Changing the Patient’s Position: Pitfalls and Benefits for Radiation Dose and Image Quality of Computed Tomography in Polytrauma
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients’ Characteristics
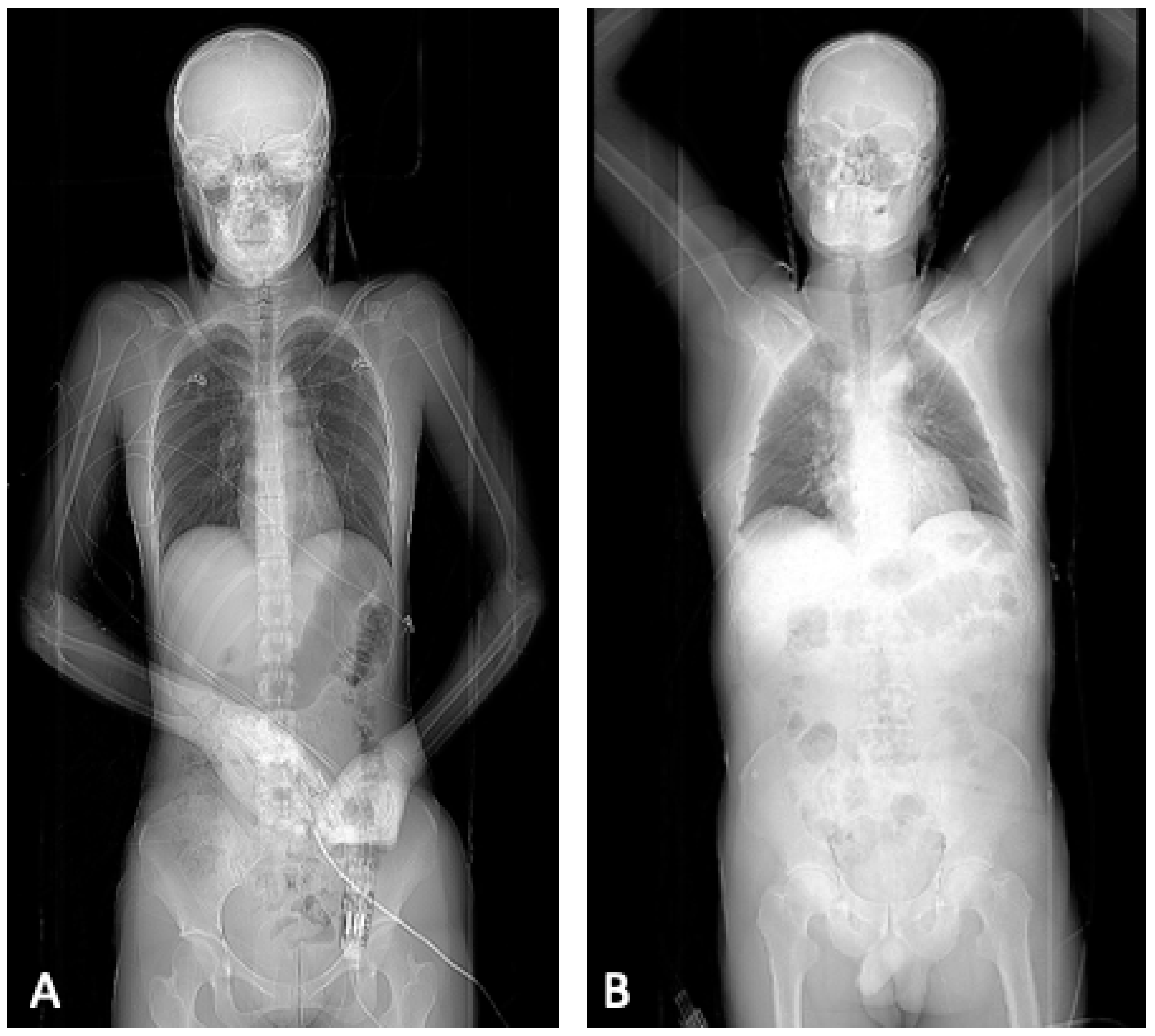
- Single whole-body scout, both arms adducted
- Non-enhanced head CT, both arms adducted
- CT-angiography of the head and neck, both arms adducted
- Contrast-enhanced examination of the thorax and abdomen using
- ○
- Protocol A: without repositioning, both arms still in adduction
- ○
- Protocol B: relocation and positioning of both arms in elevation
- First scout: head scout, both arms adducted
- Non-enhanced head CT, both arms adducted
- Second scout: whole-body scout, both arms elevated
- CT-angiography of head and neck in elevation
- Contrast-enhanced examination of thorax and abdomen in elevation
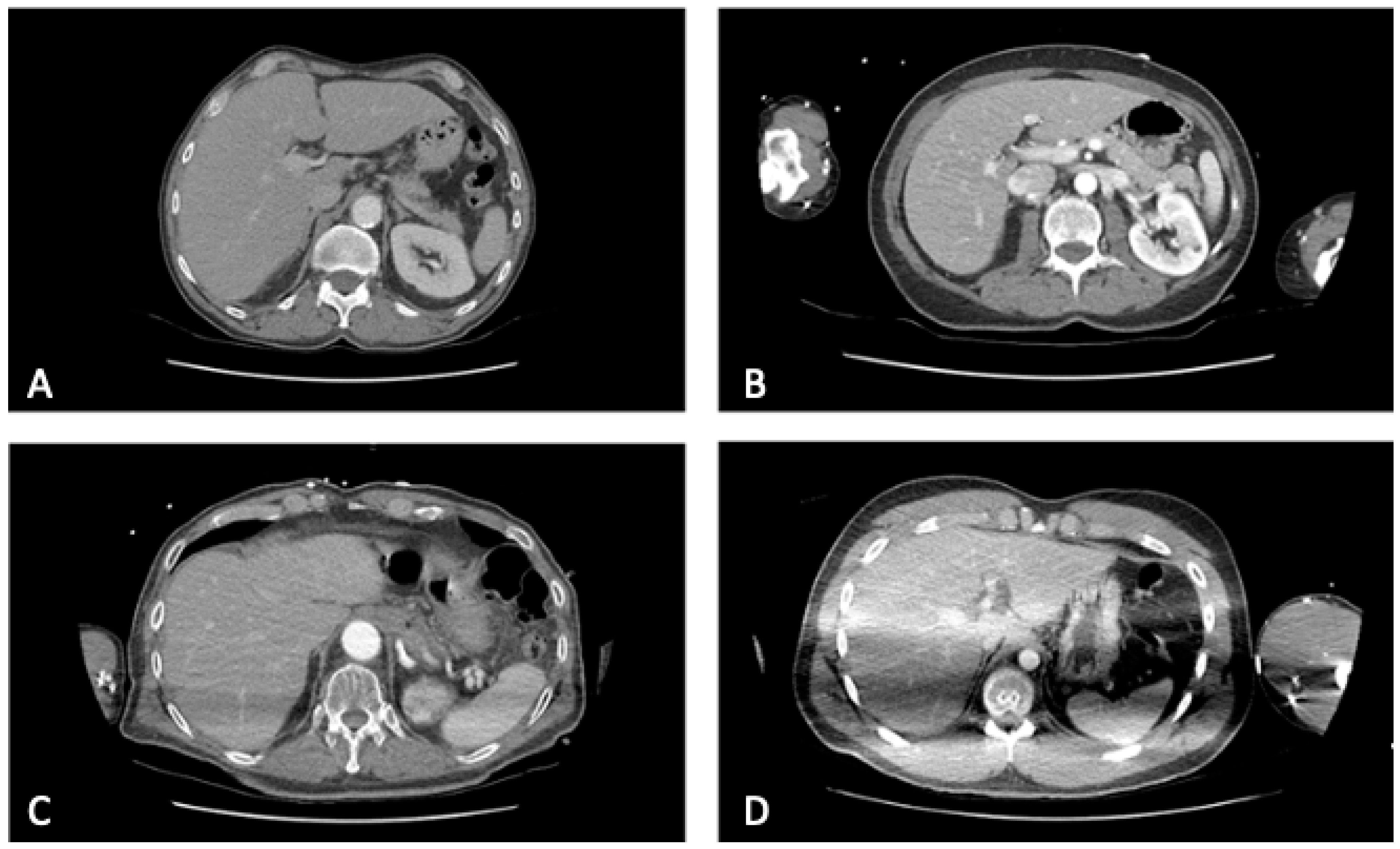
2.2. Image Quality
- = no artifacts
- = artifacts without impairment of the image quality
- = artifacts with a moderate impairment of the image quality
- = artifacts with a massive impairment of the image quality
2.3. Radiation Dose
2.4. Statistical Analysis
3. Results
3.1. Image Quality
3.2. Radiation Dose
4. Discussion
4.1. Image Quality
4.2. Radiation Dose
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kalender, W.A.; Seissler, W.; Klotz, E.; Vock, P. Spiral volumetric CT with single-breath-hold technique, continuous transport, and continuous scanner rotation. Radiology 1990, 176, 181–183. [Google Scholar] [CrossRef] [PubMed]
- Willemink, M.J.; Noel, P.B. The evolution of image reconstruction for CT-from filtered back projection to artificial intelligence. Eur. Radiol. 2019, 29, 2185–2195. [Google Scholar] [CrossRef] [PubMed]
- Piede, D. Dosisreduktion: CT-Untersuchungen „fast ohne“ Dosis. Radiopraxis 2015, 8, 19–28. [Google Scholar] [CrossRef][Green Version]
- Boas, F.E.; Fleischmann, D. CT artifacts: Causes and reduction techniques. Imaging Med. 2012, 4, 229–240. [Google Scholar] [CrossRef]
- Goeller, A.; Pogarell, T.; May, M.S.; Uder, M.; Dankerl, P. Evaluation of CT-Guided Ultra-Low-Dose Protocol for Injection Guidance in Preparation of MR-Arthrography of the Shoulder and Hip Joints in Comparison to Conventional and Low-Dose Protocols. Diagnostics 2021, 11, 1835. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, M.; Landini, N.; Sambataro, G.; Nardi, C.; Tofani, L.; Bruni, C.; Bellando-Randone, S.; Blagojevic, J.; Melchiorre, D.; Hughes, M.; et al. The role of chest CT in deciphering interstitial lung involvement: Systemic sclerosis versus COVID-19. Rheumatology 2022, 61, 1600–1609. [Google Scholar] [CrossRef] [PubMed]
- Ruaro, B.; Baratella, E.; Confalonieri, P.; Wade, B.; Marrocchio, C.; Geri, P.; Busca, A.; Pozzan, R.; Andrisano, A.G.; Cova, M.A.; et al. High-Resolution Computed Tomography: Lights and Shadows in Improving Care for SSc-ILD Patients. Diagnostics 2021, 11, 1960. [Google Scholar] [CrossRef]
- Huber-Wagner, S.; Lefering, R.; Qvick, L.M.; Korner, M.; Kay, M.V.; Pfeifer, K.J.; Reiser, M.; Mutschler, W.; Kanz, K.G.; Working Group on Polytrauma of the German Trauma, S. Effect of whole-body CT during trauma resuscitation on survival: A retrospective, multicentre study. Lancet 2009, 373, 1455–1461. [Google Scholar] [CrossRef]
- Hutter, M.; Woltmann, A.; Hierholzer, C.; Gartner, C.; Buhren, V.; Stengel, D. Association between a single-pass whole-body computed tomography policy and survival after blunt major trauma: A retrospective cohort study. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 73. [Google Scholar] [CrossRef]
- Larson, D.B.; Johnson, L.W.; Schnell, B.M.; Salisbury, S.R.; Forman, H.P. National trends in CT use in the emergency department: 1995–2007. Radiology 2011, 258, 164–173. [Google Scholar] [CrossRef]
- Kanz, K.G.; Paul, A.O.; Lefering, R.; Kay, M.V.; Kreimeier, U.; Linsenmaier, U.; Mutschler, W.; Huber-Wagner, S.; Trauma Registry of the German Trauma, S. Trauma management incorporating focused assessment with computed tomography in trauma (FACTT)—Potential effect on survival. J. Trauma Manag. Outcomes 2010, 4, 4. [Google Scholar] [CrossRef] [PubMed]
- Gunn, M.L.; Kool, D.R.; Lehnert, B.E. Improving Outcomes in the Patient with Polytrauma: A Review of the Role of Whole-Body Computed Tomography. Radiol. Clin. N. Am. 2015, 53, 639–656. [Google Scholar] [CrossRef] [PubMed]
- van den Hout, W.J.; van der Wilden, G.M.; Boot, F.; Idenburg, F.J.; Rhemrev, S.J.; Hoencamp, R. Early CT scanning in the emergency department in patients with penetrating injuries: Does it affect outcome? Eur. J. Trauma Emerg. Surg. 2018, 44, 607–614. [Google Scholar] [CrossRef]
- Huber-Wagner, S.; Kanz, K.G.; Hanschen, M.; van Griensven, M.; Biberthaler, P.; Lefering, R. Whole-body computed tomography in severely injured patients. Curr. Opin. Crit. Care 2018, 24, 55–61. [Google Scholar] [CrossRef]
- Geyer, L.L.; Koerner, M.; Wirth, S.; Mueck, F.G.; Reiser, M.F.; Linsenmaier, U. Polytrauma: Optimal imaging and evaluation algorithm. Semin. Musculoskelet. Radiol. 2013, 17, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Low, R.; Duber, C.; Schweden, F.; Lehmann, L.; Blum, J.; Thelen, M. Whole body spiral CT in primary diagnosis of patients with multiple trauma in emergency situations. RoFo Fortschr. Geb. Rontgenstrahlen Nukl. 1997, 166, 382–388. [Google Scholar] [CrossRef]
- Linsenmaier, U.; Geyer, L.L.; Korner, M.; Reiser, M.; Wirth, S. Importance of multidetector CT imaging in multiple trauma. Radiologe 2014, 54, 861–871. [Google Scholar] [CrossRef] [PubMed]
- Höfer, C.; Lefering, R. Jahresbericht 2021—TraumaRegister DGU für das Unfalljahr 2020. Available online: https://www.traumaregister-dgu.de/fileadmin/user_upload/TR-DGU_Jahresbericht_2021.pdf (accessed on 31 May 2022).
- Heyer, C.M.; Rduch, G.; Kagel, T.; Lemburg, S.P.; Theisinger, A.; Bauer, T.T.; Muhr, G.; Nicolas, V. Prospective randomized trial of a modified standard multislice CT protocol for the evaluation of multiple trauma patients. RoFo Fortschr. Geb. Rontgenstrahlen Nukl. 2005, 177, 242–249. [Google Scholar] [CrossRef]
- Tien, H.C.; Tremblay, L.N.; Rizoli, S.B.; Gelberg, J.; Spencer, F.; Caldwell, C.; Brenneman, F.D. Radiation exposure from diagnostic imaging in severely injured trauma patients. J. Trauma 2007, 62, 151–156. [Google Scholar] [CrossRef]
- Kahn, J.; Grupp, U.; Kaul, D.; Boning, G.; Lindner, T.; Streitparth, F. Computed tomography in trauma patients using iterative reconstruction: Reducing radiation exposure without loss of image quality. Acta Radiol. 2016, 57, 362–369. [Google Scholar] [CrossRef]
- Karlo, C.; Gnannt, R.; Frauenfelder, T.; Leschka, S.; Bruesch, M.; Wanner, G.A.; Alkadhi, H. Whole-body CT in polytrauma patients: Effect of arm positioning on thoracic and abdominal image quality. Emerg. Radiol. 2011, 18, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Kahn, J.; Grupp, U.; Maurer, M. How does arm positioning of polytraumatized patients in the initial computed tomography (CT) affect image quality and diagnostic accuracy? Eur. J. Radiol. 2014, 83, e67–e71. [Google Scholar] [CrossRef] [PubMed]
- Brink, M.; de Lange, F.; Oostveen, L.J.; Dekker, H.M.; Kool, D.R.; Deunk, J.; Edwards, M.J.; van Kuijk, C.; Kamman, R.L.; Blickman, J.G. Arm raising at exposure-controlled multidetector trauma CT of thoracoabdominal region: Higher image quality, lower radiation dose. Radiology 2008, 249, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Hickethier, T.; Mammadov, K.; Baessler, B.; Lichtenstein, T.; Hinkelbein, J.; Smith, L.; Plum, P.S.; Chon, S.H.; Maintz, D.; Chang, D.H. Whole-body computed tomography in trauma patients: Optimization of the patient scanning position significantly shortens examination time while maintaining diagnostic image quality. Ther. Clin. Risk Manag. 2018, 14, 849–859. [Google Scholar] [CrossRef] [PubMed]
- Flammia, F.; Chiti, G.; Trinci, M.; Danti, G.; Cozzi, D.; Grassi, R.; Palumbo, P.; Bruno, F.; Agostini, A.; Fusco, R.; et al. Optimization of CT protocol in polytrauma patients: An update. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 2543–2555. [Google Scholar] [CrossRef]
- Hoppe, H.; Vock, P.; Bonel, H.M.; Ozdoba, C.; Gralla, J. A novel multiple-trauma CT-scanning protocol using patient repositioning. Emerg. Radiol. 2006, 13, 123–128. [Google Scholar] [CrossRef]
- Bayer, J.; Pache, G.; Strohm, P.C.; Zwingmann, J.; Blanke, P.; Baumann, T.; Sudkamp, N.P.; Hammer, T. Influence of arm positioning on radiation dose for whole body computed tomography in trauma patients. J. Trauma 2011, 70, 900–905. [Google Scholar] [CrossRef]
- Geyer, L.L.; Korner, M.; Harrieder, A.; Mueck, F.G.; Deak, Z.; Wirth, S.; Linsenmaier, U. Dose reduction in 64-row whole-body CT in multiple trauma: An optimized CT protocol with iterative image reconstruction on a gemstone-based scintillator. Br. J. Radiol. 2016, 89, 20160003. [Google Scholar] [CrossRef]

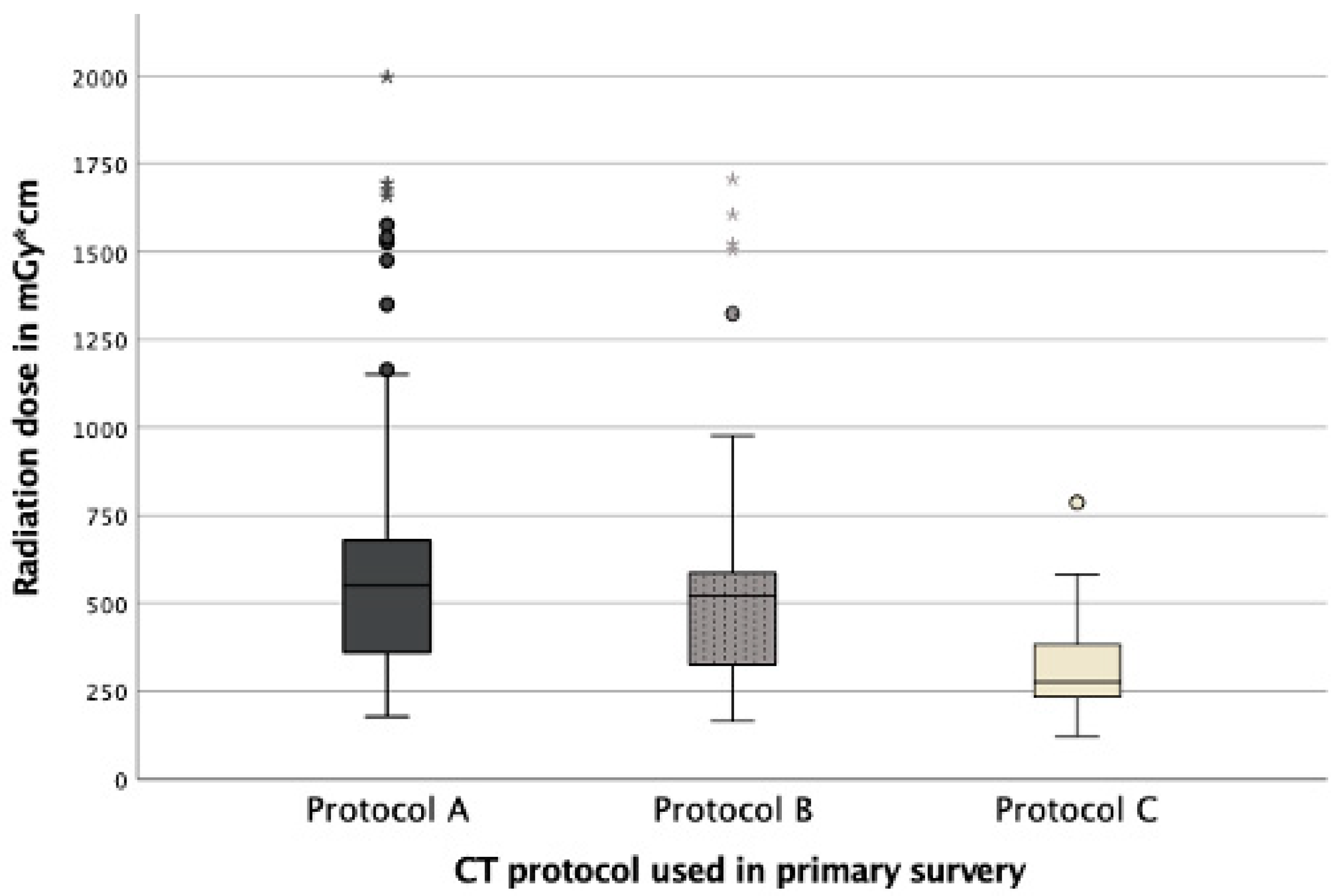
| Protocol A | Protocol B | Protocol C | p-Value * | p-Value ** | |
|---|---|---|---|---|---|
| Numbers (n) | 115 | 168 | 71 | ||
| Sex m/f | 76 (66.09%)/ 39 (33.91%) | 97 (57.40%)/ 72 (42.60%) | 48 (67.6%)/ 23 (32.4%) | 0.131 | 0.290 |
| Age mean (age range) | 58 (14–97) | 52 (13–97) | 52 (19–91) | 0.019 | 0.308 |
| Artifacts mean ± SD | 2.6 ± 0.9 | 1.0 ± 0 | 1.0 ± 0 | <0.001 | <0.001 |
| Radiation dose in mGy*cm median (minimum–maximum) | 550 (178–1997) | 521 (165–1706) | 276 (122–787) | 0.123 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graef, J.; Bressem, K.K.; Asbach, P.; Hamm, B.; Niehues, S.M. Changing the Patient’s Position: Pitfalls and Benefits for Radiation Dose and Image Quality of Computed Tomography in Polytrauma. Diagnostics 2022, 12, 2661. https://doi.org/10.3390/diagnostics12112661
Graef J, Bressem KK, Asbach P, Hamm B, Niehues SM. Changing the Patient’s Position: Pitfalls and Benefits for Radiation Dose and Image Quality of Computed Tomography in Polytrauma. Diagnostics. 2022; 12(11):2661. https://doi.org/10.3390/diagnostics12112661
Chicago/Turabian StyleGraef, Jessica, Keno K. Bressem, Patrick Asbach, Bernd Hamm, and Stefan M. Niehues. 2022. "Changing the Patient’s Position: Pitfalls and Benefits for Radiation Dose and Image Quality of Computed Tomography in Polytrauma" Diagnostics 12, no. 11: 2661. https://doi.org/10.3390/diagnostics12112661
APA StyleGraef, J., Bressem, K. K., Asbach, P., Hamm, B., & Niehues, S. M. (2022). Changing the Patient’s Position: Pitfalls and Benefits for Radiation Dose and Image Quality of Computed Tomography in Polytrauma. Diagnostics, 12(11), 2661. https://doi.org/10.3390/diagnostics12112661







