Patient-Reported Experience Measures for Colonoscopy: A Systematic Review and Meta-Ethnography
Abstract
:1. Introduction
2. Materials and Methods
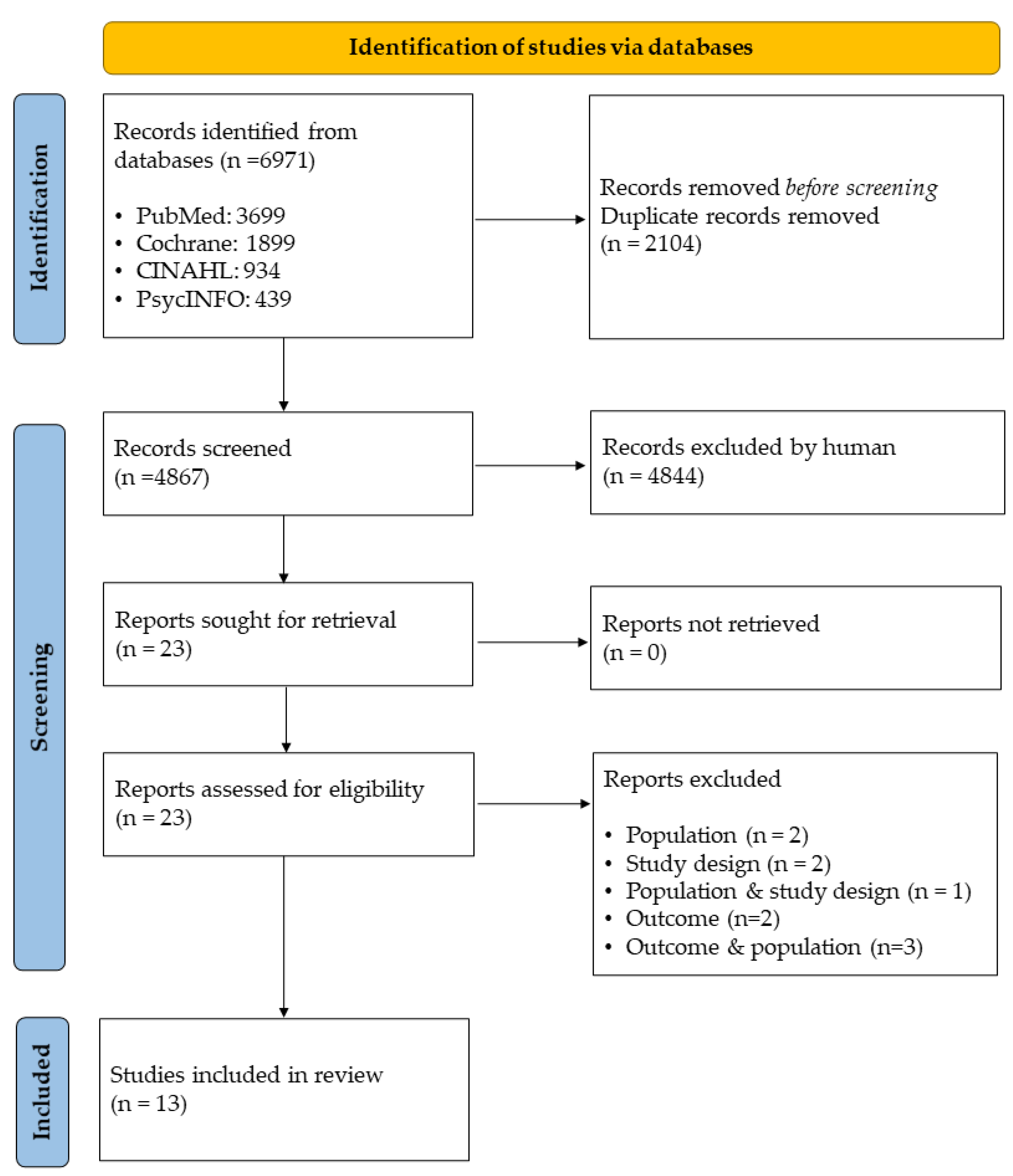
2.1. Search Strategy and Selection Process
2.2. Data Extraction and Analysis
2.3. Inclusion of Instruments
2.4. Triangulation
3. Results
3.1. Meta-Ethnography
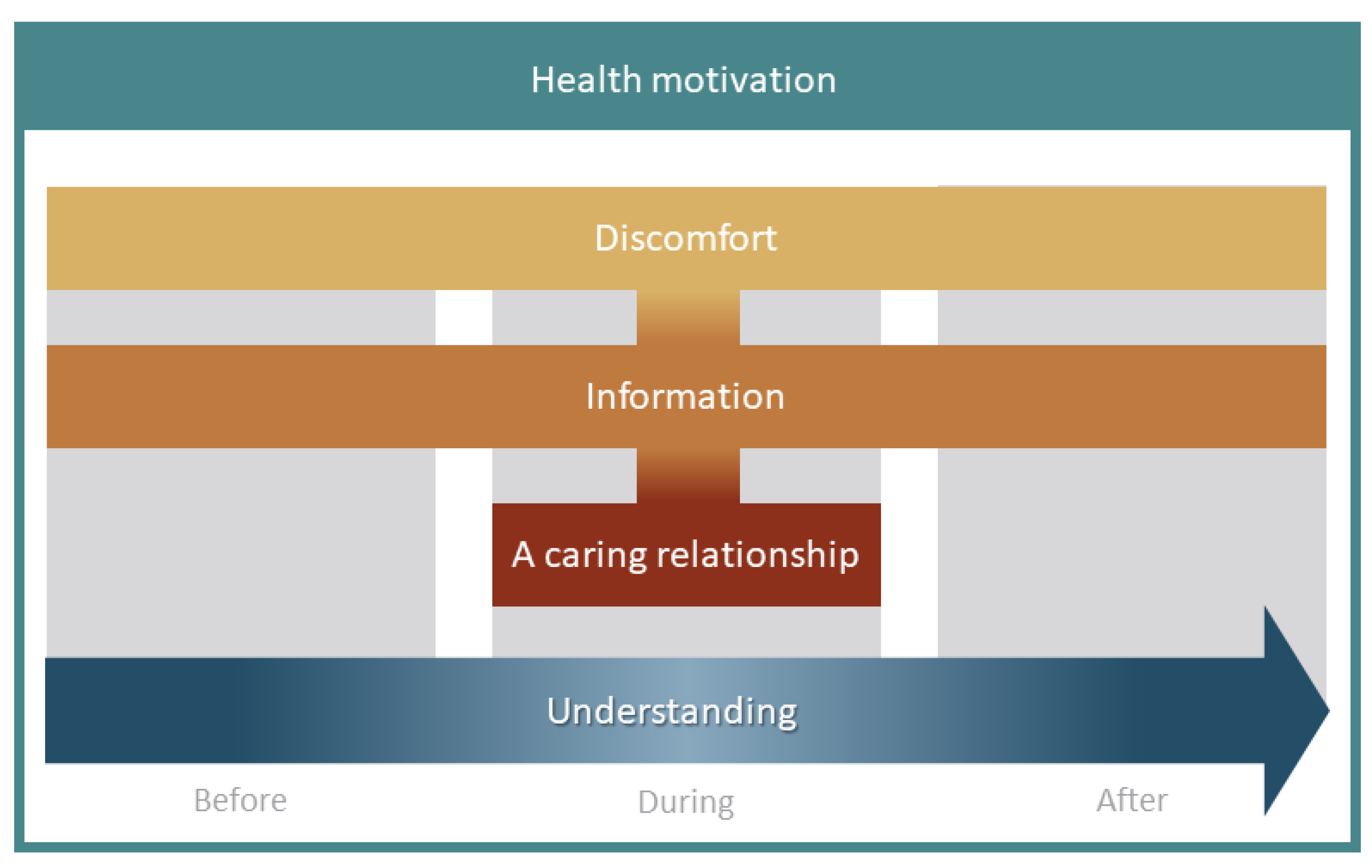
3.1.1. Health Motivation
3.1.2. Discomfort
3.1.3. Information
3.1.4. A Caring Relationship
3.1.5. Understanding
3.1.6. Line of Argument
3.2. Triangulation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Study | Sample | Data Collection | Data Analysis | Setting/Context |
|---|---|---|---|---|
| Hafeez et al., 2012 [33] | 18 patients | Individual interviews | Thematic analysis | United Kingdom |
| 7 female/11 male | Semi-structured | One University Hospital | ||
| Age range 17–65 years | ||||
| Colonic IBD (n = 10) Suspected colonic neoplasia (n = 8) Some had previous experiences of colonoscopy | MR colonoscopy two hours before routine colonoscopy Use of air insufflation | |||
| Kimura et al., 2014 [34] | 13 patients | Focus group interviews | Thematic analysis | United States |
| 6 female/7 male | 2 groups (n = 6/n = 7) | One Community-based Health Centre | ||
| Age range 50–70+ years | ||||
| CRC screening colonoscopy Previous experiences of colonoscopy | ||||
| Kirkegaard et al., 2019 [35] | 22 patients | Individual interviews | Thematic analysis | Denmark |
| 12 female/10 male Age range 58–74 years | Semi-structured | One Regional Screening Provider | ||
| CRC screening colonoscopy | All had experienced a ‘false alarm’ positive FIT | |||
| Previous experience not reported | ||||
| Mikocka-Walus et al., 2012 [36] | 13 patients | Individual interviews | Australia | |
| 7 female/6 male Age range 41–62 years Organic diagnosis 43% Functional diagnosis 57% Had undergone first colonoscopy | 4 interviews 1 week before 1 week after 2 weeks after 12 months after | Thematic analysis | One University Hospital | |
| Neilson et al., 2020 [37] | 10 patients | Individual interviews | Thematic analysis | United Kingdom |
| 5 female/5 male | Semi-structured | One NHS Trust | ||
| Age range 50–70+ years | Report findings regarding experiences of colonoscopy, CT colonography and gastroscopy | |||
| Symptoms or surveillance No CRC screening First-time colonoscopy (n = 6) | ||||
| Restall et al., 2020 [38] | 24 patients | Individual interviews | Qualitative interpretive description methodology | Canada |
| 14 female/10 male | Semi-structured | One Health Region | ||
| Age range 20–69 years | ||||
| Indication not reported First-time colonoscopy (n = 12) | ||||
| Rollbusch et al., 2014 [39] | 16 patients | Individual interviews | Thematic analysis | Australia |
| Sex not reported | Pre-interviews n = 10 Post-interviews n = 6 | One University Hospital | ||
| Age range 26–64 years | ||||
| Indication not reported Some had previous experiences of colonoscopy | ||||
| Rosvall et al., 2021 [32] | 24 patients | Individual interviews | Thematic analysis | Sweden |
| 13 female/11 male | One University Hospital | |||
| Age range 21–83 years | ||||
| Symptoms or surveillance (n = 18) CRC screening (n = 6) All first-time colonoscopy | ||||
| Shamim et al., 2021 [40] | 25 patients | Individual interviews | Inductive content analysis | Denmark |
| 12 female/13 male | Semi-structured 2 interviews 1 h before 1–2 weeks after | Two University Hospitals | ||
| Age range 23–80 years | ||||
| CRC screening (n = 10) Outpatients (n = 15) Previous experience not reported | ||||
| Sultan et al., 2017 [41] | 23 patients | Focus groups interviews | Inductive grounded approach | United States |
| 23 males | 4 groups | One Medical Centre | ||
| Age range 50–85 years | (n = 6/n = 7/n = 5/n = 5) | |||
| Symptoms, surveillance or CRC screening Some had previous experiences of colonoscopy | All patients had multiple chronic conditions | |||
| Thygesen et al., 2019 [42] | 10 patients 3 female/7 male Age range 50–74 years CRC screening colonoscopy Previous experience not reported | Individual interviews Semi-structured | Phenomenological- hermeneutically inspired method | Denmark One cohort study |
| von Wagner et al., 2009 [43] | 18 patients | Individual interviews | Thematic analysis | United Kingdom |
| Sex not reported | Semi-structured | One Centre | ||
| Age not reported | Report finding regarding experiences of colonoscopy, CT colonography and barium enema | |||
| No patients with cancer Previous experience not reported | ||||
| Wangmar et al., 2021 [44] | 29 patients Sex not reported Age range 60–62 years CRC screening colonoscopy Previous experiences of colonoscopy | Focus groups interviews 6 groups (n = 2 to 5) Individual interviews Semi-structured | Inductive content analysis | Sweden Different hospitals across Sweden |
References
- Rees, C.J.; Bevan, R.; Zimmermann-Fraedrich, K.; Rutter, M.D.; Rex, D.; Dekker, E.; Ponchon, T.; Bretthauer, M.; Regula, J.; Saunders, B.; et al. Expert opinions and scientific evidence for colonoscopy key performance indicators. Gut 2016, 65, 2045–2060. [Google Scholar] [CrossRef]
- Rex, D.K.; Petrini, J.L.; Baron, T.H.; Chak, A.; Cohen, J.; Deal, S.E.; Hoffman, B.; Jacobson, B.; Mergener, K.; Petersen, B.T.; et al. Quality indicators for colonoscopy. Gastrointest. Endosc. 2006, 63, S16–S28. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.; Sierra, M.S.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017, 66, 683–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, H.; Demers, A.A.; Xue, L.; Turner, D.; Bernstein, C.N. Time Trends in Colon Cancer Incidence and Distribution and Lower Gastrointestinal Endoscopy Utilization in Manitoba. Am. J. Gastroenterol. 2008, 103, 1249–1256. [Google Scholar] [CrossRef] [PubMed]
- Deding, U.; Valdivia, P.C.; Koulaouzidis, A.; Baatrup, G.; Toth, E.; Spada, C.; Fernández-Urién, I.; Pennazio, M.; Bjørsum-Meyer, T. Patient-Reported Outcomes and Preferences for Colon Capsule Endoscopy and Colonoscopy: A Systematic Review with Meta-Analysis. Diagnostics 2021, 11, 1730. [Google Scholar] [CrossRef]
- Kaminski, M.; Thomas-Gibson, S.; Bugajski, M.; Bretthauer, M.; Rees, C.J.; Dekker, E.; Hoff, G.; Jover, R.; Suchanek, S.; Ferlitsch, M.; et al. Performance measures for lower gastrointestinal endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Laryngo-Rhino-Otologie 2017, 49, 378–397. [Google Scholar] [CrossRef] [Green Version]
- Agency for Healthcare Research and Quality. What is Patient Experience? Available online: https://www.ahrq.gov/cahps/about-cahps/patient-experience/index.html (accessed on 26 April 2021).
- National Institute for Health and Care Excellence. Patient Experience in Adult NHS Services: Improving the Experience of Care for People Using Adult NHS Services—Clinical Guideline; NICE: London, UK, 2012. [Google Scholar]
- Doyle, C.; Lennox, L.; Bell, D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013, 3, e001570. [Google Scholar] [CrossRef] [PubMed]
- Larson, E.; Sharma, J.; Bohren, M.A.; Tunçalp, O. When the patient is the expert: Measuring patient experience and satisfaction with care. Bull. World Health Organ. 2019, 97, 563–569. [Google Scholar] [CrossRef] [PubMed]
- Kingsley, M.B.F.C.; Patel, M.B.F.S. Patient-reported outcome measures and patient-reported experience measures. BJA Educ. 2017, 17, 137–144. [Google Scholar] [CrossRef] [Green Version]
- Brown, S.; Bevan, R.; Rubin, G.; Nixon, C.; Dunn, S.; Panter, S.; Rees, C.J. Patient-derived measures of GI endoscopy: A meta-narrative review of the literature. Gastrointest. Endosc. 2015, 81, 1130–1140. [Google Scholar] [CrossRef] [PubMed]
- Selva, A.; Selva, C.; Álvarez-Pérez, Y.; Torà, N.; López, P.; Terraza-Núñez, R.; Rodríguez, V.; Solà, I.; Burón, A.; Macià, F.; et al. Satisfaction and experience with colorectal cancer screening: A systematic review of validated patient reported outcome measures. BMC Med Res. Methodol. 2021, 21, 230. [Google Scholar] [CrossRef]
- Tierney, M.; Bevan, R.; Rees, C.J.; Trebble, T.M. What do patients want from their endoscopy experience? The importance of measuring and understanding patient attitudes to their care. Front. Gastroenterol. 2016, 7, 191–198. [Google Scholar] [CrossRef] [PubMed]
- McLachlan, S.-A.; Clements, A.; Austoker, J. Patients’ experiences and reported barriers to colonoscopy in the screening context—A systematic review of the literature. Patient Educ. Couns. 2012, 86, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Honein-AbouHaidar, G.N.; Kastner, M.; Vuong, V.; Perrier, L.; Daly, C.; Rabeneck, L.; Straus, S.; Baxter, N.N. Systematic Review and Meta-study Synthesis of Qualitative Studies Evaluating Facilitators and Barriers to Participation in Colorectal Cancer Screening. Cancer Epidemiol. Biomark. Prev. 2016, 25, 907–917. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tan, K.-K.; Lopez, V.; Wong, M.-L.; Koh, G.C.-H. Uncovering the barriers to undergoing screening among first degree relatives of colorectal cancer patients: A review of qualitative literature. J. Gastrointest. Oncol. 2018, 9, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Decruz, G.M.; Ng, C.H.; Lim, K.T.; Devi, M.K.; Lim, F.; Tai, C.H.; Chong, C.S. Afterthoughts on colonoscopy. Was it that bad? J. Med Screen. 2020, 21, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.T.; Ng, C.H.; Decruz, G.M.; Lim, T.Z.; Devi, K.; Tan, K.-K.; Chong, C.S. Barriers and facilitators towards colonoscopy: A qualitative systematic review. Eur. J. Cancer Prev. 2020, 30, 232–238. [Google Scholar] [CrossRef]
- Kerrison, R.S.; Sheik-Mohamud, D.; McBride, E.; Whitaker, K.L.; Rees, C.; Duffy, S.; von Wagner, C. Patient barriers and facilitators of colonoscopy use: A rapid systematic review and thematic synthesis of the qualitative literature. Prev. Med. 2021, 145, 106413. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health. Guidance for industry: Patient-reported outcome measures: Use in medical product development to support labeling claims: Draft guidance. Health Qual. Life Outcomes 2006, 4, 1–79. [Google Scholar] [CrossRef] [Green Version]
- Noblit, G.W.; Hare, R.D. Meta-Ethnography: Synthesizing Qualitative Studies; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 1988. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Britten, N.; Campbell, R.; Pope, C.; Donovan, J.; Morgan, M.; Pill, R. Using meta ethnography to synthesise qualitative research: A worked example. J. Health Serv. Res. Policy 2002, 7, 209–215. [Google Scholar] [CrossRef] [PubMed]
- France, E.F.; Cunningham, M.; Ring, N.; Uny, I.; Duncan, E.A.; Jepson, R.G.; Maxwell, M.; Roberts, R.J.; Turley, R.L.; Booth, A.; et al. Improving reporting of meta-ethnography: The eMERG e reporting guidance. J. Adv. Nurs. 2019, 75, 1126–1139. [Google Scholar] [CrossRef] [PubMed]
- Farmer, T.; Robinson, K.; Elliott, S.J.; Eyles, J.; Farmer, T.; Robinson, K.; Elliott, S.J.; Eyles, J. Developing and Implementing a Triangulation Protocol for Qualitative Health Research. Qual. Health Res. 2006, 16, 377–394. [Google Scholar] [CrossRef]
- Bettany-Saltikov, J.; McSherry, R. How to Do a Systematic Literature Review in Nursing. A Step-by-Step Guide, 2nd ed.; Open University Press: Maidenhead, UK, 2016. [Google Scholar]
- Bramer, W.M.; Giustini, D.; De Jonge, G.B.; Holland, L.; Bekhuis, T. De-duplication of database search results for systematic reviews in EndNote. J. Med Libr. Assoc. 2016, 104, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Critical Appraisal Skills Programme. CASP-Qualitative-Checklist. 2018. Available online: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf (accessed on 30 March 2021).
- SBU. Evaluation and Synthesis of Studies Using Qualitative Methods of Analysis; Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU): Stockholm, Sweden, 2016. [Google Scholar]
- Rosvall, A.; Axelsson, M.; Toth, E.; Kumlien, C.; Gershater, M.A. Patients’ Experiences Before, During, and After a Colonoscopy Procedure. A Qualitative Study. Gastroenterol. Nurs. 2021, 44, 392–402. [Google Scholar] [CrossRef] [PubMed]
- Hafeez, R.; Wagner, C.V.; Smith, S.; Boulos, P.; Halligan, S.; Bloom, S.; Taylor, S.A. Patient experiences of MR colonography and colonoscopy: A qualitative study. Br. J. Radiol. 2012, 85, 765–769. [Google Scholar] [CrossRef] [Green Version]
- Kimura, A.; Sin, M.-K.; Spigner, C.; Tran, A.; Tu, S.-P. Barriers and Facilitators to Colorectal Cancer Screening in Vietnamese Americans: A Qualitative Analysis. J. Cancer Educ. 2014, 29, 728–734. [Google Scholar] [CrossRef] [Green Version]
- Kirkegaard, P.; Edwards, A.; Andersen, B. A stitch in time saves nine: Perceptions about colorectal cancer screening after a non-cancer colonoscopy result. Qualitative study. Patient Educ. Couns. 2019, 102, 1373–1379. [Google Scholar] [CrossRef]
- Mikocka-Walus, A.A.; Moulds, L.; Rollbusch, N.; Andrews, J.M. “It’s a Tube Up Your Bottom; It Makes People Nervous”. The experience of anxiety in initial colonoscopy patients. Gastroenterol. Nurs. 2012, 35, 392–401. [Google Scholar] [CrossRef]
- Neilson, L.J.; Patterson, J.; Von Wagner, C.; Hewitson, P.; McGregor, L.M.; Sharp, L.; Rees, C.J. Patient experience of gastrointestinal endoscopy: Informing the development of the Newcastle ENDOPREM™. Front. Gastroenterol. 2020, 11, 209–217. [Google Scholar] [CrossRef]
- Restall, G.; Michaud, V.; Walker, J.R.; Waldman, C.; Bernstein, C.N.; Park, J.; Wittmeier, K.; Singh, H. Patient Experiences with Colonoscopy: A Qualitative Study. J. Can. Assoc. Gastroenterol. 2019, 3, 249–256. [Google Scholar] [CrossRef]
- Rollbusch, N.; Mikocka-Walus, A.A.; Andrews, J.M. The Experience of Anxiety in Colonoscopy Outpatients: A mixed-method study. Gastroenterol. Nurs. 2014, 37, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Shamim, S.; Andresen, Y.L.M.; Thaysen, H.V.; Jakobsen, I.H.; Nielsen, J.; Danielsen, A.K.; Konradsen, H. Experiences of Patients Undergoing Bowel Preparation and Colonoscopy: A Qualitative Longitudinal Study. J. Multidiscip. Health 2021, 14, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Sultan, S.; Partin, M.R.; Shah, P.; LeLaurin, J.; Freytes, I.M.; Nightingale, C.L.; Fesperman, S.F.; Curbow, B.A.; Beyth, R.J. Barriers and facilitators associated with colonoscopy completion in individuals with multiple chronic conditions: A qualitative study. Patient Prefer. Adherence 2017, 11, 985–994. [Google Scholar] [CrossRef] [Green Version]
- Thygesen, M.K.; Baatrup, G.; Petersen, C.; Qvist, N.; Krøijer, R.; Kobaek-Larsen, M. Screening individuals’ experiences of colonoscopy and colon capsule endoscopy; a mixed methods study. Acta Oncol. 2019, 58, S71–S76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Wagner, C.; Knight, K.; Halligan, S.; Atkin, W.; Lilford, R.; Morton, D.; Wardle, J. Patient experiences of colonoscopy, barium enema and CT colonography: A qualitative study. Br. J. Radiol. 2009, 82, 13–19. [Google Scholar] [CrossRef]
- Johanna, W.; Yvonne, W.; Anna, J.; Kaisa, F. Two sides of every coin: Individuals’ experiences of undergoing colorectal cancer screening by faecal immunochemical test and colonoscopy. Eur. J. Public Health 2021, 31, 1290–1295. [Google Scholar] [CrossRef] [PubMed]
- Lin, O.S.; Schembre, D.B.; Ayub, K.; Gluck, M.; McCormick, S.E.; Patterson, D.J.; Cantone, N.; Soon, M.-S.; Kozarek, R.A. Patient satisfaction scores for endoscopic procedures: Impact of a survey-collection method. Gastrointest. Endosc. 2007, 65, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Joint Advisory Group on GI Endoscopy. Global Rating Scale (GRS) for UK Services. Available online: https://www.thejag.org.uk/AboutUs/DownloadCentre.aspx?PageId=134 (accessed on 16 January 2022).
- Ko, H.H.; Zhang, H.; Telford, J.J.; Enns, R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest. Endosc. 2009, 69, 883–891. [Google Scholar] [CrossRef]
- Scotto, F.; De Ceglie, A.; Guerra, V.; Misciagna, G.; Pellecchia, A. Determinants of patient satisfaction survey in a gastrointestinal endoscopy service. Clin. Governance: Int. J. 2009, 14, 86–97. [Google Scholar] [CrossRef]
- Ghanouni, A.; Plumb, A.; Hewitson, P.; Nickerson, C.; Rees, C.J.; Von Wagner, C. Patients’ experience of colonoscopy in the English Bowel Cancer Screening Programme. Laryngo-Rhino-Otologie 2016, 48, 232–240. [Google Scholar] [CrossRef]
- Brotons, A.; Guilabert, M.; Lacueva, F.J.; Mira, J.J.; Lumbreras, B.; Picó, M.D.; Vitaller, J.; García-Sepulcre, M.F.; Belda, G.; Sola-Vera, J. The Colonoscopy Satisfaction and Safety Questionnaire (CSSQP) for Colorectal Cancer Screening: A Development and Validation Study. Int. J. Environ. Res. Public Health 2019, 16, 392. [Google Scholar] [CrossRef] [Green Version]
- Hoff, G.; Bretthauer, M.; Huppertz-Hauss, G.; Kittang, E.; Stallemo, A.; Høie, O.; Dahler, S.; Nyhus, S.; Halvorsen, F.-A.; Pallenschat, J.; et al. The Norwegian Gastronet project: Continuous quality improvement of colonoscopy in 14 Norwegian centres. Scand. J. Gastroenterol. 2006, 41, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Hutchings, H.A.; Cheung, W.-Y.; Alrubaiy, L.; Durai, D.; Russell, I.T.; Williams, J.G. Development and validation of the Gastrointestinal Endoscopy Satisfaction Questionnaire (GESQ). Endosc. 2015, 47, 1137–1143. [Google Scholar] [CrossRef] [Green Version]
- Steffenssen, M.W.; Al-Najami, I.; Baatrup, G. Patient-reported minor adverse events after colonoscopy: A systematic review. Acta Oncol. 2019, 58, S22–S28. [Google Scholar] [CrossRef] [Green Version]
- Sheng, L.-P.; Han, C.-Q.; Nie, C.; Xu, T.; Zhang, K.; Li, X.-J.; Xie, X.-R.; Lin, R.; Ding, Z. Watching Videos of Colonoscopies and Receiving Interpretations Reduce Pain and Anxiety While Increasing the Satisfaction of Patients. Dig. Dis. Sci. 2021, 66, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Bechtold, M.L.; Puli, S.R.; Othman, M.O.; Bartalos, C.R.; Marshall, J.B.; Roy, P.K. Effect of Music on Patients Undergoing Colonoscopy: A Meta-Analysis of Randomized Controlled Trials. Dig. Dis. Sci. 2009, 54, 19–24. [Google Scholar] [CrossRef]
- Morgan, J.; Roufeil, L.; Kaushik, S.; Bassett, M. Influence of coping style and precolonoscopy information on pain and anxiety of colonoscopy. Gastrointest. Endosc. 1998, 48, 119–127. [Google Scholar] [CrossRef]
- Hsu, Y.-H.; Lin, F.-S.; Yang, C.-C.; Lin, C.-P.; Hua, M.-S.; Sun, W.-Z. Evident cognitive impairments in seemingly recovered patients after midazolam-based light sedation during diagnostic endoscopy. J. Formos. Med Assoc. 2015, 114, 489–497. [Google Scholar] [CrossRef] [Green Version]
- Nilsson, M.; From, I.; Lindwall, L. The significance of patient participation in nursing care—A concept analysis. Scand. J. Caring Sci. 2019, 33, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Dubois, H.; Creutzfeldt, J.; Törnqvist, M.; Bergenmar, M. Patient participation in gastrointestinal endoscopy—From patients’ perspectives. Health Expect. 2020, 23, 893–903. [Google Scholar] [CrossRef] [PubMed]
- Hatoum, H.T.; Lin, S.-J.; Joseph, R.E.; Dahdal, D.N. Validation of a Patient Satisfaction Scale in Patients Undergoing Bowel Preparation Prior to Colonoscopy. Patient 2016, 9, 27–34. [Google Scholar] [CrossRef] [Green Version]
- Telford, J.; Tavakoli, I.; Takach, O.; Kwok, R.; Harris, N.; Yonge, J.; Galorpart, C.; Whittaker, S.; Amar, J.; Rosenfeld, G.; et al. Validation of the St. Paul’s Endoscopy Comfort Scale (SPECS) for Colonoscopy. J. Can. Assoc. Gastroenterol. 2020, 3, 91–95. [Google Scholar] [CrossRef]
- Mitchell, K.A.; Rawl, S.; Champion, V.; Jeffries, P.R.; Welch, J.L. Development and Psychometric Testing of the Colonoscopy Embarrassment Scale. West. J. Nurs. Res. 2021, 34, 548–564. [Google Scholar] [CrossRef] [PubMed]
- Rostom, A.; Ross, E.D.; Dubé, C.; Rutter, M.D.; Lee, T.; Valori, R.; Bridges, R.J.; Pontifex, D.; Webbink, V.; Rees, C.; et al. Development and validation of a nurse-assessed patient comfort score for colonoscopy. Gastrointest. Endosc. 2013, 77, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Peng, W.; Huang, Q.; Lun, D.; Carcioppolo, N. The Development and Validation of the Colonoscopy Joking Scale. Health Commun. 2020, 16–19. [Google Scholar] [CrossRef] [PubMed]
| Population | Exposure | Outcome |
|---|---|---|
| Adult patients who have undergone a colonoscopy | A colonoscopy | The patients’ experiences of the colonoscopy |
| Study | Sample | Data Collection | Data Analysis | Setting | Quality 1 |
|---|---|---|---|---|---|
| Hafeez et al., 2012 [33] | 18 patients | Individual interviews | Thematic analysis | United Kingdom | Moderate |
| Kimura et al., 2014 [34] | 13 patients | Focus group interviews | Thematic analysis | United States | Moderate |
| Kirkegaard et al., 2019 [35] | 22 patients | Individual interviews | Thematic analysis | Denmark | High |
| Mikocka-Walus et al., 2012 [36] | 13 patients | Individual interviews | Thematic analysis | Australia | High |
| Neilson et al., 2020 [37] | 10 patients | Individual interviews | Thematic analysis | United Kingdom | Moderate |
| Restall et al., 2020 [38] | 24 patients | Individual interviews | Qualitative interpretive description methodology | Canada | High |
| Rollbusch et al., 2014 [39] | 16 patients | Individual interviews | Thematic analysis | Australia | High |
| Rosvall et al., 2021 [32] | 24 patients | Individual interviews | Thematic analysis | Sweden | High |
| Shamim et al., 2021 [40] | 25 patients | Individual interviews | Inductive content analysis | Denmark | High |
| Sultan et al., 2017 [41] | 23 patients | Focus groups interviews | Inductive grounded approach | United States | High |
| Thygesen et al., 2019 [42] | 10 patients | Individual interviews | Phenomenological- hermeneutical method | Denmark | Moderate |
| von Wagner et al., 2009 [43] | 18 patients | Individual interviews | Thematic analysis | United Kingdom | Moderate |
| Wangmar et al., 2021 [44] | 29 patients | Focus groups interviews Individual interviews | Inductive content analysis | Sweden | High |
| Instruments | Health Motivation n = 10 | Discomfort n = 12 | Information n = 10 | A Caring Relationship n = 10 | Understanding n = 8 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | Before | During | After | Before | During | After | Before | During | After | Before | During | After | |
| CSSQP [50] | − | − | + | − | + | + | + | − | + | − | − | − | − |
| Colonoscopy Questionnaire BCSP-NHS [49] | − | − | + | + | + | − | + | − | + | − | + | − | − |
| Gastronet [51] | − | − | + | − | +/− | − | + | − | + | − | − | − | − |
| GESQ [52] | − | − | + | − | + | − | + | − | + | − | − | − | − |
| GI Procedure Patient Satisfaction Survey [45] | − | + | + | + | + | − | + | − | + | − | − | − | − |
| Global Rating Scale (GRS) 1 [46] | − | − | + | − | + | +/− | + | − | + | − | − | − | − |
| mGHAA-9 [47] | − | − | + | − | + | − | + | − | + | − | + | − | + |
| Patient satisfaction questionnaire [48] | − | − | − | − | + | + | + | − | + | − | + | − | − |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosvall, A.; Annersten Gershater, M.; Kumlien, C.; Toth, E.; Axelsson, M. Patient-Reported Experience Measures for Colonoscopy: A Systematic Review and Meta-Ethnography. Diagnostics 2022, 12, 242. https://doi.org/10.3390/diagnostics12020242
Rosvall A, Annersten Gershater M, Kumlien C, Toth E, Axelsson M. Patient-Reported Experience Measures for Colonoscopy: A Systematic Review and Meta-Ethnography. Diagnostics. 2022; 12(2):242. https://doi.org/10.3390/diagnostics12020242
Chicago/Turabian StyleRosvall, Annica, Magdalena Annersten Gershater, Christine Kumlien, Ervin Toth, and Malin Axelsson. 2022. "Patient-Reported Experience Measures for Colonoscopy: A Systematic Review and Meta-Ethnography" Diagnostics 12, no. 2: 242. https://doi.org/10.3390/diagnostics12020242
APA StyleRosvall, A., Annersten Gershater, M., Kumlien, C., Toth, E., & Axelsson, M. (2022). Patient-Reported Experience Measures for Colonoscopy: A Systematic Review and Meta-Ethnography. Diagnostics, 12(2), 242. https://doi.org/10.3390/diagnostics12020242







