Current Evidence and Theories in Understanding the Relationship between Cognition and Depression in Childhood and Adolescence: A Narrative Review
Abstract
1. Introduction
Aims
2. Materials and Methods
Search Strategy and Study Selection
3. Results
3.1. The Trait Hypothesis
3.2. The Scar Hypothesis
3.3. The State Hypothesis
3.4. Cognitive Vulnerability as an Index of Hot Cognitive Dimension in Depression: The Role of Cognitive Biases
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Paus, T.; Keshavan, M.; Giedd, J.N. Why Do Many Psychiatric Disorders Emerge during Adolescence? Nat. Rev. Neurosci. 2008, 9, 947–957. [Google Scholar] [CrossRef] [PubMed]
- Paus, T. Mapping Brain Maturation and Cognitive Development during Adolescence. Trends Cogn. Sci. 2005, 9, 60–68. [Google Scholar] [CrossRef]
- Pine, D.S.; Cohen, E.; Cohen, P.; Brook, J. Adolescent Depressive Symptoms as Predictors of Adult Depression: Moodiness or Mood Disorder? Am. J. Psychiatry 1999, 156, 133–135. [Google Scholar] [CrossRef] [PubMed]
- Lewinsohn, P.M.; Rohde, P.; Seeley, J.R.; Klein, D.N.; Gotlib, I.H. Natural Course of Adolescent Major Depressive Disorder in a Community Sample: Predictors of Recurrence in Young Adults. Am. J. Psychiatry 2000, 157, 1584–1591. [Google Scholar] [CrossRef] [PubMed]
- Fergusson, D.M.; Horwood, L.J.; Ridder, E.M.; Beautrais, A.L. Subthreshold Depression in Adolescence and Mental Health Outcomes in Adulthood. Arch. Gen. Psychiatry 2005, 62, 66–72. [Google Scholar] [CrossRef]
- Malhotra, S.; Sahoo, S. Antecedents of Depression in Children and Adolescents. Ind. Psychiatry J. 2018, 27, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Aalto-Setälä, T.; Marttunen, M.; Tuulio-Henriksson, A.; Poikolainen, K.; Lönnqvist, J. Depressive Symptoms in Adolescence as Predictors of Early Adulthood Depressive Disorders and Maladjustment. Am. J. Psychiatry 2002, 159, 1235–1237. [Google Scholar] [CrossRef]
- Marmorstein, N.R. Longitudinal Associations between Alcohol Problems and Depressive Symptoms: Early Adolescence through Early Adulthood. Alcohol. Clin. Exp. Res. 2009, 33, 49–59. [Google Scholar] [CrossRef]
- Edwards, A.C.; Joinson, C.; Dick, D.M.; Kendler, K.S.; Macleod, J.; Munafò, M.; Hickman, M.; Lewis, G.; Heron, J. The Association between Depressive Symptoms from Early to Late Adolescence and Later Use and Harmful Use of Alcohol. Eur. Child Adolesc. Psychiatry 2014, 23, 1219–1230. [Google Scholar] [CrossRef]
- Bora, E.; Binnur Akdede, B.; Alptekin, K. Neurocognitive Impairment in Deficit and Non-Deficit Schizophrenia: A Meta-Analysis. Psychol. Med. 2017, 47, 2401–2413. [Google Scholar] [CrossRef]
- Rock, P.L.; Roiser, J.P.; Riedel, W.J.; Blackwell, A.D. Cognitive Impairment in Depression: A Systematic Review and Meta-Analysis. Psychol. Med. 2014, 44, 2029–2040. [Google Scholar] [CrossRef] [PubMed]
- Bortolato, B.; Miskowiak, K.W.; Köhler, C.A.; Vieta, E.; Carvalho, A.F. Cognitive Dysfunction in Bipolar Disorder and Schizophrenia: A Systematic Review of Meta-Analyses. Neuropsychiatr. Dis. Treat. 2015, 11, 3111–3125. [Google Scholar] [CrossRef] [PubMed]
- Shin, N.Y.; Lee, T.Y.; Kim, E.; Kwon, J.S. Cognitive Functioning in Obsessive-Compulsive Disorder: A Meta-Analysis. Psychol. Med. 2014, 44, 1121–1130. [Google Scholar] [CrossRef] [PubMed]
- Reville, M.-C.; O’Connor, L.; Frampton, I. Literature Review of Cognitive Neuroscience and Anorexia Nervosa. Curr. Psychiatry Rep. 2016, 18, 18. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Deste, G.; Smieskova, R.; Barlati, S.; Yung, A.R.; Howes, O.; Stieglitz, R.-D.; Vita, A.; McGuire, P.; Borgwardt, S. Cognitive Functioning in Prodromal Psychosis: A Meta-Analysis. Arch. Gen. Psychiatry 2012, 69, 562–571. [Google Scholar] [CrossRef]
- Lee, R.S.C.; Hermens, D.F.; Porter, M.A.; Redoblado-Hodge, M.A. A Meta-Analysis of Cognitive Deficits in First-Episode Major Depressive Disorder. J. Affect. Disord. 2012, 140, 113–124. [Google Scholar] [CrossRef]
- Trotta, A.; Murray, R.M.; MacCabe, J.H. Do Premorbid and Post-Onset Cognitive Functioning Differ between Schizophrenia and Bipolar Disorder? A Systematic Review and Meta-Analysis. Psychol. Med. 2015, 45, 381–394. [Google Scholar] [CrossRef]
- Bora, E.; Pantelis, C. Meta-Analysis of Cognitive Impairment in First-Episode Bipolar Disorder: Comparison with First-Episode Schizophrenia and Healthy Controls. Schizophr. Bull. 2015, 41, 1095–1104. [Google Scholar] [CrossRef]
- Allott, K.; Liu, P.; Proffitt, T.-M.; Killackey, E. Cognition at Illness Onset as a Predictor of Later Functional Outcome in Early Psychosis: Systematic Review and Methodological Critique. Schizophr. Res. 2011, 125, 221–235. [Google Scholar] [CrossRef]
- Van Rheenen, T.E.; Rossell, S.L. Objective and Subjective Psychosocial Functioning in Bipolar Disorder: An Investigation of the Relative Importance of Neurocognition, Social Cognition and Emotion Regulation. J. Affect. Disord. 2014, 162, 134–141. [Google Scholar] [CrossRef]
- Cambridge, O.; Knight, M.; Mills, N.; Baune, B. The Clinical Relationship between Cognitive Impairment and Psychosocial Functioning in Major Depressive Disorder: A Systematic Review. Psychiatry Res. 2018, 269, 157–171. [Google Scholar] [CrossRef] [PubMed]
- Allott, K.; Proffitt, T.-M.; McGorry, P.D.; Pantelis, C.; Wood, S.J.; Cumner, M.; Brewer, W.J. Clinical Neuropsychology within Adolescent and Young-Adult Psychiatry: Conceptualizing Theory and Practice. Appl. Neuropsychol. Child 2013, 2, 47–63. [Google Scholar] [CrossRef]
- Keefe, R.S.E. The Longitudinal Course of Cognitive Impairment in Schizophrenia: An Examination of Data from Premorbid through Posttreatment Phases of Illness. J. Clin. Psychiatry 2014, 75 (Suppl. 2), 8–13. [Google Scholar] [CrossRef] [PubMed]
- Mohn-Haugen, C.R.; Mohn, C.; Larøi, F.; Teigset, C.M.; Øie, M.G.; Rund, B.R. A Systematic Review of Premorbid Cognitive Functioning and Its Timing of Onset in Schizophrenia Spectrum Disorders. Schizophr. Res. Cogn. 2022, 28, 100246. [Google Scholar] [CrossRef] [PubMed]
- Vita, A.; Barlati, S.; Ceraso, A.; Nibbio, G.; Ariu, C.; Deste, G.; Wykes, T. Effectiveness, Core Elements, and Moderators of Response of Cognitive Remediation for Schizophrenia: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Psychiatry 2021, 78, 848–858. [Google Scholar] [CrossRef] [PubMed]
- Vita, A.; Gaebel, W.; Mucci, A.; Sachs, G.; Barlati, S.; Giordano, G.M.; Nibbio, G.; Nordentoft, M.; Wykes, T.; Galderisi, S. European Psychiatric Association Guidance on Treatment of Cognitive Impairment in Schizophrenia. Eur. Psychiatry 2022, 65, e57. [Google Scholar] [CrossRef]
- Thapar, A.; Collishaw, S.; Pine, D.S.; Thapar, A.K. Depression in Adolescence. Lancet 2012, 379, 1056–1067. [Google Scholar] [CrossRef]
- Hankin, B.L.; Abramson, L.Y.; Moffitt, T.E.; Silva, P.A.; McGee, R.; Angell, K.E. Development of Depression from Preadolescence to Young Adulthood: Emerging Gender Differences in a 10-Year Longitudinal Study. J. Abnorm. Psychol. 1998, 107, 128–140. [Google Scholar] [CrossRef]
- Garber, J. Depression in Children and Adolescents: Linking Risk Research and Prevention. Am. J. Prev. Med. 2006, 31, 104–125. [Google Scholar] [CrossRef]
- Yaroslavsky, I.; Pettit, J.W.; Lewinsohn, P.M.; Seeley, J.R.; Roberts, R.E. Heterogeneous Trajectories of Depressive Symptoms: Adolescent Predictors and Adult Outcomes. J. Affect. Disord. 2013, 148, 391–399. [Google Scholar] [CrossRef]
- Chaiton, M.; Contreras, G.; Brunet, J.; Sabiston, C.M.; O’Loughlin, E.; Low, N.C.P.; Karp, I.; Barnett, T.A.; O’Loughlin, J. Heterogeneity of Depressive Symptom Trajectories through Adolescence: Predicting Outcomes in Young Adulthood. J. Can. Acad. Child Adolesc. Psychiatry 2013, 22, 96–105. [Google Scholar] [PubMed]
- Weavers, B.; Heron, J.; Thapar, A.K.; Stephens, A.; Lennon, J.; Bevan Jones, R.; Eyre, O.; Anney, R.J.; Collishaw, S.; Thapar, A.; et al. The Antecedents and Outcomes of Persistent and Remitting Adolescent Depressive Symptom Trajectories: A Longitudinal, Population-Based English Study. Lancet Psychiatry 2021, 8, 1053–1061. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Cha, D.S.; Soczynska, J.K.; Woldeyohannes, H.O.; Gallaugher, L.A.; Kudlow, P.; Alsuwaidan, M.; Baskaran, A. Cognitive Deficits and Functional Outcomes in Major Depressive Disorder: Determinants, Substrates, and Treatment Interventions. Depress. Anxiety 2013, 30, 515–527. [Google Scholar] [CrossRef] [PubMed]
- Vita, A.; Barlati, S. Depressione e Cognitività. Noos 2016, 22, 85–97. [Google Scholar] [CrossRef]
- Hammar, A.; Ardal, G. Cognitive Functioning in Major Depression—A Summary. Front. Hum. Neurosci. 2009, 3, 26. [Google Scholar] [CrossRef] [PubMed]
- Reppermund, S.; Ising, M.; Lucae, S.; Zihl, J. Cognitive Impairment in Unipolar Depression Is Persistent and Non-Specific: Further Evidence for the Final Common Pathway Disorder Hypothesis. Psychol. Med. 2009, 39, 603–614. [Google Scholar] [CrossRef]
- Bora, E.; Harrison, B.J.; Yücel, M.; Pantelis, C. Cognitive Impairment in Euthymic Major Depressive Disorder: A Meta-Analysis. Psychol. Med. 2013, 43, 2017–2026. [Google Scholar] [CrossRef]
- Ahern, E.; Bockting, C.L.H.; Semkovska, M. A Hot-Cold Cognitive Model of Depression: Integrating the Neuropsychological Approach into the Cognitive Theory Framework. Clin. Psychol. Eur. 2019, 1, 1–35. [Google Scholar] [CrossRef]
- Gollan, J.; Raffety, B.; Gortner, E.; Dobson, K. Course Profiles of Early- and Adult-Onset Depression. J. Affect. Disord. 2005, 86, 81–86. [Google Scholar] [CrossRef]
- Dunn, V.; Goodyer, I.M. Longitudinal Investigation into Childhood-and Adolescence-Onset Depression: Psychiatric Outcome in Early Adulthood. Br. J. Psychiatry 2006, 188, 216–222. [Google Scholar] [CrossRef]
- Bernaras, E.; Jaureguizar, J.; Garaigordobil, M. Child and Adolescent Depression: A Review of Theories, Evaluation Instruments, Prevention Programs, and Treatments. Front. Psychol. 2019, 10, 543. [Google Scholar] [CrossRef]
- Abela, J.R.Z.; Hankin, B.L. (Eds.) Handbook of Depression in Children and Adolescents; The Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Bogner, H.R.; Bruce, M.L.; Reynolds, C.F., 3rd; Mulsant, B.H.; Cary, M.S.; Morales, K.; Alexopoulos, G.S. The Effects of Memory, Attention, and Executive Dysfunction on Outcomes of Depression in a Primary Care Intervention Trial: The PROSPECT Study. Int. J. Geriatr. Psychiatry 2007, 22, 922–929. [Google Scholar] [CrossRef] [PubMed]
- Beaudreau, S.A.; Rideaux, T.; O’Hara, R.; Arean, P. Does Cognition Predict Treatment Response and Remission in Psychotherapy for Late-Life Depression? Am. J. Geriatr. Psychiatry Off. J. Am. Assoc. Geriatr. Psychiatry 2015, 23, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Groves, S.J.; Douglas, K.M.; Porter, R.J. A Systematic Review of Cognitive Predictors of Treatment Outcome in Major Depression. Front. Psychiatry 2018, 9, 382. [Google Scholar] [CrossRef] [PubMed]
- Bruder, G.E.; Alvarenga, J.E.; Alschuler, D.; Abraham, K.; Keilp, J.G.; Hellerstein, D.J.; Stewart, J.W.; McGrath, P.J. Neurocognitive Predictors of Antidepressant Clinical Response. J. Affect. Disord. 2014, 166, 108–114. [Google Scholar] [CrossRef]
- Gordon, E.; Rush, A.J.; Palmer, D.M.; Braund, T.A.; Rekshan, W. Toward an Online Cognitive and Emotional Battery to Predict Treatment Remission in Depression. Neuropsychiatr. Dis. Treat. 2015, 11, 517–531. [Google Scholar] [CrossRef]
- Seeberg, I.; Kjaerstad, H.L.; Miskowiak, K.W. Neural and Behavioral Predictors of Treatment Efficacy on Mood Symptoms and Cognition in Mood Disorders: A Systematic Review. Front. Psychiatry 2018, 9, 337. [Google Scholar] [CrossRef]
- Miskowiak, K.W.; Petersen, C.S. Neuronal Underpinnings of Cognitive Impairment and-Improvement in Mood Disorders. CNS Spectr. 2019, 24, 30–53. [Google Scholar] [CrossRef]
- López-Solà, C.; Subirà, M.; Serra-Blasco, M.; Vicent-Gil, M.; Navarra-Ventura, G.; Aguilar, E.; Acebillo, S.; Palao, D.J.; Cardoner, N. Is Cognitive Dysfunction Involved in Difficult-to-Treat Depression? Characterizing Resistance from a Cognitive Perspective. Eur. Psychiatry 2020, 63, e74. [Google Scholar] [CrossRef]
- Lee, R.S.C.; Hermens, D.F.; Redoblado-Hodge, M.A.; Naismith, S.L.; Porter, M.A.; Kaur, M.; White, D.; Scott, E.M.; Hickie, I.B. Neuropsychological and Socio-Occupational Functioning in Young Psychiatric Outpatients: A Longitudinal Investigation. PLoS ONE 2013, 8, e58176. [Google Scholar] [CrossRef]
- Woo, Y.S.; Rosenblat, J.D.; Kakar, R.; Bahk, W.M.; McIntyre, R.S. Cognitive Deficits as a Mediator of Poor Occupational Function in Remitted Major Depressive Disorder Patients. Clin. Psychopharmacol. Neurosci. 2016, 14, 311. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.S.C.; Hermens, D.F.; Naismith, S.L.; Kaur, M.; Guastella, A.J.; Glozier, N.; Scott, J.; Scott, E.M.; Hickie, I.B. Clinical, Neurocognitive and Demographic Factors Associated with Functional Impairment in the Australian Brain and Mind Youth Cohort Study (2008–2016). BMJ Open 2018, 8, e022659. [Google Scholar] [CrossRef] [PubMed]
- Gregory, E.; Torres, I.J.; Ge, R.; Blumberger, D.M.; Downar, J.H.; Daskalakis, Z.J.; Lam, R.W.; Vila-Rodriguez, F. Predictors of Cognitive Impairment in Treatment-Resistant Depression. J. Affect. Disord. 2020, 274, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Keilp, J.G.; Gorlyn, M.; Russell, M.; Oquendo, M.A.; Burke, A.K.; Harkavy-Friedman, J.; Mann, J.J. Neuropsychological Function and Suicidal Behavior: Attention Control, Memory and Executive Dysfunction in Suicide Attempt. Psychol. Med. 2013, 43, 539–551. [Google Scholar] [CrossRef] [PubMed]
- Richard-Devantoy, S.; Berlim, M.T.; Jollant, F. A Meta-Analysis of Neuropsychological Markers of Vulnerability to Suicidal Behavior in Mood Disorders. Psychol. Med. 2014, 44, 1663–1673. [Google Scholar] [CrossRef] [PubMed]
- Lara, E.; Olaya, B.; Garin, N.; Ayuso-Mateos, J.L.; Miret, M.; Moneta, V.; Haro, J.M. Is Cognitive Impairment Associated with Suicidality? A Population-Based Study. Eur. Neuropsychopharmacol. J. Eur. Coll. Neuropsychopharmacol. 2015, 25, 203–213. [Google Scholar] [CrossRef]
- Pu, S.; Setoyama, S.; Noda, T. Association between Cognitive Deficits and Suicidal Ideation in Patients with Major Depressive Disorder. Sci. Rep. 2017, 7, 11637. [Google Scholar] [CrossRef]
- Bortolato, B.; Miskowiak, K.W.; Köhler, C.A.; Maes, M.; Fernandes, B.S.; Berk, M.; Carvalho, A.F. Cognitive Remission: A Novel Objective for the Treatment of Major Depression? BMC Med. 2016, 14, 9. [Google Scholar] [CrossRef]
- Allott, K.; Fisher, C.A.; Amminger, G.P.; Goodall, J.; Hetrick, S. Characterizing Neurocognitive Impairment in Young People with Major Depression: State, Trait, or Scar? Brain Behav. 2016, 6, e00527. [Google Scholar] [CrossRef]
- Scult, M.A.; Paulli, A.R.; Mazure, E.S.; Moffitt, T.E.; Hariri, A.R.; Strauman, T.J. The Association between Cognitive Function and Subsequent Depression: A Systematic Review and Meta-Analysis. Psychol. Med. 2017, 47, 1–17. [Google Scholar] [CrossRef]
- Hammar, Å.; Ronold, E.H.; Rekkedal, G.Å. Cognitive Impairment and Neurocognitive Profiles in Major Depression-A Clinical Perspective. Front. Psychiatry 2022, 13, 764374. [Google Scholar] [CrossRef] [PubMed]
- MacKenzie, L.E.; Uher, R.; Pavlova, B. Cognitive Performance in First-Degree Relatives of Individuals with vs. Without Major Depressive Disorder: A Meta-Analysis. JAMA Psychiatry 2019, 76, 297–305. [Google Scholar] [CrossRef]
- Belleau, E.L.; Phillips, M.L.; Birmaher, B.; Axelson, D.A.; Ladouceur, C.D. Aberrant Executive Attention in Unaffected Youth at Familial Risk for Mood Disorders. J. Affect. Disord. 2013, 147, 397–400. [Google Scholar] [CrossRef] [PubMed]
- Vinberg, M.; Miskowiak, K.W.; Kessing, L.V. Impairment of Executive Function and Attention Predicts Onset of Affective Disorder in Healthy High-Risk Twins. J. Clin. Psychiatry 2013, 74, e747–e753. [Google Scholar] [CrossRef] [PubMed]
- Simons, C.J.P.; Jacobs, N.; Derom, C.; Thiery, E.; Jolles, J.; van Os, J.; Krabbendam, L. Cognition as Predictor of Current and Follow-up Depressive Symptoms in the General Population. Acta Psychiatr. Scand. 2009, 120, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.K.; Leslie, S.M.; Bhattacharjee, K.; Gross, M.; Weisman, E.F.; Soudi, L.M.; Phillips, O.R.; Onopa, A. Vulnerabilities in Sequencing and Task Switching in Healthy Youth Offspring of Parents with Mood Disorders. J. Clin. Exp. Neuropsychol. 2018, 40, 606–618. [Google Scholar] [CrossRef]
- Snyder, H.R. Major Depressive Disorder Is Associated with Broad Impairments on Neuropsychological Measures of Executive Function: A Meta-Analysis and Review. Psychol. Bull. 2013, 139, 81–132. [Google Scholar] [CrossRef]
- Han, G.; Helm, J.; Iucha, C.; Zahn-Waxler, C.; Hastings, P.D.; Klimes-Dougan, B. Are Executive Functioning Deficits Concurrently and Predictively Associated with Depressive and Anxiety Symptoms in Adolescents? J. Clin. Child Adolesc. Psychol. 2016, 45, 44–58. [Google Scholar] [CrossRef]
- Halse, M.; Steinsbekk, S.; Hammar, Å.; Wichstrøm, L. Longitudinal Relations between Impaired Executive Function and Symptoms of Psychiatric Disorders in Childhood. J. Child Psychol. Psychiatry 2022. [Google Scholar] [CrossRef]
- Hawkey, E.J.; Tillman, R.; Luby, J.L.; Barch, D.M. Preschool Executive Function Predicts Childhood Resting-State Functional Connectivity and Attention-Deficit/Hyperactivity Disorder and Depression. Biol. Psychiatry. Cogn. Neurosci. Neuroimaging 2018, 3, 927–936. [Google Scholar] [CrossRef]
- Valsecchi, P.; Nibbio, G.; Rosa, J.; Tamussi, E.; Turrina, C.; Sacchetti, E.; Vita, A. Adult ADHD: Prevalence and Clinical Correlates in a Sample of Italian Psychiatric Outpatients. J. Atten. Disord. 2021, 25, 530–539. [Google Scholar] [CrossRef] [PubMed]
- Biederman, J.; Ball, S.W.; Monuteaux, M.C.; Mick, E.; Spencer, T.J.; McCreary, M.; Cote, M.; Faraone, S. V New Insights into the Comorbidity between ADHD and Major Depression in Adolescent and Young Adult Females. J. Am. Acad. Child Adolesc. Psychiatry 2008, 47, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Peters, A.T.; Jacobs, R.H.; Crane, N.A.; Ryan, K.A.; Weisenbach, S.L.; Ajilore, O.; Lamar, M.; Kassel, M.T.; Gabriel, L.B.; West, A.E.; et al. Domain-Specific Impairment in Cognitive Control among Remitted Youth with a History of Major Depression. Early Interv. Psychiatry 2017, 11, 383–392. [Google Scholar] [CrossRef]
- Sarapas, C.; Shankman, S.A.; Harrow, M.; Goldberg, J.F. Parsing Trait and State Effects of Depression Severity on Neurocognition: Evidence from a 26-Year Longitudinal Study. J. Abnorm. Psychol. 2012, 121, 830–837. [Google Scholar] [CrossRef] [PubMed]
- Klimes-Dougan, B.; Ronsaville, D.; Wiggs, E.A.; Martinez, P.E. Neuropsychological Functioning in Adolescent Children of Mothers with a History of Bipolar or Major Depressive Disorders. Biol. Psychiatry 2006, 60, 957–965. [Google Scholar] [CrossRef]
- Maalouf, F.T.; Brent, D.; Clark, L.; Tavitian, L.; McHugh, R.M.; Sahakian, B.J.; Phillips, M.L. Neurocognitive Impairment in Adolescent Major Depressive Disorder: State vs. Trait Illness Markers. J. Affect. Disord. 2011, 133, 625–632. [Google Scholar] [CrossRef]
- Schaefer, J.D.; Scult, M.A.; Caspi, A.; Arseneault, L.; Belsky, D.W.; Hariri, A.R.; Harrington, H.; Houts, R.; Ramrakha, S.; Poulton, R.; et al. Is Low Cognitive Functioning a Predictor or Consequence of Major Depressive Disorder? A Test in Two Longitudinal Birth Cohorts. Dev. Psychopathol. 2017, 1–15. [Google Scholar] [CrossRef]
- Koenen, K.C.; Moffitt, T.E.; Roberts, A.L.; Martin, L.T.; Kubzansky, L.; Harrington, H.; Poulton, R.; Caspi, A. Childhood IQ and Adult Mental Disorders: A Test of the Cognitive Reserve Hypothesis. Am. J. Psychiatry 2009, 166, 50–57. [Google Scholar] [CrossRef]
- Glaser, B.; Gunnell, D.; Timpson, N.J.; Joinson, C.; Zammit, S.; Smith, G.D.; Lewis, G. Age- and Puberty-Dependent Association between IQ Score in Early Childhood and Depressive Symptoms in Adolescence. Psychol. Med. 2011, 41, 333–343. [Google Scholar] [CrossRef][Green Version]
- Mac Giollabhui, N.; Olino, T.M.; Nielsen, J.; Abramson, L.Y.; Alloy, L.B. Is Worse Attention a Risk Factor for or a Consequence of Depression, or Are Worse Attention and Depression Better Accounted for by Stress? A Prospective Test of Three Hypotheses. Clin. Psychol. Sci. J. Assoc. Psychol. Sci. 2019, 7, 93–109. [Google Scholar] [CrossRef]
- Semkovska, M. Chapter 33—Cognitive Function and Neurocognitive Deficits in Depression; Martin, C.R., Hunter, L.-A., Patel, V.B., Preedy, V.R., Rajendram, R.B.T.-T.N., Eds.; Academic Press: Cambridge, MA, USA, 2021; pp. 361–371. [Google Scholar] [CrossRef]
- Vreeburg, S.A.; Hoogendijk, W.J.G.; van Pelt, J.; Derijk, R.H.; Verhagen, J.C.M.; van Dyck, R.; Smit, J.H.; Zitman, F.G.; Penninx, B.W.J.H. Major Depressive Disorder and Hypothalamic-Pituitary-Adrenal Axis Activity: Results from a Large Cohort Study. Arch. Gen. Psychiatry 2009, 66, 617–626. [Google Scholar] [CrossRef] [PubMed]
- Vilgis, V.; Silk, T.J.; Vance, A. Executive Function and Attention in Children and Adolescents with Depressive Disorders: A Systematic Review. Eur. Child Adolesc. Psychiatry 2015, 24, 365–384. [Google Scholar] [CrossRef] [PubMed]
- Vijayakumar, N.; Whittle, S.; Yücel, M.; Byrne, M.L.; Schwartz, O.; Simmons, J.G.; Allen, N.B. Impaired Maturation of Cognitive Control in Adolescents Who Develop Major Depressive Disorder. J. Clin. Child Adolesc. Psychol. 2016, 45, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Beaujean, A.A.; Parker, S.; Qiu, X. The Relationship between Cognitive Ability and Depression: A Longitudinal Data Analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 1983–1992. [Google Scholar] [CrossRef]
- Steiger, A.E.; Fend, H.A.; Allemand, M. Testing the Vulnerability and Scar Models of Self-Esteem and Depressive Symptoms from Adolescence to Middle Adulthood and across Generations. Dev. Psychol. 2015, 51, 236–247. [Google Scholar] [CrossRef]
- Steinberger, D.C.; Barch, D.M. Investigating the Link between Depression, Cognition, and Motivation in Late Childhood. Child Psychiatry Hum. Dev. 2021. [Google Scholar] [CrossRef]
- Stange, J.P.; Connolly, S.L.; Burke, T.A.; Hamilton, J.L.; Hamlat, E.J.; Abramson, L.Y.; Alloy, L.B. Inflexible cognition predicts first onset of major depressive episodes in adolescence. Depress. Anxiety 2016, 33, 1005–1012. [Google Scholar] [CrossRef]
- Baune, B.T.; Fuhr, M.; Air, T.; Hering, C. Neuropsychological Functioning in Adolescents and Young Adults with Major Depressive Disorder—A Review. Psychiatry Res. 2014, 218, 261–271. [Google Scholar] [CrossRef]
- Micco, J.A.; Henin, A.; Biederman, J.; Rosenbaum, J.F.; Petty, C.; Rindlaub, L.A.; Murphy, M.; Hirshfeld-Becker, D.R. Executive Functioning in Offspring at Risk for Depression and Anxiety. Depress. Anxiety 2009, 26, 780–790. [Google Scholar] [CrossRef]
- Maalouf, F.T.; Clark, L.; Tavitian, L.; Sahakian, B.J.; Brent, D.; Phillips, M.L. Bias to Negative Emotions: A Depression State-Dependent Marker in Adolescent Major Depressive Disorder. Psychiatry Res. 2012, 198, 28–33. [Google Scholar] [CrossRef]
- Orchard, F.; Reynolds, S. The Combined Influence of Cognitions in Adolescent Depression: Biases of Interpretation, Self-Evaluation, and Memory. Br. J. Clin. Psychol. 2018, 57, 420–435. [Google Scholar] [CrossRef] [PubMed]
- Voelz, Z.R.; Walker, R.L.; Pettit, J.W.; Joiner, T.E.; Wagner, K.D. Depressogenic attributional style: Evidence of trait-like nature in youth psychiatric inpatients. Personal. Individ. Differ. 2003, 34, 1129–1140. [Google Scholar] [CrossRef]
- Hankin, B.L.; Fraley, R.C.; Abela, J.R.Z. Daily Depression and Cognitions about Stress: Evidence for a Traitlike Depressogenic Cognitive Style and the Prediction of Depressive Symptoms in a Prospective Daily Diary Study. J. Pers. Soc. Psychol. 2005, 88, 673–685. [Google Scholar] [CrossRef] [PubMed]
- Hankin, B.L. Stability of Cognitive Vulnerabilities to Depression: A Short-Term Prospective Multiwave Study. J. Abnorm. Psychol. 2008, 117, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Abramson, L.Y.; Metalsky, G.I.; Alloy, L.B. Hopelessness depression: A theory-based subtype of depression. Psychol. Rev. 1989, 96, 358–372. [Google Scholar] [CrossRef]
- Alloy, L.B.; Abramson, L.Y.; Walshaw, P.D.; Neeren, A.M. Cognitive vulnerability to unipolar and bipolar mood disorders. J. Soc. Clin. Psychol. 2006, 25, 726–754. [Google Scholar] [CrossRef]
- Hankin, B.L. Cognitive Vulnerability-Stress Model of Depression during Adolescence: Investigating Depressive Symptom Specificity in a Multi-Wave Prospective Study. J. Abnorm. Child Psychol. 2008, 36, 999–1014. [Google Scholar] [CrossRef]
- Mac Giollabhui, N.; Hamilton, J.L.; Nielsen, J.; Connolly, S.L.; Stange, J.P.; Varga, S.; Burdette, E.; Olino, T.M.; Abramson, L.Y.; Alloy, L.B. Negative Cognitive Style Interacts with Negative Life Events to Predict First Onset of a Major Depressive Episode in Adolescence via Hopelessness. J. Abnorm. Psychol. 2018, 127, 1–11. [Google Scholar] [CrossRef]
- Beck, A.T. Depression: Clinical, Experimental, and Theoretical Aspects; Harper & Row: New York, NY, USA, 1967. [Google Scholar]
- Hankin, B.L.; Lakdawalla, Z.; Lee, A.; Grace, D.; Roesch, L. Cognitive vulnerabilities for emotional distress in adolescence: Disentangling the comorbidity of depression and anxiety in a multi-wave prospective study. BL Hankin & JRZ Abela (co-chairs), Depression and Anxiety: Issues of Specificity and Comorbidity. In Proceedings of the Symposium Conducted at the 38th annual Meeting of the Association for Advancement of Behavior Therapy, New Orleans, LA, USA, 2004. [Google Scholar]
- Lewinsohn, P.M.; Joiner, T.E.; Rohde, P. Evaluation of cognitive diathesis–stress models in predicting major depressive disorder in adolescents. J. Abnorm. Psychol. 2001, 110, 203–215. [Google Scholar] [CrossRef]
- Nolen-Hoeksema, S. Responses to Depression and Their Effects on the Duration of Depressive Episodes. J. Abnorm. Psychol. 1991, 100, 569–582. [Google Scholar] [CrossRef]
- Abela, J.R.Z.; Aydin, C.M.; Auerbach, R.P. Responses to depression in children: Reconceptualizing the relation among response styles. J. Abnorm. Child Psychol. 2007, 35, 913–927. [Google Scholar] [CrossRef] [PubMed]
- Kuyken, W.; Watkins, E.; Holden, E.; Cook, W. Rumination in Adolescents at Risk for Depression. J. Affect. Disord. 2006, 96, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Hankin, B.L. Rumination and Depression in Adolescence: Investigating Symptom Specificity in a Multiwave Prospective Study. J. Clin. Child Adolesc. Psychol. 2008, 37, 701–713. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, K.; Lopez, C.; Kistner, J. A Diathesis-Stress Test of Response Styles in Children. J. Soc. Clin. Psychol. 2009, 28, 1050–1070. [Google Scholar] [CrossRef]
- Cohen, J.R.; So, F.K.; Hankin, B.L.; Young, J.F. Translating Cognitive Vulnerability Theory into Improved Adolescent Depression Screening: A Receiver Operating Characteristic Approach. J. Clin. Child Adolesc. Psychol. 2019, 48, 582–595. [Google Scholar] [CrossRef]
- Gotlib, I.H.; Joormann, J. Cognition and Depression: Current Status and Future Directions. Annu. Rev. Clin. Psychol. 2010, 6, 285–312. [Google Scholar] [CrossRef]
- Connolly, S.L.; Wagner, C.A.; Shapero, B.G.; Pendergast, L.L.; Abramson, L.Y.; Alloy, L.B. Rumination Prospectively Predicts Executive Functioning Impairments in Adolescents. J. Behav. Ther. Exp. Psychiatry 2014, 45, 46–56. [Google Scholar] [CrossRef]
- Wagner, C.A.; Alloy, L.B.; Abramson, L.Y. Trait Rumination, Depression, and Executive Functions in Early Adolescence. J. Youth Adolesc. 2015, 44, 18–36. [Google Scholar] [CrossRef]
- Alloy, L.B.; Abramson, L.Y.; Whitehouse, W.G.; Hogan, M.E.; Tashman, N.A.; Steinberg, D.L.; Rose, D.T.; Donovan, P. Depressogenic Cognitive Styles: Predictive Validity, Information Processing and Personality Characteristics, and Developmental Origins. Behav. Res. Ther. 1999, 37, 503–531. [Google Scholar] [CrossRef]
- Alloy, L.B.; Black, S.K.; Young, M.E.; Goldstein, K.E.; Shapero, B.G.; Stange, J.P.; Boccia, A.S.; Matt, L.M.; Boland, E.M.; Moore, L.C.; et al. Cognitive Vulnerabilities and Depression versus Other Psychopathology Symptoms and Diagnoses in Early Adolescence. J. Clin. Child Adolesc. Psychol. 2012, 41, 539–560. [Google Scholar] [CrossRef]
- Alloy, L.B.; Riskind, J.H. Cognitive Vulnerability to Emotional Disorders; Lawrence Erlbaum Associates Publishers: Pittsburgh, PA, USA, 2006. [Google Scholar]
- Iacoviello, B.M.; Alloy, L.B.; Abramson, L.Y.; Whitehouse, W.G.; Hogan, M.E. The Course of Depression in Individuals at High and Low Cognitive Risk for Depression: A Prospective Study. J. Affect. Disord. 2006, 93, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.; Leboyer, M.; Hickie, I.; Berk, M.; Kapczinski, F.; Frank, E.; Kupfer, D.; McGorry, P. Clinical Staging in Psychiatry: A Cross-Cutting Model of Diagnosis with Heuristic and Practical Value. Br. J. Psychiatry 2013, 202, 243–245. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; McGorry, P.D.; Kane, J.M. Improving outcomes of first-episode psychosis: An overview. World Psychiatry 2017, 16, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Berk, M.; Post, R.; Ratheesh, A.; Gliddon, E.; Singh, A.; Vieta, E.; Carvalho, A.F.; Ashton, M.M.; Berk, L.; Cotton, S.M.; et al. Staging in bipolar disorder: From theoretical framework to clinical utility. World Psychiatry 2017, 16, 236–244. [Google Scholar] [CrossRef]
- Hetrick, S.E.; Parker, A.G.; Hickie, I.B.; Purcell, R.; Yung, A.R.; McGorry, P.D. Early identification and intervention in depressive disorders: Towards a clinical staging model. Psychother. Psychosom. 2008, 770, 263–270. [Google Scholar] [CrossRef]
- Maj, M. Beyond Diagnosis in Psychiatric Practice. Ann. Gen. Psychiatry 2020, 19, 27. [Google Scholar] [CrossRef]
- McGorry, P.D.; Hickie, I.B.; Yung, A.R.; Pantelis, C.; Jackson, H.J. Clinical Staging of Psychiatric Disorders: A Heuristic Framework for Choosing Earlier, Safer and More Effective Interventions. Aust. N. Z. J. Psychiatry 2006, 40, 616–622. [Google Scholar] [CrossRef]
- McGorry, P.; Keshavan, M.; Goldstone, S.; Amminger, P.; Allott, K.; Berk, M.; Lavoie, S.; Pantelis, C.; Yung, A.; Wood, S.; et al. Biomarkers and Clinical Staging in Psychiatry. World Psychiatry 2014, 13, 211–223. [Google Scholar] [CrossRef]
- Catalan, A.; Salazar de Pablo, G.; Aymerich, C.; Damiani, S.; Sordi, V.; Radua, J.; Oliver, D.; McGuire, P.; Giuliano, A.J.; Stone, W.S.; et al. Neurocognitive Functioning in Individuals at Clinical High Risk for Psychosis: A Systematic Review and Meta-Analysis. JAMA Psychiatry 2021, 78, 859–867. [Google Scholar] [CrossRef]
- Mesholam-Gately, R.I.; Giuliano, A.J.; Goff, K.P.; Faraone, S.V.; Seidman, L.J. Neurocognition in First-Episode Schizophrenia: A Meta-Analytic Review. Neuropsychology 2009, 23, 315–336. [Google Scholar] [CrossRef]
- Heilbronner, U.; Samara, M.; Leucht, S.; Falkai, P.; Schulze, T.G. The Longitudinal Course of Schizophrenia across the Lifespan: Clinical, Cognitive, and Neurobiological Aspects. Harv. Rev. Psychiatry 2016, 24, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Daban, C.; Martinez-Aran, A.; Torrent, C.; Tabarés-Seisdedos, R.; Balanzá-Martínez, V.; Salazar-Fraile, J.; Selva-Vera, G.; Vieta, E. Specificity of Cognitive Deficits in Bipolar Disorder versus Schizophrenia. A Systematic Review. Psychother. Psychosom. 2006, 75, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Keramatian, K.; Torres, I.J.; Yatham, L.N. Neurocognitive Functioning in Bipolar Disorder: What We Know and What We Don’t. Dialogues Clin. Neurosci. 2021, 23, 29–38. [Google Scholar] [CrossRef]
- Martino, D.J.; Samamé, C.; Ibañez, A.; Strejilevich, S.A. Neurocognitive Functioning in the Premorbid Stage and in the First Episode of Bipolar Disorder: A Systematic Review. Psychiatry Res. 2015, 226, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Bora, E.; Yucel, M.; Pantelis, C. Cognitive Endophenotypes of Bipolar Disorder: A Meta-Analysis of Neuropsychological Deficits in Euthymic Patients and Their First-Degree Relatives. J. Affect. Disord. 2009, 113, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Arts, B.; Jabben, N.; Krabbendam, L.; van Os, J. Meta-Analyses of Cognitive Functioning in Euthymic Bipolar Patients and Their First-Degree Relatives. Psychol. Med. 2008, 38, 771–785. [Google Scholar] [CrossRef]
- Bora, E.; Yücel, M.; Pantelis, C.; Berk, M. Meta-Analytic Review of Neurocognition in Bipolar II Disorder. Acta Psychiatr. Scand. 2011, 123, 165–174. [Google Scholar] [CrossRef]
- Bora, E.; Özerdem, A. A Meta-Analysis of Neurocognition in Youth with Familial High Risk for Bipolar Disorder. Eur. Psychiatry 2017, 44, 17–23. [Google Scholar] [CrossRef]
- Ratheesh, A.; Lin, A.; Nelson, B.; Wood, S.J.; Brewer, W.; Betts, J.; Berk, M.; McGorry, P.; Yung, A.R.; Bechdolf, A. Neurocognitive Functioning in the Prodrome of Mania--an Exploratory Study. J. Affect. Disord. 2013, 147, 441–445. [Google Scholar] [CrossRef]
- Knudsen, C.B.; Hemager, N.; Greve, A.N.; Lambek, R.; Andreassen, A.K.; Veddum, L.; Brandt, J.M.; Gregersen, M.; Krantz, M.F.; Søndergaard, A.; et al. Neurocognitive Development in Children at Familial High Risk of Schizophrenia or Bipolar Disorder. JAMA Psychiatry 2022, 79, 589–599. [Google Scholar] [CrossRef]
- Kyte, Z.A.; Goodyer, I.M.; Sahakian, B.J. Selected Executive Skills in Adolescents with Recent First Episode Major Depression. J. Child Psychol. Psychiatry. 2005, 46, 995–1005. [Google Scholar] [CrossRef] [PubMed]
- Wagner, S.; Müller, C.; Helmreich, I.; Huss, M.; Tadić, A. A Meta-Analysis of Cognitive Functions in Children and Adolescents with Major Depressive Disorder. Eur. Child Adolesc. Psychiatry 2015, 24, 5–19. [Google Scholar] [CrossRef] [PubMed]
- Oliver, A.; Pile, V.; Elm, D.; Lau, J. The Cognitive Neuropsychology of Depression in Adolescents. Curr. Behav. Neurosci. Rep. 2019, 6, 227–235. [Google Scholar] [CrossRef]
- Grant, M.M.; Thase, M.E.; Sweeney, J.A. Cognitive Disturbance in Outpatient Depressed Younger Adults: Evidence of Modest Impairment. Biol. Psychiatry 2001, 50, 35–43. [Google Scholar] [CrossRef]
- Castaneda, A.E.; Tuulio-Henriksson, A.; Marttunen, M.; Suvisaari, J.; Lönnqvist, J. A Review on Cognitive Impairments in Depressive and Anxiety Disorders with a Focus on Young Adults. J. Affect. Disord. 2008, 106, 1–27. [Google Scholar] [CrossRef]
- Porter, R.J.; Robinson, L.J.; Malhi, G.S.; Gallagher, P. The Neurocognitive Profile of Mood Disorders-a Review of the Evidence and Methodological Issues. Bipolar Disord. 2015, 17 (Suppl. 2), 21–40. [Google Scholar] [CrossRef]
- Delagneau, G.; Bowden, S.C.; van-der-El, K.; Bryce, S.; Hamilton, M.; Adams, S.; Burgat, L.; Killackey, E.; Rickwood, D.; Allott, K. Perceived Need for Neuropsychological Assessment According to Geographic Location: A Survey of Australian Youth Mental Health Clinicians. Appl. Neuropsychol. Child 2021, 10, 123–132. [Google Scholar] [CrossRef]
- Weightman, M.J.; Air, T.M.; Baune, B.T. A Review of the Role of Social Cognition in Major Depressive Disorder. Front. Psychiatry 2014, 5, 179. [Google Scholar] [CrossRef]
- Healy, C.; Brannigan, R.; Dooley, N.; Staines, L.; Keeley, H.; Whelan, R.; Clarke, M.; Zammit, S.; Kelleher, I.; Cannon, M. Person-Centered Trajectories of Psychopathology from Early Childhood to Late Adolescence. JAMA Netw. Open 2022, 5, e229601. [Google Scholar] [CrossRef]
- Kjelkenes, R.; Wolfers, T.; Alnæs, D.; van der Meer, D.; Pedersen, M.L.; Dahl, A.; Voldsbekk, I.; Moberget, T.; Tamnes, C.K.; Andreassen, O.A.; et al. Mapping Normative Trajectories of Cognitive Function and Its Relation to Psychopathology Symptoms and Genetic Risk in Youth. Biol. Psychiatry Glob. Open Sci. 2022. [Google Scholar] [CrossRef]
- Choate, A.M.; Bornovalova, M.A.; Hipwell, A.E.; Chung, T.; Stepp, S.D. The General Psychopathology Factor (p) from Adolescence to Adulthood: Exploring the Developmental Trajectories of p Using a Multi-Method Approach. Dev. Psychopathol. 2022, 11, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Bonoldi, I.; Yung, A.R.; Borgwardt, S.; Kempton, M.J.; Valmaggia, L.; Barale, F.; Caverzasi, E.; McGuire, P. Predicting Psychosis: Meta-Analysis of Transition Outcomes in Individuals at High Clinical Risk. Arch. Gen. Psychiatry 2012, 69, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.M.; Oosterlaan, J.; Sergeant, J.A.; Buitelaar, J.K. Executive Functioning in Adult ADHD: A Meta-Analytic Review. Psychol. Med. 2005, 35, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
| Key Points |
|---|
| Cognitive impairments are among the main manifestations of MDD, comprising disturbances in the cold, hot and social cognition domains that negatively influence treatments response, illness course and psychosocial functioning. |
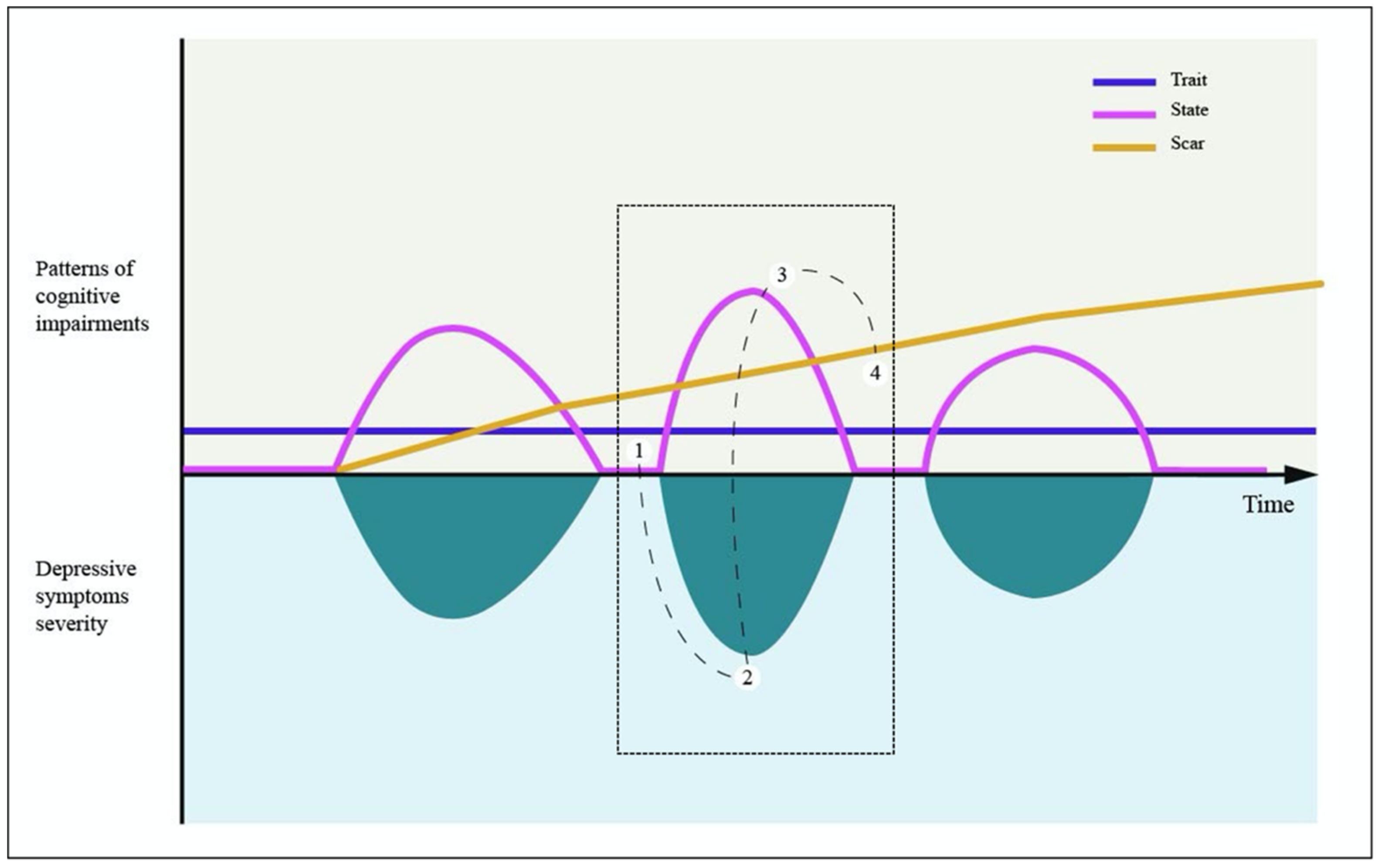
| Cognitive impairments in MDD could be described according to the trait, scar and state hypotheses that considered, respectively, these disturbances as a pre-existing vulnerability marker, a scarring manifestation due to the chronicity/severity of affective episodes, or a temporary feature of an acute depressive episode decreasing with it resolution. |
| While cognitive impairments have been commonly described in adults with MDD, cognitive impairments in youth still represent a neglected area of scientific interest although this topic is crucial to further identify clinical endophenotypes at increased risked for MDD and to develop preventive and therapeutic interventions in youth. |
| Unlike schizophrenia or bipolar disorder, only limited and inconclusive data are available considering cognitive impairments in childhood and adolescence during the pre-morbid phase of MDD or even among at-risk individuals, so that current evidence does not allow to confirm the superiority of one specific hypothesis on the nature of cognitive disturbances in youth. |
| In youth samples, although most of the current data considered cold cognitive domain impairments, disturbances of the hot cognition (i.e., ruminations) might represent another feasible marker to further understand the nature of these deficits during the depressive cycle. |
| Current limitations regarding cognitive impairments in youth population include heterogeneity of study design, the lack of systematic assessment of cold, hot, and social cognition cognitive domains and of their possible interaction, of their influences on quality of life and daily functioning, and of possible contributions by other psychiatric comorbidities. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barlati, S.; Lisoni, J.; Nibbio, G.; Baldacci, G.; Cicale, A.; Ferrarin, L.C.; Italia, M.; Zucchetti, A.; Deste, G.; Vita, A. Current Evidence and Theories in Understanding the Relationship between Cognition and Depression in Childhood and Adolescence: A Narrative Review. Diagnostics 2022, 12, 2525. https://doi.org/10.3390/diagnostics12102525
Barlati S, Lisoni J, Nibbio G, Baldacci G, Cicale A, Ferrarin LC, Italia M, Zucchetti A, Deste G, Vita A. Current Evidence and Theories in Understanding the Relationship between Cognition and Depression in Childhood and Adolescence: A Narrative Review. Diagnostics. 2022; 12(10):2525. https://doi.org/10.3390/diagnostics12102525
Chicago/Turabian StyleBarlati, Stefano, Jacopo Lisoni, Gabriele Nibbio, Giulia Baldacci, Andrea Cicale, Laura Chiara Ferrarin, Mauro Italia, Andrea Zucchetti, Giacomo Deste, and Antonio Vita. 2022. "Current Evidence and Theories in Understanding the Relationship between Cognition and Depression in Childhood and Adolescence: A Narrative Review" Diagnostics 12, no. 10: 2525. https://doi.org/10.3390/diagnostics12102525
APA StyleBarlati, S., Lisoni, J., Nibbio, G., Baldacci, G., Cicale, A., Ferrarin, L. C., Italia, M., Zucchetti, A., Deste, G., & Vita, A. (2022). Current Evidence and Theories in Understanding the Relationship between Cognition and Depression in Childhood and Adolescence: A Narrative Review. Diagnostics, 12(10), 2525. https://doi.org/10.3390/diagnostics12102525








