The Value of Infrared Thermography to Assess Foot and Limb Perfusion in Relation to Medical, Surgical, Exercise or Pharmacological Interventions in Peripheral Artery Disease: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Data Collection
3. Results
3.1. Included Studies
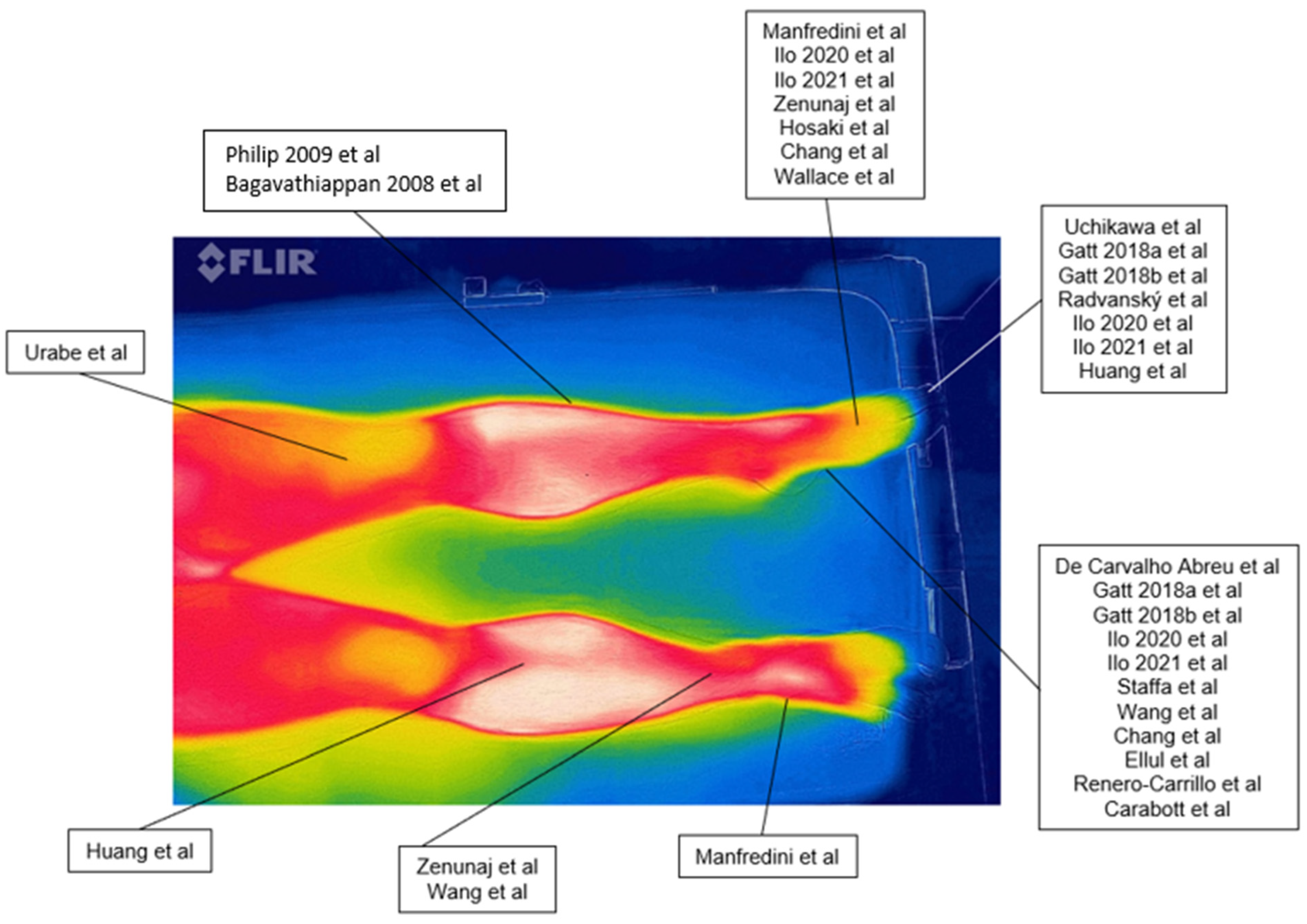
3.2. Measurement Locations
3.3. Diagnosis of PAD and Assessment of Peripheral Perfusion
3.4. Assessment after Different Interventions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Registration
References
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.R.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC Guideline on the Management of Patients with Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2017, 69, 1465–1508. [Google Scholar] [CrossRef] [PubMed]
- Radvansky, M.; Radvansky, M.; Kudelka, M. Identification of the Occurrence of Poor Blood Circulation in Toes by Processing Thermal Images from Flir Lepton Module. In Advances in Intelligent Networking and Collaborative Systems; Barolli, L., Chen, H.-C., Miwa, H., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 264–273. [Google Scholar]
- Treat-Jacobson, D.; McDermott, M.M.; Bronas, U.G.; Campia, U.; Collins, T.C.; Criqui, M.H.; Gardner, A.W.; Hiatt, W.R.; Regensteiner, J.G.; Rich, K.; et al. Optimal Exercise Programs for Patients with Peripheral Artery Disease: A Scientific Statement From the American Heart Association. Circulation 2019, 139, e10–e33. [Google Scholar] [CrossRef] [PubMed]
- Boezeman, R.P.; Moll, F.L.; Ünlü, Ç.; de Vries, J.-P.P. Systematic review of clinical applications of monitoring muscle tissue oxygenation with near-infrared spectroscopy in vascular disease. Microvasc. Res. 2016, 104, 11–22. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, F.; Lamberti, N.; Rossi, T.; Mascoli, F.; Basaglia, N.; Zamboni, P. A Toe Flexion NIRS assisted Test for Rapid Assessment of Foot Perfusion in Peripheral Arterial Disease: Feasibility, Validity, and Diagnostic Accuracy. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2017, 54, 187–194. [Google Scholar] [CrossRef]
- Tehan, P.E.; Santos, D.; Chuter, V.H. A systematic review of the sensitivity and specificity of the toe–brachial index for detecting peripheral artery disease. Vasc. Med. 2016, 21, 382–389. [Google Scholar] [CrossRef] [Green Version]
- Høyer, C.; Sandermann, J.; Petersen, L.J. The toe-brachial index in the diagnosis of peripheral arterial disease. J. Vasc. Surg. 2013, 58, 231–238. [Google Scholar] [CrossRef] [Green Version]
- Bajwa, A.; Wesolowski, R.; Patel, A.; Saha, P.; Ludwinski, F.; Smith, A.; Nagel, E.; Modarai, B. Assessment of tissue perfusion in the lower limb: Current methods and techniques under development. Circ. Cardiovasc. Imaging 2014, 7, 836–843. [Google Scholar] [CrossRef] [Green Version]
- Vardi, M.; Nini, A. Near-infrared spectroscopy for evaluation of peripheral vascular disease. A systematic review of literature. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2008, 35, 68–74. [Google Scholar] [CrossRef] [Green Version]
- Ubbink, D.; Koopman, B. Near-infrared Spectroscopy in the Routine Diagnostic Work-up of Patients with Leg Ischaemia. Eur. J. Vasc. Endovasc. Surg. 2006, 31, 394–400. [Google Scholar] [CrossRef] [Green Version]
- Grassi, B.; Quaresima, V. Near-infrared spectroscopy and skeletal muscle oxidative function in vivo in health and disease: A review from an exercise physiology perspective. J. Biomed. Opt. 2016, 21, 91313. [Google Scholar] [CrossRef]
- Jones, S.; Chiesa, S.T.; Chaturvedi, N.; Hughes, A.D. Recent developments in near-infrared spectroscopy (NIRS) for the assessment of local skeletal muscle microvascular function and capacity to utilise oxygen. Artery Res. 2016, 16, 25–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manfredini, F.; Malagoni, A.; Felisatti, M.; Mandini, S.; Mascoli, F.; Basaglia, N.; Zamboni, P. A Dynamic Objective Evaluation of Peripheral Arterial Disease by Near-Infrared Spectroscopy. Eur. J. Vasc. Endovasc. Surg. 2009, 38, 441–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamamoto, K.; Miyata, T.; Onozuka, A.; Koyama, H.; Ohtsu, H.; Nagawa, H. Plantar Flexion as an Alternative to Treadmill Exercise for Evaluating Patients with Intermittent Claudication. Eur. J. Vasc. Endovasc. Surg. 2007, 33, 325–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bækgaard, N.; Quistorff, B.; Pedersen, B.L. A Near Infrared Spectroscopy-Based Test of Calf Muscle Function in Patients with Peripheral Arterial Disease. Int. J. Angiol. 2015, 24, 25–34. [Google Scholar] [CrossRef] [Green Version]
- Shan, X.-F.; Ouyang, S.-Y.; Cai, Z.-G.; Zhang, J. Evaluation of Foot Perfusion After Fibula Flap Surgery. J. Craniofacial Surg. 2014, 25, 1346–1347. [Google Scholar] [CrossRef] [Green Version]
- Neidrauer, M.; Zubkov, L.; Weingarten, M.S.; Pourrezaei, K.; Papazoglou, E.S. Near Infrared Wound Monitor Helps Clinical Assessment of Diabetic Foot Ulcers. J. Diabetes Sci. Technol. 2010, 4, 792–798. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boezeman, R.P.E.; Becx, B.P.; van den Heuvel, D.A.F.; Ünlü, Ç.; Vos, J.A.; de Vries, J.P.P.M. Monitoring of Foot Oxygenation with Near-infrared Spectroscopy in Patients with Critical Limb Ischemia Undergoing Percutaneous Transluminal Angioplasty: A Pilot Study. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2016, 52, 650–656. [Google Scholar] [CrossRef] [Green Version]
- Manfredini, F.; Malagoni, A.M.; Felisatti, M.; Mandini, S.; Lamberti, N.; Manfredini, R.; Mascoli, F.; Basaglia, N.; Zamboni, P. Acute oxygenation changes on ischemic foot of a novel intermittent pneumatic compression device and of an existing sequential device in severe peripheral arterial disease. BMC Cardiovasc. Disord. 2014, 14, 40. [Google Scholar] [CrossRef] [Green Version]
- Wermelink, B.; Ma, K.F.; Haalboom, M.; El Moumni, M.; de Vries, J.-P.P.M.; Geelkerken, R.H. A Systematic Review and Critical Appraisal of Peri-Procedural Tissue Perfusion Techniques and their Clinical Value in Patients with Peripheral Arterial Disease. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2021, 62, 896–908. [Google Scholar] [CrossRef]
- Philip, J.; Jayakumar, T.; Raj, B.; Karunanithi, R.; Panicker, T.M.R.; Korath, M.P.; Jagadeesan, K.; Bagavathiappan, S.; Saravanan, T. Infrared thermal imaging for detection of peripheral vascular disorders. J. Med. Phys. 2009, 34, 43–47. [Google Scholar] [CrossRef]
- Antônio de Carvalho Abreu, J.; de Oliveira, R.A.; Martin, A.A. Correlation between ankle-brachial index and thermography measurements in patients with peripheral arterial disease. Vascular 2022, 30, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Astasio, A.; Martínez, E.E.; Martin, B.G.; Mart, E.E. Comparison of Thermal Foot Maps between Diabetic Patients with Neuropathic, Vascular, Neurovascular, and No Complications. Curr. Diabetes Rev. 2019, 15, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Schiavon, G.; Capone, G.; Frize, M.; Zaffagnini, S.; Candrian, C.; Filardo, G. Infrared Thermography for the Evaluation of Inflammatory and Degenerative Joint Diseases: A Systematic Review. Cartilage 2021, 13, 1790S–1801S. [Google Scholar] [CrossRef] [PubMed]
- Dias de Lacerda, A.P.; Rodrigues de Andrade, P.; Kamonseki, D.H.; Parizotto, N.A.; Alves da Silva, A.S.; Bernardo de Medeiros, L.; de Almeida Ferreira, J.J. Accuracy of infrared thermography in detecting tendinopathy: A systematic review with meta-analysis. Phys. Ther. Sport Off. J. Assoc. Chart. Physiother. Sport Med. 2022, 58, 117–125. [Google Scholar] [CrossRef]
- Dang, J.; Lin, M.; Tan, C.; Pham, C.H.; Huang, S.; Hulsebos, I.F.; Yenikomshian, H.; Gillenwater, J. Use of Infrared Thermography for Assessment of Burn Depth and Healing Potential: A Systematic Review. J. Burn Care Res. 2021, 42, 1120–1127. [Google Scholar] [CrossRef]
- Moreira, A.; Batista, R.; Oliveira, S.; Branco, C.A.; Mendes, J.; Figueiral, M.H. Role of thermography in the assessment of temporomandibular disorders and other musculoskeletal conditions: A systematic review. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2021, 235, 1099–1112. [Google Scholar] [CrossRef]
- Hakim, A.; Awale, R.N. Thermal Imaging—An Emerging Modality for Breast Cancer Detection: A Comprehensive Review. J. Med Syst. 2020, 44, 136. [Google Scholar] [CrossRef]
- Lahiri, B.; Bagavathiappan, S.; Jayakumar, T.; Philip, J. Medical applications of infrared thermography: A review. Infrared Phys. Technol. 2012, 55, 221–235. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Ilo, A.; Romsi, P.; Mäkelä, J. Infrared Thermography as a Diagnostic Tool for Peripheral Artery Disease. Adv. Ski. Wound Care 2020, 33, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Ilo, A.; Romsi, P.; Pokela, M.; Mäkelä, J. Infrared Thermography Follow-Up After Lower Limb Revascularization. J. Diabetes Sci. Technol. 2021, 15, 807–815. [Google Scholar] [CrossRef] [PubMed]
- Staffa, E.; Bernard, V.; Kubíček, L.; Vlachovský, R.; Vlk, D.; Mornstein, V.; Staffa, R. Using Noncontact infrared Thermography for long-term monitoring of foot temperatures in a patient with diabetes mellitus. Ostomy Wound Manag. 2016, 62, 54–61. [Google Scholar]
- Renero-C, F.-J.; Ziga-Martínez, A.; Silva-González, M.; Carbajal-Robles, V. The Peripheral Artery Disease through the Thermogram and the Photoplethysmogram Before and After a Revascularization Surgery. J. Diabetes Sci. Technol. 2021, 15, 1200–1201. [Google Scholar] [CrossRef]
- Ellul, C.; Formosa, C.; Gatt, A.; Hamadani, A.A.; Armstrong, D.G. The Effectiveness of Calf Muscle Electrostimulation on Vascular Perfusion and Walking Capacity in Patients Living with Type 2 Diabetes Mellitus and Peripheral Artery Disease. Int. J. Low. Extremity Wounds 2017, 16, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Wallace, G.A.; Singh, N.; Quiroga, E.; Tran, N.T. The Use of Smart Phone Thermal Imaging for Assessment of Peripheral Perfusion in Vascular Patients. Ann. Vasc. Surg. 2018, 47, 157–161. [Google Scholar] [CrossRef]
- Manfredini, F.; Lamberti, N.; Traina, L.; Zenunaj, G.; Medini, C.; Piva, G.; Straudi, S.; Manfredini, R.; Gasbarro, V. Effectiveness of Home-Based Pain-Free Exercise versus Walking Advice in Patients with Peripheral Artery Disease: A Randomized Controlled Trial. Methods Protoc. 2021, 4, 29. [Google Scholar] [CrossRef]
- Zenunaj, G.; Lamberti, N.; Manfredini, F.; Traina, L.; Acciarri, P.; Bisogno, F.; Scian, S.; Serra, R.; Abatangelo, G.; Gasbarro, V. Infrared Thermography as a Diagnostic Tool for the Assessment of Patients with Symptomatic Peripheral Arterial Disease Undergoing Infrafemoral Endovascular Revascularisations. Diagnostics 2021, 11, 1701. [Google Scholar] [CrossRef]
- Carabott, M.; Formosa, C.; Mizzi, A.; Papanas, N.; Gatt, A. Thermographic Characteristics of the Diabetic Foot with Peripheral Arterial Disease Using the Angiosome Concept. Exp. Clin. Endocrinol. Diabetes 2021, 129, 93–98. [Google Scholar] [CrossRef]
- Gatt, A.; Falzon, O.; Cassar, K.; Camilleri, K.P.; Gauci, J.; Ellul, C.; Mizzi, S.; Mizzi, A.; Papanas, N.; Sturgeon, C.; et al. The Application of Medical Thermography to Discriminate Neuroischemic Toe Ulceration in the Diabetic Foot. Int. J. Low. Extremity Wounds 2018, 17, 102–105. [Google Scholar] [CrossRef]
- Gatt, A.; Cassar, K.; Falzon, O.; Ellul, C.; Camilleri, K.P.; Gauci, J.; Mizzi, S.; Mizzi, A.; Sturgeon, C.; Chockalingam, N.; et al. The identification of higher forefoot temperatures associated with peripheral arterial disease in type 2 diabetes mellitus as detected by thermography. Prim. Care Diabetes 2018, 12, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Uchikawa, T.; Murakami, T.; Furukawa, H. Effects of the anti-platelet agent cilostazol on peripheral vascular disease in patients with diabetes mellitus. Arzneim. Forsch. 1992, 42, 322–324. [Google Scholar]
- Wang, H.; Wade, D.R., Jr.; Kam, J. IR imaging of blood circulation of patients with vascular disease. In Thermosense XXVI; SPIE: Bellingham, WA, USA, 2004; pp. 115–123. [Google Scholar]
- Urabe, Y.; Ideishi, M.; Sasaguri, M.; Ikeda, M.; Arakawa, K. Beneficial effects of a serine protease inhibitor in peripheral vascular disease. Am. J. Cardiol. 1993, 72, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Hosaki, Y.; Mitsunobu, F.; Ashida, K.; Tsugeno, H.; Okamoto, M.; Nishida, N.; Takata, S.; Yokoi, T.; Tanizaki, Y.; Ochi, K.; et al. Non-invasive study for peripheral circulation in patients with diabetes mellitus. OKAYAMA Univ. Sci. Achiev. Repos. 2002, 72, 31–37. [Google Scholar]
- Bagavathiappan, S.; Saravanan, T.; Philip, J.; Jayakumar, T.; Raj, B.; Karunanithi, R.; Panicker, T.; Korath, P.; Jagadeesan, K. Investigation of peripheral vascular disorders using thermal imaging. Br. J. Diabetes 2008, 8, 102–104. [Google Scholar] [CrossRef]
- Huang, C.-L.; Wu, Y.-W.; Hwang, C.-L.; Jong, Y.-S.; Chao, C.-L.; Chen, W.-J.; Wu, Y.-T.; Yang, W.-S. The application of infrared thermography in evaluation of patients at high risk for lower extremity peripheral arterial disease. J. Vasc. Surg. 2011, 54, 1074–1080. [Google Scholar] [CrossRef] [Green Version]
- Chang, W.-C.; Wang, C.-Y.; Cheng, Y.; Hung, Y.-P.; Lin, T.-H.; Chen, W.-J.; Su, C.-S.; Hsu, C.-Y.; Liu, T.-J.; Lee, W.-L. Plantar thermography predicts freedom from major amputation after endovascular therapy in critical limb ischemic patients. Medicine 2020, 99, e22391. [Google Scholar] [CrossRef]
- Gatt, A.; Falzon, O.; Cassar, K.; Ellul, C.; Camilleri, K.P.; Gauci, J.; Mizzi, S.; Mizzi, A.; Sturgeon, C.; Camilleri, L.; et al. Establishing Differences in Thermographic Patterns between the Various Complications in Diabetic Foot Disease. Int. J. Endocrinol. 2018, 2018, 9808295. [Google Scholar] [CrossRef] [Green Version]
- de Deus Passos, M.; Da Rocha, A.F. Evaluation of infrared thermography with a portable camera as a diagnostic tool for peripheral arterial disease of the lower limbs compared with color Doppler ultrasonography. Arch. Med. Sci. Atheroscler. Dis. 2022, 7, e66–e72. [Google Scholar] [CrossRef]

| Model | Resolution | Spectral Range | Standard Temperature Range | Accuracy | Reference |
|---|---|---|---|---|---|
| FLIR A325sc | 320 × 240 | 7.5–13 μm | −20 °C to 120 °C; 0 °C to 350 °C | ±2 °C or ±2% of reading | [32,33] |
| FLIR B200 | 1280 × 1024 | 7.5–13 μm | −20 °C to 120 °C; up to 1200 °C | ±2 °C or ±2% of reading | [34] |
| FLIR E6 | 320 × 240 | 7.5–13 μm | −20 °C to 250 °C | ±2 °C or ±2% of reading | [35] |
| FLIR I3 | 60 × 60 | 7.5–13 μm | −20 °C to 250 °C | ±2 °C or ±2% of reading | [36] |
| FLIR Lepton 3.5 | 160 h × 120 v | 8–14 μm | −10 °C to 140 °C; −10 °C to 400 °C; −10 °C to 450 °C | ±5 °C or 5%; ±10 °C or 10% | [2] |
| FLIR ONE-Pro | 1440 × 1080 | 8–14 µm | −20 °C to 400 °C | ±3 °C o ±5% | [37,38,39] |
| FLIR SC630 | NA | NA | NA | NA | [40] |
| FLIR SC7200 | 320 × 256 | 1.5–5.1 µm | −20 °C to 300 °C; 5°C to 1500 °C; up to 2500 °C | ±1 °C or ±1% of reading | [41,42] |
| FLIR T430SC | 320 × 240 | 7.5–13 μm | −20 °C to 120 °C; 0 °C to 650 °C | ±2 °C or ±2% of reading | [22] |
| Infra-eye-150 | NA | NA | NA | NA | [43] |
| Raytheon Radiance HS | 256 × 256 | 3–5 µm | NA | NA | [44] |
| Thermo Tracer 6T66 | NA | NA | NA | NA | [45,46] |
| Thermovision 550 | NA | 3.6–5 µm | −20 °C to 250 °C, up to 1500 °C | ±2 °C or ±2% of reading | [21,47] |
| Spectrum 9000-MB Series | 320 × 240 | NA | NA | NA | [48,49] |
| Study (Year) | Study Design | Scope of the Study | PAD Stage | Sample Size | Age | Measurement Location | Temperature Variations | Other Outcomes | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Bagavathiappan et al. (2008) | Case report | Detection of PAD | NA | 3 | 35.7 (28–48) | Shins, Feet | NA | NA | [47] |
| Philip et al. (2009) | Technical note | Detection of PAD | NA | 4 | 36.7 (28–40) | Shins, Feet | NA | NA | [21] |
| Carabott et al. (2021) | Observational study | Assessment after limb elevation challenge | I–III | 27 | 62.7 ± 6 non-PAD; 71.1 ± 7 mild PAD; 71 ± 5 severe PAD | Feet | −0.03 °C (non-PAD) −0.18 °C (mild PAD) −0.27 °C (severe PAD) | NA | [40] |
| Chang et al. (2020) | Observational study | Assessment after revascularization | IV | 124 | 73 (63–80) | Feet | +1.3 °C (healing) +1.3 °C (nonhealing) | NA | [49] |
| de Carvalho Abreu et al. (2022) | Nonrandomized | Correlation IRT-ABI | I–IV | 53 | 59.9 ± 16.3 | Feet | NA | ABI | [22] |
| Ellul et al. (2017) | Randomized | Assessment after EMS | II | 40 | 70.8 ± 7 | Feet | −0.5 °C (baseline) −0.3 °C (follow-up) | ABI, ACD | [36] |
| Gatt et al. (2018) | Nonrandomized | Assessment of peripheral perfusion | III | 53 | 64.5 ± 5 females DM + PAD; 72.2 ± 8 males DM + PAD; 59.8 ± 11 females DM; 65.8 ± 7 males DM | Feet | NA | ABI, SD | [41] |
| Gatt et al. (2018) | Nonrandomized | Detection of foot complications | I–II | 182 | NA | Feet | NA | ABI, SD, 10 g monofilament | [42] |
| Hosaki et al. (2002) | Case report | Assessment of peripheral perfusion | NA | 27 | 67.4 (51–82) | Feet | NA | LDBF | [46] |
| Huang et al. (2011) | Observational study | Detection of PAD | NA | 51 | 72.9 ± 10 PAD; 68.2 ± 8 non-PAD | Shins, Feet | −1.25 °C (PAD) −0.15 (non-PAD) | 6MWD, ABI, SBP | [48] |
| Ilo et al. (2020) | Observational study | Detection of PAD | I–II | 257 | 73 ± 10 PAD; 61 ± 18 non-PAD | Feet | NA | ABI, TP | [32] |
| Ilo et al. (2021) | Nonrandomized | Assessment after revascularization | I–III | 54 | 72 ± 10 treated;75 ± 8 control | Feet | +0.5 °C (treated) −0.3 °C (nontreated) −0.2 °C (control) | ABI, TP | [33] |
| Manfredini et al. (2021) | Study protocol | Assessment after exercise program | II | 60 | >60 | Feet | NA | 6MWD, ABI, QoL, 5TSTS | [38] |
| Radvanský et al. (2022) | Commentary | Detection of PAD | NA | NA | NA | Feet | NA | NA | [2] |
| Renero-Carrillo et al. (2021) | Nonrandomized | Assessment after revascularization | NA | 2 | 60.5 (55–66) | Feet | +6 °C (treated) −0.7 °C (nontreated) | PPG | [35] |
| Staffa et al. (2016) | Nonrandomized | Assessment after revascularization | I–III | 41 | 60.2 ± 18 PAD; 55.6 ± 18 non-PAD | Feet | +0.4 °C (treated) −0.5 °C (nontreated) | ABI | [34] |
| Uchikawa et al. (1992) | Observational study | Assessment after pharmacological therapy | II | 10 | 51 (36–68) | Feet | +3.3 °C (average) +4.4 °C (lowest) | NA | [43] |
| Urabe et al. (1993) | Randomized | Assessment after pharmacological therapy | II | 20 | 65.6 ± 2.3 | Legs | +0.2 °C | Walking distance, Lac, PPG | [45] |
| Wallace et al. (2018) | Case report | Assessment of peripheral perfusion | I-IV | 23 | 66 (30–76) | Feet | NA | ABI | [37] |
| Wang et al. (2004) | Observational study | Assessment of peripheral perfusion | NA | 7 | NA | Ankle, Feet | NA | NA | [44] |
| Zenunaj et al. (2021) | Observational study | Assessment after revascularization | II-IV | 40 | 76 ± 11 | Ankle, Feet | +2.1 °C (lowest) +0.5 °C (highest) | ABI | [39] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piva, G.; Crepaldi, A.; Zenunaj, G.; Caruso, L.; Rinaldo, N.; Gasbarro, V.; Lamberti, N.; Lòpez-Soto, P.J.; Manfredini, F. The Value of Infrared Thermography to Assess Foot and Limb Perfusion in Relation to Medical, Surgical, Exercise or Pharmacological Interventions in Peripheral Artery Disease: A Systematic Review. Diagnostics 2022, 12, 3007. https://doi.org/10.3390/diagnostics12123007
Piva G, Crepaldi A, Zenunaj G, Caruso L, Rinaldo N, Gasbarro V, Lamberti N, Lòpez-Soto PJ, Manfredini F. The Value of Infrared Thermography to Assess Foot and Limb Perfusion in Relation to Medical, Surgical, Exercise or Pharmacological Interventions in Peripheral Artery Disease: A Systematic Review. Diagnostics. 2022; 12(12):3007. https://doi.org/10.3390/diagnostics12123007
Chicago/Turabian StylePiva, Giovanni, Anna Crepaldi, Gladiol Zenunaj, Lorenzo Caruso, Natascia Rinaldo, Vincenzo Gasbarro, Nicola Lamberti, Pablo Jesùs Lòpez-Soto, and Fabio Manfredini. 2022. "The Value of Infrared Thermography to Assess Foot and Limb Perfusion in Relation to Medical, Surgical, Exercise or Pharmacological Interventions in Peripheral Artery Disease: A Systematic Review" Diagnostics 12, no. 12: 3007. https://doi.org/10.3390/diagnostics12123007
APA StylePiva, G., Crepaldi, A., Zenunaj, G., Caruso, L., Rinaldo, N., Gasbarro, V., Lamberti, N., Lòpez-Soto, P. J., & Manfredini, F. (2022). The Value of Infrared Thermography to Assess Foot and Limb Perfusion in Relation to Medical, Surgical, Exercise or Pharmacological Interventions in Peripheral Artery Disease: A Systematic Review. Diagnostics, 12(12), 3007. https://doi.org/10.3390/diagnostics12123007









