Applicability of American College of Radiology Appropriateness Criteria Decision-Making Model for Acute Appendicitis Diagnosis in Children
Abstract
:1. Introduction
2. Material and Method
2.1. Study Design
2.2. Fuzzy PROMETHEE (F-PROMETHEE)
2.3. TOPSIS
3. Results
Multi Criteria Decision Making Theory Results (MCDM)
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Omari, A.H.; Khammash, M.R.; Qasaimeh, G.R.; Shammari, A.K.; Yaseen, M.K.B.; Hammori, S.K. Acute appendicitis in the elderly: Risk factors for perforation. World J. Emerg. Surg. 2014, 9, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ashdown, H.F.; D’Souza, N.; Karim, D.; Stevens, R.J.; Huang, A.; Harnden, A. Pain over speed bumps in diagnosis of acute appendicitis: Diagnostic accuracy study. BMJ 2012, 345, e8012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andersson, R.E. The magic of an appendicitis score. World J. Surg. 2015, 39, 110–111. [Google Scholar] [CrossRef]
- Benabbas, R.; Hanna, M.; Shah, J.; Sinert, R. Diagnostic Accuracy of History, Physical Examination, Laboratory Tests, and Point-of-care Ultrasound for Paediatric Acute Appendicitis in the Emergency Department: A Systematic Review and Meta-analysis. Acad. Emerg. Med. 2017, 24, 523–551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atema, J.J.; Van Rossem, C.C.; Leeuwenburgh, M.M.; Stoker, J.; A Boermeester, M. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br. J. Surg. 2015, 102, 979–990. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.W.; Juan, L.I.; Wu, M.H.; Shen, C.; Wu, J.; Lee, C. Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis. Br. J. Surg. 2013, 100, 322–329. [Google Scholar] [CrossRef]
- Acharya, A.; Markar, S.R.; Ni, M.; Hanna, G.B. Biomarkers of acute appendicitis: Systematic review and cost–benefit trade-off analysis. Surg. Endosc. 2017, 31, 1022–1031. [Google Scholar] [CrossRef] [Green Version]
- Becker, T.; Kharbanda, A.; Bachur, R. Atypical clinical features of paediatric appendicitis. Acad. Emerg. Med. 2007, 14, 124–129. [Google Scholar] [CrossRef] [Green Version]
- Nance, M.L.; Adamson, W.T.; Hedrick, H.L. Appendicitis in the young child: A continuing diagnostic challenge. Pediatr. Emerg. Care 2000, 16, 160–162. [Google Scholar] [CrossRef]
- Davenport, M. Acute abdominal pain in children. BMJ 1996, 312, 498–501. [Google Scholar] [CrossRef]
- Narsule, C.K.; Kahle, E.J.; Kim, D.S.; Anderson, A.C.; Luks, F.I. Effect of delay in presentation on rate of perforation in children with appendicitis. Am. J. Emerg. Med. 2011, 29, 890–893. [Google Scholar] [CrossRef] [PubMed]
- Kharbanda, A.B.; Taylor, G.A.; Fishman, S.J.; Bachur, R.G. A clinical decision rule to identify children at low risk for appendicitis. Paediatrics 2005, 116, 709–716. [Google Scholar] [CrossRef]
- Martin, A.E.; Vollman, D.; Adler, B.; Caniano, D.A. CT scans may not reduce the negative appendectomy rate in children. J. Pediatr. Surg. 2004, 39, 886–890, discussion 886–890. [Google Scholar] [CrossRef]
- Partrick, D.A.; Janik, J.E.; Janik, J.S.; Bensard, D.D.; Karrer, F.M. Increased CT scan utilization does not improve the diagnostic accuracy of appendicitis in children. J. Paediatr. Surg. 2003, 38, 659–662. [Google Scholar] [CrossRef] [PubMed]
- Miglioretti, D.L.; Johnson, E.; Williams, A.; Greenlee, R.T.; Weinmann, S.; Solberg, L.I.; Feigelson, H.S.; Roblin, D.; Flynn, M.J.; Vanneman, N.; et al. The use of computed tomography in paediatrics and the associated radiation exposure and estimated cancer risk. JAMA Paediatr. 2013, 167, 700–707. [Google Scholar] [CrossRef]
- Alvarado, A. Diagnostic Scores in Acute Appendicitis. In Current Issues in the Diagnostics and Treatment of Acute Appendicitis; IntechOpen: London, UK, 2018; 43p. [Google Scholar] [CrossRef]
- de Castro, S.M.M.; Unlu, C.; Ph Steller, E.; van Wangensveld, A.; Vrouenraets, B.C. Evaluation of the appendicitis inflammatory response score for patients with acute appendicitis. World J. Surg. 2012, 36, 1540–1545. [Google Scholar] [CrossRef] [Green Version]
- Di Saverio, S.; Podda, M.; De Simone, B.; Ceresoli, M.; Augustin, G.; Gori, A.; Boermeester, M.; Sartelli, M.; Coccolini, F.; Tarasconi, A.; et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J. Emerg. Surg. 2020, 15, 27. [Google Scholar] [CrossRef]
- Andersson, M.; Kolodziej, B.; Andersson, R.E. Validation of the Appendicitis Inflammatory Response (AIR) Score. World J. Surg. 2021, 45, 2081–2091. [Google Scholar] [CrossRef]
- Cartwright, S.L.; Knudson, M.P. Diagnostic imaging of acute abdominal pain in adults. Am. Fam. Physician 2015, 91, 452–459. [Google Scholar]
- Tseng, J.; Cohen, T.; Melo, N.; Alban, R.F. Imaging utilization affects negative appendectomy rates in appendicitis: An ACS-NSQIP study. Am. J. Surg. 2019, 217, 1094–1098. [Google Scholar] [CrossRef]
- Chiu, Y.H.; Chen, J.D.; Wang, S.H.; Tiu, C.M.; How, C.K.; Lai, J.I.; Chou, Y.H.; Chen, R.J. Whether intravenous contrast is necessary for CT diagnosis of acute appendicitis in adult ED patients? Acad. Radiol. 2013, 20, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Repplinger, M.D.; Levy, J.F.; Peethumnongsin, E.; Gussick, M.E.; Svenson, J.E.; Golden, S.K.; Ehlenbach, W.J.; Westergaard, R.P.; Reeder, S.B.; Vanness, D.J. Systematic review and meta-analysis of the accuracy of MRI to diagnose appendicitis in the general population. J. Magn. Reason. Imaging 2016, 43, 1346–1354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, L.; Yang, J.-B. Introduction to Multi-Criteria Decision Making and the Evidential Reasoning Approach; Manchester School of Management: Manchester, UK, 2001; ISBN 186115111X. [Google Scholar]
- Zarghami, M.; Szidarovszky, F. Multicriteria Analysis: Applications to Water and Environment Management; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Karamouz, M.; Szidarovszky, F.; Zahraie, B. Water Resources Systems Analysis; Lewis Publishers: Boca Raton, FL, USA, 2003. [Google Scholar]
- Pardalos, P.M.; Hearn, D. Multi-Criteria Decision Making Methods: A Comparative Study. In Multi-Criteria Decision Making Methods: A Comparative Study; Springer: Boston, MA, USA, 2000. [Google Scholar]
- Kittur, J. Using the PROMETHEE and TOPSIS multi-criteria decision making methods to evaluate optimal generation. In Proceedings of the 2015 International Conference on Power and Advanced Control Engineering (ICPACE), Bengaluru, India, 12–14 August 2015; pp. 80–85. [Google Scholar] [CrossRef]
- El Hachami, K.; Alaoui, Y.L.; Tkiouat, M. Sectorial evaluation of islamic banking contracts: A fuzzy multi-criteria-decision-making approach. Invest. Manag. Financ. Innov. 2019, 16, 370–382. [Google Scholar] [CrossRef]
- Brans, J.P.; Mareschal, B.; Vincke, P. Promethee: A New Family of Outranking Methods in Multicriteria Analysis. ULB Inst. Repos. 1984, 477–490. [Google Scholar]
- Uzun, B.; Yıldırım, F.S.; Sayan, M.; Şanlıdağ, T.; Ozsahin, D.U. The Use of Fuzzy PROMETHEE Technique in Antiretroviral Combination Decision in Paediatric HIV Treatments. In Proceedings of the 2019 Advances in Science and Engineering Technology International Conferences (ASET), Dubai, United Arab Emirates, 26 March–10 April 2019. [Google Scholar] [CrossRef]
- Uzun, B.; Ozsahin, I.; Oru Agbor, V.; Uzun Ozsahin, D. Chapter 2—Theoretical aspects of multi-criteria decision-making (MCDM) methods. In Applications of Multi-Criteria Decision-Making Theories in Healthcare and Biomedical Engineering; Ozsahin, I., Ozsahin, D.U., Uzun, B., Eds.; Academic Press: London, UK, 2021; pp. 3–40. ISBN 9780128240861. [Google Scholar]
- Aydin, E.; Turkmen, I.U.; Namlı, G.; Ozturk, C.; Esen, A.B.; Eray, Y.N.; Eroglu, E.; Akova, F. A novel and simple machine learning algorithm for preoperative diagnosis of acute appendicitis in children. Pediatr. Surg. Int. 2020, 36, 735–742. [Google Scholar] [CrossRef]


| Diagnosis | Score |
|---|---|
| Vomit | 1 |
| Pain in RLQ | 1 |
| Rebound tenderness low | 1 |
| Rebound tenderness mild | 2 |
| Rebound tenderness severe | 3 |
| Temperature > 38.5 °C | 1 |
| PNL 70–84% | 1 |
| PNL > 85% | 2 |
| Leukocytes (WBC) > 10.0–14.9 × 109/L | 1 |
| Leukocytes (WBC) > 15.0 × 109/L | 2 |
| CRP 10–49 g/L | 1 |
| CRP > 50 g/L | 2 |
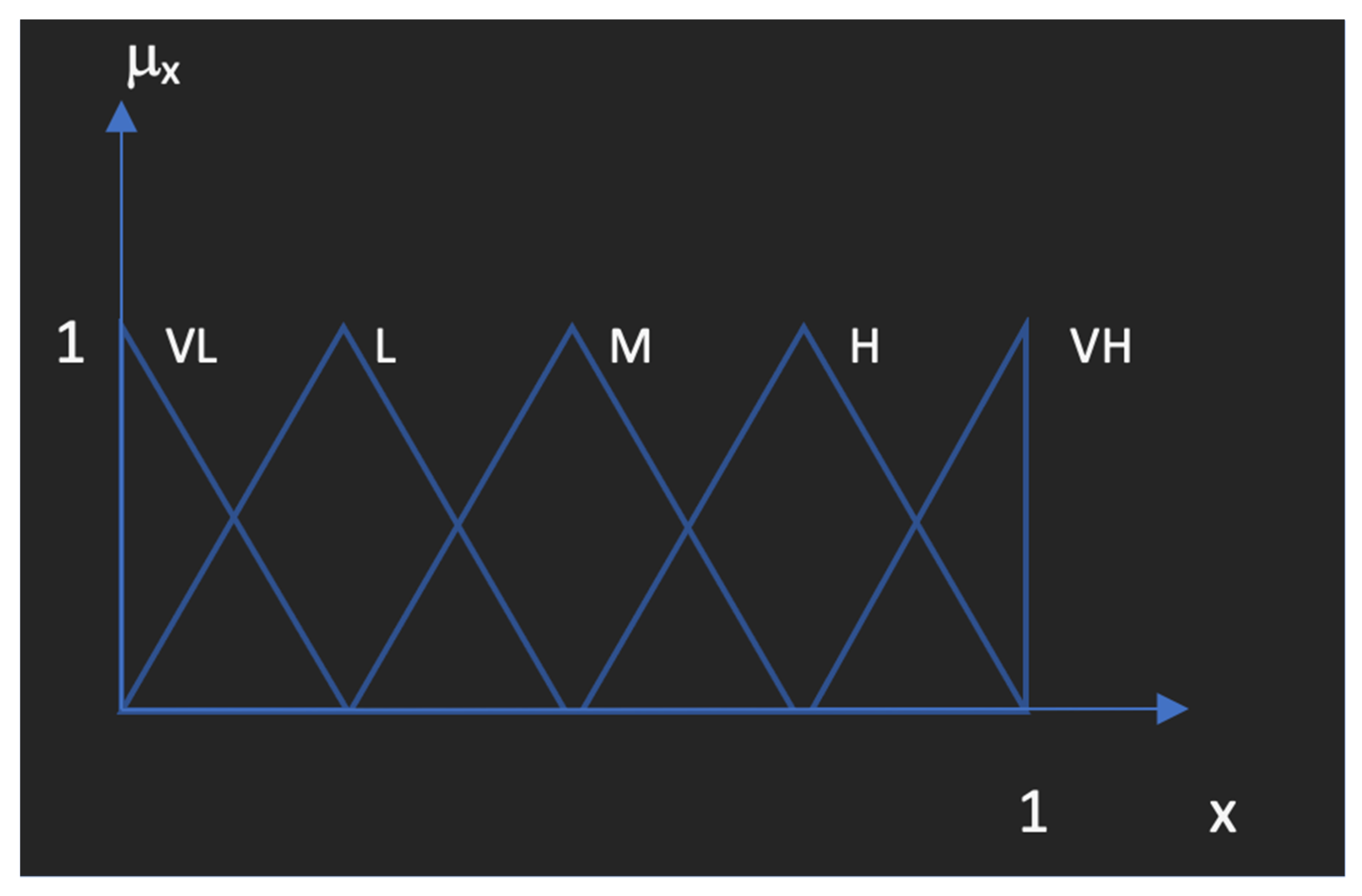
| Linguistic Scale for Evaluation | Triangular Fuzzy Scale | Criteria of the Decision Alternatives |
|---|---|---|
| VH | (0.75, 1, 1) | specificity, diagnostic precision, time of imaging, user dependency, radiation dose, comfortability |
| H | (0.50, 0.75, 1) | sensitivity, air score, disposition |
| M | (0.25, 0.50, 0.75) | time of order, result time, cost |
| L | (0, 0.25, 0.50) | - |
| VL | (0, 0, 0.25) | - |
| Rank | Alternatives | |
|---|---|---|
| 1 | CT non-contrast | 0.0733 |
| 2 | CT contrast | 0.0535 |
| 3 | US | 0.1305 |
| 4 | MRI | −0.0432 |
| Rank | Alternatives | Ri | ||
|---|---|---|---|---|
| 1 | CT non-contrast | 0.0927 | 0.1588 | 0.6315 |
| 2 | CT contrast | 0.0946 | 0.1561 | 0.6227 |
| 3 | US | 0.1210 | 0.1435 | 0.5425 |
| 4 | MRI | 0.1288 | 0.1405 | 0.5217 |
| Rank | Alternatives | |
|---|---|---|
| 1 | CT non-contrast | 0.0702 |
| 2 | US | 0.0617 |
| 3 | CT contrast | 0.0503 |
| 4 | MRI | 0.0456 |
| Ranking | Alternatives | Ri | ||
|---|---|---|---|---|
| 1 | CT non-contrast | 0.0977 | 0.1588 | 0.6191 |
| 2 | CT contrast | 0.0995 | 0.1561 | 0.6107 |
| 3 | US | 0.1210 | 0.1468 | 0.5481 |
| 4 | MRI | 0.1316 | 0.1399 | 0.5153 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tuncyurek, O.; Kadam, K.; Uzun, B.; Uzun Ozsahin, D. Applicability of American College of Radiology Appropriateness Criteria Decision-Making Model for Acute Appendicitis Diagnosis in Children. Diagnostics 2022, 12, 2915. https://doi.org/10.3390/diagnostics12122915
Tuncyurek O, Kadam K, Uzun B, Uzun Ozsahin D. Applicability of American College of Radiology Appropriateness Criteria Decision-Making Model for Acute Appendicitis Diagnosis in Children. Diagnostics. 2022; 12(12):2915. https://doi.org/10.3390/diagnostics12122915
Chicago/Turabian StyleTuncyurek, Ozum, Koray Kadam, Berna Uzun, and Dilber Uzun Ozsahin. 2022. "Applicability of American College of Radiology Appropriateness Criteria Decision-Making Model for Acute Appendicitis Diagnosis in Children" Diagnostics 12, no. 12: 2915. https://doi.org/10.3390/diagnostics12122915
APA StyleTuncyurek, O., Kadam, K., Uzun, B., & Uzun Ozsahin, D. (2022). Applicability of American College of Radiology Appropriateness Criteria Decision-Making Model for Acute Appendicitis Diagnosis in Children. Diagnostics, 12(12), 2915. https://doi.org/10.3390/diagnostics12122915







