Identification of Novel Diagnostic Markers for Malignant Pleural Mesothelioma Using a Reverse Translational Approach Based on a Rare Synchronous Tumor
Abstract
1. Introduction
2. Materials and Methods
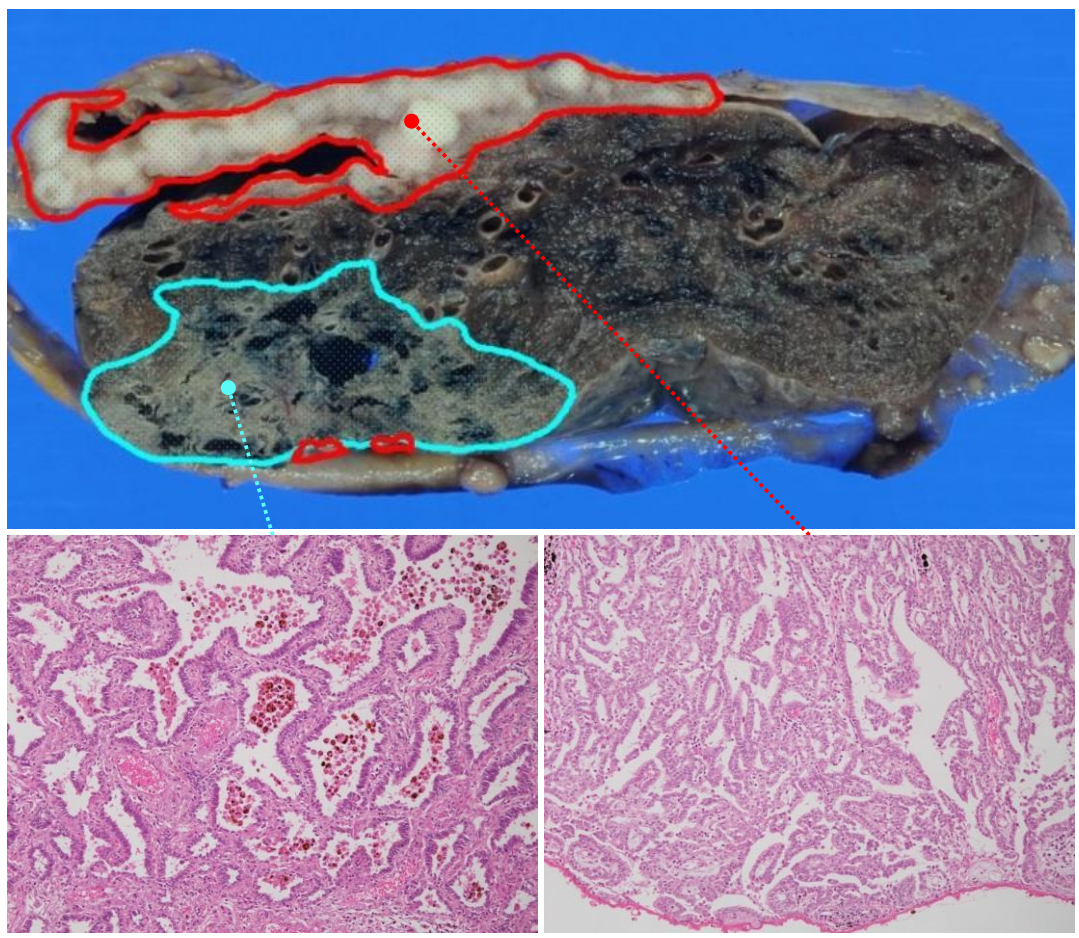
2.1. A Synchronous Collision Tumor Composed of Malignant Pleural Mesothelioma and Pulmonary Adenocarcinoma
2.2. GEP Analysis
2.3. qRT-PCR Analysis
2.4. Immunohistochemical Evaluation of MM and PAC Cases
2.5. Immunohistochemical Analysis of Various Tissues and Organs
3. Results
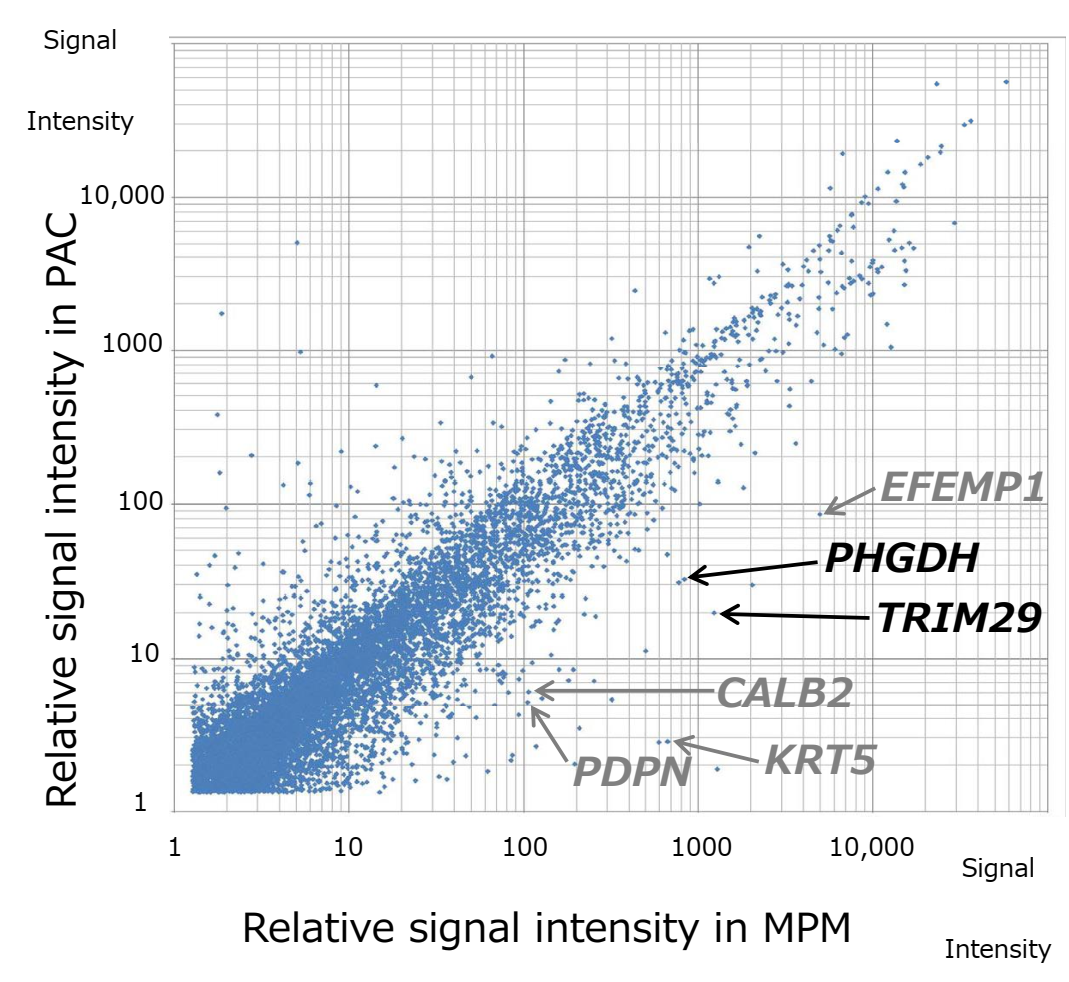
3.1. Differential GEP Analysis of MPM and PAC
3.2. Validation of MPM Markers
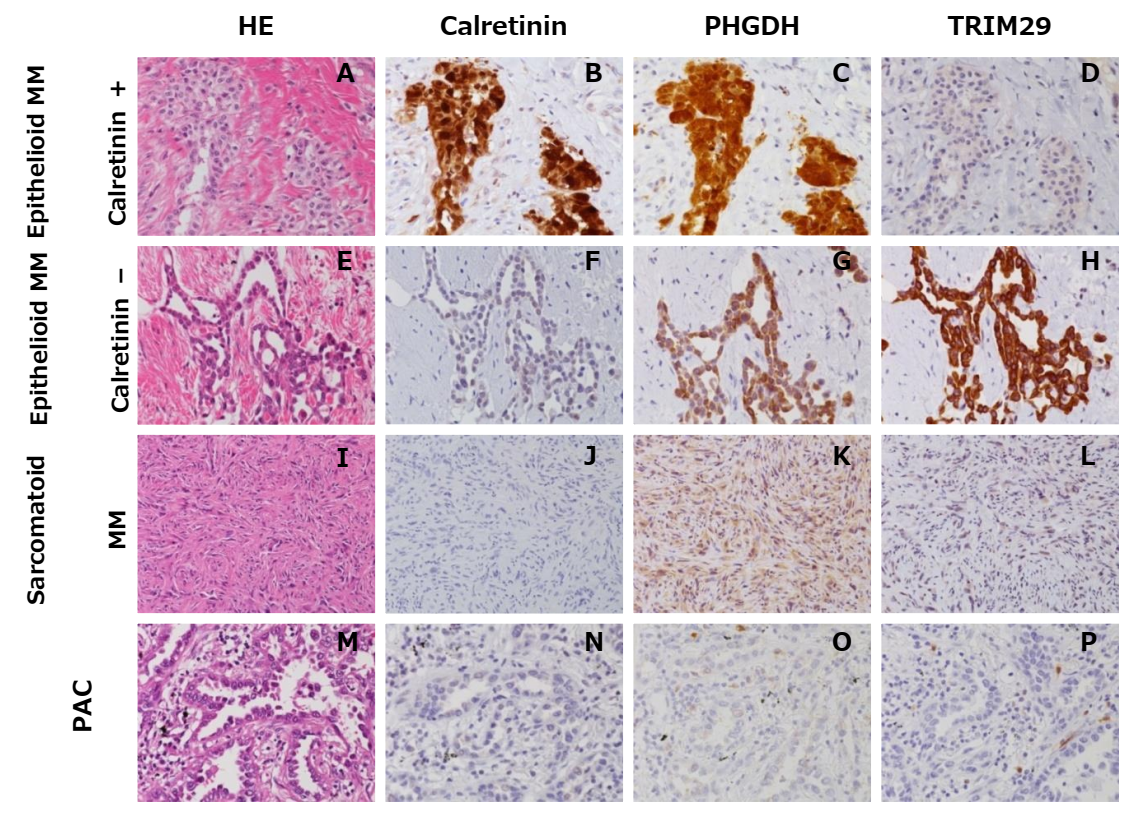
3.3. Immunohistochemical Evaluation of PHGDH and TRIM29
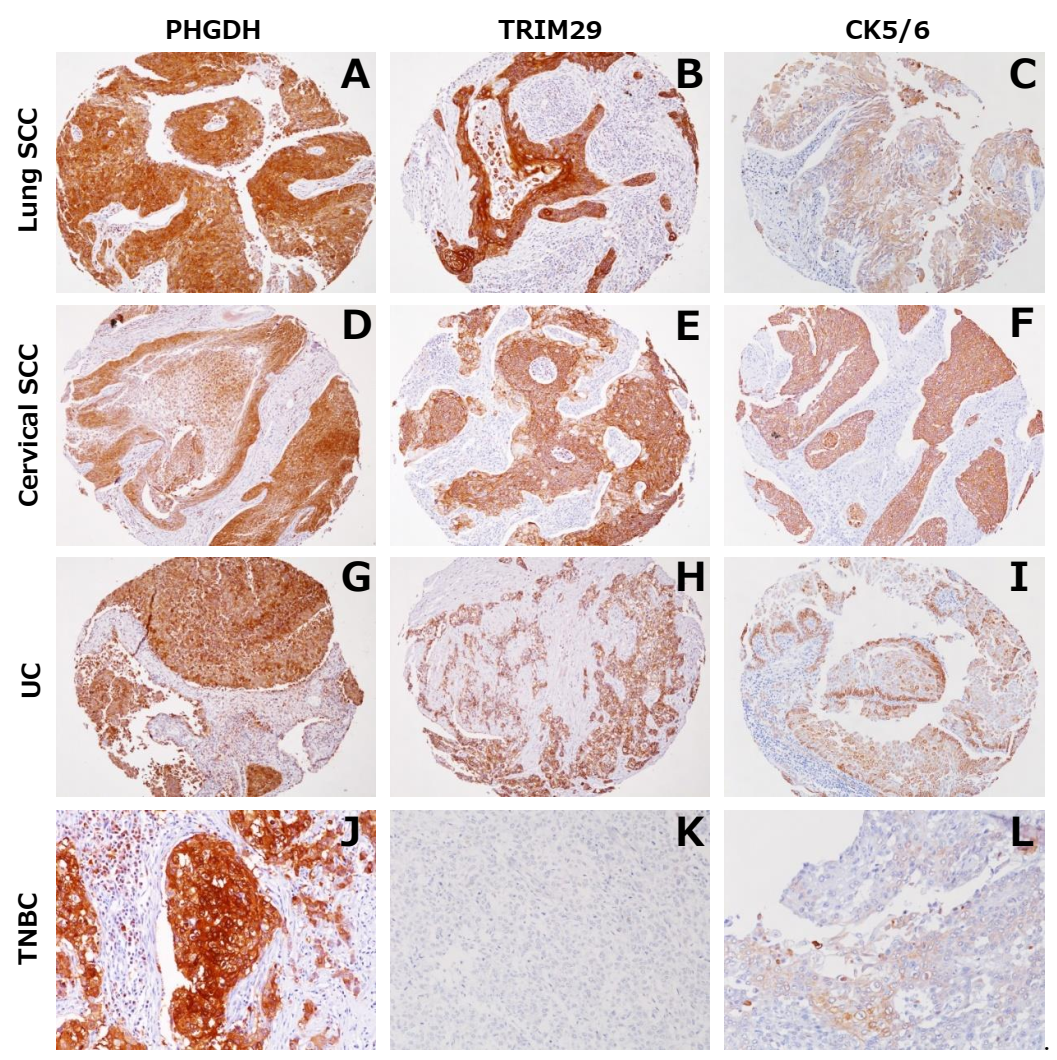
3.4. Expression of PHGDH and TRIM29 in Tumors other than MM and in Normal Tissues
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Murayama, T.; Takahashi, K.; Natori, Y.; Kurumatani, N. Estimation of future mortality from pleural malignant mesothelioma in Japan based on an age-cohort model. Am. J. Ind. Med. 2005, 49, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Kjærgaard, J.; Andersson, M. Incidence rates of malignant mesothelioma in Denmark and predicted future number of cases among men. Scand. J. Work. Environ. Health 2000, 26, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Miller, A. Mesothelioma in household members of asbestos-exposed workers: 32 United States cases since 1990. Am. J. Ind. Med. 2005, 47, 458–462. [Google Scholar] [CrossRef] [PubMed]
- Metintas, S.; Ak, G.; Metintas, M. Potential years of life and productivity loss due to malignant mesothelioma in Turkey. Arch. Environ. Occup. Health 2020, 75, 464–470. [Google Scholar] [CrossRef]
- Singhal, S.; Wiewrodt, R.; Malden, L.D.; Amin, K.M.; Matzie, K.; Friedberg, J.; Kucharczuk, J.C.; A Litzky, L.; Johnson, S.W.; Kaiser, L.R.; et al. Gene expression profiling of malignant mesothelioma. Clin. Cancer Res. 2003, 9, 3080–3097. [Google Scholar]
- Gordon, G.J.; Rockwell, G.N.; Jensen, R.V.; Rheinwald, J.G.; Glickman, J.N.; Aronson, J.P.; Pottorf, B.J.; Nitz, M.D.; Richards, W.G.; Sugarbaker, D.J.; et al. Identification of Novel Candidate Oncogenes and Tumor Suppressors in Malignant Pleural Mesothelioma Using Large-Scale Transcriptional Profiling. Am. J. Pathol. 2005, 166, 1827–1840. [Google Scholar] [CrossRef]
- López-Ríos, F.; Chuai, S.; Flores, R.; Shimizu, S.; Ohno, T.; Wakahara, K.; Illei, P.B.; Hussain, S.; Krug, L.; Zakowski, M.F.; et al. Global Gene Expression Profiling of Pleural Mesotheliomas: Overexpression of Aurora Kinases and P16/CDKN2A Deletion as Prognostic Factors and Critical Evaluation of Microarray-Based Prognostic Prediction. Cancer Res. 2006, 66, 2970–2979. [Google Scholar] [CrossRef]
- Davidson, B.; Zhang, Z.; Kleinberg, L.; Li, M.; Flørenes, V.A.; Wang, T.-L.; Shih, I.-M. Gene Expression Signatures Differentiate Ovarian/Peritoneal Serous Carcinoma from Diffuse Malignant Peritoneal Mesothelioma. Clin. Cancer Res. 2006, 12, 5944–5950. [Google Scholar] [CrossRef]
- Crispi, S.; Calogero, R.A.; Santini, M.; Mellone, P.; Vincenzi, B.; Citro, G.; Vicidomini, G.; Fasano, S.; Meccariello, R.; Cobellis, G.; et al. Global Gene Expression Profiling of Human Pleural Mesotheliomas: Identification of Matrix Metalloproteinase 14 (MMP-14) as Potential Tumour Target. PLoS ONE 2009, 4, e7016. [Google Scholar] [CrossRef]
- Suraokar, M.B.; Nunez, M.I.; Diao, L.; Chow, C.W.; Kim, D.; Behrens, C.; Lin, H.; Lee, S.; Raso, G.; Moran, C.; et al. Expression profiling stratifies mesothelioma tumors and signifies deregulation of spindle checkpoint pathway and microtubule network with therapeutic implications. Ann. Oncol. 2014, 25, 1184–1192. [Google Scholar] [CrossRef]
- Amatya, V.J.; Kushitani, K.; Mawas, A.S.; Miyata, Y.; Okada, M.; Kishimoto, T.; Inai, K.; Takeshima, Y. MUC4, a novel immunohistochemical marker identified by gene expression profiling, differentiates pleural sarcomatoid mesothelioma from lung sarcomatoid carcinoma. Mod. Pathol. 2017, 30, 672–681. [Google Scholar] [CrossRef]
- Bruno, R.; Alì, G.; Poma, A.M.; Proietti, A.; Libener, R.; Mariani, N.; Niccoli, C.; Chella, A.; Ribechini, A.; Grosso, F.; et al. Differential Diagnosis of Malignant Pleural Mesothelioma on Cytology. J. Mol. Diagn. 2020, 22, 457–466. [Google Scholar] [CrossRef]
- Morani, F.; Bisceglia, L.; Rosini, G.; Mutti, L.; Melaiu, O.; Landi, S.; Gemignani, F. Identification of Overexpressed Genes in Malignant Pleural Mesothelioma. Int. J. Mol. Sci. 2021, 22, 2738. [Google Scholar] [CrossRef]
- Minca, E.C.; Tubbs, R.R.; Portier, B.P.; Wang, Z.; Lanigan, C.; Aronow, M.E.; Triozzi, P.L.; Singh, A.; Cook, J.R.; Saunthararajah, Y.; et al. Genomic microarray analysis on formalin-fixed paraffin-embedded material for uveal melanoma prognostication. Cancer Genet. 2014, 207, 306–315. [Google Scholar] [CrossRef]
- Tyekucheva, S.; Martin, N.E.; Stack, E.C.; Wei, W.; Vathipadiekal, V.; Waldron, L.; Fiorentino, M.; Lis, R.T.; Stampfer, M.J.; Loda, M.; et al. Comparing Platforms for Messenger RNA Expression Profiling of Archival Formalin-Fixed, Paraffin-Embedded Tissues. J. Mol. Diagn. 2015, 17, 374–381. [Google Scholar] [CrossRef]
- Naka, T.; Hatanaka, Y.; Marukawa, K.; Okada, H.; Hatanaka, K.C.; Sakakibara-Konishi, J.; Oizumi, S.; Hida, Y.; Kaga, K.; Mitsuhashi, T.; et al. Comparative genetic analysis of a rare synchronous collision tumor composed of malignant pleural mesothelioma and primary pulmonary adenocarcinoma. Diagn. Pathol. 2016, 11, 38. [Google Scholar] [CrossRef][Green Version]
- Pass, H.I.; Levin, S.M.; Harbut, M.R.; Melamed, J.; Chiriboga, L.; Donington, J.; Huflejt, M.; Carbone, M.; Chia, D.; Goodglick, L.; et al. Fibulin-3 as a Blood and Effusion Biomarker for Pleural Mesothelioma. New Engl. J. Med. 2012, 367, 1417–1427. [Google Scholar] [CrossRef]
- Barone, E.; Gemignani, F.; Landi, S. Overexpressed genes in malignant pleural mesothelioma: Implications in clinical management. J. Thorac. Dis. 2018, 10, S369–S382. [Google Scholar] [CrossRef]
- Smits, A.J.; Vink, A.; Tolenaars, G.; Herder, G.J.; Kummer, J.A. Different Cutoff Values for Thyroid Transcription Factor-1 Antibodies in the Diagnosis of Lung Adenocarcinoma. Appl. Immunohistochem. Mol. Morphol. 2015, 23, 416–421. [Google Scholar] [CrossRef]
- Gromova, I.; Gromov, P.; Honma, N.; Kumar, S.; Rimm, D.; Talman, M.-L.M.; Wielenga, V.T.; Moreira, J.M. High level PHGDH expression in breast is predominantly associated with keratin 5-positive cell lineage independently of malignancy. Mol. Oncol. 2015, 9, 1636–1654. [Google Scholar] [CrossRef]
- Mullarky, E.; Mattaini, K.R.; Vander Heiden, M.G.; Cantley, L.C.; Locasale, J.W. PHGDH amplification and altered glucose metabolism in human melanoma. Pigment. Cell Melanoma Res. 2011, 24, 1112–1115. [Google Scholar] [CrossRef]
- Cho, H.M.; Jun, D.Y.; Bae, M.A.; Ahn, J.D.; Kim, Y.H. Nucleotide sequence and differential expression of the human 3-phosphoglycerate dehydrogenase gene. Gene 2000, 245, 193–201. [Google Scholar] [CrossRef]
- Jing, Z.; Heng, W.; Aiping, D.; Yafei, Q.; Shulan, Z. Expression and Clinical Significance of Phosphoglycerate Dehydrogenase and Squamous Cell Carcinoma Antigen in Cervical Cancer. Int. J. Gynecol. Cancer 2013, 23, 1465–1469. [Google Scholar] [CrossRef]
- Huang, W.; Williamson, S.; Rao, Q.; López-Beltrán, A.; Montironi, R.; Eble, J.N.; Grignon, D.J.; Idrees, M.T.; Emerson, R.E.; Zhou, X.-J.; et al. Novel markers of squamous differentiation in the urinary bladder. Hum. Pathol. 2013, 44, 1989–1997. [Google Scholar] [CrossRef]
- Hatakeyama, S. TRIM proteins and cancer. Nat. Cancer 2011, 11, 792–804. [Google Scholar] [CrossRef] [PubMed]
- Hosoi, Y.; Kapp, L.N. Expression of a Candidate Ataxia-Telangiectasia Group D Gene in Cultured Fibroblast Cell Lines and Human Tissues. Int. J. Radiat. Biol. 1994, 66, S71–S76. [Google Scholar] [CrossRef]
- Noh, S.; Kim, D.H.; Jung, W.H.; Koo, J.S. Expression levels of serine/glycine metabolism-related proteins in triple negative breast cancer tissues. Tumor Biol. 2014, 35, 4457–4468. [Google Scholar] [CrossRef]
- Kanno, Y.; Watanabe, M.; Kimura, T.; Nonomura, K.; Tanaka, S.; Hatakeyama, S. TRIM29 as a novel prostate basal cell marker for diagnosis of prostate cancer. Acta Histochem. 2014, 116, 708–712. [Google Scholar] [CrossRef]
- Masuda, Y.; Takahashi, H.; Hatakeyama, S. TRIM29 regulates the p63-mediated pathway in cervical cancer cells. Biochim. et Biophys. Acta (BBA)—Bioenerg. 2015, 1853, 2296–2305. [Google Scholar] [CrossRef] [PubMed]
- Palmbos, P.L.; Wang, Y.; Iii, A.B.; Kelleher, A.J.; Wang, L.; Yang, H.; Ahmet, M.L.; Gumkowski, E.R.; Welling, S.D.; Magnuson, B.; et al. ATDC mediates a TP63-regulated basal cancer invasive program. Oncogene 2019, 38, 3340–3354. [Google Scholar] [CrossRef]
- Song, X.; Fu, C.; Yang, X.; Sun, D.; Zhang, X.; Zhang, J. Tripartite motif-containing 29 as a novel biomarker in non-small cell lung cancer. Oncol. Lett. 2015, 10, 2283–2288. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Zheng, A.; Hydbring, P.; Ambroise, G.; Ouchida, A.T.; Goiny, M.; Vakifahmetoglu-Norberg, H.; Norberg, E. PHGDH Defines a Metabolic Subtype in Lung Adenocarcinomas with Poor Prognosis. Cell Rep. 2017, 19, 2289–2303. [Google Scholar] [CrossRef]
- Zhu, J.; Ma, J.; Wang, X.; Ma, T.; Zhang, S.; Wang, W.; Zhou, X.; Shi, J. High Expression of PHGDH Predicts Poor Prognosis in Non–Small Cell Lung Cancer. Transl. Oncol. 2016, 9, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.-K.; Lei, H.-M.; Liang, Q.; Tang, Y.-B.; Zhou, Y.; Wang, Y.; Zhang, S.; Li, W.-B.; Tong, Y.; Zhuang, G.; et al. Overcoming erlotinib resistance in EGFR mutation-positive lung adenocarcinomas through repression of phosphoglycerate dehydrogenase. Theranostics 2018, 8, 1808–1823. [Google Scholar] [CrossRef]
| MM | PAC (n = 20) | ||||
|---|---|---|---|---|---|
| Total (n = 48) | Epithelioid (n = 23) | Biphasic (n = 13) | Sarcomatoid (n = 12) | ||
| Mean age (range) | 63 (39–83) | 60 (39–80) | 62 (52–73) | 69 (66–83) | 66 (53–78) |
| Male/Female | 44/4 | 19/4 | 13/0 | 12/0 | 14/6 |
| Antibody | Source | Clone | Dilution | Antigen Retrieval |
|---|---|---|---|---|
| PHGDH | abcam | ab57030 | 1:100 | Dako TRS High pH |
| TRIM29 | abcam | ab22207 | 1:50 | Dako TRS High pH |
| Calretinin | Dako | DAK-Calret 1 | 1:50 | Leica BOND ER2 |
| PHGDH Positive Case/n (%) | TRIM29 Positive Case/n (%) | Calretinin Positive Case/n (%) | |
|---|---|---|---|
| MM | 25/48 (52) | 22/48 (46) | 30/48 (63) |
| Epithelioid | 17/23 (74) | 17 */23 (74) | 20/23 (87) |
| Biphasic | 8/13 (62) | 6/13 (46) | 9/13 (69) |
| Sarcomatoid | 0/12 (0) | 0/12 (0) | 1/12 (8) |
| PAC | 1 a/20 (5) | 0/20 (0) | 0/14 (0) |
| PHGDH Positive Case/n (%) | TRIM29 Positive Case/n (%) | |
|---|---|---|
| Lung squamous cell carcinoma | 6/9 (67) | 9/9 (100) |
| Urothelial carcinoma | 7/10 (70) | 9/10 (90) |
| Prostatic adenocarcinoma | 9/10 (90) | 0/10 (0) |
| Clear cell renal cell carcinoma | 0/10 (0) | 0/10 (0) |
| Hepatocellular carcinoma | 2/10 (20) | 3/10 (30) |
| Gastric adenocarcinoma | 2/10 (20) | 3/10 (30) |
| Colon adenocarcinoma | 0/10 (0) | 0/10 (0) |
| Pancreatic duct carcinoma | 2/10 (20) | 3/10 (30) |
| Invasive ductal carcinoma of the breast | ||
| HR- and/or HER2-positive | 5/10 (50) | 1/10 (10) |
| Triple-negative | 5/7 (71) | 2/7 (29) |
| Uterine cervical squamous cell carcinoma | 4/7 (57) | 7/7 (100) |
| Uterine cervical adenocarcinoma | 0/2 (0) | 1/2 (50) |
| Endometrial adenocarcinoma | 8/10 (80) | 2/10 (20) |
| Ovarian adenocarcinoma | 6/10 (60) | 1/10 (10) |
| GIST | 0/5 (0) | 0/5 (0) |
| Gastrointestinal NET | 0/5 (0) | 0/5 (0) |
| Malignant lymphoma | 1/9 (11) | 0/9 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naka, T.; Hatanaka, Y.; Tabata, Y.; Takasawa, A.; Akiyama, H.; Hida, Y.; Okada, H.; Hatanaka, K.C.; Mitsuhashi, T.; Kushitani, K.; et al. Identification of Novel Diagnostic Markers for Malignant Pleural Mesothelioma Using a Reverse Translational Approach Based on a Rare Synchronous Tumor. Diagnostics 2022, 12, 316. https://doi.org/10.3390/diagnostics12020316
Naka T, Hatanaka Y, Tabata Y, Takasawa A, Akiyama H, Hida Y, Okada H, Hatanaka KC, Mitsuhashi T, Kushitani K, et al. Identification of Novel Diagnostic Markers for Malignant Pleural Mesothelioma Using a Reverse Translational Approach Based on a Rare Synchronous Tumor. Diagnostics. 2022; 12(2):316. https://doi.org/10.3390/diagnostics12020316
Chicago/Turabian StyleNaka, Tomoaki, Yutaka Hatanaka, Yukiko Tabata, Akira Takasawa, Hideo Akiyama, Yasuhiro Hida, Hiromi Okada, Kanako C. Hatanaka, Tomoko Mitsuhashi, Kei Kushitani, and et al. 2022. "Identification of Novel Diagnostic Markers for Malignant Pleural Mesothelioma Using a Reverse Translational Approach Based on a Rare Synchronous Tumor" Diagnostics 12, no. 2: 316. https://doi.org/10.3390/diagnostics12020316
APA StyleNaka, T., Hatanaka, Y., Tabata, Y., Takasawa, A., Akiyama, H., Hida, Y., Okada, H., Hatanaka, K. C., Mitsuhashi, T., Kushitani, K., Amatya, V. J., Takeshima, Y., Inai, K., Kaga, K., & Matsuno, Y. (2022). Identification of Novel Diagnostic Markers for Malignant Pleural Mesothelioma Using a Reverse Translational Approach Based on a Rare Synchronous Tumor. Diagnostics, 12(2), 316. https://doi.org/10.3390/diagnostics12020316






