The Role of Active or Passive Drainage after Evacuation of Chronic Subdural Hematoma: An Analysis of Two Randomized Controlled Trials (cSDH-Drain-Trial and TOSCAN Trial)
Abstract
:1. Introduction
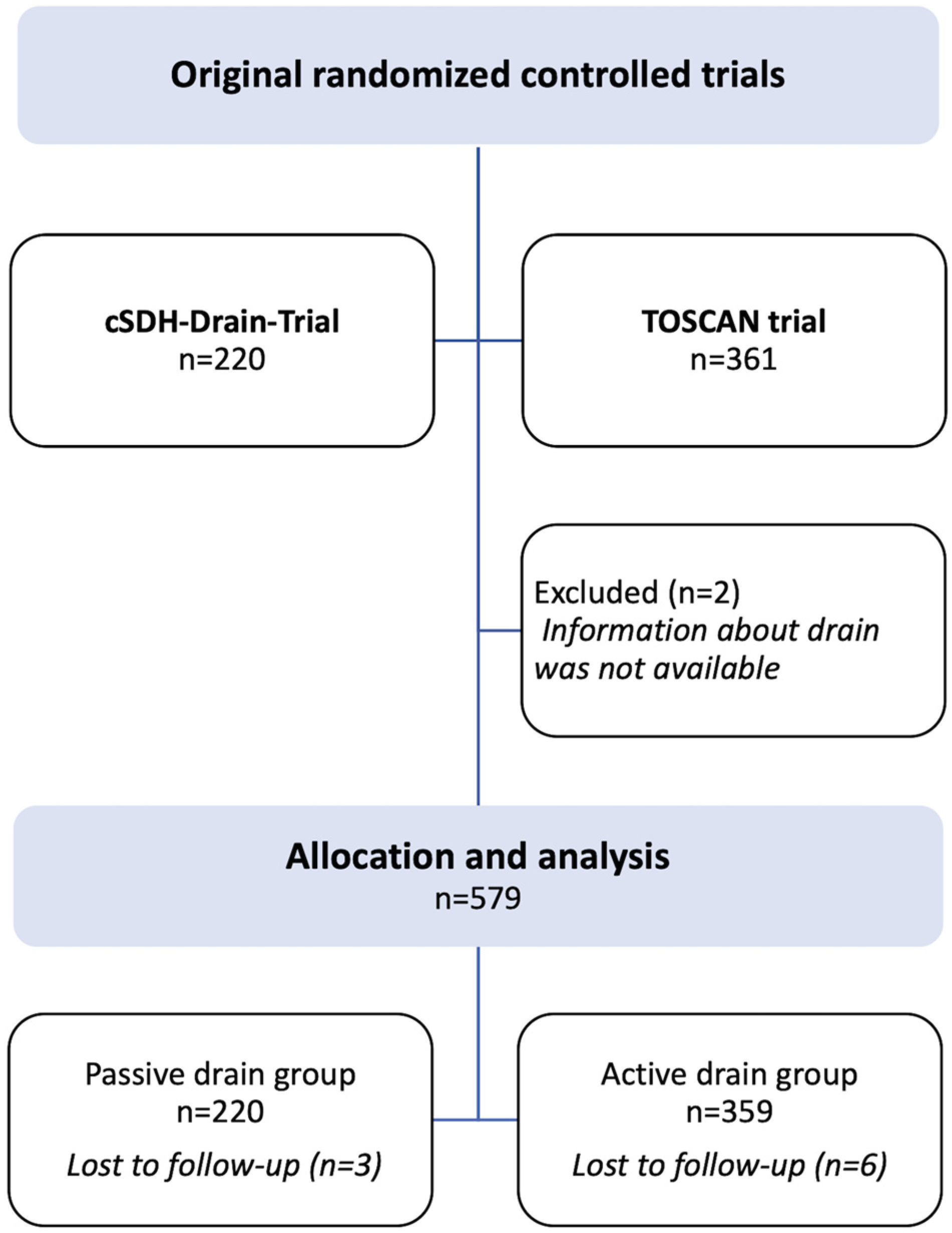
2. Materials and Methods
2.1. Patient Population
2.2. Surgical and Postoperative Management
2.3. Primary and Secondary Endpoints
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Primary and Secondary Outcomes
3.3. Risk Factors for Recurrence
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, W.; Huang, J. Chronic Subdural Hematoma: Epidemiology and Natural History. Neurosurg. Clin. N. Am. 2017, 28, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Balser, D.; Farooq, S.; Mehmood, T.; Reyes, M.; Samadani, U. Actual and projected incidence rates for chronic subdural hematomas in United States Veterans Administration and civilian populations. J. Neurosurg. 2015, 123, 1209–1215. [Google Scholar] [CrossRef] [Green Version]
- Weigel, R.; Schmiedek, P.; Krauss, J.K. Outcome of contemporary surgery for chronic subdural haematoma: Evidence based review. J. Neurol. Neurosurg. Psychiatry 2003, 74, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Santarius, T.; Kirkpatrick, P.J.; Ganesan, D.; Chia, H.L.; Jalloh, I.; Smielewski, P.; Richards, H.K.; Marcus, H.; Parker, R.A.; Price, S.J.; et al. Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: A randomised controlled trial. Lancet 2009, 374, 1067–1073. [Google Scholar] [CrossRef] [PubMed]
- Soleman, J.; Lutz, K.; Schaedelin, S.; Kamenova, M.; Guzman, R.; Mariani, L.; Fandino, J. Subperiosteal vs Subdural Drain After Burr-Hole Drainage of Chronic Subdural Hematoma: A Randomized Clinical Trial (cSDH-Drain-Trial). Neurosurgery 2019, 85, E825–E834. [Google Scholar] [CrossRef] [PubMed]
- Gazzeri, R.; Galarza, M.; Neroni, M.; Canova, A.; Refice, G.M.; Esposito, S. Continuous subgaleal suction drainage for the treatment of chronic subdural haematoma. Acta Neurochir. 2007, 149, 487–493. [Google Scholar] [CrossRef] [PubMed]
- Ram, Z.; Hadani, M.; Sahar, A.; Spiegelmann, R. Continuous irrigation-drainage of the subdural space for the treatment of chronic subdural haematoma. A prospective clinical trial. Acta Neurochir. 1993, 120, 40–43. [Google Scholar] [CrossRef]
- Sjåvik, K.; Bartek, J.; Sagberg, L.M.; Henriksen, M.L.; Gulati, S.; Ståhl, F.; Kristiansson, H.; Solheim, O.; Förander, P.; Jakola, A. Assessment of drainage techniques for evacuation of chronic subdural hematoma: A consecutive population-based comparative cohort study. J. Neurosurg. 2020, 133, 1113–1119. [Google Scholar] [CrossRef] [Green Version]
- Kurabe, S.; Ozawa, T.; Watanabe, T.; Aiba, T. Efficacy and safety of postoperative early mobilization for chronic subdural hematoma in elderly patients. Acta Neurochir. 2010, 152, 1171–1174. [Google Scholar] [CrossRef]
- Nakajima, H.; Yasui, T.; Nishikawa, M.; Kishi, H.; Kan, M. The role of postoperative patient posture in the recurrence of chronic subdural hematoma: A prospective randomized trial. Surg. Neurol. 2002, 58, 385–387. [Google Scholar] [CrossRef]
- Abouzari, M.; Rashidi, A.; Rezaii, J.; Esfandiari, K.; Asadollahi, M.; Aleali, H.; Abdollahzadeh, M. The Role of Postoperative Patient Posture in The Recurrence of Traumatic Chronic Subdural Hematoma after Burr-Hole Surgery. Neurosurgery 2007, 61, 794–797. [Google Scholar] [CrossRef] [PubMed]
- Adeolu, A.A.; Rabiu, T.B.; Adeleye, A.O. Post-operative day two versus day seven mobilization after burr-hole drainage of subacute and chronic subdural haematoma in Nigerians. Br. J. Neurosurg. 2012, 26, 743–746. [Google Scholar] [CrossRef] [PubMed]
- Kale, A.; Öz, I.I.; Gün, E.G.; Kalaycı, M.; Gül, Ş. Is the recurrence rate of chronic subdural hematomas dependent on the duration of drainage? Neurol. Res. 2017, 39, 399–402. [Google Scholar] [CrossRef] [PubMed]
- Soleman, J.; Lutz, K.; Schaedelin, S.; Mariani, L.; Fandino, J.; Brand, E.; Kaliaperumal, C. Use of Subperiosteal Drain Versus Subdural Drain in Chronic Subdural Hematomas Treated with Burr-Hole Trepanation: Study Protocol for a Randomized Controlled Trial. JMIR Res. Protoc. 2016, 5, e38. [Google Scholar] [CrossRef] [PubMed]
- Schucht, P.; Fischer, U.; Fung, C.; Bernasconi, C.; Fichtner, J.; Vulcu, S.; Schöni, D.; Nowacki, A.; Wanderer, S.; Eisenring, C.; et al. Follow-up Computed Tomography after Evacuation of Chronic Subdural Hematoma. N. Engl. J. Med. 2019, 380, 1186–1187. [Google Scholar] [CrossRef]
- Baschera, D.; Tosic, L.; Westermann, L.; Oberle, J.; Alfieri, A. Treatment Standards for Chronic Subdural Hematoma: Results from a Survey in Austrian, German, and Swiss Neurosurgical Units. World Neurosurg. 2018, 116, e983–e995. [Google Scholar] [CrossRef] [PubMed]
- Häni, L.; Vulcu, S.; Branca, M.; Fung, C.; Z’Graggen, W.J.; Murek, M.; Raabe, A.; Beck, J.; Schucht, P. Subdural versus subgaleal drainage for chronic subdural hematomas: A post hoc analysis of the TOSCAN trial. J. Neurosurg. 2019, 133, 1147–1155. [Google Scholar] [CrossRef]
- Mehta, V.; Harward, S.C.; Sankey, E.W.; Nayar, G.; Codd, P.J. Evidence based diagnosis and management of chronic subdural hematoma: A review of the literature. J. Clin. Neurosci. 2018, 50, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Lewis, A.; Sen, R.; Hill, T.C.; James, H.; Lin, J.; Bhamra, H.; Martirosyan, N.; Pacione, D. Antibiotic prophylaxis for subdural and subgaleal drains. J. Neurosurg. 2017, 126, 908–912. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Surgical Site Infection Prevention Guidelines Web Appendix 26: Advanced Dressing; World Health Organization: Geneva, Switzerland, 2016; pp. 1–67. [Google Scholar]
- Brennan, P.M.; Kolias, A.G.; Joannides, A.J.; Shapey, J.; Marcus, H.J.; Gregson, B.A.; Grover, P.J.; Hutchinson, P.J.; Coulter, I.C. Coulter, The management and outcome for patients with chronic subdural hematoma: A prospective, multicenter, observational cohort study in the United Kingdom. J. Neurosurg. 2017, 127, 732–739. [Google Scholar] [CrossRef]
- Soleman, J.; Kamenova, M.; Lutz, K.; Guzman, R.; Fandino, J.; Mariani, L. Drain Insertion in Chronic Subdural Hematoma: An International Survey of Practice. World Neurosurg. 2017, 104, 528–536. [Google Scholar] [CrossRef] [PubMed]
- Glancz, L.J.; Poon, M.T.C.; Coulter, I.C.; Hutchinson, P.J.; Kolias, A.G.; Brennan, P.M. Does Drain Position and Duration Influence Outcomes in Patients Undergoing Burr-Hole Evacuation of Chronic Subdural Hematoma? Lessons from a UK Multicenter Prospective Cohort Study. Neurosurgery 2019, 85, 486–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jensen, T.S.R.; Haldrup, M.; Grønhøj, M.H.; Miscov, R.; Larsen, C.C.; Debrabant, B.; Poulsen, F.R.; Bergholt, B.; Hundsholt, T.; Bjarkam, C.R.; et al. National randomized clinical trial on subdural drainage time after chronic subdural hematoma evacuation. J. Neurosurg. 2021, 137, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Soleman, J.; Taussky, P.; Fandino, J.; Muroi, C. Evidence-Based Treatment of Chronic Subdural Hematoma. Trauma. Brain Inj. 2014, 12, 249–281. [Google Scholar] [CrossRef]


| Drain Group | Passive | Active | p-Value |
|---|---|---|---|
| n | 220 | 359 | |
| Sex = male (%) | 149 (67.7) | 243 (67.7) | 1 |
| Age (mean ±SD) | 77.25 (10.06) | 73.46 (11.07) | <0.001 |
| Drain type (%) | 0.13 | ||
| subdural | 100 (45.5) | 135 (37.6) | |
| subperiosteal | 120 (54.5) | 214 (59.6) | |
| Mobilization for 48 h (%) | <0.001 | ||
| Bed rest, flat | 220 (100.0) | 8 (2.3) | |
| Bed rest, 30° | 0 (0.0) | 54 (15.3) | |
| Partial mobilization | 0 (0.0) | 122 (33.9) | |
| Full mobilization | 0 (0.0) | 169 (47.1) | |
| Drain duration (mean ±SD), hours | 48.00 (0.00) | 34.60 (11.58) | <0.001 |
| GCS at presentation (median [IQR]) | 15.00 [14.00, 15.00] | 15.00 [15.00, 15.00] | <0.001 |
| GCS at presentation grouped (%) | <0.001 | ||
| good | 179 (81.4) | 333 (92.8) | |
| moderate | 35 (15.9) | 24 (6.7) | |
| bad | 6 (2.7) | 2 (0.6) | |
| mRS at presentation (median [IQR]) | 2.00 [1.00, 3.00] | 1.00 [1.00, 2.00] | <0.001 |
| mRS at presentation grouped = good (%) | 169 (76.8) | 334 (93.0) | <0.001 |
| MLS preoperative (mean ±SD), cm | 0.73 (0.52) | 0.74 (0.50) | 0.871 |
| Aphasia = yes (%) | 47 (21.4) | 80 (22.3) | 0.876 |
| Motor deficit = yes (%) | 108 (49.1) | 105 (29.2) | <0.001 |
| Headache = yes (%) | 67 (30.6) | 222 (61.8) | <0.001 |
| Urinary incontinence = yes (%) | 6 (2.7) | 10 (2.8) | 1 |
| Seizure = yes (%) | 12 (5.5) | 13 (3.6) | 0.399 |
| Hypertension = yes (%) | 30 (13.6) | 57 (15.9) | 0.54 |
| Diabetes mellitus = yes (%) | 30 (13.6) | 54 (15.5) | 0.631 |
| CAD = yes (%) | 63 (28.6) | 98 (27.3) | 0.8 |
| Atrial fibrillation = yes (%) | 46 (20.9) | 91 (25.3) | 0.263 |
| Stroke = yes (%) | 27 (12.3) | 26 (7.2) | 0.059 |
| COPD = yes (%) | 5 (2.3) | 12 (3.3) | 0.627 |
| Smoking = yes (%) | 8 (3.6) | 18 (5.0) | 0.569 |
| Alcohol = yes (%) | 13 (5.9) | 13 (3.6) | 0.279 |
| DVT = yes (%) | 8 (3.6) | 21 (6.0) | 0.288 |
| Blood thinner = yes (%) | 133 (60.5) | 191 (53.2) | 0.105 |
| Drain Group | Passive | Active | p-Value |
|---|---|---|---|
| n | 220 | 359 | |
| Recurrence = yes (%) | 31 (14.1) | 83 (23.1) | 0.011 |
| Time to recurrence (mean ±SD), days | 21.16 (24.99) | 23.41 (25.58) | 0.228 |
| GCS after 24–48 h (median [IQR]) | 15.00 [14.00, 15.00] | 15.00 [15.00, 15.00] | <0.001 |
| GCS grouped after 24–48 h (%) | <0.001 | ||
| good | 195 (88.6) | 357 (99.7) | |
| moderate | 22 (10.0) | 1 (0.3) | |
| bad | 3 (1.4) | 0 (0.0) | |
| GCS after 4–6 weeks (median [IQR]) | 15.00 [15.00, 15.00] | 15.00 [15.00, 15.00] | <0.001 |
| GCS grouped after 4–6 weeks (%) | 0.256 | ||
| good | 197 (97.5) | 327 (99.7) | |
| moderate | 4 (2.0) | 1 (0.3) | |
| bad | 1 (0.5) | 0 (0) | |
| mRS after 4–6 weeks (median [IQR]) | 1.00 [0.00, 2.00] | 1.00 [0.50, 2.00] | 0.261 |
| mRS grouped after 4–6 weeks (%) | 0.087 | ||
| good | 184 (88.0) | 322 (93.3) | |
| bad | 18 (8.6) | 15 (4.3) | |
| GCS after 6–12 months (median [IQR]) | 15.00 [15.00, 15.00] | 15.00 [15.00, 15.00] | 0.019 |
| GCS grouped after 6–12 months | 0.256 | ||
| good | 171 (98.3) | 316 (99.7) | |
| moderate | 3 (1.7) | 1 (0.3) | |
| mRS after 6–12 months (median [IQR]) | 1.00 [0.00, 3.00] | 1.00 [0.00, 1.00] | 0.018 |
| mRS grouped after 6–12 months (%) | 0.008 | ||
| good | 160 (81.6) | 316 (90.8) | |
| bad | 14 (7.1) | 12 (3.4) | |
| Diameter of remaining hematoma after 24–48 h (mean ±SD) cm | 1.05 (0.54) | 1.17 (0.56) | 0.029 |
| Diameter of remaining hematoma after 4–6 weeks (mean ±SD), cm | 0.56 (0.57) | 0.72 (0.59) | 0.007 |
| MLS 24–48 h postoperative (mean ±SD), cm | 0.34 (0.28) | 0.34 (0.32) | 0.893 |
| MLS 4–6 weeks postoperative (mean ±SD), cm | 0.09 (0.19) | 0.16 (0.31) | 0.005 |
| Hemorrhagic complications = yes (%) | 5 (2.3) | 6 (1.7) | 0.877 |
| Hemorrhage type (%) | 0.424 | ||
| EDH | 1 (0.5) | 0 (0.0) | |
| ICB | 4 (1.8) | 6 (1.7) | |
| Surgical infections = yes (%) | 11 (5) | 6 (1.7) | 0.047 |
| Medical complication (%) | 0.440 | ||
| DVT | 2 (0.9) | 2 (0.6) | |
| PE | 2 (0.9) | 2 (0.6) | |
| Pneumonia | 3 (1.4) | 1 (0.3) | |
| Mortality = yes (%) | 12 (5.5) | 20 (5.6) | 0.968 |
| Mortality, surgery related = yes (%) | 5 (2.3) | 0 (0.0) | 0.073 |
| Recurrence | No | Yes | p-Value |
|---|---|---|---|
| n | 465 | 114 | |
| Suction = yes (%) | 276 (59.4) | 83 (72.8) | 0.011 |
| Sex = male (%) | 311 (66.9) | 81 (71.1) | 0.458 |
| Age (mean ±SD), years | 74.80 (10.83) | 75.29 (10.96) | 0.669 |
| Drain type (%) | 0.998 | ||
| subdural | 189 (40.6) | 46 (40.4) | |
| subperiosteal | 268 (57.6) | 66 (57.9) | |
| both | 8 (1.7) | 2 (1.8) | |
| Mobilization for 48 h (%) | 0.043 | ||
| Bed rest, flat | 194 (42.1) | 34 (30.4) | |
| Bed rest, 30° | 37 (8.0) | 17 (15.2) | |
| Partial mobilization | 100 (21.5) | 22 (19.3) | |
| Full mobilization | 130 (28) | 39 (34.2) | |
| Drain duration (mean ±SD), hours | 43.53 (9.10) | 40.34 (11.42) | 0.013 |
| Blood thinner = yes (%) | 253 (54.4) | 71 (62.3) | 0.158 |
| MLS preoperative (mean ±SD), cm | 0.72 (0.47) | 0.78 (0.62) | 0.256 |
| Hematoma width, preoperative (mean (±SD)), cm | 1.96 (0.76) | 2.06 (0.74) | 0.207 |
| Membranes n (mean ±SD) | 0.88 (0.94) | 0.75 (0.95) | 0.188 |
| Motor deficit, preoperative = yes (%) | 179 (38.5) | 34 (29.8) | 0.107 |
| Hypertension = yes (%) | 75 (16.1) | 12 (10.5) | 0.176 |
| CAD = yes (%) | 121 (26.0) | 40 (35.1) | 0.069 |
| Atrial fibrillation = yes (%) | 110 (23.7) | 27 (23.7) | 1 |
| COPD = yes (%) | 12 (2.6) | 5 (4.4) | 0.475 |
| Dementia = yes (%) | 29 (6.2) | 7 (6.1) | 1 |
| Smoking = yes (%) | 21 (4.5) | 5 (4.4) | 1 |
| Alcohol = yes (%) | 22 (4.7) | 4 (3.5) | 0.755 |
| GCS at presentation (median [IQR]) | 15.00 [14.00, 15.00] | 15.00 [14.00, 15.00]) | 0.246 |
| GCS at presentation grouped (%) | 0.571 | ||
| good | 408 (87.7) | 104 (91.2) | |
| moderate | 50 (10.8) | 9 (7.9) | |
| bad | 7 (1.5) | 1 (0.9) | |
| mRS at presentation (median [IQR]) | 2.00 [1.00, 3.00] | 2.00 [1.00, 2.00] | 0.352 |
| mRS at presentation grouped = good (%) | 399 (85.8) | 104 (91.2) | 0.167 |
| Recurrence | Odds Ratio (OR) | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Suction = yes (%) | |||
| no | Ref. | ||
| yes | 2.4 | 0.1–30.5 | 0.51 |
| Drain duration (mean ±SD), hours | 0.99 | 0.95–1.03 | 0.67 |
| Mobilization within the first 48 h | |||
| Bed rest, flat | Ref. | ||
| Bed rest, 30° | 1.1 | 0.09–24.8 | 0.96 |
| Partial mobilization | 0.06 | 0.002–2.1 | 0.08 |
| Full mobilization | 0.99 | 0.09–22.4 | 0.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ebel, F.; Greuter, L.; Lutz, K.; Häni, L.; Fandino, J.; Guzman, R.; Mariani, L.; Beck, J.; Raabe, A.; Z’Graggen, W.J.; et al. The Role of Active or Passive Drainage after Evacuation of Chronic Subdural Hematoma: An Analysis of Two Randomized Controlled Trials (cSDH-Drain-Trial and TOSCAN Trial). Diagnostics 2022, 12, 3045. https://doi.org/10.3390/diagnostics12123045
Ebel F, Greuter L, Lutz K, Häni L, Fandino J, Guzman R, Mariani L, Beck J, Raabe A, Z’Graggen WJ, et al. The Role of Active or Passive Drainage after Evacuation of Chronic Subdural Hematoma: An Analysis of Two Randomized Controlled Trials (cSDH-Drain-Trial and TOSCAN Trial). Diagnostics. 2022; 12(12):3045. https://doi.org/10.3390/diagnostics12123045
Chicago/Turabian StyleEbel, Florian, Ladina Greuter, Katharina Lutz, Levin Häni, Javier Fandino, Raphael Guzman, Luigi Mariani, Jürgen Beck, Andreas Raabe, Werner J. Z’Graggen, and et al. 2022. "The Role of Active or Passive Drainage after Evacuation of Chronic Subdural Hematoma: An Analysis of Two Randomized Controlled Trials (cSDH-Drain-Trial and TOSCAN Trial)" Diagnostics 12, no. 12: 3045. https://doi.org/10.3390/diagnostics12123045
APA StyleEbel, F., Greuter, L., Lutz, K., Häni, L., Fandino, J., Guzman, R., Mariani, L., Beck, J., Raabe, A., Z’Graggen, W. J., Schucht, P., & Soleman, J. (2022). The Role of Active or Passive Drainage after Evacuation of Chronic Subdural Hematoma: An Analysis of Two Randomized Controlled Trials (cSDH-Drain-Trial and TOSCAN Trial). Diagnostics, 12(12), 3045. https://doi.org/10.3390/diagnostics12123045








