Indeterminacy of the Diagnosis of Sudden Infant Death Syndrome Leading to Problems with the Validity of Data
Abstract
1. Introduction
2. Literature Review
- (SIDS) AND (wrong diagnos *)—2 texts, both irrelevant;
- (SIDS) AND (fals * diagnos *)—6 texts, one relevant [27];
- A vulnerable stage of CNS and immune system development (vulnerable period);
- Predisposing factors include genetic factors (vulnerable individual);
- Trigger events, e.g., the child’s sleeping position, a smoking mother, or infection (vulnerable environment).
- -
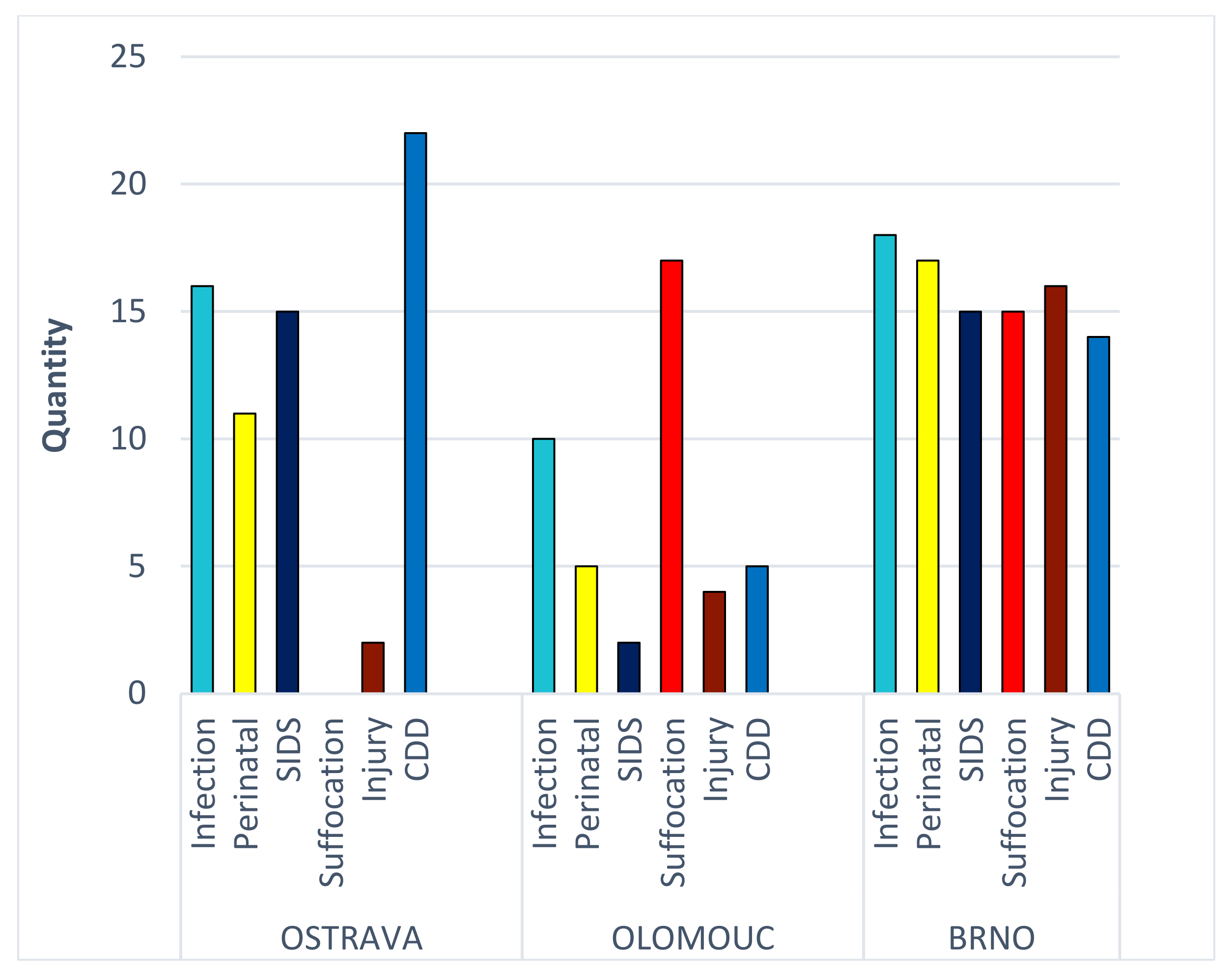
- What specific differences exist between departments regarding the diagnosed causes of death?
- -
- What specific differences exist between departments regarding how information is collected on social risk factors?
- -
- What specific differences exist between departments regarding the identification of social factors?
3. Materials and Methods
3.1. Sample
- Medical autopsies aimed at determining the cause of death and clarifying all the circumstances of people who died as a result of a sudden, unexpected, or violent death;
- Forensic autopsies are performed when it is suspected that the death caused by a criminal offense was stated.
3.2. Measures
- Childbirth-related deaths (P00–P96—certain conditions originating in the perinatal period);
- Injuries (burns, injuries, accidents, traffic accidents, i.e., mainly V01–Y98—external causes of morbidity and mortality and S00–T98—injury, poisoning, and other inevitable consequences of external causes, willful harm);
- Suffocation (W00–X59—other external causes of accidental injury and T17—foreign body in the respiratory tract (most often, cases of aspiration of milk/vomit or death due to mechanical pressure on the rib cage or covering of the nose and mouth. Five out of seventeen such cases were closed as R96–R99—ill-defined and unknown causes of mortality, with a non-specific autopsy finding suggesting an indication of some form of suffocation));
- Congenital malformations (Q00–Q99—congenital malformations, deformities, and chromosomal abnormalities. Most frequently, these were heart and digestive system disorders);
- Infections (most commonly J00–J99—respiratory and N00–N99—genitourinary diseases);
- SIDS R95.
3.3. Statistical Analyses
4. Results
- Hostile behavior of mothers (guest)—included cases not only of proven homicides but also cases of proven violent behavior with the child victim, leading to medical complications of the child leading to his death.
- Socio-economic factors (soc)—included aspects related to the socio-economic background of the child’s family, e.g., inadequate housing conditions and low level of hygiene in the household.
- Factors related to health (health)—included aspects related to health, such as poor hygiene of the child’s body, signs of poor nutrition, untreated inflammation, congenital developmental defects, etc.
- Relevant documentation (absent)—the absence of documents on the file containing information on the above, whether police reports, medical records, or social services information.
5. Discussion
5.1. Strengths and Limitations
5.2. Implication
6. Conclusions
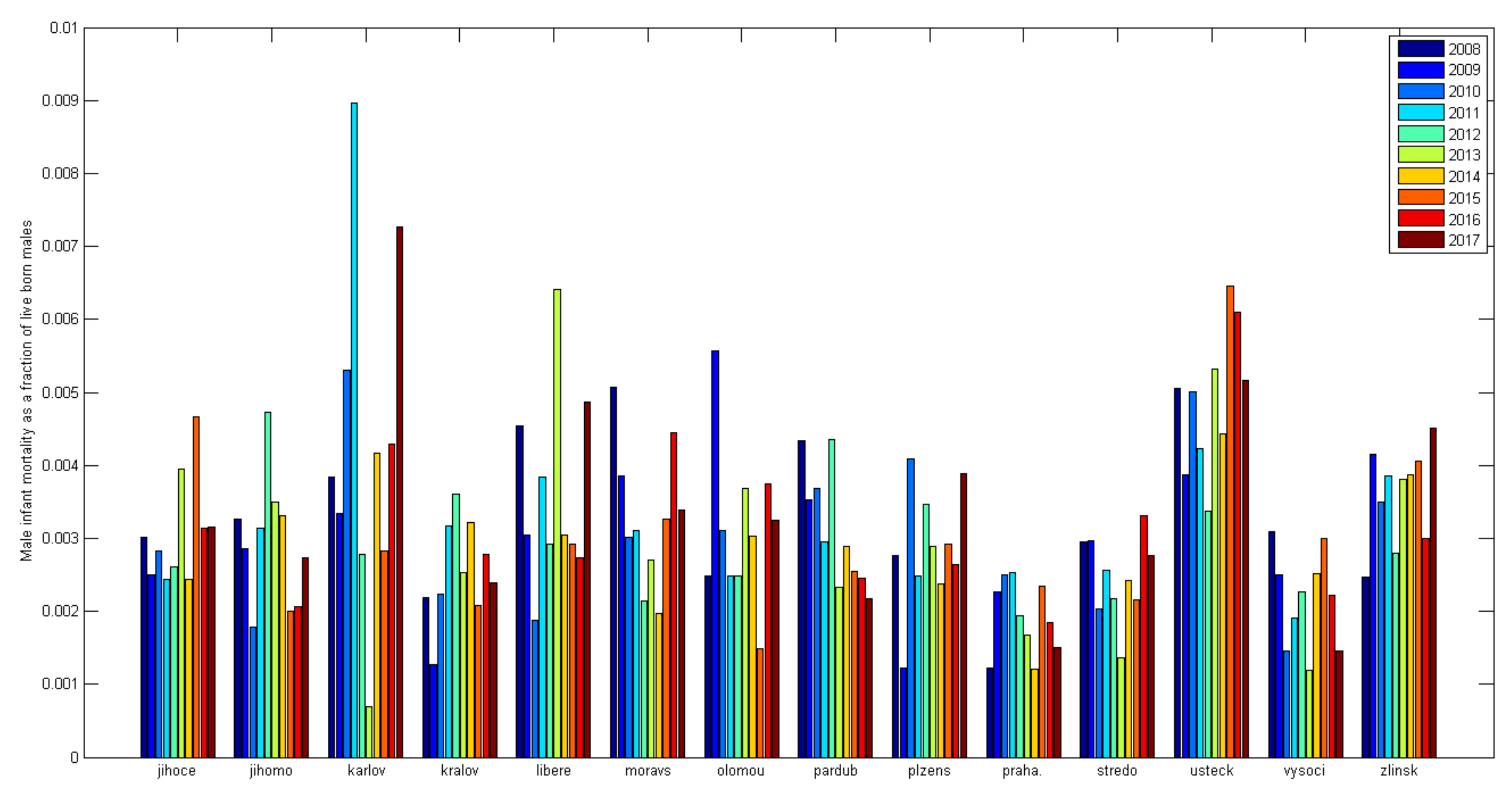
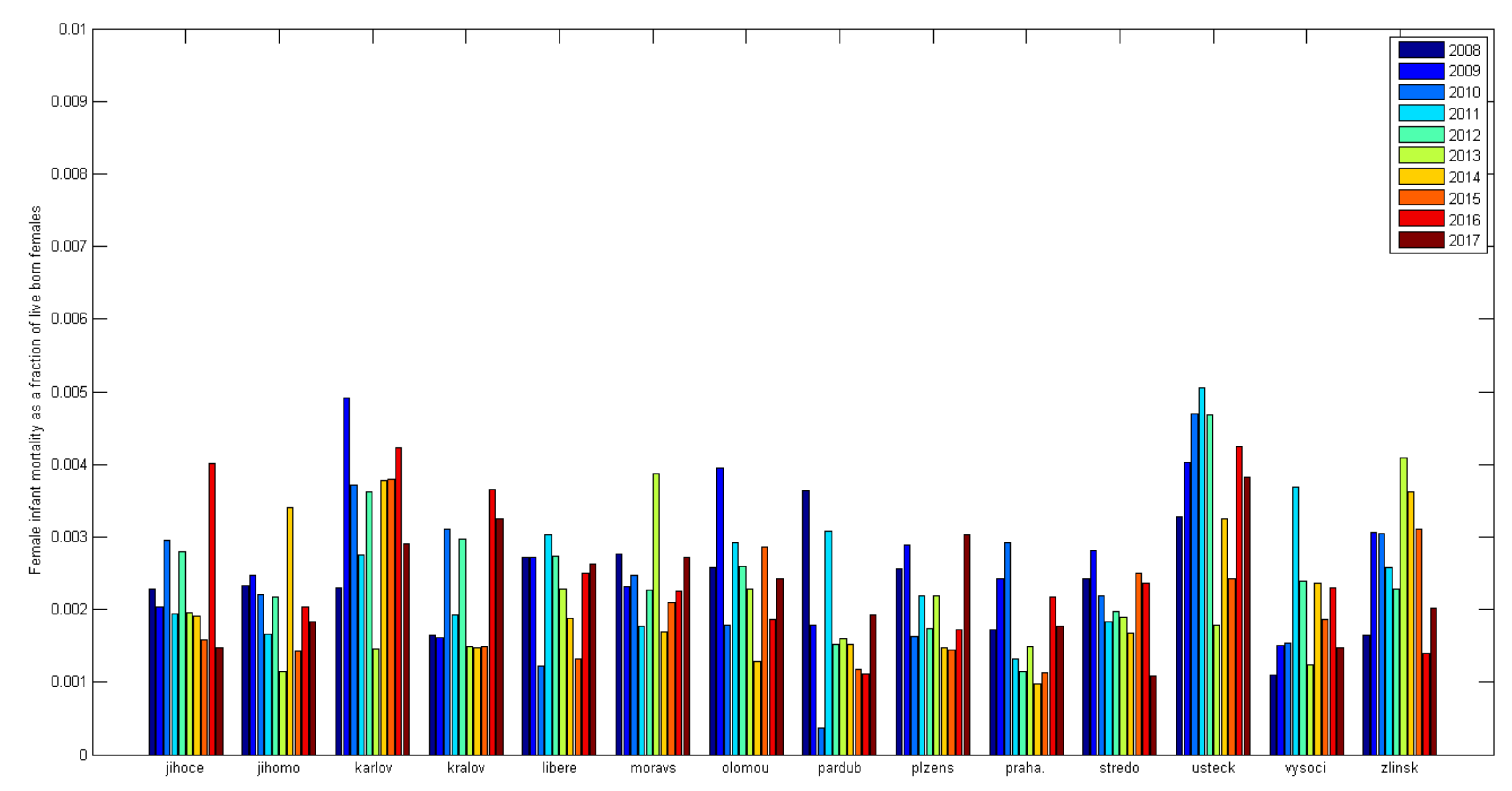
- The proportion of forensic and medical autopsies varies significantly from one department to another (while in OL, there are 4.4 times more forensic than medical, in BR only 1.5 times more).
- The most significant differences between departments were found in diagnosing asphyxia and SIDS (OVA—asphyxia 0%, OL 40%; SIDS OVA 23%, OL 5%).
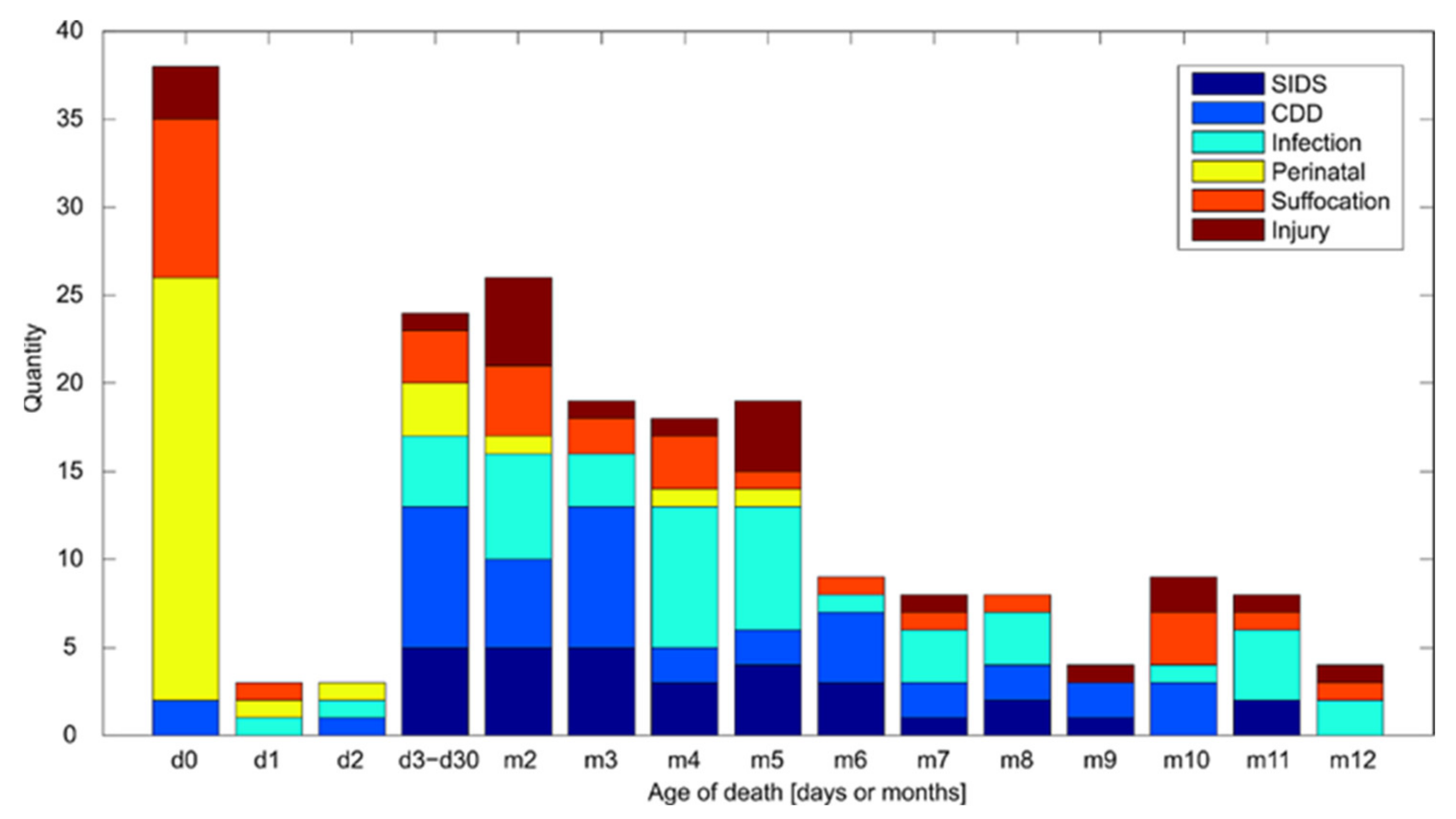
- Most SIDS are diagnosed between one month and three months, with infant mortality generally decreasing after six months. The research results confirm Meadow’s theory, and this trend has not changed over the years.
- It can be concluded that diagnosis suffocation is found more significant where SIDS is not diagnosed as a cause of death.
- The diagnosis of suffocation is typical for up to 4 months of infant life; predominantly, infants die of suffocation in the first month of age.
- There was a variation in the frequency of diagnosis of suffocation (BR—16.8% of total cases of the workplace, OL 9.3%, OVA 3%) throughout the study period.
- Most often, only health risk factors are listed in the documentation, even for diagnoses requiring social findings.
- For diagnoses where social risk factors are not required (infections), these are reported statistically significantly more often than other diagnoses (OVA 1:8).
- Diagnoses of infections in hostile factors are tracked significantly more often (especially OL and OVA). Despite the collection of this information, diagnosis of infection is usually ultimately determined as the cause of death.
- A significant amount of relevant information on social and host risk factors is missing (out of 204 autopsy files, 116 files were missing backup information).
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- MacDorman, M.F.; Mathews, T.J.; Mohangoo, A.D.; Zeitlin, J. International Comparisons of Infant Mortality and Related Factors: United States and Europe, 2010; CDC: Atlanta, GA, USA, 2014.
- WHO. Health 21-Health for All in the 21st Century; WHO: Copenhagen, Denmark, 1999; Volume 68, p. 146. [Google Scholar]
- Andreev, E.M.; Kingkade, W.W. Average Age at Death in Infancy and Infant Mortality Level: Reconsidering the Coale-Demeny Formulas at Current Levels of Low Mortality; Max Planck Institute for Demographic Research Working Paper: Munich, Germany, 2011; Volume 16. [Google Scholar]
- WHO International Classification of Diseases (ICD). Available online: https://www.who.int/standards/classifications/classification-of-diseases (accessed on 23 April 2022).
- Meadow, R. Unnatural Sudden Infant Death. Arch. Dis. Child. 1999, 80, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Stanton, J.; Simpson, A. Murder Misdiagnosed as SIDS: A Perpetrator’s Perspective. Arch. Dis. Child. 2001, 85, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Leach, C.E.A.; Blair, P.S.; Fleming, P.J.; Smith, I.J.; Ward-Platt, M.; Berry, P.J.; BCH, F.; Golding, J. Epidemiology of SIDS and Explained Sudden Infant Deaths. Pediatrics 1999, 104, e43–e53. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, K.; Mcgarvey, C.; Devaney, D.; Matthews, T. How Reliable Are SIDS Rates? Arch. Dis. Child. 2005, 90, 1082–1083. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Busuttil, A.; Keeling, J. Paediatric Forensic Medicine and Pathology; Hodder Arnold: London, UK, 2009; ISBN 0-340-73157-5. [Google Scholar]
- Ottaviani, G. Crib Death: Sudden Unexplained Death of Infants—The Pathologist’s Viewpoint; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Gilbert-Barness, E.; Debich-Spicer, D.E. Handbook of Pediatric Autopsy Pathology; Springer: Berlin/Heidelberg, Germany, 2005. [Google Scholar]
- Matějů, MUDr Eva. Forenzní Pohled Na Problematiku SIDS v České Republice; Matějů, MUDr Eva: Brno, Czech Republic, 2009. [Google Scholar]
- Gilbert-Barness, E.; Spicer, D.E.; Steffensen, T.S. Handbook of Pediatric Autopsy Pathology; Springer: Berlin/Heidelberg, Germany, 2013; pp. 329–354. [Google Scholar]
- Corey, T.S.; Hanzlick, R.; Howard, J.; Nelson, C.; Krous, H. Ad Hoc Committee on Sudden Unexplained Infant Death. A Functional Approach to Sudden Unexplained Infant Deaths. Am. J. Forensic Med. Pathol. 2007, 28, 271–277. [Google Scholar] [CrossRef]
- Jorch, G.; Tapiainen, T.; Bonhoeffer, J.; Fischer, T.; Heininger, U.; Hoet, B.; Kohl, K.; Lewis, N.; Meyer, C.; Nelson, T.; et al. Unexplained Sudden Death, Including Sudden Infant Death Syndrome (SIDS), in the First and Second Years of Life: Case Definition and Guidelines for Collection, Analysis, and Presentation of Immunization Safety Data. Vaccine 2007, 25, 5707–5716. [Google Scholar] [CrossRef]
- Weber, M.A.; Ashworth, M.T.; Risdon, R.A.; Hartley, J.C.; Malone, M.; Sebire, N.J. The Role of Post-Mortem Investigations in Determining the Cause of Sudden Unexpected Death in Infancy. Arch. Dis. Child. 2008, 93, 1048–1053. [Google Scholar] [CrossRef]
- Shapiro-Mendoza, C.K.; Kim, S.Y.; Chu, S.Y.; Kahn, E.; Anderson, R.N. Using Death Certificates to Characterize Sudden Infant Death Syndrome (SIDS): Opportunities and Limitations. J. Pediatr. 2010, 156, 38–43. [Google Scholar] [CrossRef]
- Shapiro-Mendoza, C.K.; Camperlengo, L.; Ludvigsen, R.; Cottengim, C.; Anderson, R.N.; Andrew, T.; Covington, T.; Hauck, F.R.; Kemp, J.; MacDorman, M. Classification System for the Sudden Unexpected Infant Death Case Registry and Its Application. Pediatrics 2014, 134, e210–e219. [Google Scholar] [CrossRef]
- Devitt, M. AAP Expands Recommendations on SIDS and Other Sleep-Related Deaths. AFP 2012, 85, 918–923. [Google Scholar]
- Byard, R.W.; Krous, H.F. Sudden Infant Death Syndrome: Overview and Update. Pediatr. Dev. Pathol. 2003, 6, 112–127. [Google Scholar] [CrossRef]
- Pollack, H.A. Changes in the Timing of SIDS Deaths in 1989 and 1999: Indirect Evidence of Low Homicide Prevalence among Reported Cases. Paediatr. Perinat. Epidemiol. 2006, 20, 2–13. [Google Scholar] [CrossRef]
- Takatsu, A.; Shigeta, A.; Sakai, K.; Abe, S. Risk Factors, Diagnosis and Prevention of Sudden Unexpected Infant Death. Legal Med. 2007, 9, 76–82. [Google Scholar] [CrossRef]
- Pinho, A.P.S.; Nunes, M.L. Epidemiological Profile and Strategies for Diagnosing SIDS in a Developing Country. J. Pediatr. 2011, 87, 115–122. [Google Scholar] [CrossRef][Green Version]
- Sharma, B.R. Sudden Infant Death Syndrome: A Subject of Medicolegal Research. Am. J. Forensic Med. Pathol. 2007, 28, 69–72. [Google Scholar] [CrossRef]
- Ahmed, S.; Mitchell, I.; Wolbring, G. Analysis of Sudden Infant Death Syndrome Coverage in Canadian Newspapers. J. Child Health Care 2018, 22, 545–562. [Google Scholar] [CrossRef]
- Krous, H.F.; Nadeau, J.M.; Silva, P.D.; Byard, R.W. Infanticide: Is Its Incidence among Postneonatal Infant Deaths Increasing? An 18-Year Population-Based Analysis in California. Am. J. Forensic Med. Pathol. 2002, 23, 127–131. [Google Scholar] [CrossRef]
- Goldstein, R.D.; Blair, P.S.; Sens, M.A.; Shapiro-Mendoza, C.K.; Krous, H.F.; Rognum, T.O.; Moon, R.Y. Inconsistent Classification of Unexplained Sudden Deaths in Infants and Children Hinders Surveillance, Prevention and Research: Recommendations from The 3rd International Congress on Sudden Infant and Child Death. Forensic Sci. Med. Pathol. 2019, 15, 622–628. [Google Scholar] [CrossRef]
- Shapiro-Mendoza, C.K.; Parks, S.E.; Brustrom, J.; Andrew, T.; Camperlengo, L.; Fudenberg, J.; Payn, B.; Rhoda, D. Variations in Cause-of-Death Determination for Sudden Unexpected Infant Deaths. Pediatrics 2017, 140, e20170087. [Google Scholar] [CrossRef]
- Bamber, A.R.; Paine, S.M.; Ridout, D.A.; Pryce, J.W.; Jacques, T.S.; Sebire, N.J. Brain Weight in Sudden Unexpected Death in Infancy: Experience from a Large Single-centre Cohort. Neuropathol. Appl. Neurobiol. 2016, 42, 344–351. [Google Scholar] [CrossRef]
- Vazquez, R.E.Z.; Coetzee, A.; Harlock, E.; Simmerson, M.; Cohen, M.C. Measurement of Nucleated Red Blood Cells in the Peripheral Blood as a Marker of Hypoxia in Sudden Unexpected Death in Infancy. J. Clin. Pathol. 2015, 68, 718–722. [Google Scholar] [CrossRef]
- Takiguchi, M.; Knight, T.; Nguyen, T.T.; Limm, B.; Hayes, D.; Reddy, V.; Bratincsak, A. Underdiagnosis of Conditions Associated with Sudden Cardiac Death in Children-Is It the Absence of a Comprehensive Screening Program or a True Low Prevalence? Hawai’i J. Med. Public Health 2016, 75, 42. [Google Scholar]
- Matshes, E.W.; Lew, E.O. An Approach to the Classification of Apparent Asphyxial Infant Deaths. Acad. Forensic Pathol. 2017, 7, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Shipstone, R.A.; Young, J.; Thompson, J.M.D.; Byard, R.W. An Evaluation of Pathologists’ Application of the Diagnostic Criteria from the San Diego Definition of SIDS and Unclassified Sudden Infant Death. Int. J. Leg. Med. 2020, 134, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Byard, R.W.; Shipstone, R.A.; Young, J. Continuing Major Inconsistencies in the Classification of Unexpected Infant Deaths. J. Forensic Leg. Med. 2019, 64, 20–22. [Google Scholar] [CrossRef]
- Erck Lambert, A.B.; Parks, S.E.; Shapiro-Mendoza, C.K. National and State Trends in Sudden Unexpected Infant Death: 1990-2015. Pediatrics 2018, 141, e20173519. [Google Scholar] [CrossRef] [PubMed]
- Moon, R.Y. SIDS and Other Sleep-Related Infant Deaths: Evidence Base for 2016 Updated Recommendations for a Safe Infant Sleeping Environment. Pediatrics 2016, 138, e20162940. [Google Scholar] [CrossRef] [PubMed]
- Pasquale-Styles, M.A.; Regensburg, M.; Bao, R. Sudden Unexpected Infant Death Certification in New York City: Intra-Agency Guideline Compliance and Variables That May Influence Death Certification. Acad. Forensic Pathol. 2017, 7, 536–550. [Google Scholar] [CrossRef]
- Wilson, A.L.; Randall, B. Trends in Rates of Sudden Unexpected Infant Death (SUID): Hopes for Prevention. South Dak. Med. J. South Dak. State Med. Assoc. 2021, 74, 220–226. [Google Scholar]
- Nya, S.; Abouzahir, H.; Belhouss, A.; Benyaich, H. Unexpected Death of an Infant Suffocated in the Course of Breastfeeding When the Mother Fell Asleep. Medico-Legal J. 2021, 89, 139–142. [Google Scholar] [CrossRef]
- Kim, H.; Pearson-Shaver, A.L. Sudden Infant Death Syndrome; StatPearls [Internet]: Treasure Island, FL, USA, 2021. [Google Scholar]
- Byard, R.W. Sudden Infant Death Syndrome: Definitions; University of Adelaide Press: Adelaide, Australia, 2018. [Google Scholar]
- Bouška, I.; Toupalík, P. Soudnělékařská Diagnostika Náhlé Smrti; Karolinum: Prague, Czech Republic, 2012; ISBN 80-246-2138-X. [Google Scholar]
- Meadow, R. Suffocation, Recurrent Apnea, and Sudden Infant Death. J. Pediatr. 1990, 117, 351–357. [Google Scholar] [CrossRef]
- Bajanowski, T.; Brinkmann, B.; Vennemann, M. The San Diego Definition of SIDS: Practical Application and Comparison with the GeSID Classification. Int. J. Leg. Med. 2006, 120, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Rognum, T.O.; Saugstad, O.D. Biochemical and Immunological Studies in SIDS Victims. Clues to Understanding the Death Mechanism. Acta Paediatr. 1993, 82, 82–85. [Google Scholar] [CrossRef] [PubMed]
- Hymel, K.P.; American Academy of Pediatrics. Distinguishing Sudden Infant Death Syndrome from Child Abuse Fatalities. Pediatrics 2006, 118, 421–427. [Google Scholar]
- Perrone, S.; Lembo, C.; Moretti, S.; Prezioso, G.; Buonocore, G.; Toscani, G.; Marinelli, F.; Nonnis-Marzano, F.; Esposito, S. Sudden Infant Death Syndrome: Beyond Risk Factors. Life 2021, 11, 184. [Google Scholar] [CrossRef]
- Galván-Tejada, C.E.; Villagrana-Bañuelos, K.E.; Zanella-Calzada, L.A.; Moreno-Báez, A.; Luna-García, H.; Celaya-Padilla, J.M.; Galván-Tejada, J.I.; Gamboa-Rosales, H. Univariate Analysis of Short-Chain Fatty Acids Related to Sudden Infant Death Syndrome. Diagnostics 2020, 10, 896. [Google Scholar] [CrossRef]
- Olecká, I. Sociální Rizikové Faktory Matek Dětí Zemřelých Náhle, Neočekávaně a Násilně Do Jednoho Roku Života [Social Risk Factors of Mothers of Children Up to One Year of Age Who Died Suddenly, Unexpectedly and Violently]. Ph.D. Dissertation, Univerzita Palackého v Olomouci, Lékařská fakulta, Prague, Czech Republic, 2018. [Google Scholar]
- Ivanová, K.; Olecká, I. Kumulativní Efekt Sociálních Rizikových Faktorů u Kojenců Zemřelých Udušením; Czecho-Slovak Pediatrics/Cesko-Slovenska Pediatrie: Prague, Czech Republic, 2020; Volume 75. [Google Scholar]
- Olecká, I.; Ivanová, K.; Lemrová, A.; Dobiáš, M. Handlos Petr Náhlá, Neočekávaná a Násilná Úmrtí Dětí Do 1 Roku Na Severní Moravě v Letech 2007–2016: Sudden, Unexpected and Violent Deaths of Children up to 1 Year in Northern Moravia Region between 2007 and 2016. Folia Soc. Med. Leg. Slovacae 2018, 8, 8–15. [Google Scholar]
- Ivanová, K.; Olecká, I.; Dobiáš, M.; Hrubá; Jurickova, L.; Hanák, P.; Ondra, P. Analýza Pitevních Protokolů Dětí Zemřelých Do Jednoho Roku Života v Olomouckém a Zlínském Kraji: Možné Souvislosti Zdravotní Gramotnosti Matek s Diagnózou SIDS. Folia Soc. Med. Leg. Slovacae 2016, 6, 38–44. [Google Scholar]
- ÚZIS ÚZIS ČR–Knihovna a Archiv: Deaths within One Year by Cause of Death in Years 2014–2016. Available online: https://www.uzis.cz/index.php?pg=vystupy--knihovna&id=275 (accessed on 23 April 2022).
- ČSÚ. Demographic Yearbooks (Pramenná Díla) 2017–2010; ČSÚ: Prague, Czech Republic, 2018. [Google Scholar]
- Committee on Child Abuse and Neglect Distinguishing Sudden Infant Death Syndrome From Child Abuse Fatalities. Pediatrics 1994, 94, 124–126. [CrossRef]
- James, L.F. Wrongful Diagnosis of Child Abuse—A Master Theory. J. R. Soc. Med. 2005, 98, 249–254. [Google Scholar] [CrossRef]
- Eurostat Database-Health-Eurostat. Available online: https://ec.europa.eu/eurostat/web/health/data/database (accessed on 23 April 2022).
- Levene, S.; Bacon, C.J. Sudden Unexpected Death and Covert Homicide in Infancy. Arch. Dis. Child. 2004, 89, 443–447. [Google Scholar] [CrossRef]
- Lemrová, A.; Olecká, I.; Ivanová, K. Children’s Violent Deaths in Families at Risk-Is There Any Possibility of Prevention? Kontakt 2021, 23, 297–304. [Google Scholar] [CrossRef]
- CDC Guidelines for Death Scene Investigation of Sudden, Unexplained Infant Deaths: Recommendations of the Interagency Panel on Sudden Infant Death Synd. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/00042657.htm (accessed on 23 April 2022).
- Koehler, S.A. The Importance of a Forensics Investigation of Sudden Infant Death Syndrome: Recommendations for Developing, Low and Middle Income Countries. Acta Med. Acad. 2010, 39, 165–174. [Google Scholar]
- Health 21: The Health for All Policy Framework for the WHO European Region. Available online: https://www.euro.who.int/en/publications/abstracts/health21-the-health-for-all-policy-framework-for-the-who-european-region (accessed on 23 April 2022).
- MZČR. Dlouhodobý Program Zlepšování Zdravotního Stavu Obyvatelstva ČR-Zdraví pro Všechny v 21; Století: Staré Město, Czech Republic, 2002. [Google Scholar]
- MZČR. Zdraví 2020-Národní Strategie Ochrany a Podpory Zdraví a Prevence Nemocí, 1st ed.; Ministerstvo zdravotnictví ČR: Praha, Czech Republic, 2014; ISBN 978-80-85047-47-9. [Google Scholar]
- Zeitlin, J.; Mortensen, L.; Cuttini, M.; Lack, N.; Nijhuis, J.; Haidinger, G.; Blondel, B.; Hindori-Mohangoo, A.D. Euro-Peristat Scientific Committee Declines in Stillbirth and Neonatal Mortality Rates in Europe between 2004 and 2010: Results from the Euro-Peristat Project. J. Epidemiol. Community Health 2016, 70, 609–615. [Google Scholar] [CrossRef]

| Forensic | Medical | Total | % | |
|---|---|---|---|---|
| OV | 47 | 19 | 66 | 32% |
| OL | 35 | 8 | 43 | 21% |
| BR | 57 | 38 | 95 | 47% |
| Total | 139 | 65 | 204 | 100% |
| Host | Soc | Health | Absent | ||
|---|---|---|---|---|---|
| SIDS | 0:2 | 0:2 | 2:0 | OVA | 13:2 |
| CDD | 0:1 | 0:1 | 1:0 | 21:1 | |
| Infection | 4:5 | 1:8 | 5:4 | 7:9 | |
| Perinatal | 0:3 | 0:3 | 1:2 | 8:3 | |
| Suffocation | 0:0 | 0:0 | 0:0 | 0:0 | |
| Injury | 0:0 | 0:0 | 0:0 | 2:0 | |
| SIDS | 1:0 | 0:1 | 1:0 | OL | 1:1 |
| CDD | 3:2 | 0:5 | 2:3 | 0:5 | |
| Infection | 6:1 | 1:6 | 3:4 | 3:7 | |
| Perinatal | 2:1 | 0:3 | 1:2 | 2:3 | |
| Suffocation | 7:5 | 6:6 | 10:2 | 5:12 | |
| Injury | 0:1 | 0:1 | 1:0 | 3:1 | |
| SIDS | 0:4 | 1:3 | 4:0 | BR | 11:4 |
| CDD | 1:3 | 0:4 | 1:3 | 10:4 | |
| Infection | 1:5 | 2:4 | 3:3 | 12:6 | |
| Perinatal | 3:4 | 2:5 | 5:2 | 10:7 | |
| Suffocation | 9:1 | 6:4 | 9:1 | 5:10 | |
| Injury | 11:5 | 9:7 | 13:3 | 3:13 |
| GEO/TIME | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| European Union—27 countries | 5 | 16 | 15 | 5 | 7 | 4 | 1 | 6 | 1 | 1 | : | : |
| Austria | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Belgium | 1 | 1 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
| Czechia | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 1 | 2 |
| Finland | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Germany | 0 | 5 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hungary | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Ireland | 1 | 3 | 2 | 1 | 0 | 2 | 1 | 3 | 0 | 0 | 0 | 0 |
| Latvia | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 |
| Norway | 3 | 3 | 0 | 0 | 2 | 3 | 3 | 1 | 1 | 1 | 1 | 1 |
| Poland | 3 | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Portugal | 0 | 0 | 0 | 0 | 0 | : | : | 0 | 1 | : | 0 | 0 |
| Spain | 0 | 3 | 3 | 3 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sweden | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Switzerland | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| United Kingdom | 8 | 7 | 3 | 8 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olecká, I.; Dobiáš, M.; Lemrová, A.; Ivanová, K.; Fürst, T.; Krajsa, J.; Handlos, P. Indeterminacy of the Diagnosis of Sudden Infant Death Syndrome Leading to Problems with the Validity of Data. Diagnostics 2022, 12, 1512. https://doi.org/10.3390/diagnostics12071512
Olecká I, Dobiáš M, Lemrová A, Ivanová K, Fürst T, Krajsa J, Handlos P. Indeterminacy of the Diagnosis of Sudden Infant Death Syndrome Leading to Problems with the Validity of Data. Diagnostics. 2022; 12(7):1512. https://doi.org/10.3390/diagnostics12071512
Chicago/Turabian StyleOlecká, Ivana, Martin Dobiáš, Adéla Lemrová, Kateřina Ivanová, Tomáš Fürst, Jan Krajsa, and Petr Handlos. 2022. "Indeterminacy of the Diagnosis of Sudden Infant Death Syndrome Leading to Problems with the Validity of Data" Diagnostics 12, no. 7: 1512. https://doi.org/10.3390/diagnostics12071512
APA StyleOlecká, I., Dobiáš, M., Lemrová, A., Ivanová, K., Fürst, T., Krajsa, J., & Handlos, P. (2022). Indeterminacy of the Diagnosis of Sudden Infant Death Syndrome Leading to Problems with the Validity of Data. Diagnostics, 12(7), 1512. https://doi.org/10.3390/diagnostics12071512






