Practical Approach to the Diagnosis of the Vulvo-Vaginal Stromal Tumors: An Overview
Abstract
:1. Introduction
2. Materials and Methods
3. Results
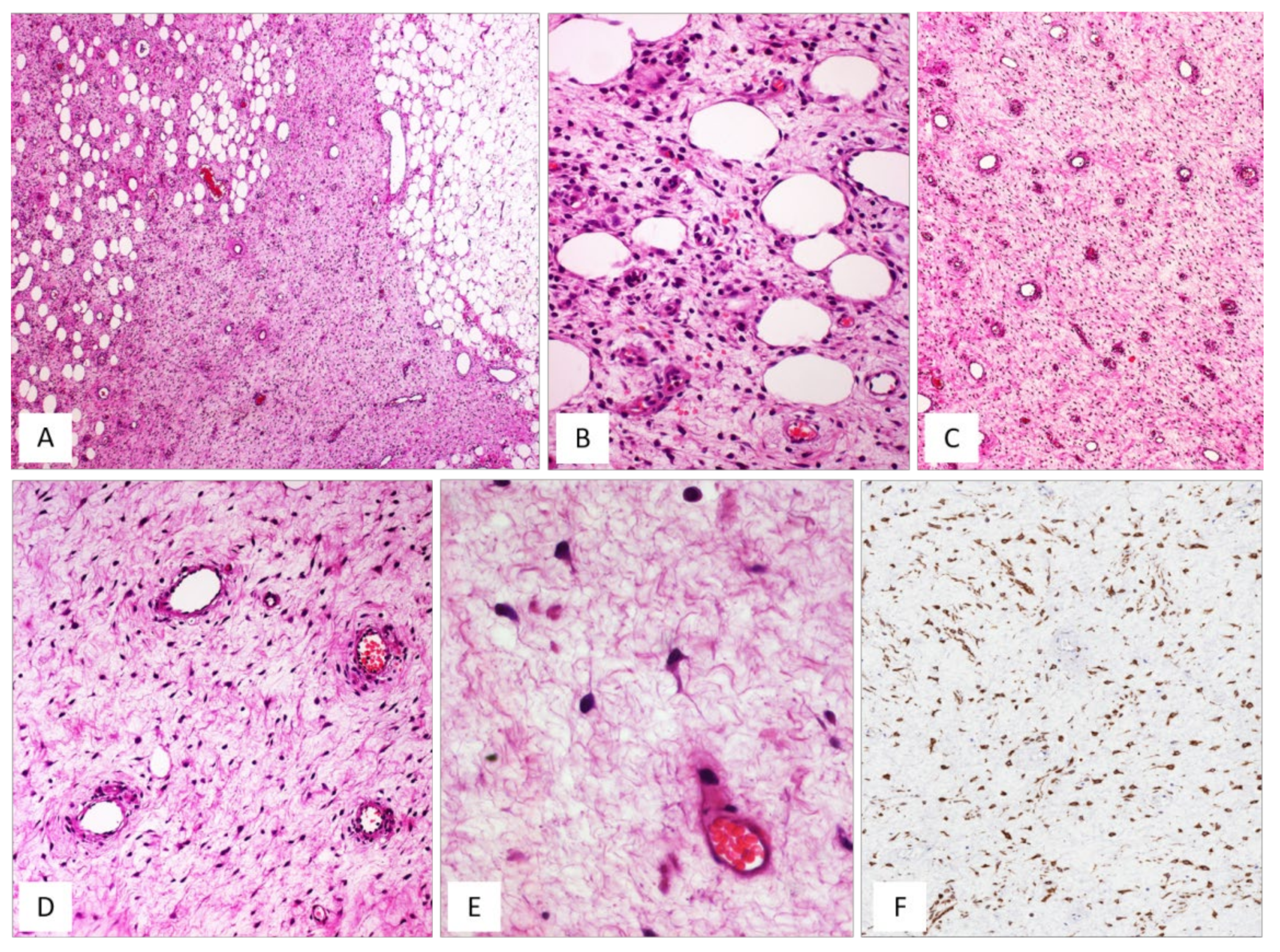
3.1. Deep (Aggressive) Angiomyxoma (DAM)
3.2. Cellular Angiofibroma (CAF)
3.3. Angiomyofibroblastoma (AMFB)
3.4. Myofibroblastoma (MFB)
4. Differential Diagnosis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McCluggage, W.G. A review and update of morphologically bland vulvovaginal mesenchymal lesions. Int. J. Gynecol. Pathol. 2005, 24, 26–38. [Google Scholar] [PubMed]
- McCluggage, W.G. Recent developments in vulvovaginal pathology. Histopathology 2009, 54, 156–173. [Google Scholar] [CrossRef] [PubMed]
- Magro, G.; Righi, A.; Casorzo, L.; Antonietta, T.; Salvatorelli, L.; Kacerovská, D.; Kazakov, D.; Michal, M. Mammary and vaginal myofibroblastomas are genetically related lesions: Fluorescence in situ hybridization analysis shows deletion of 13q14 region. Hum. Pathol. 2012, 43, 1887–1893. [Google Scholar] [CrossRef] [PubMed]
- Flucke, U.; van Krieken, J.H.; Mentzel, T. Cellular angiofibroma: Analysis of 25 cases emphasizing its relationship to spindle cell lipoma and mammary-type myofibroblastoma. Mod. Pathol. 2011, 24, 82–89. [Google Scholar] [CrossRef] [Green Version]
- Tajiri, R.; Shiba, E.; Iwamura, R.; Kubo, C.; Nawata, A.; Harada, H.; Yoshino, K.; Hisaoka, M. Potential pathogenetic link between angiomyofibroblastoma and superficial myofibroblastoma in the female lower genital tract based on a novel MTG1-CYP2E1 fusion. Mod. Pathol. 2021, 34, 2222–2228. [Google Scholar] [CrossRef]
- Cordaro, A.; Haynes, H.R.; Murigu, T.; Michal, M.; Maggiani, F.; Poyiatzis, D.; Palmer, A.; Melegh, Z. A report of a patient presenting with three metachronous 13q14LOH mesenchymal tumours: Spindle cell lipoma, cellular angiofibroma and mammary myofibroblastoma. Virchows Arch. 2021, 479, 631–635. [Google Scholar] [CrossRef]
- Magro, G. Stromal tumors of the lower female genital tract: Histogenetic, morphological and immunohistochemical similarities with the “benign spindle cell tumors of the mammary stroma”. Pathol. Res. Pract. 2007, 203, 827–829. [Google Scholar] [CrossRef]
- Steeper, T.A.; Rosai, J. Aggressive angiomyxoma of the female pelvis and perineum. Report of nine cases of a distinctive type of gynecologic soft-tissue neoplasm. Am. J. Surg. Pathol. 1983, 7, 463–475. [Google Scholar] [CrossRef]
- Nucci, M.R.; Bridge, J.A. Deep (aggressive) angiomyxoma. In WHO Classification of Soft Tissue and Bone Tumours, 5th ed.; WHO Classification of Tumours Editorial Board; International Agency for Research on Cancer: Lyon, France, 2020; Volume 3, pp. 266–267. [Google Scholar]
- Granter, S.R.; Nucci, M.R.; Fletcher, C.D. Aggressive angiomyxoma: Reappraisal of its relationship to angiomyofibroblastoma in a series of 16 cases. Histopathology 1997, 30, 3–10. [Google Scholar] [CrossRef]
- Fetsch, J.F.; Laskin, W.B.; Lefkowitz, M.; Kindblom, L.G.; Meis-Kindblom, J.M. Aggressive angiomyxoma: A clinicopathologic study of 29 female patients. Cancer 1996, 78, 79–90. [Google Scholar] [CrossRef]
- Amezcua, C.A.; Begley, S.J.; Mata, N.; Felix, J.C.; Ballard, C.A. Aggressive angiomyxoma of the female genital tract: A clinicopathologic and immunohistochemical study of 12 cases. Int. J. Gynecol. Cancer 2005, 15, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Magro, G.; Angelico, G.; Michal, M.; Broggi, G.; Zannoni, G.F.; Covello, R.; Marletta, S.; Salvatorelli, L.; Parenti, R. The Wide Morphological Spectrum of Deep (Aggressive) Angiomyxoma of the Vulvo-Vaginal Region: A Clinicopathologic Study of 36 Cases, including Recurrent Tumors. Diagnostics 2021, 11, 1360. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, F.; Erickson-Johnson, M.R.; Keeney, G.L.; Clayton, A.C.; Nascimento, A.G.; Wang, X.; Oliveira, A.M. Frequency and Characterization of HMGA2 and HMGA1 Rearrangements in Mesenchymal Tumors of the Lower Genital Tract. Genes Chromosomes Cancer 2007, 46, 981–990. [Google Scholar] [CrossRef] [PubMed]
- Harkness, R.; McCluggage, W.G. HMGA2 Is a Useful Marker of Vulvovaginal Aggressive Angiomyxoma but May Be Positive in Other Mesenchymal Lesions at This Site. Int. J. Gynecol. Pathol. 2021, 40, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Nucci, M.R.; Granter, S.R.; Fletcher, C.D. Cellular angiofibroma: A benign neoplasm distinct from angiomyofibroblastoma and spindle cell lipoma. Am. J. Surg. Pathol. 1997, 21, 636–644. [Google Scholar] [CrossRef] [PubMed]
- Ywasa, Y.; Fletcher, C.D.M.; Flucke, U. Cellular angiofibroma. In WHO Classification of Soft Tissue and Bone Tumours, 5th ed.; WHO Classification of Tumours Editorial Board; International Agency for Research on Cancer: Lyon, France, 2020; Volume 3, pp. 80–81. [Google Scholar]
- Laskin, W.B.; Fetsch, J.F.; Mostofi, F.K. Angiomyofibroblastomalike tumor of the male genital tract: Analysis of 11 cases with comparison to female angiomyofibroblastoma and spindle cell lipoma. Am. J. Surg. Pathol. 1998, 22, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Iwasa, Y.; Fletcher, C.D. Cellular angiofibroma: Clinicopathologic and immunohistochemical analysis of 51 cases. Am. J. Surg. Pathol. 2004, 28, 1426–1435. [Google Scholar] [CrossRef]
- McCluggage, W.G.; Ganesan, R.; Hirschowitz, L.; Rollason, T.P. Cellular angiofibroma and related fibromatous lesions of the vulva: Report of a series of cases with a morphological spectrum wider than previously described. Histopathology 2004, 45, 360–368. [Google Scholar] [CrossRef]
- Maggiani, F.; Debiec-Rychter, M.; Vanbockrijck, M.; Sciot, R. Cellular angiofibroma: Another mesenchymal tumour with 13q14 involvement, suggesting a link with spindle cell lipoma and (extra)-mammary myofibroblastoma. Histopathology 2007, 51, 410–412. [Google Scholar] [CrossRef]
- Chen, E.; Fletcher, C.D. Cellular angiofibroma with atypia or sarcomatous transformation: Clinicopathologic analysis of 13 cases. Am. J. Surg. Pathol. 2010, 34, 707–714. [Google Scholar] [CrossRef]
- Chien, Y.C.; Mokánszki, A.; Huang, H.Y.; Geronimo Silva, R., Jr.; Chen, C.C.; Beke, L.; Mónus, A.; Méhes, G. First Glance of Molecular Profile of Atypical Cellular Angiofibroma/Cellular Angiofibroma with Sarcomatous Transformation by Next Generation Sequencing. Diagnostics 2020, 10, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Creytens, D. Cellular Angiofibroma with Sarcomatous Transformation Showing Pleomorphic Liposarcoma-Like and Atypical Lipomatous Tumor-Like Features. Am. J. Dermatopathol. 2016, 38, 712–714. [Google Scholar] [CrossRef] [PubMed]
- McCluggage, W.G.; Perenyei, M.; Irwin, S.T. Recurrent cellular angiofibroma of the vulva. J. Clin. Pathol. 2002, 55, 477–479. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dargent, J.L.; de Saint Aubain, N.; Galdón, M.G.; Valaeys, V.; Cornut, P.; Noël, J.C. Cellular angiofibroma of the vulva: A clinicopathological study of two cases with documentation of some unusual features and review of the literature. J. Cutan. Pathol. 2003, 30, 405–411. [Google Scholar] [CrossRef]
- Fletcher, C.D.; Tsang, W.Y.; Fisher, C.; Lee, K.C.; Chan, J.K. Angiomyofibroblastoma of the vulva. A benign neoplasm distinct from aggressive angiomyxoma. Am. J. Surg. Pathol. 1992, 16, 373–382. [Google Scholar] [CrossRef] [PubMed]
- Nucci, M.R.; Fletcher, C.D. Vulvovaginal soft tissue tumours: Update and review. Histopathology 2000, 36, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, C.D.M. Angiomyofibroblastoma. In WHO Classification of Soft Tissue and Bone Tumours, 5th ed.; WHO Classification of Tumours Editorial Board; International Agency for Research on Cancer: Lyon, France, 2020; Volume 3, pp. 78–79. [Google Scholar]
- Nagai, K.; Aadachi, K.; Saito, H. Huge pedunculated angiomyofibroblastoma of the vulva. Int. J. Clin. Oncol. 2010 15, 201–205. [CrossRef]
- Omori, M.; Toyoda, H.; Hirai, T.; Ogino, T.; Okada, S. Angiomyofibroblastoma of the vulva: A large pedunculated mass formation. Acta Med. Okayama 2006, 60, 237–242. [Google Scholar]
- Ockner, D.M.; Sayadi, H.; Swanson, P.E.; Ritter, J.H.; Wick, M.R. Genital angiomyofibroblastoma. Comparison with aggressive angiomyxoma and other myxoid neoplasms of skin and soft tissue. Am. J. Clin. Pathol. 1997, 107, 36–44. [Google Scholar] [CrossRef] [Green Version]
- Nasu, K.; Fujisawa, K.; Takai, N.; Miyakawa, I. Angiomyofibroblastoma of the vulva. Int. J. Gynecol. Cancer 2002, 12, 228–231. [Google Scholar] [CrossRef]
- Perko, Z.; Durdov, M.G.; Druzijanić, N.; Kraljević, D.; Juricić, J. Giant Perianal Angiomyofibroblastoma—A Case Report. Coll. Antropol. 2006, 1, 243–246. [Google Scholar]
- Upreti, S.; Morine, A.; Ng, D.; Bigby, S.M. Lipomatous variant of angiomyofibroblastoma: A case report and review of the literature. J. Cutan. Pathol. 2015, 42, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Magro, G.; Righi, A.; Caltabiano, R.; Casorzo, L.; Michal, M. Vulvovaginal angiomyofibroblastomas: Morphologic, immunohistochemical, and fluorescence in situ hybridization analysis for deletion of 13q14 region. Hum. Pathol. 2014, 45, 1647–1655. [Google Scholar] [CrossRef] [PubMed]
- Magro, G.; Salvatorelli, L.; Angelico, G.; Vecchio, G.M.; Caltabiano, R. Lipomatous angiomyofibroblastoma of the vulva: Diagnostic and histogenetic considerations. Pathologica 2014, 106, 322–326. [Google Scholar]
- Luis, P.P.; Quiñonez, E.; Nogales, F.F.; McCluggage, W.G. Lipomatous variant of angiomyofibroblastoma involving the vulva: Report of 3 cases of an extremely rare neoplasm with discussion of the differential diagnosis. Int. J. Gynecol. Pathol. 2015, 34, 204–207. [Google Scholar] [CrossRef]
- Nili, F.; Nicknejad, N.; Salarvand, S.; Akhavan, S. Lipomatous Angiomyofibroblastoma of the Vulva: Report of a Rare Variant. Int. J. Gynecol. Pathol. 2017, 36, 300–303. [Google Scholar] [CrossRef]
- Nielsen, G.P.; Young, R.H.; Dickersin, G.R.; Rosenberg, A.E. Angiomyofibroblastoma of the vulva with sarcomatous transformation (“angiomyofibrosarcoma”). Am. J. Surg. Pathol. 1997, 21, 1104–1108. [Google Scholar] [CrossRef] [PubMed]
- Folpe, A.L.; Tworek, J.A.; Weiss, S.W. Sarcomatous transformation in angiomyofibroblastomas: A clinicopathological, histological and immunohistochemical study of eleven cases. Mod. Pathol. 2001, 14, 12A. [Google Scholar]
- Barat, S.; TirgarTabari, S.; Shafaee, S. Angiomyofibroblastoma of the Vulva. Arch. Iran. Med. 2008, 11, 224–226. [Google Scholar]
- Laskin, W.B.; Fetsch, J.F.; Tavassoli, F.A. Angiomyofibroblastoma of the female genital tract: Analysis of 17 cases including a lipomatous variant. Hum. Pathol. 1997, 28, 1046–1055. [Google Scholar] [CrossRef]
- Takeshima, Y.; Shinkoh, Y.; Inai, K. Angiomyofibroblastoma of the vulva: A mitotically active variant? Pathol. Int. 1998, 48, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Fukunaga, M.; Nomura, K.; Matsumoto, K.; Doi, K.; Endo, Y.; Ushigome, S. Vulval angiomyofibroblastoma. Clinicopathologic analysis of six cases. Am. J. Clin. Pathol. 1997, 107, 45–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsukuma, S.; Koga, A.; Suematsu, R.; Takeo, H.; Sato, K. Lipomatous angiomyofibroblastoma of the vulva: A case report and review of the literature. Mol. Clin. Oncol/ 2017, 6, 83–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hara, N.; Kawaguchi, M.; Koike, H.; Nishiyama, T.; Takahashi, K. Angiomyxoid tumor with an intermediate feature between cellular angiofibroma and angiomyofibroblastoma in the male inguinal region. Int. J. Urol. 2005, 12, 768–772. [Google Scholar] [CrossRef]
- Suleiman, M.; Duc, C.; Ritz, S.; Bieri, S. Pelvic excision of large aggressive angiomyxoma in a woman: Irradiation for recurrent disease. Int. J. Gynecol. Cancer 2006, 16 (Suppl. S1), 356–360. [Google Scholar] [CrossRef]
- Laskin, W.B.; Fetsch, J.F.; Tavassoli, F.A. Superficial cervicovaginal myofibroblastoma: Fourteen cases of a distinctive mesenchymal tumor arising from the specialized subepithelial stroma of the lower female genital tract. Hum. Pathol. 2001, 32, 715–725. [Google Scholar] [CrossRef]
- Ganesan, R.; McCluggage, W.G.; Hirschowitz, L.; Rollason, T.P. Superficial myofibroblastoma of the lower female genital tract: Report of a series including tumours with a vulval location. Histopathology 2005, 46, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.J.; Amanuel, B.; Brennan, B.A.; Jain, S.; Rajakaruna, R.; Wallace, S. Superficial cervico-vaginal myofibroblastoma: A report of five cases. Pathology 2005, 37, 144–148. [Google Scholar] [CrossRef]
- Magro, G.; Caltabiano, R.; Kacerovská, D.; Vecchio, G.M.; Kazakov, D.; Michal, M. Vulvovaginal myofibroblastoma: Expanding the morphological and immunohistochemical spectrum. A clinicopathologic study of 10 cases. Hum. Pathol. 2012, 43, 243–253. [Google Scholar] [CrossRef] [PubMed]
- McMenamin, M.E.; Fletcher, C.D. Mammary-type myofibroblastoma of soft tissue: A tumor closely related to spindle cell lipoma. Am. J. Surg. Pathol. 2001, 25, 1022–1029. [Google Scholar] [CrossRef] [PubMed]
- Howitt, B.E.; Fletcher, C.D. Mammary-type Myofibroblastoma: Clinicopathologic Characterization in a Series of 143 Cases. Am. J. Surg. Pathol. 2016, 40, 361–367. [Google Scholar] [CrossRef] [PubMed]










| Definition |
|
| Clinical Features |
|
| Gross Pathology |
|
| Histopathology |
|
| Immunohistochemistry/Molecular Diagnostic Features |
|
| Treatment/Prognosis |
|
|
| Definition |
|
| Clinical features |
|
| Gross pathology |
|
| Histopathology |
|
| Immunohistochemistry/Molecular Diagnostic Features |
|
| Treatment/Prognosis |
|
|
| Definition |
|
| Clinical features |
|
| Gross pathology |
|
| Histopathology |
|
| Immunohistochemistry/Molecular Features |
|
| Treatment/Prognosis |
|
|
| Definition |
|
| Clinical Features |
|
| Gross Pathology |
|
| Histopathology |
|
| Immunohistochemistry/Molecular Diagnostic Features |
|
| Treatment/Prognosis |
|
|
| Tumor | DAM | CAF | AMFB | MFB |
|---|---|---|---|---|
| localization | deep soft tissues | dermal/subcutaneous | subcutaneous | sub-epithelial/dermal lesion; the surgical samples often contain overlying vaginal mucosa or vulvar skin |
| hmargins | minimally/widely infiltrative; entrapment of adipose tissue and/or skeletal muscle and/or nerve fibres | circumscribed; occasionally minimally infiltrative | circumscribed | well circumscribed; band of native connective tissue (Grenz zone) between tumour and overlying epithelium |
| cellularity | uniformly hypocellular | uniformly cellular | alternating hypercellular and hypocellular areas | variable |
| cytology | small-sized, spindled-to-stellate cells | spindled cells, often with bipolar processes and wavy appearance (perineuroma-like resemblance) | spindled/epithelioid cells | spindled/stellate cells |
| mitoses | rare | rare; occasionally up to 3 mitoses/10HPF | rare | rare |
| growth pattern | haphazard arrangement | haphazard arrangement; short fascicles | perivascular arrangement; single cells, nests, cords, | single cells; reticular, lace-like or sieve-like pattern; short fascicles. |
| vasculature | numerous small-to-medium-to-large-sized blood vessels | numerous small-to-medium-to-large-sized blood vessels, often with hyalinized walls | numerous small-sized, thin-walled, capillary-like vessels | small-to-medium-sized blood vessels, often with hyalinized walls |
| stroma | uniformly myxoedematous with wispy collagen fibres | fibrous to focally myxoid with wispy collagen fibres | myxoid-to-focally fibrous | oedematous-to-finely-collagenous stroma; isolated thick collagen bands may be seen |
| metaplastic component | small bundles of mature, smooth-muscle cells (30% of cases) | mature fatty tissue (30% of cases) | mature, fatty tissue (10% of cases) | not reported |
| sarcomatous transformation | not reported | rare: single or multiple nodules of pleomorphic sarcoma | very rare: spindle-cell sarcoma | not reported |
| immunophenotype | desmin-positive; variable expression of α-smooth-muscle actin and HMGA2 | CD34-positive; loss of nuclear RB1 expression; variable expression of α-smooth-muscle actin; desmin is usually negative | CYP2E1-positive; variable expression of desmin (40–50% of cases), α-smooth-muscle actin and CD34; | desmin-positive; variable expression of CD34 and α-smooth-muscle actin; loss of nuclear RB1 expression |
| molecular analyses | HMGA2 rearrangements | monoallelic loss of RB1 and FOXO1 at the 13q14 locus (F.I.S.H.) | MTG1–CYP2E1 fusion transcripts | monoallelic loss of RB1 and FOXO1 at the 13q14 locus (F.I.S.H.); MTG1–CYP2E1 fusion transcripts |
| DAM vs. CAF |
|---|
Shared Features:
|
Distinguishing Features:
|
| DAM vs. MFB |
Shared Features:
|
Distinguishing Features:
|
| DAM vs. AMFB |
Shared Features:
|
Distinguishing Features:
|
| CAF vs. AMFB |
|---|
Shared Features
|
Distinguishing Features:
|
| CAF vs. MFB |
Shared Features:
|
Distinguishing Features:
|
| AMFB vs. MFB |
Shared Features:
|
Distinguishing Features:
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angelico, G.; Marletta, S.; Broggi, G.; Vigneri, P.; Vecchio, G.M.; Salvatorelli, L.; Magro, G. Practical Approach to the Diagnosis of the Vulvo-Vaginal Stromal Tumors: An Overview. Diagnostics 2022, 12, 357. https://doi.org/10.3390/diagnostics12020357
Angelico G, Marletta S, Broggi G, Vigneri P, Vecchio GM, Salvatorelli L, Magro G. Practical Approach to the Diagnosis of the Vulvo-Vaginal Stromal Tumors: An Overview. Diagnostics. 2022; 12(2):357. https://doi.org/10.3390/diagnostics12020357
Chicago/Turabian StyleAngelico, Giuseppe, Stefano Marletta, Giuseppe Broggi, Paolo Vigneri, Giada Maria Vecchio, Lucia Salvatorelli, and Gaetano Magro. 2022. "Practical Approach to the Diagnosis of the Vulvo-Vaginal Stromal Tumors: An Overview" Diagnostics 12, no. 2: 357. https://doi.org/10.3390/diagnostics12020357
APA StyleAngelico, G., Marletta, S., Broggi, G., Vigneri, P., Vecchio, G. M., Salvatorelli, L., & Magro, G. (2022). Practical Approach to the Diagnosis of the Vulvo-Vaginal Stromal Tumors: An Overview. Diagnostics, 12(2), 357. https://doi.org/10.3390/diagnostics12020357








