Investigation of the New Advantages of Colonoscope Insertion with an Endoscopic Position Detection Unit
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Colonoscopes and Other Instruments
2.3. Colonoscopy
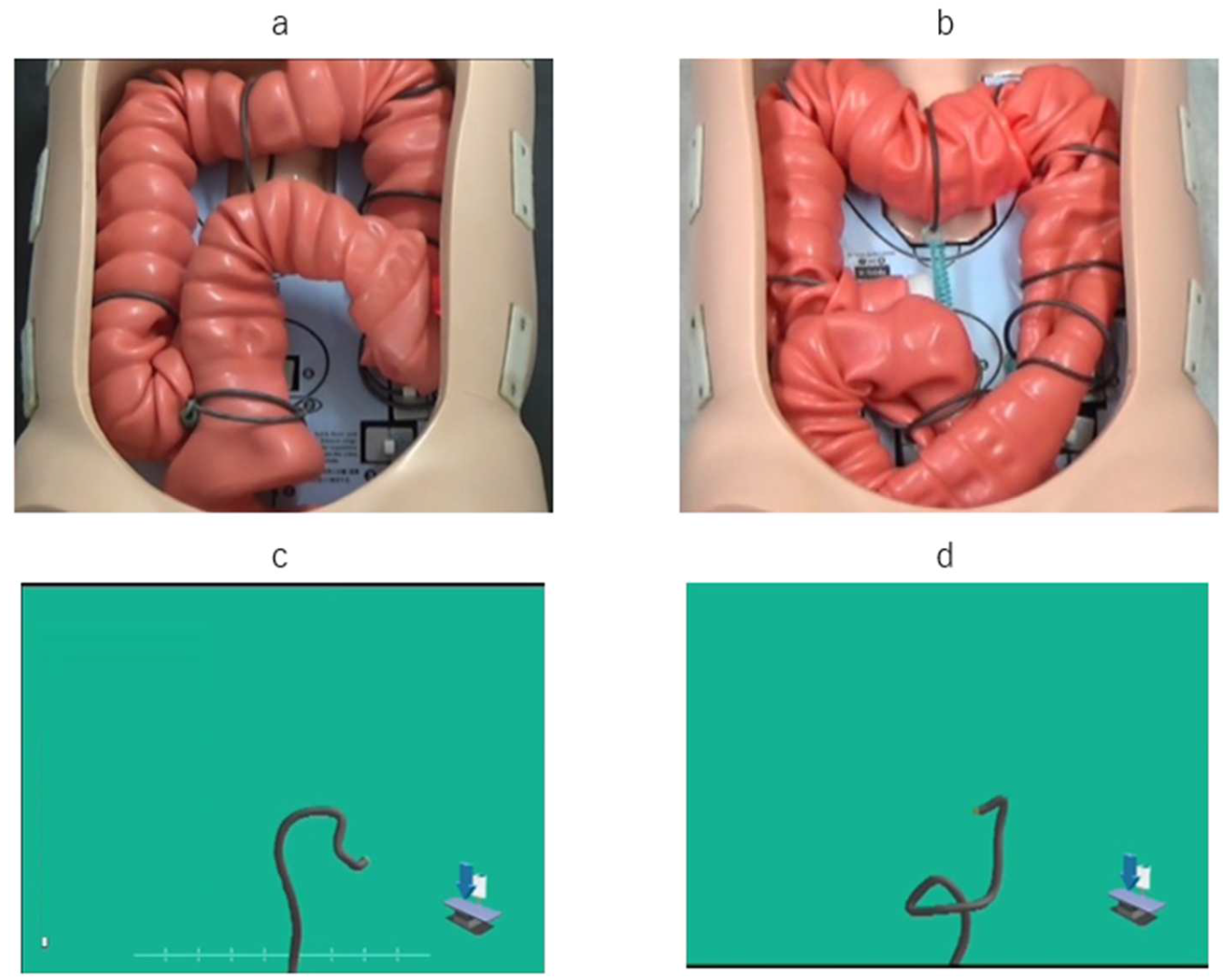
2.4. UPD System Pictures and Explanation
2.5. Study Endpoints
2.6. Statistical Analysis
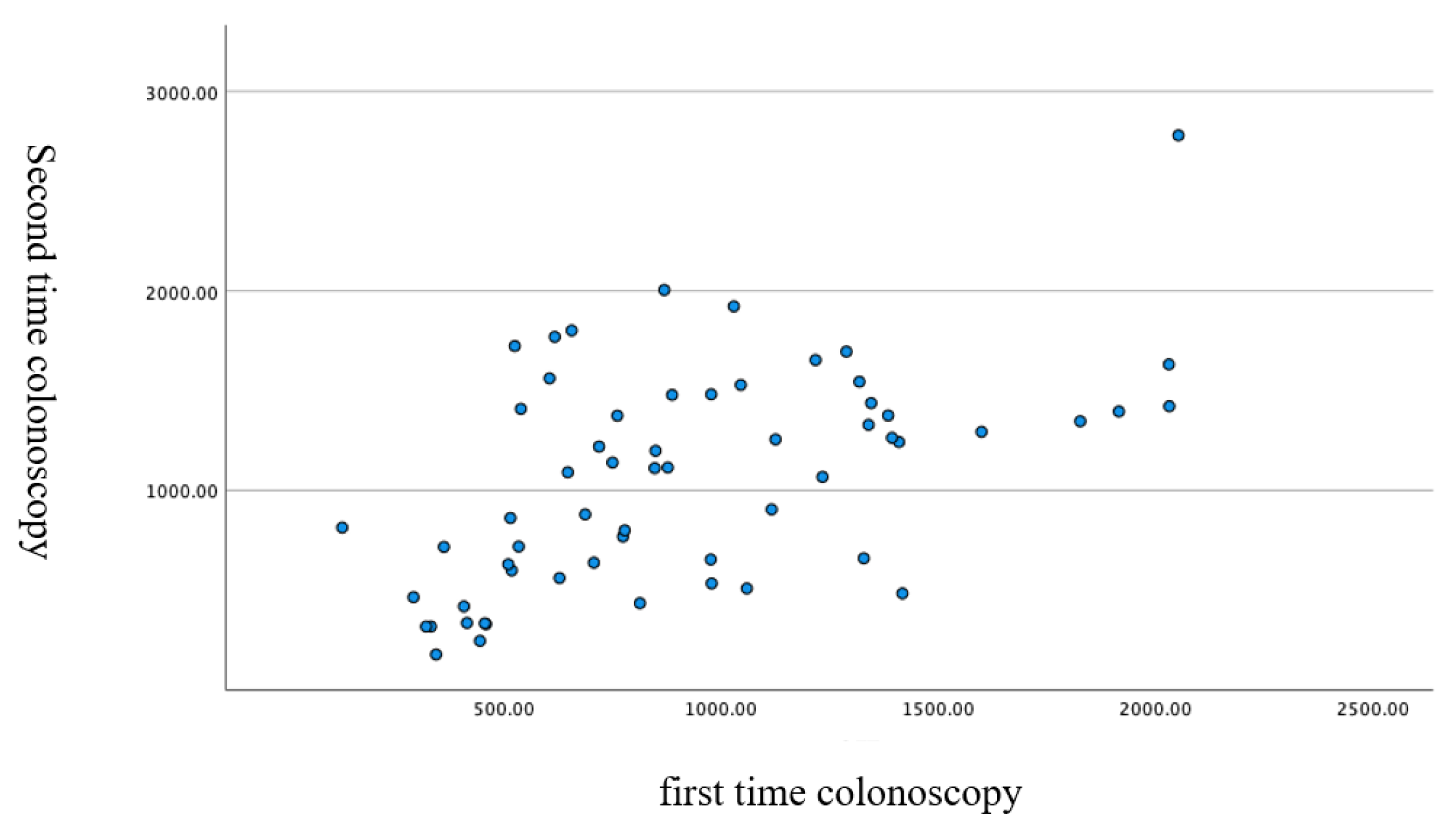
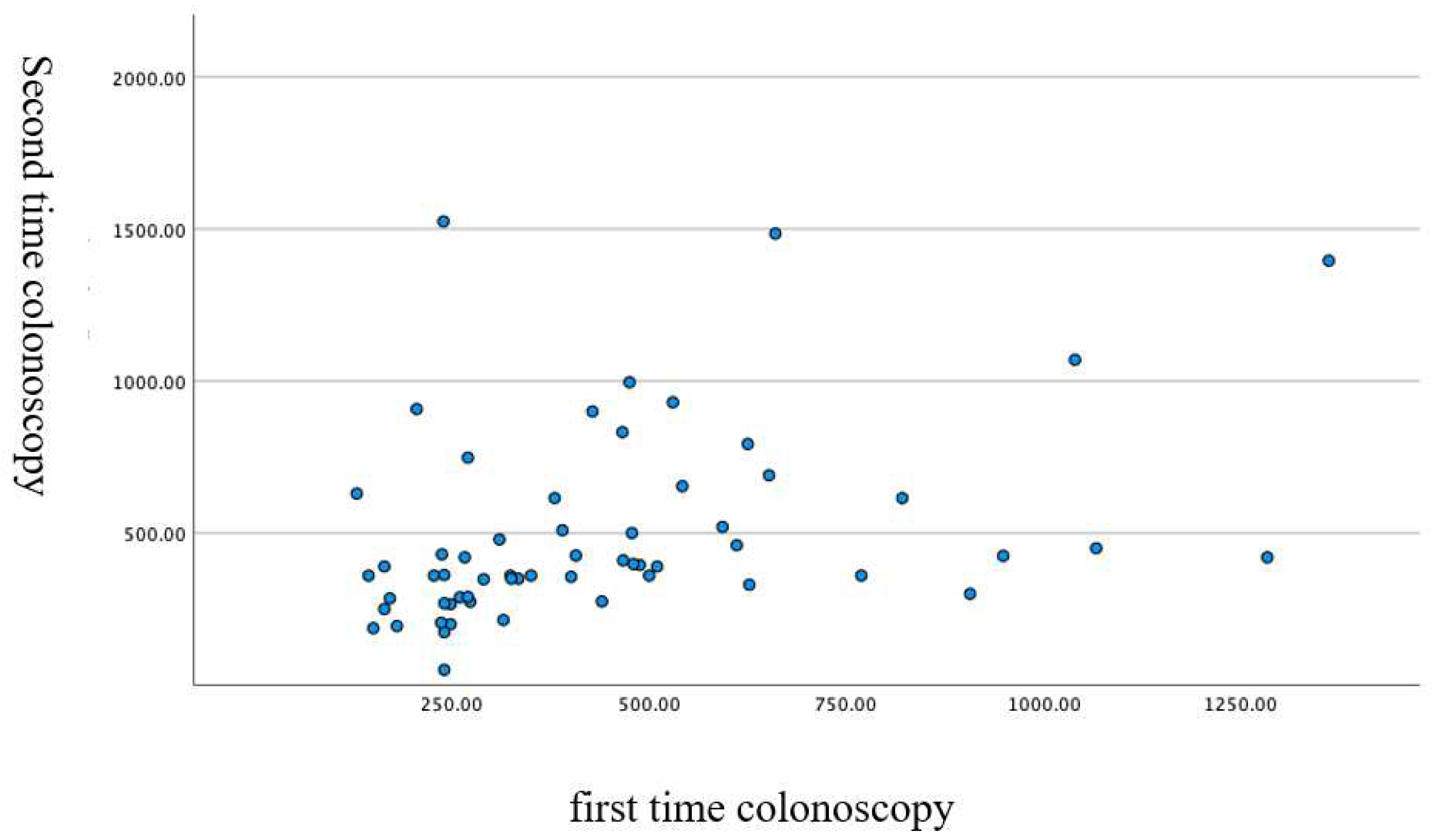
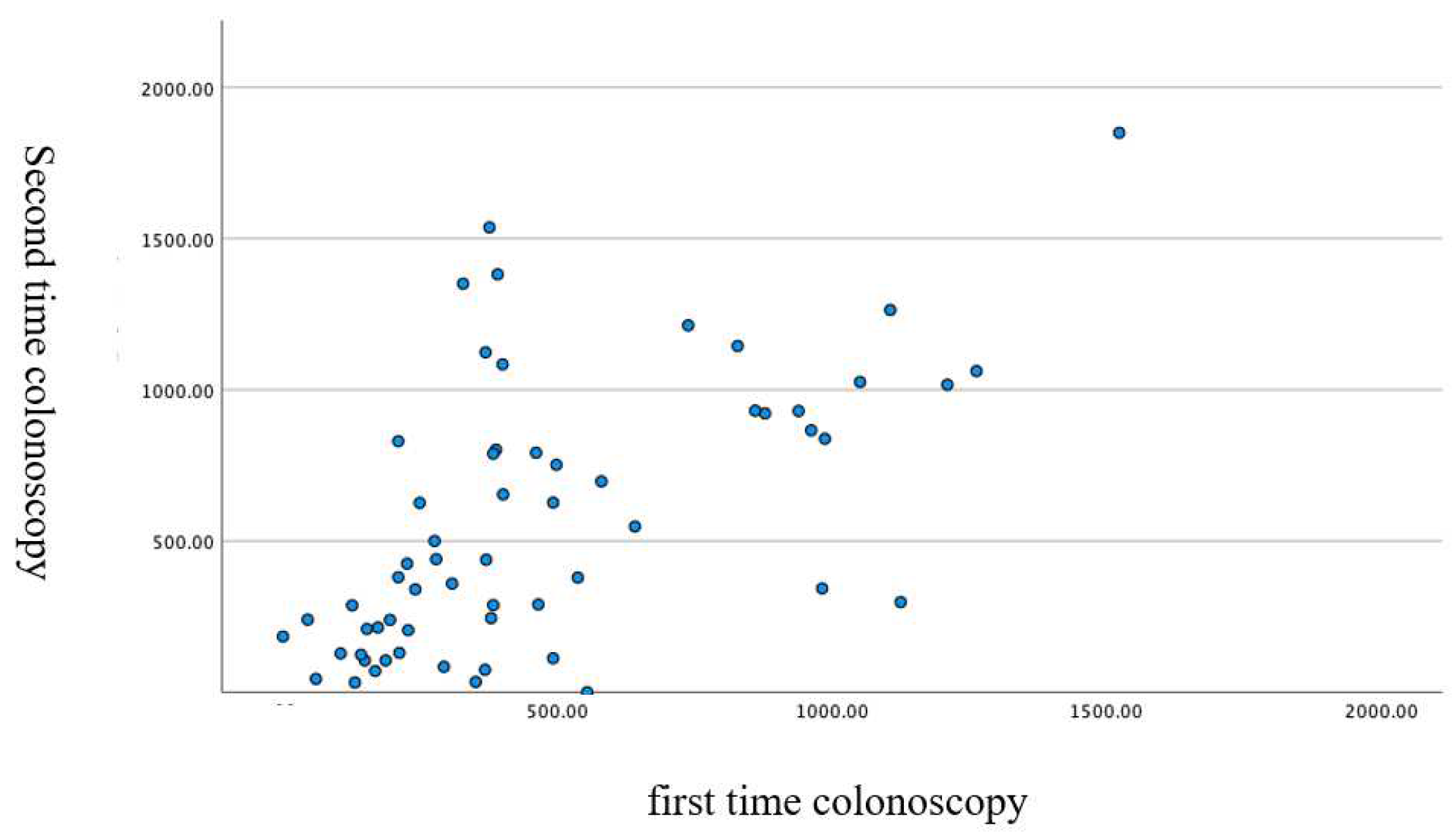
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cancer Information Service at National Cancer Research Center: Cancer Registration and Statistics. Available online: http://ganjoho.jp/reg_stat (accessed on 4 July 2021).
- Mandel, J.S.; Church, T.R.; Bond, J.H.; Ederer, F.; Geisser, M.S.; Mongin, S.J.; Snover, D.C.; Schuman, L.M. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N. Engl. J. Med. 2000, 343, 1603–1607. [Google Scholar] [CrossRef] [PubMed]
- Atkin, W.S.L.; Edwards, R.; Kralj-Hans, I.; Wooldrage, K.; Hart, A.R.; Northover, J.M.; Parkin, D.M.; Wardle, J.; Duffy, S.W.; Cuzick, J. UK Flexible Sigmoidoscopy Trial Investigators. Once-only flexible sigmoidoscopy screening in prevention of colorectal cancer: A multicentre randomised controlled trial. Lancet 2010, 375, 1624–1633. [Google Scholar] [CrossRef]
- Zauber, A.G.; Winawer, S.J.; O'Brien, M.J.; Lansdorp-Vogelaar, I.; van Ballegooijen, M.; Hankey, B.F.; Shi, W.; Bond, J.H.; Schapiro, M.; Panish, J.F.; et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N. Engl. J. Med. 2012, 366, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Edwards, B.K.; Ward, E.; Kohler, B.A.; Eheman, C.; Zauber, A.G.; Anderson, R.N.; Jemal, A.; Schymura, M.J.; Lansdorp-Vogelaar, I.; Seeff, L.C.; et al. Annual report to the nation on the status of cancer, 1975–2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer 2010, 116, 544–573. [Google Scholar] [CrossRef]
- Matsuda, T. Expectations for and challenges in population-based endoscopic gastric and colorectal cancer screening. Dig. Endosc. 2022, 34 (Suppl. 2), 15–19. [Google Scholar] [CrossRef]
- Shah, S.G.; Brooker, J.C.; Williams, C.B.; Thapar, C.; Saunders, B.P. Effect of magnetic endoscope imaging on colonoscopy performance: A randomised controlled trial. Lancet 2000, 356, 1718–1722. [Google Scholar] [CrossRef]
- Furuta, T.; Kato, M.; Ito, T.; Inaba, T.; Komura, N.; katanuma, A.; Shimizu, S.; Hiyama, T.; Matsuda, K.; Yasuda, I.; et al. The 6th nationwide surveillance of accidents during intestinal endoscopy in 5 years from 2008 through 2012. Gastroenterol. Endosc. 2017, 58, 1466–1491. (In Japanese) [Google Scholar]
- Yamasaki, A.; Chino, A.; Ide, D.; Taegai, Y.; Igarashi, M.; Saito, S. The intelligent insert method for difficult cases each of three colorectal scope. J. Colon. Exam. 2018, 34, 102–110. (In Japanese) [Google Scholar]
- Shah, H.A.; Paszat, L.F.; Saskin, R.; Stukel, T.A.; Linda, R. Factors associated with incomplete colonoscopy: A population based study. Gastroenterology 2007, 132, 2297–2303. [Google Scholar] [CrossRef]
- Jaruvongvanich, V.; Sempokuya, T.; Laoveeravat, P.; Ungprasert, P. Risk factors associated with longer cecal insertion time: A systematic review and meta-analysis. Int. J. Colorectal. Dis. 2018, 33, 359–365. [Google Scholar] [CrossRef]
- Xie, Q.; Chen, B.; Liu, L.; Gan, H. Does the variable-stiffness colonoscope makes colonoscopy easier? A meta-analysis of the efficacy of the variable stiffness colonoscope compared with the standard adult colonoscope. BMC Gastroenterol. 2012, 24, 151. [Google Scholar] [CrossRef] [PubMed]
- Othman, M.O.; Bradley, A.G.; Choudhary, A.; Hoffman, R.M.; Roy, P.K. Variable stiffness colonoscope versus regular adult colonoscope: Meta-analysis of randomized controlled trials. Endoscopy 2009, 41, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Sofi, A.A.; Nawras, A.; Khan, M.A.; Howden, C.W.; Lee, W.M. Meta-analysis of the performance of ultrathin vs. standard colonoscopes. Endoscopy 2017, 49, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Ito, S.; Shigiyama, F.; Kitagawa, T.; Hirahata, K.; Tominaga, K.; Maetani, I. A prospective randomized study on the benefits of a new small caliber colonoscope. Endoscopy 2012, 44, 746–753. [Google Scholar] [CrossRef] [PubMed]
- Memon, M.A.; Memon, B.; Yunus, R.M.; Khan, S. Carbon dioxide versus air insufflation for elective colonoscopy: A meta-analysis and systematic review of randomized controlled trials. Surg. Laparosc. Endosc. Percutan. Tech. 2016, 26, 102–116. [Google Scholar] [CrossRef]
- Wu, J.; Hu, B. The role of carbon dioxide insufflation in colonoscopy: A systematic review and meta-analysis. Endoscopy 2012, 44, 128–136. [Google Scholar] [CrossRef]
- Kondo, S.; Yamaji, Y.; Watabe, H.; Yamada, A.; Sugimoto, T.; Ohta, M.; Ogura, K.; Okamoto, M.; Yoshida, H.; Kawabe, T.; et al. A randomized controlled trial evaluating the usefulness of a transparent hood attached to the tip of the colonoscope. Am. J. Gastroenterol. 2007, 102, 75–81. [Google Scholar] [CrossRef]
- Mizukami, T.; Yokoyama, A.; Imaeda, H.; Kumai, K. Collapse-submergence method: Simple colonoscopic technique combining water infusion with complete air removal from the rectosigmoid colon. Dig. Endosc. 2007, 19, 43–48. [Google Scholar] [CrossRef]
- Anbefalinger Vedrørende Screening for Tyk-Og Endetarmskræft © Sundhedsstyrelsen, 2010 og 2012. Sundhedsstyrelsen, Axel Heides Gade 1, 2300 København S. Available online: http://www.sst.dk (accessed on 29 April 2019).
- Saito, Y.; Oka, S.; Kawamura, T.; Shimoda, R.; Sekiguchi, M.; Tamai, N.; Hotta, K.; Matsuda, T.; Misawa, M.; Tanaka, S.; et al. Colonoscopy screening and surveillance guidelines. Dig. Endosc. 2021, 33, 486–519. [Google Scholar] [CrossRef]
- Cheung, H.Y.; Chung, C.C.; Kwok, S.Y.; Tsang, W.W.; Li, M.K. Improvement in colonoscopy performance with adjunctive magnetic endoscope imaging: A randomized controlled trial. Endoscopy 2006, 38, 214–217. [Google Scholar] [CrossRef]
- Hoff, G.; Bretthauer, M.; Dahler, S.; Huppertz-Hauss, G.; Sauar, J.; Paulsen, J.; Seip, B.; Moritz, V. Improvement in caecal insertion rate and pain reduction by using 3-dimensional magnetic imaging for unsedated colonoscopy: A randomized trial of patients referred for colonoscopy. Scand. J. Gastroenterol. 2007, 42, 885–889. [Google Scholar] [CrossRef] [PubMed]
- Jess, P.; Bulut, O.; Almasi, A.; Waaddegaard, P. The usefulness of a magnetic endoscope locating device in colonoscopy in daily practice: A prospective case-controlled study. Surg. Endosc. 2009, 23, 1353–1355. [Google Scholar] [CrossRef] [PubMed]
- Fukuzawa, M.; Uematsu, J.; Kono, S.; Suzuki, S.; Sato, T.; Yagi, N.; Tsuji, Y.; Yagi, K.; Kusano, C.; Gotoda, T.; et al. Clinical impact of endoscopy position detecting unit (UPD-3) for a non-sedated colonoscopy. World J. Gastroenterol. 2015, 21, 4903–4910. [Google Scholar] [CrossRef] [PubMed]
- Sato, K.; Fujinuma, S.; Sakai, Y. Evaluation of the looping formation and pain during insertion into the cecum in colonoscopy. Dig. Endosc. 2006, 18, 181–187. [Google Scholar] [CrossRef]


| Second | |||||||
|---|---|---|---|---|---|---|---|
| First | SDJ | Straight | N-loop | alpha | Reverse-alpha | Other | |
| Straight | 10 | 1 | 1 | 0 | 0 | ||
| N-loop | 1 | 30 | 3 | 1 | 0 | ||
| Alpha | 0 | 3 | 5 | 1 | 0 | ||
| Reverse | 1 | 1 | 0 | 2 | 0 | ||
| Other | 0 | 0 | 1 | 0 | 0 | ||
| Hepatic flexure | Right rotation | Positional change | Push | Other | |||
| Right rotation | 30 | 7 | 0 | 0 | |||
| Positional change | 2 | 1 | 1 | 0 | |||
| Push forward | 5 | 4 | 10 | 0 | |||
| Other | 0 | 0 | 0 | 1 | |||
| Overall | Straight | N-Loop | Alpha | Reverse-Alpha | Other | p Value | ||
|---|---|---|---|---|---|---|---|---|
| n | 122 | 24 | 70 | 19 | 8 | 1 | ||
| Age, mean ± SD | 69.7 ± 10.5 | 66.7 ± 13.7 | 70.5 ± 9.8 | 72.1 ± 4.9 | 67.4 ± 13.9 | 62.0 | 0.365 | |
| Sex | Male/female | 110/12 | 20/4 | 64/6 | 18/1 | 7/1 | 1/0 | 0.734 |
| BMI, mean ± SD | 24.6 ± 2.8 | 23.6 ± 1.7 | 25.1 ± 3.1 | 24.6 ± 2.5 | 23.1 ± 1.9 | 22.6 | 0.103 | |
| History of surgery | No/yes | 76/46 | 15/9 | 39/31 | 13/6 | 8/0 | 1/0 | 0.134 |
| CS times | First/second | 61/61 | 12/12 | 36/34 | 9/10 | 4/4 | 1/0 | 0.902 |
| HFP | R/PO/PU/O | 74/16/30/2 | 19/2/3/0 | 40/10/20/0 | 11/4/4/0 | 4/0/2/2 | 0/0/1/0 | <0.001 |
| Scope used | H190/H290 | 77/45 | 14/10 | 45/25 | 10/9 | 7/1 | 1/0 | 0.791 |
| TCT | Seconds | 990 ± 511 | 667 ± 447 | 1069 ± 517 | 1044 ± 439 | 1188 ± 524 | 1060 | 0.012 |
| A to F | Seconds | 470 ± 297 | 321 ± 250 | 510 ± 258 | 432 ± 296 | 651 ± 596 | 907 | 0.015 |
| S to C | Seconds | 520 ± 402 | 346 ± 302 | 558 ± 402 | 611 ± 415 | 537 ± 585 | 153 | 0.136 |
| Overall | Right Rotation | Positional Change | Push | Others | p Value | ||
|---|---|---|---|---|---|---|---|
| n | 122 | 74 | 16 | 30 | 2 | ||
| Age | 69.7 ± 10.5 | 69.1 ± 9.9 | 69.9 ± 11.7 | 71.1 ± 11.7 | 71.0 | 0.856 | |
| Sex | Male/female | 110/12 | 69/5 | 16/0 | 23/7 | 2/0 | 0.03 |
| BMI | 24.6 ± 2.8 | 24.5 ± 2.7 | 25.9 ± 3.6 | 24.2 ± 2.4 | 21.5 | 0.082 | |
| Surgical history | No/yes | 76/46 | 49/25 | 11/5 | 14/16 | 2/0 | 0.165 |
| CS times | First/second | 61/61 | 37/37 | 4/12 | 19/11 | 1/1 | 0.105 |
| SDJ pattern | S/N/A/RA/O | 24/70/19/8/1 | 19/40/11/4/0 | 2/10/4/0/0 | 3/20/4/2/1 | 0/0/0/2/0 | <0.001 |
| Scope used | H190/H290 | 77/45 | 46/28 | 7/9 | 23/6 | 1/1 | 0.169 |
| TCS time | Seconds | 990 ± 511 | 777 ± 414 | 1260 ± 356 | 1373 ± 517 | <0.001 | |
| A to F | Seconds | 470 ± 297 | 441 ± 298 | 509 ± 237 | 521 ± 321 | 0.4 | |
| S to C | Seconds | 520 ± 402 | 336 ± 272 | 750 ± 316 | 851 ± 402 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawai, T.; Kawai, Y.; Akimoto, Y.; Hamada, M.; Iwata, E.; Niikura, R.; Nagata, N.; Sugimoto, M.; Yanagisawa, K.; Yamagishi, T.; et al. Investigation of the New Advantages of Colonoscope Insertion with an Endoscopic Position Detection Unit. Diagnostics 2022, 12, 2610. https://doi.org/10.3390/diagnostics12112610
Kawai T, Kawai Y, Akimoto Y, Hamada M, Iwata E, Niikura R, Nagata N, Sugimoto M, Yanagisawa K, Yamagishi T, et al. Investigation of the New Advantages of Colonoscope Insertion with an Endoscopic Position Detection Unit. Diagnostics. 2022; 12(11):2610. https://doi.org/10.3390/diagnostics12112610
Chicago/Turabian StyleKawai, Takashi, Yusuke Kawai, Yoshika Akimoto, Mariko Hamada, Eri Iwata, Ryota Niikura, Naoyoshi Nagata, Mitsushige Sugimoto, Kyosuke Yanagisawa, Tetsuya Yamagishi, and et al. 2022. "Investigation of the New Advantages of Colonoscope Insertion with an Endoscopic Position Detection Unit" Diagnostics 12, no. 11: 2610. https://doi.org/10.3390/diagnostics12112610
APA StyleKawai, T., Kawai, Y., Akimoto, Y., Hamada, M., Iwata, E., Niikura, R., Nagata, N., Sugimoto, M., Yanagisawa, K., Yamagishi, T., Fukuzawa, M., & Itoi, T. (2022). Investigation of the New Advantages of Colonoscope Insertion with an Endoscopic Position Detection Unit. Diagnostics, 12(11), 2610. https://doi.org/10.3390/diagnostics12112610








