Visceral Obesity and Lipid Profiles in Chinese Adults with Normal and High Body Mass Index
Abstract
1. Introduction
2. Materials and Methods
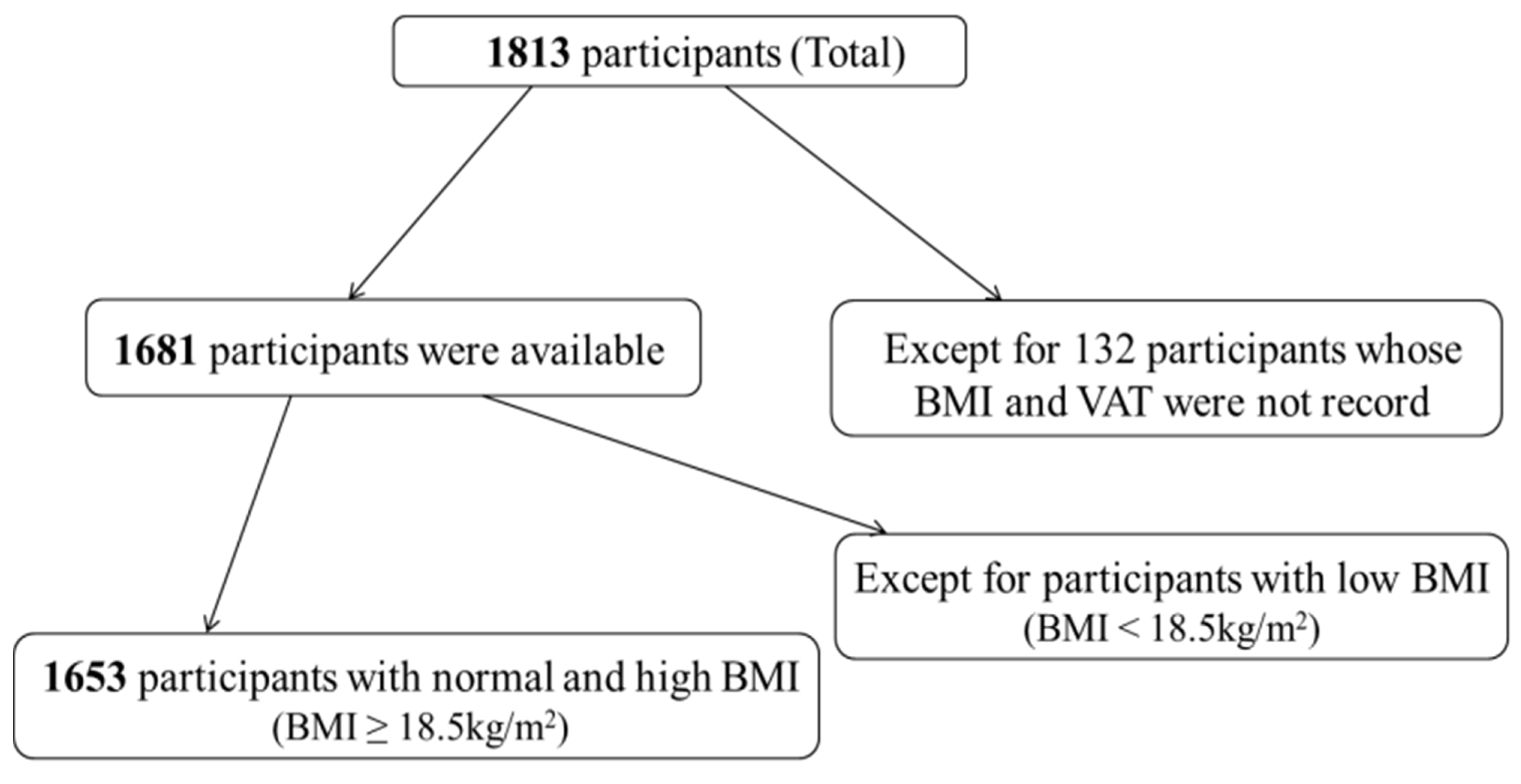
2.1. Study Population
2.2. Anthropometric Measurements
2.3. Visceral Fat Measurements
2.4. Blood Lipid Measurements
2.5. Statistical Analysis
3. Results
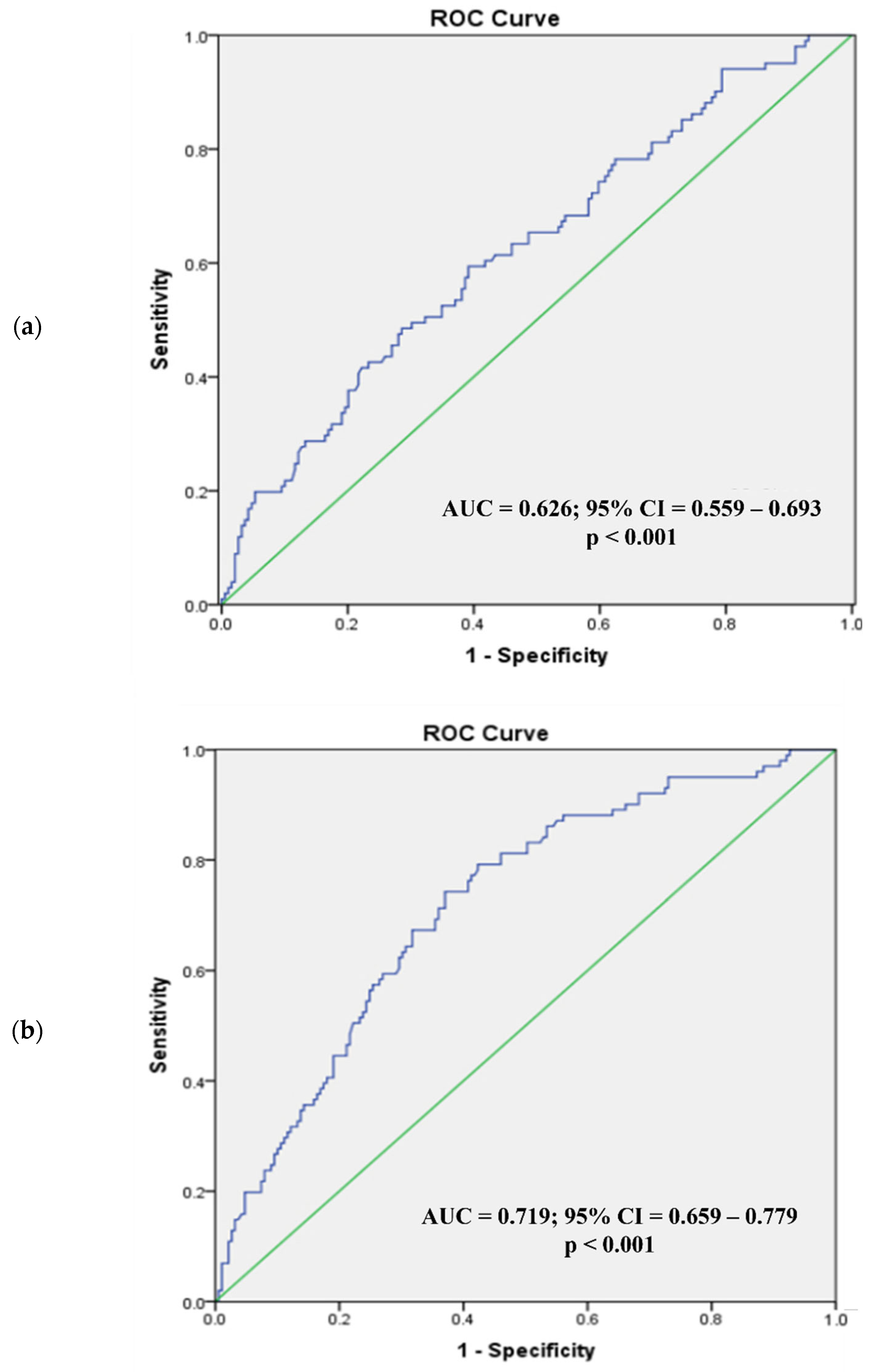
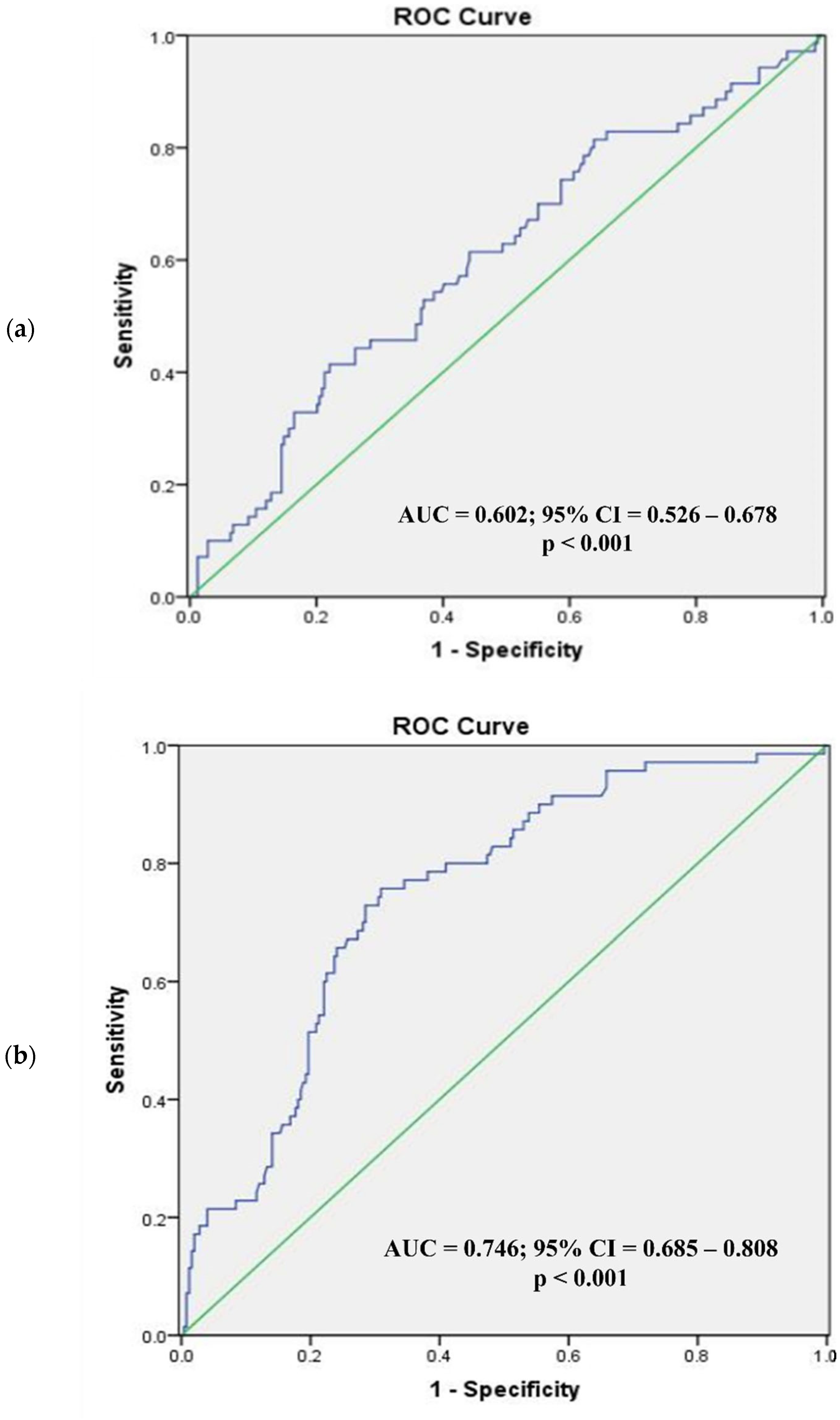
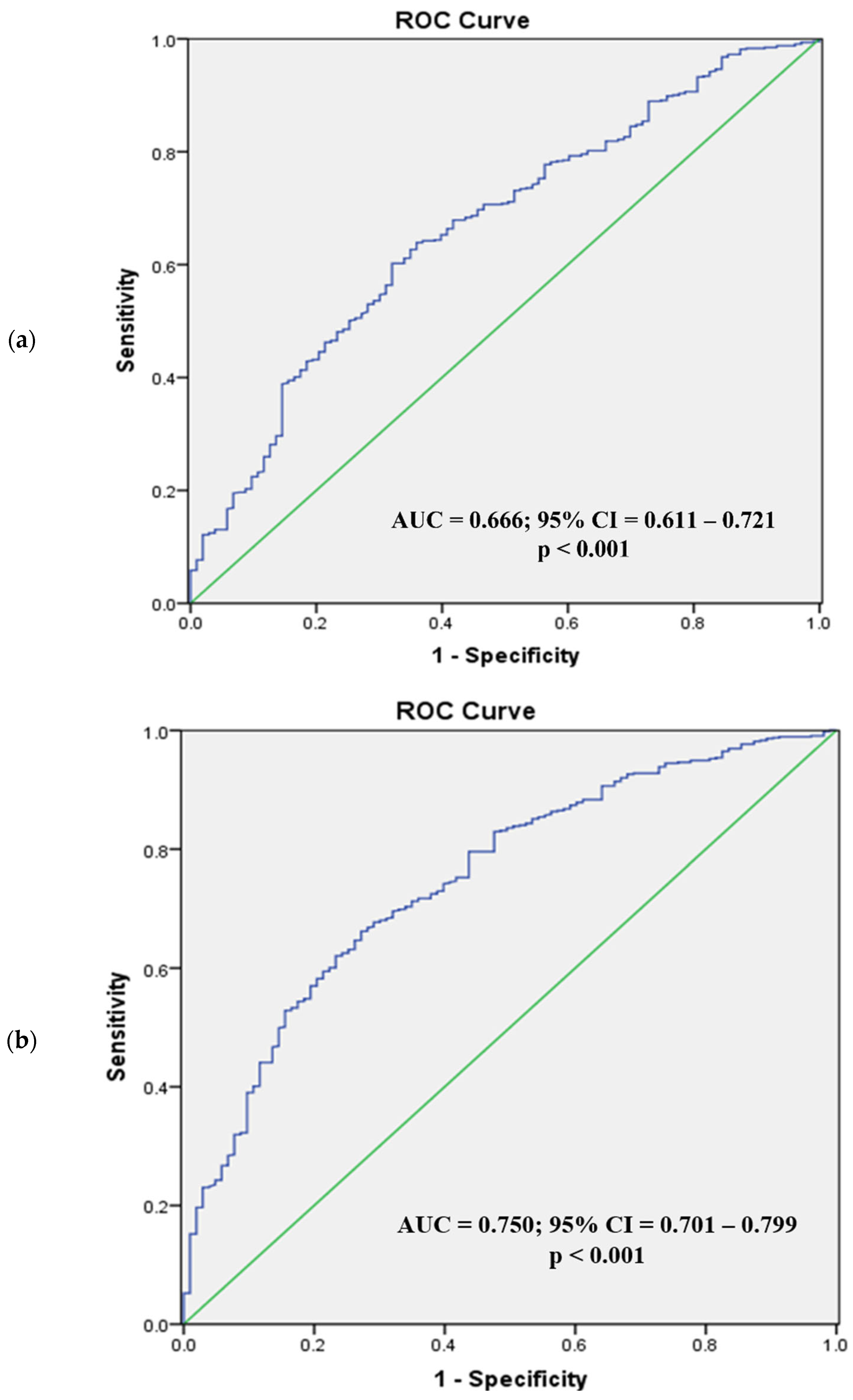
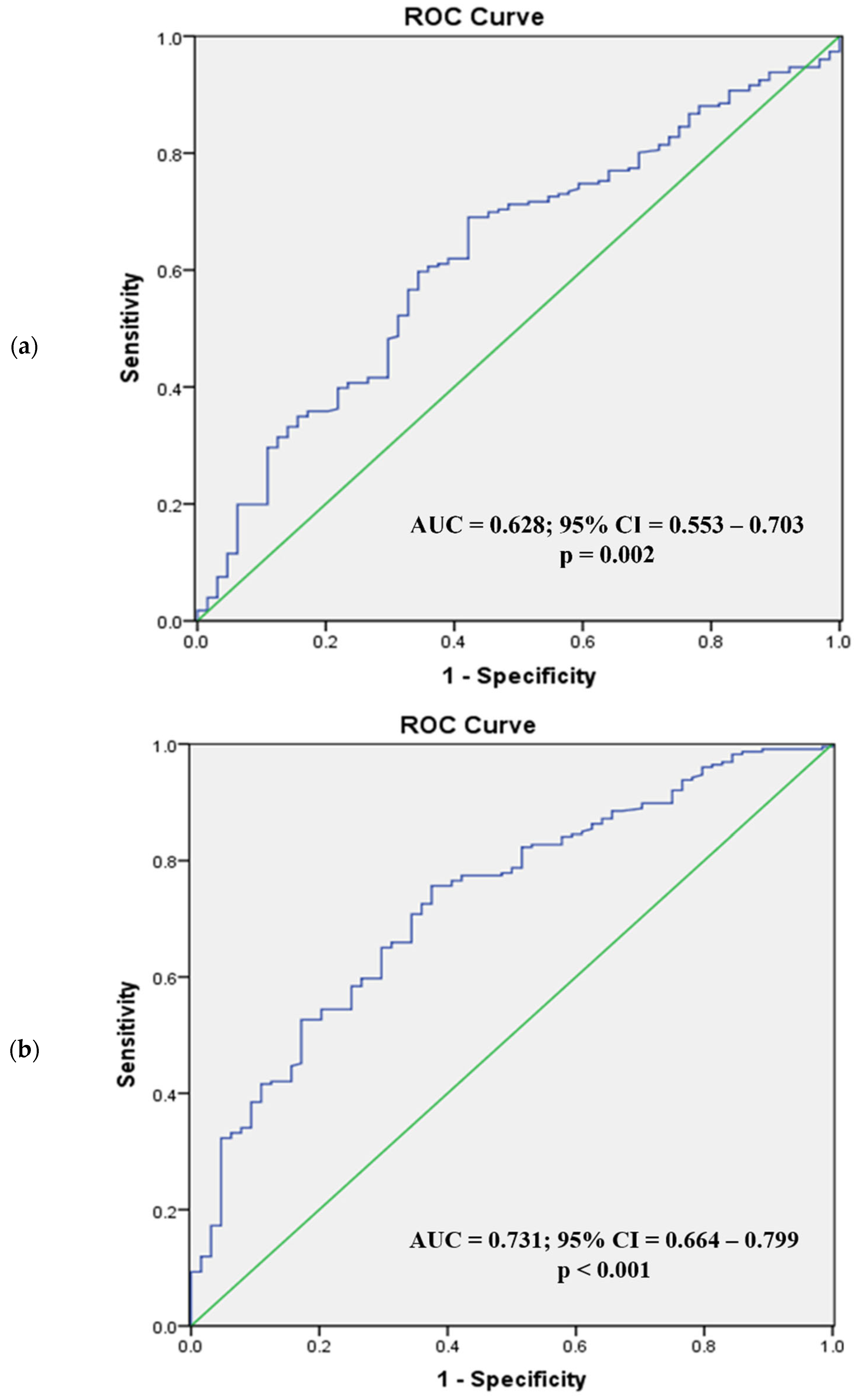
3.1. Phenotypic Predictors of Visceral Obesity
3.2. Lipid Profiles of All Participations
3.3. Lipid Profiles of High vs. Normal Visceral Fat Sub-Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Friedrich, M.J. Global Obesity Epidemic Worsening. JAMA 2017, 318, 603. [Google Scholar] [CrossRef]
- Malik, V.S.; Willett, W.C.; Hu, F.B. Global obesity: Trends, risk factors and policy implications. Nat. Rev. Endocrinol. 2013, 9, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 9 June 2021).
- Thomas, G.N.; Ho, S.Y.; Lam, K.S.; Janus, E.D.; Hedley, A.J.; Lam, T.H.; Hong Kong Cardiovascular Risk Factor Prevalence Study Steering Committee. Impact of obesity and body fat distribution on cardiovascular risk factors in Hong Kong Chinese. Obes. Res. 2004, 12, 1805–1813. [Google Scholar] [CrossRef] [PubMed]
- He, M.; Tan, K.C.; Li, E.T.; Kung, A.W. Bosdy fat determination by dual energy X-ray absorptiometry and its relation to body mass index and waist circumference in Hong Kong Chinese. Int. J. Obes. 2001, 25, 748–752. [Google Scholar] [CrossRef]
- Zhou, B.F.; Coorperative Meta-Analysis Group Of China Obesity Task Force. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cutoff points of body mass index and waist circumference in Chinese adults. Biomed Environ. Sci. 2002, 15, 83–96. [Google Scholar] [PubMed]
- Katsuki, A.; Sumida, Y.; Urakawa, H.; Gabazza, E.C.; Murashima, S.; Maruyama, N.; Morioka, K.; Nakatani, K.; Yano, Y.; Adachi, Y. Increased visceral fat and serum levels of triglyceride are associated with insulin resistance in Japanese metabolically obese, normal weight subjects with normal glucose tolerance. Diabetes Care 2003, 26, 2341–2344. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, L.; Cai, X.; Wu, S.; Andersen, N.D.; Martin, M.; Malek, J.; Guthrie, P.; Veves, A.; Logerfo, F.W. Gene expression of pro-inflammatory cytokines and neuropeptides in diabetic wound healing. J. Surg. Res. 2011, 167, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Cinti, S. Adipose Organ Development and Remodeling. Compr. Physiol. 2018, 8, 1357–1431. [Google Scholar]
- Kishida, K.; Funahashi, T.; Matsuzawa, Y.; Shimomura, I. Visceral adiposity as a target for the management of the metabolic syndrome. Ann. Med. 2012, 44, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Britton, K.A.; Massaro, J.M.; Murabito, J.M.; Kreger, B.E.; Hoffmann, U.; Fox, C.S. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J. Am. Coll. Cardiol. 2013, 62, 921–925. [Google Scholar] [CrossRef]
- Cheng, X.; Zhang, Y.; Wang, C.; Deng, W.; Wang, L.; Duanmu, Y.; Li, K.; Yan, D.; Xu, L.; Wu, C.; et al. The optimal anatomic site for a single slice to estimate the total volume of visceral adipose tissue by using the quantitative computed tomography (QCT) in Chinese population. Eur. J. Clin. Nutr. 2018, 72, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Huo, L.; Li, K.; Deng, W.; Wang, L.; Xu, L.; Shaw, J.E.; Jia, P.; Zhou, D.; Cheng, X.G. Optimal cut-points of visceral adipose tissue areas for cardiometabolic risk factors in a Chinese population: A cross-sectional study. Diabet. Med. 2019, 36, 1268–1275. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Katashima, M.; Yasumasu, T.; Li, K.J. Visceral fat area, waist circumference and metabolic risk factors in abdominally obese Chinese adults. Biomed Environ. Sci. 2012, 25, 141–148. [Google Scholar] [PubMed]
- Stevenson, P.H. Height.weight.surface formula for the estimation of surface area in Chinese subjects. Chin. J. Physiol. 1937, 12, 327–330. [Google Scholar]
- Joint Committee for Developing Chinese guidelines on Prevention and Treatment of Dyslipidemia in Adults. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 2007, 35, 390–419. [Google Scholar]
- Assmann, G.; Schulte, H.; Funke, H.; von Eckardstein, A. The emergence of triglycerides as a significant independent risk factor in coronary artery disease. Eur. Heart J. 1998, 19, M8-14. [Google Scholar] [PubMed]
- Manninen, V.; Tenkanen, L.; Koskinen, P.; Huttunen, J.K.; Manttari, M.; Heinonen, O.P.; Frick, M.H. Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study. Implications for treatment. Circulation 1992, 85, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Gao, L.; Xie, X.; Tan, S.C. Epidemiology of dyslipidemia in Chinese adults: Meta-analysis of prevalence, awareness, treatment, and control. Popul. Health Metr. 2014, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Yoon, K.H.; Lee, J.H.; Kim, J.W.; Cho, J.H.; Choi, Y.H.; Ko, S.H.; Zimmet, P.; Son, H.Y. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006, 368, 1681–1688. [Google Scholar] [CrossRef]
- Hashemipour, S.; Esmailzadehha, N.; Hamid, H.; Oveisi, S.; Yakhchaliha, P.; Ziaee, A. Association of metabolic syndrome components with insulin resistance in normal weight population: The Qazvin Metabolic Diseases study. J. Endocrinol. Investig. 2015, 38, 1111–1115. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Wu, S.; Huang, J.; Yuan, J.; Chen, H.; Chen, Y. Metabolic syndrome increases cardiovascular risk in a population with prediabetes: A prospective study in a cohort of Chinese adults. J. Diabetes Investig. 2019, 10, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Busetto, L. Visceral obesity and the metabolic syndrome: Effects of weight loss. Nutr. Metab. Cardiovasc. Dis. 2001, 11, 195–204. [Google Scholar]
- Xu, R.; Gao, X.; Wan, Y.; Fan, Z. Association of Metabolically Healthy Overweight Phenotype With Abnormalities of Glucose Levels and Blood Pressure Among Chinese Adults. JAMA Netw. Open 2019, 2, e1914025. [Google Scholar] [CrossRef] [PubMed]
- Conus, F.; Allison, D.B.; Rabasa-Lhoret, R.; St-Onge, M.; St-Pierre, D.H.; Tremblay-Lebeau, A.; Poehlman, E.T. Metabolic and behavioral characteristics of metabolically obese but normal-weight women. J. Clin. Endocrinol. Metab. 2004, 89, 5013–5020. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.F. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases--report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ. Sci. 2002, 15, 245–252. [Google Scholar]
- Jia, W.P.; Lu, J.X.; Xiang, K.S.; Bao, Y.Q.; Lu, H.J.; Chen, L. Prediction of abdominal visceral obesity from body mass index, waist circumference and waist-hip ratio in Chinese adults: Receiver operating characteristic curves analysis. Biomed Environ. Sci. 2003, 16, 206–211. [Google Scholar]
- Han, M.; Qin, P.; Li, Q.; Qie, R.; Liu, L.; Zhao, Y.; Liu, D.; Zhang, D.; Guo, C.; Zhou, Q.; et al. Chinese visceral adiposity index: A reliable indicator of visceral fat function associated with risk of type 2 diabetes. Diabetes/Metab. Res. Rev. 2021, 37, e3370. [Google Scholar] [CrossRef]
| High VAT * (n = 101) | Normal VAT (n = 189) | Difference (p) | ||
|---|---|---|---|---|
| Normal BMI (n = 290) | VAT area, cm2 | 179.70 ± 25.55 | 96.48 ± 30.17 | - |
| Age, y | 48.39 ± 11.54 | 46.32 ± 11.02 | 0.14 | |
| Weight, kg | 66.73 ± 5.12 | 63.45 ± 5.54 | <0.001 | |
| Height, cm | 170.78 ± 5.77 | 170.13 ± 5.53 | 0.35 | |
| BMI, kg/m2 | 22.86 ± 1.01 | 21.90 ± 1.37 | <0.001 | |
| BSA, m2 | 1.74 ± 0.096 | 1.70 ± 0.097 | <0.001 | |
| (n = 651) | (n = 103) | |||
| Overweight and obese (n = 754) | VAT area, cm2 | 216.28 ± 48.88 | 114.16 ± 26.57 | - |
| Age, y | 46.93 ± 10.58 | 47.24 ± 10.88 | 0.78 | |
| Weight, kg | 80.20 ± 8.83 | 74.19 ± 7.08 | <0.001 | |
| Height, cm | 170.56 ± 6.05 | 169.82 ± 6.90 | 0.25 | |
| BMI, kg/m2 | 27.54 ± 2.39 | 25.70 ± 1.55 | <0.001 | |
| BSA, m2 | 1.91 ± 0.14 | 1.83 ± 0.13 | <0.001 | |
| High VAT * (n = 70) | Normal VAT (n = 249) | Difference (p) | ||
|---|---|---|---|---|
| Normal BMI (n = 319) | VAT area, cm2 | 144 ± 24.3 | 73.5 ± 24.6 | - |
| Age, y | 55.6 ± 10.2 | 44.9 ± 11.2 | <0.001 | |
| Weight, kg | 56.9 ± 4.81 | 54.4 ± 4.75 | <0.001 | |
| Height, cm | 158 ± 5.29 | 159 ± 5.61 | 0.50 | |
| BMI, kg/m2 | 22.7 ± 1.04 | 21.5 ± 1.39 | <0.001 | |
| BSA, m2 | 1.54 ± 0.09 | 1.51 ± 0.09 | 0.013 | |
| (n = 226) | (n = 64) | |||
| Overweight and obese (n = 290) | VAT area, cm2 | 161 ± 35.5 | 96.1 ± 15.1 | - |
| Age, y | 53.2 ± 10.9 | 48.3 ± 9.95 | 0.002 | |
| Weight, kg | 66.6 ± 7.25 | 63 ± 5.41 | <0.001 | |
| Height, cm | 157 ± 5.50 | 157 ± 6.21 | 0.58 | |
| BMI, kg/m2 | 27.1 ± 2.41 | 25.5 ± 1.37 | <0.001 | |
| BSA, m2 | 1.66 ± 0.12 | 1.61 ± 0.10 | 0.007 | |
| Estimated Factors | Odds Ratio | 95% Confidence Interval | p |
|---|---|---|---|
| Men (n = 290) | |||
| Age (≥50 vs. <50 years) | 1.62 | 0.93–2.81 | 0.09 |
| BSA (>1.72 vs. ≤1.72 m2) | 1.64 | 0.94–2.87 | 0.08 |
| BMI (>22.5 vs. ≤22.5 kg/m2) | 4.41 | 2.52–7.69 | <0.001 |
| Women (n = 319) | |||
| Age (≥50 vs. <50 Years) | 5.43 | 2.82–10.5 | <0.001 |
| BSA (>1.57 vs. ≤1.57 m2) | 2.41 | 1.23–4.71 | 0.07 |
| BMI (>22.3 vs. ≤22.3 kg/m2) | 5.18 | 2.71–9.89 | <0.001 |
| Estimated Factors | Odds Ratio | 95% Confidence Interval | p |
|---|---|---|---|
| Men (n = 754) | |||
| BSA (>1.87 vs. ≤1.87 m2) | 1.84 | 1.14–2.96 | 0.012 |
| BMI (>26.3 vs.≤26.3 kg/m2) | 4.26 | 2.61–6.96 | <0.001 |
| Women (n = 290) | |||
| Age (≥50 vs. <50 Years) | 3.77 | 1.94–7.31 | <0.001 |
| BSA (>1.62 vs. ≤1.62 m2) | 2.99 | 1.53–5.85 | 0.001 |
| BMI (>25.3 vs. ≤25.3 kg/m2) | 3.99 | 2.13–7.46 | <0.001 |
| High VAT n = 101 | Normal VAT n = 189 | Difference p | ||
|---|---|---|---|---|
| Normal BMI (n = 290) | TC | 5.04 ± 0.83 | 4.76 ± 0.84 | 0.007 |
| TG | 1.80 ± 1.05 | 1.42 ± 1.42 | 0.02 | |
| LDL/HDL | 2.54 ± 0.78 | 2.15 ± 0.86 | <0.001 | |
| LDL | 3.11 ± 0.68 | 2.84 ± 0.72 | 0.002 | |
| HDL | 1.29 ± 0.30 | 1.43 ± 0.39 | 0.001 | |
| n = 651 | n = 103 | |||
| Overweight and obese (n = 754) | TC | 5.02 ± 0.92 | 4.89 ± 1.02 | 0.18 |
| TG | 2.37 ± 2.22 | 1.70 ± 1.39 | <0.001 | |
| LDL/HDL | 2.71 ± 0.91 | 2.41 ± 0.87 | 0.002 | |
| LDL | 3.02 ± 0.80 | 3.00 ± 0.83 | 0.81 | |
| HDL | 1.17 ± 0.29 | 1.31 ± 0.31 | <0.001 | |
| High VAT n = 70 | Low VAT n = 249 | Difference p | ||
|---|---|---|---|---|
| Normal BMI (n = 319) | TC | 5.32 ± 1.06 | 4.75 ± 0.85 | <0.001 |
| TG | 1.75 ± 1.54 | 1.03 ± 0.55 | <0.001 | |
| LDL/HDL | 3.41 ± 9.00 | 1.71 ± 0.67 | 0.12 | |
| LDL | 3.24 ± 0.89 | 2.71 ± 0.75 | <0.001 | |
| HDL | 1.44 ± 0.37 | 1.68 ± 0.39 | <0.001 | |
| n = 226 | n = 64 | |||
| Overweight and obese (n = 290) | TC | 5.12 ± 0.99 | 4.93 ± 0.89 | 0.16 |
| TG | 1.84 ± 1.84 | 1.23 ± 0.74 | <0.001 | |
| LDL/HDL | 2.30 ± 0.70 | 1.99 ± 0.73 | 0.002 | |
| LDL | 3.06 ± 0.78 | 2.95 ± 0.76 | 0.31 | |
| HDL | 1.39 ± 0.36 | 1.57 ± 0.40 | 0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, Y.; Li, N.; Kamishima, T.; Jia, P.; Zhou, D.; Hind, K.; Sutherland, K.; Cheng, X. Visceral Obesity and Lipid Profiles in Chinese Adults with Normal and High Body Mass Index. Diagnostics 2022, 12, 2522. https://doi.org/10.3390/diagnostics12102522
Lu Y, Li N, Kamishima T, Jia P, Zhou D, Hind K, Sutherland K, Cheng X. Visceral Obesity and Lipid Profiles in Chinese Adults with Normal and High Body Mass Index. Diagnostics. 2022; 12(10):2522. https://doi.org/10.3390/diagnostics12102522
Chicago/Turabian StyleLu, Yutong, Na Li, Tamotsu Kamishima, Peng Jia, Dan Zhou, Karen Hind, Kenneth Sutherland, and Xiaoguang Cheng. 2022. "Visceral Obesity and Lipid Profiles in Chinese Adults with Normal and High Body Mass Index" Diagnostics 12, no. 10: 2522. https://doi.org/10.3390/diagnostics12102522
APA StyleLu, Y., Li, N., Kamishima, T., Jia, P., Zhou, D., Hind, K., Sutherland, K., & Cheng, X. (2022). Visceral Obesity and Lipid Profiles in Chinese Adults with Normal and High Body Mass Index. Diagnostics, 12(10), 2522. https://doi.org/10.3390/diagnostics12102522





