; Vesely, S.K.; Cataland, S.R.; Coppo, P.; Geldziler, B.; Iorio, A.; Matsumoto, M.; Mustafa, R.A.; Pai, M.; Rock, G.; et al. ISTH guidelines for treatment of thrombotic thrombocytopenic purpura. J. Thromb. Haemost. 2020, 18, 2496–2502. [Google Scholar] [CrossRef]
- Miesbach, W.; Menne, J.; Bommer, M.; Schönermarck, U.; Feldkamp, T.; Nitschke, M.; Westhoff, T.H.; Seibert, F.S.; Woitas, R.; Sousa, R.; et al. Incidence of acquired thrombotic thrombocytopenic purpura in Germany: A hospital level study. Orphanet J. Rare Dis. 2019, 14, 260. [Google Scholar] [CrossRef] [PubMed]
| Differential Diagnosis | ||
|---|---|---|
| Diagnostic | Characteristics | |
| TTP |
| |
| DIC |
| |
| Disseminated Lupus Erythematosus (Vasculitis from Antiphospholipid syndrome) |
| |
| HELLP Syndrome and Preeclampsia |
| |
| not more than in PTT | ||
| Hemolytic Uremic Syndrome |
| |
| Viral Infection Acute Sepsis COVID-19, Vaccination with Pfizer BioNTech (BNT2b2) |
| |
| Acute Fatty Liver |
| |
| Time of Admission | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 19 April 2021 | 20 April 2021 | 21 April 2021 | 22 April 2021 | ||||||
| Tests | Result 1 | Result 2 | Result 1 | Result 2 | Result 1 | Result 2 | Result 1 | Result 2 | Normal Value |
| Leukocytes (WBC) | 14.7 × 109/L | 16.2 × 109/L | 14.2 × 109/L | - | 14.8 × 109/L | 17.4 × 109/L | 15.8 × 109/L | - | 4.00–10.00 × 109/L |
| Hemoglobin (HGB) | 5.3 g/dL | 5.5 g/dL | 6.9 g/dL | - | 6.1 g/dL | 8.0 g/dL | 7.7 g/dL | - | 11.5–16 g/dL |
| Hematocrit (HCT) | 17.2% | 17.4% | 23% | - | 20.7% | 26.5% | 25.5 | - | 35–48% |
| Platelets (PLT) | 13 × 109/L | 11 × 109/L | 18 × 109/L | - | 22 × 109/L | 32 × 109/L | 26 × 109/L | 150–450 × 109/L | |
| INR (International Normalized Ratio) | 1.05 | - | 1.09 | - | 1.1 | - | 1.04 | - | 0.8–1.2 |
| APTT | 29.1 | - | 25.1 | - | 25.5 | - | 26.5 | 25–38 s | |
| Fibrinogen | 410 mg/dL | - | 453 mg/dL | - | 387 mg/dL | - | 415 mg/dL | - | 180–450 mg/dL |
| Creatinine | 1.36 mg/dL | 1.38 mg/dL | 1.54 mg/dL | - | 1.48 mg/dL | 1.62 mg/dL | 1.56 mg/dL | - | 0.50–0.90 mg/dL |
| Urea | 53 mg/dL | 50.47 mg/dL | 51.03 mg/dL | - | 60.06 mg/dL | 58.86 mg/dL | 69.96 mg/dL | - | 16–43 mg/dL |
| Uric Acid | 6.94 mg/dL | 6.97 mg/dL | - | - | - | - | - | - | 2.3–6.10 mg/dL |
| Total Bilirubin | - | - | 1.30 mg/dL | - | 1.66 mg/dL | - | 1.39 mg/dL | - | 0.30–1.10 mg/dL |
| Direct Bilirubin | - | - | 0.37 mg/dL | - | 0.31 mg/dL | - | 0.49 mg/dL | - | 0.10–0.40 mg/dL |
| C Reactive Protein (CRP) | 75.5 mg/L | 79.04 mg/L | 85.47 mg/L | - | 84.5 mg/L | - | 0.00–5.00 mg/L | ||
| Lactate dehydrogenase (LDH) | - | - | - | - | 1374 U/L | 1582 U/L | 1764 U/L | - | 0.00–247.00 U/L |
| Total Protein | - | - | 5.6 g/dL | - | 5.26 g/dL | 5.71 g/dL | 5.84 g/dL | - | 6.60–8.30 g/dL |
| Peripheral Blood Smear | Frequent target erythrocytes and schizocytes, aspect that is consistent | ||||||||
| Reticulocytes | Reticulocytes 66 per 1000 red blood cells are found (normal is 5–15 per 1000 red blood cells) | ||||||||
| Troponin I | 7.11 ng/mL | <0.5 ng/mL | |||||||
| D-dimers | >3000 ng/mL | <100 ng/mL | |||||||
| COVID19 (PCR) | Negative | ||||||||
| Cultures | All cultures were negative | ||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitranovici, M.I.; Pușcașiu, L.; Oală, I.E.; Petre, I.; Craina, M.L.; Mager, A.R.; Vasile, K.; Chiorean, D.M.; Sabău, A.-H.; Turdean, S.G.; et al. A Race against the Clock: A Case Report and Literature Review Concerning the Importance of ADAMTS13 Testing in Diagnosis and Management of Thrombotic Thrombocytopenic Purpura during Pregnancy. Diagnostics 2022, 12, 1559. https://doi.org/10.3390/diagnostics12071559
Mitranovici MI, Pușcașiu L, Oală IE, Petre I, Craina ML, Mager AR, Vasile K, Chiorean DM, Sabău A-H, Turdean SG, et al. A Race against the Clock: A Case Report and Literature Review Concerning the Importance of ADAMTS13 Testing in Diagnosis and Management of Thrombotic Thrombocytopenic Purpura during Pregnancy. Diagnostics. 2022; 12(7):1559. https://doi.org/10.3390/diagnostics12071559
Chicago/Turabian StyleMitranovici, Melinda Ildiko, Lucian Pușcașiu, Ioan Emilian Oală, Izabella Petre, Marius Lucian Craina, Antonia Rebeka Mager, Kinga Vasile, Diana Maria Chiorean, Adrian-Horațiu Sabău, Sabin Gligore Turdean, and et al. 2022. "A Race against the Clock: A Case Report and Literature Review Concerning the Importance of ADAMTS13 Testing in Diagnosis and Management of Thrombotic Thrombocytopenic Purpura during Pregnancy" Diagnostics 12, no. 7: 1559. https://doi.org/10.3390/diagnostics12071559
APA StyleMitranovici, M. I., Pușcașiu, L., Oală, I. E., Petre, I., Craina, M. L., Mager, A. R., Vasile, K., Chiorean, D. M., Sabău, A.-H., Turdean, S. G., & Cotoi, O. S. (2022). A Race against the Clock: A Case Report and Literature Review Concerning the Importance of ADAMTS13 Testing in Diagnosis and Management of Thrombotic Thrombocytopenic Purpura during Pregnancy. Diagnostics, 12(7), 1559. https://doi.org/10.3390/diagnostics12071559









