“3D Counterpart Analysis”: A Novel Method for Enlow’s Counterpart Analysis on CBCT
Abstract
1. Introduction
2. Materials and Methods
2.1. 2D Horizontal Counterpart Analysis
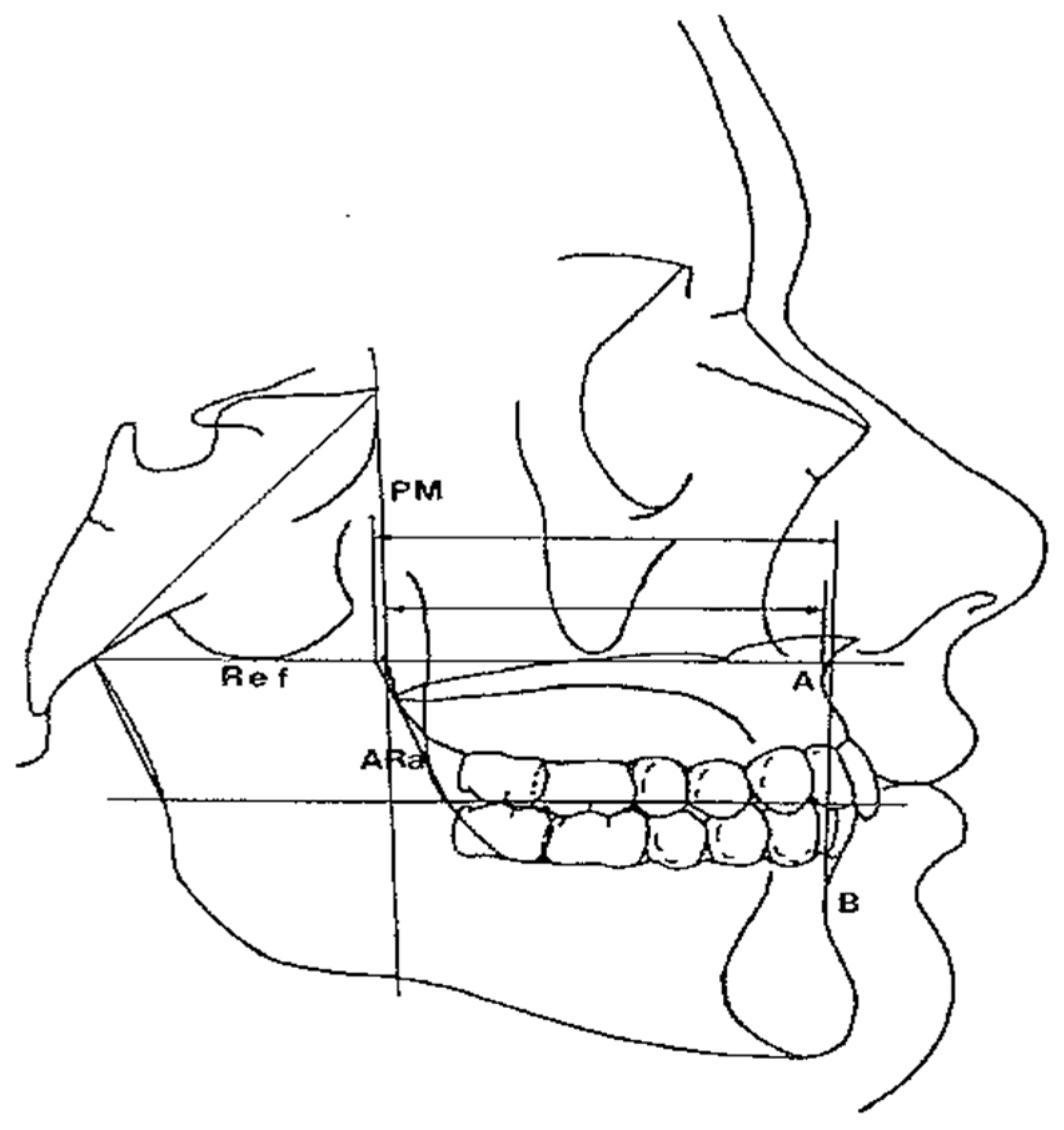
- Maxillary and Mandibular skeletal arches (Figure 1): this parameter compares the lengths of the maxillary and mandibular skeletal arches. The maxillary skeletal arch was measured by the distance between A point and PM, in parallel with Ref. The mandibular skeletal arch was measured by the distance between the orthogonal projection of B point on Ref and ARa, at its intersection point with Ref.
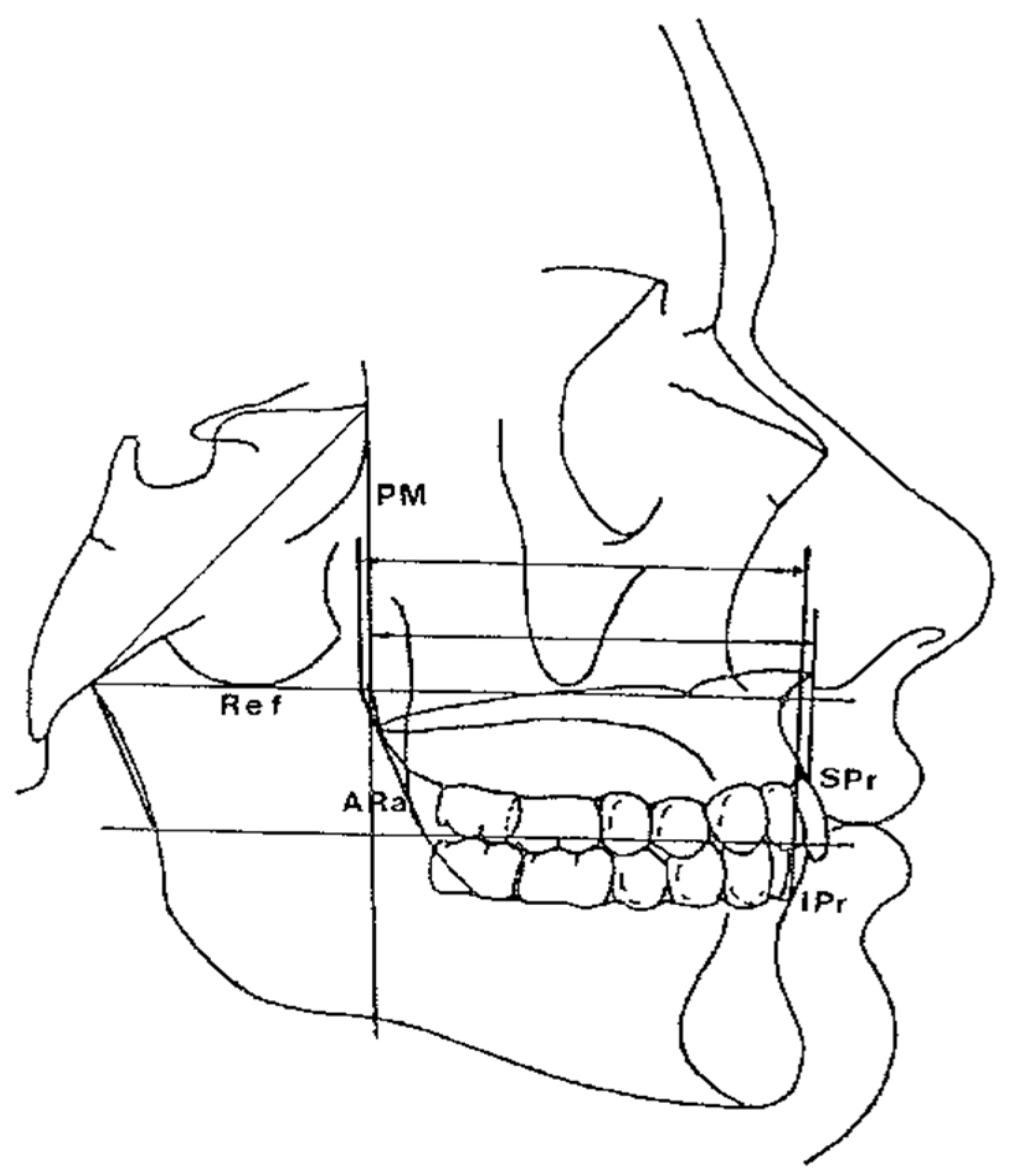
- Maxillary and Mandibular dento-alveolar arches (Figure 2): this parameter compares the lengths of maxillary and mandibular dento-alveolar arches. The maxillary dental arch was measured by the distance between PM and SPr, in parallel with Ref. The mandibular dental arch was measured by the distance between the orthogonal projection of IPr on Ref and Ara, at its intersection point with Ref.
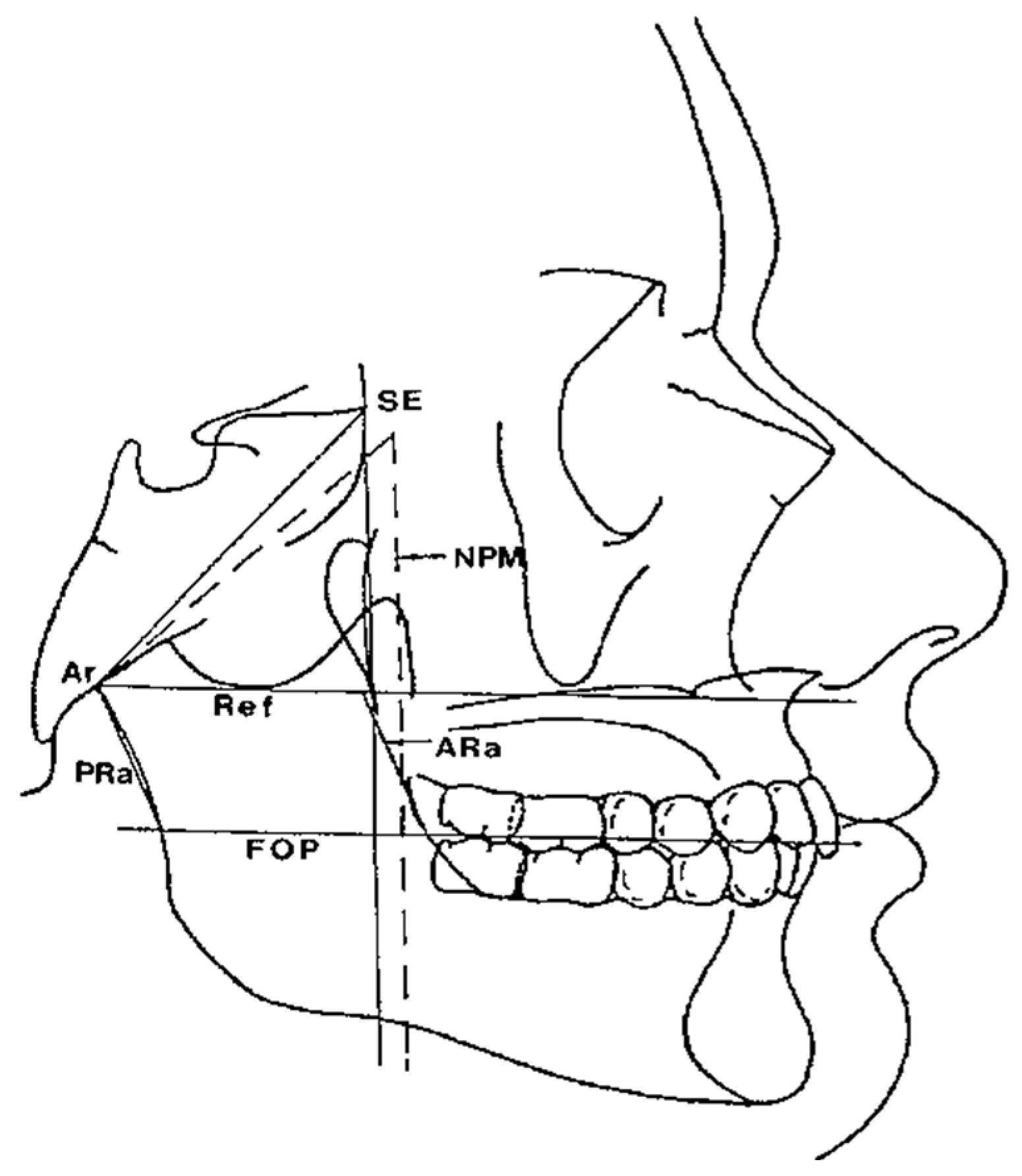
- Middle Cranial Floor (MCF) and Mandibular ramus (Figure 3): this parameter compares the horizontal dimension of the middle cranial floor (Ar to neutral PM) and the width of the ramus (Ar to ARa). These parameters were measured along the Ref.
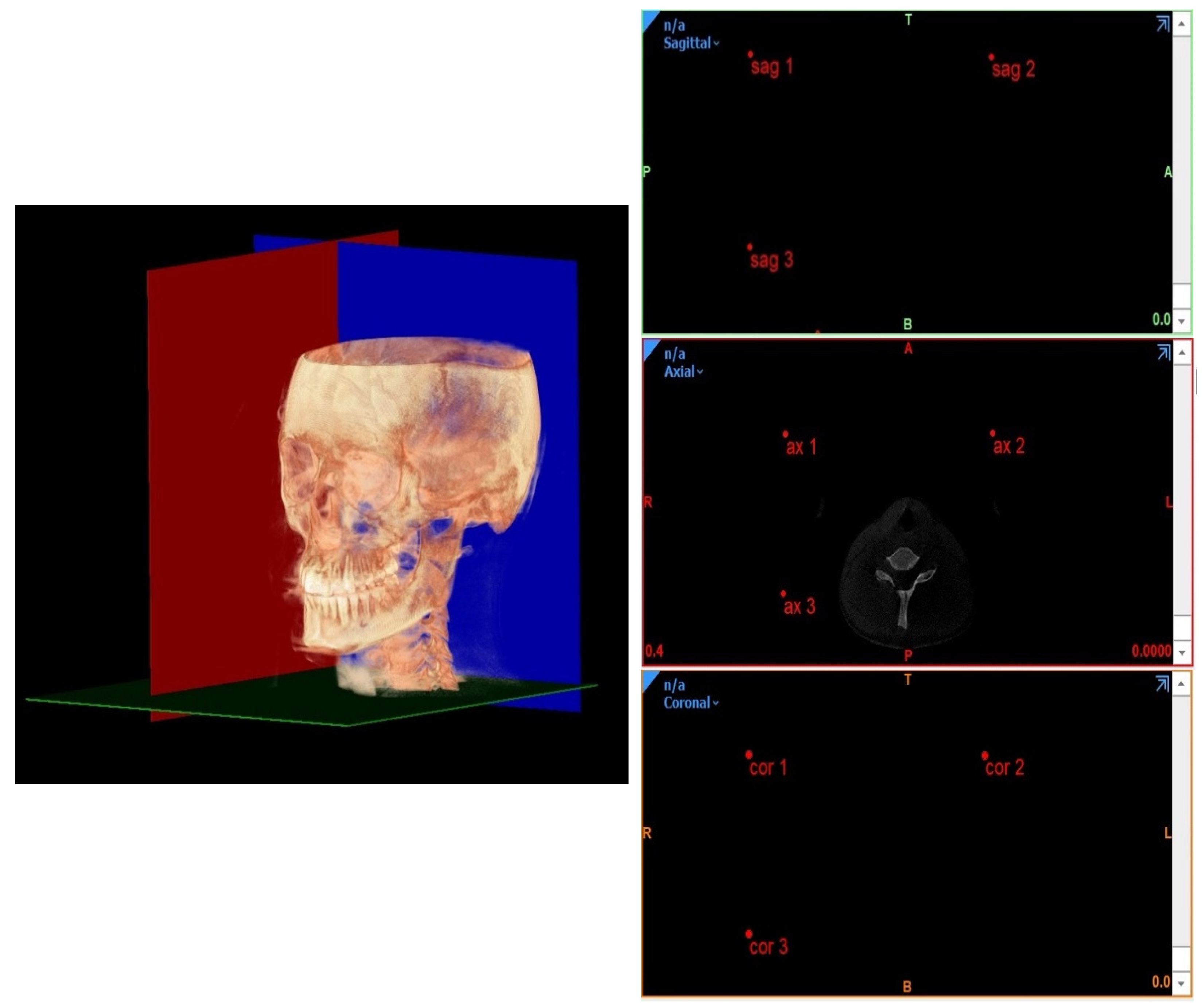
2.2. 3D Horizontal Counterpart Analysis
- Planes passing through 3 points;
- Planes passing through 2 points normal to a plane;
- Planes passing through 1 point parallel to a plane.
- ○
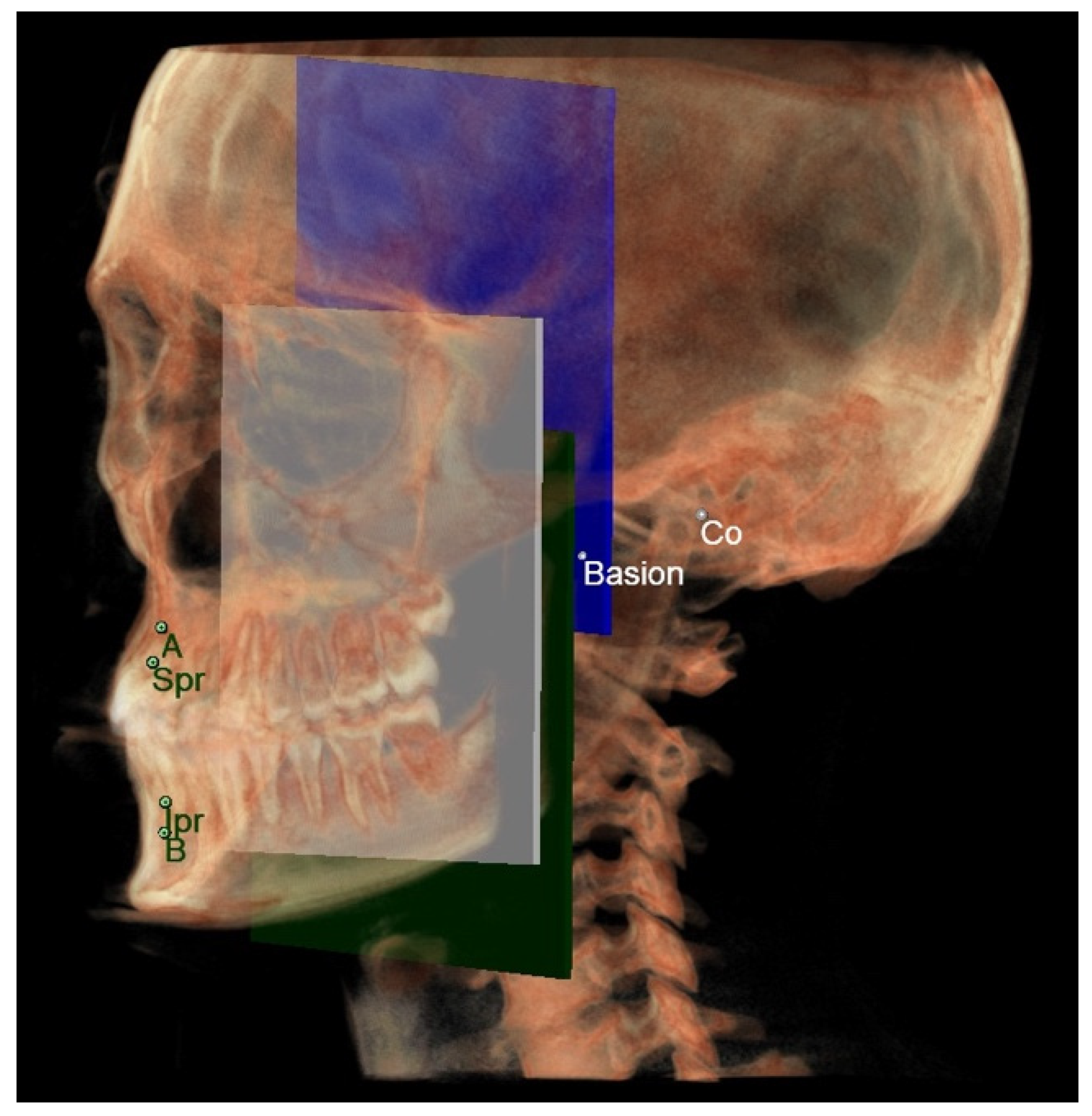
- The maxillary skeletal arch (Figure 6) was measured from point A to a plane passing through the PNS and parallel to the coronal plane.
- ○
- The mandibular skeletal arch (Figure 7) was measured from the point B to a plane passing through the two lingual tuberosity and normal to the axial plane
- ○
- The maxillary dento-alveolar arch (Figure 8) was measured from the point SPr to a plane passing through the PNS and parallel to the coronal plane.
- ○
- The mandibular dento-alveolar arch (Figure 9) was measured from the point IPr to a plane passing through the two lingual tuberosity and normal to the axial plane.
- ○
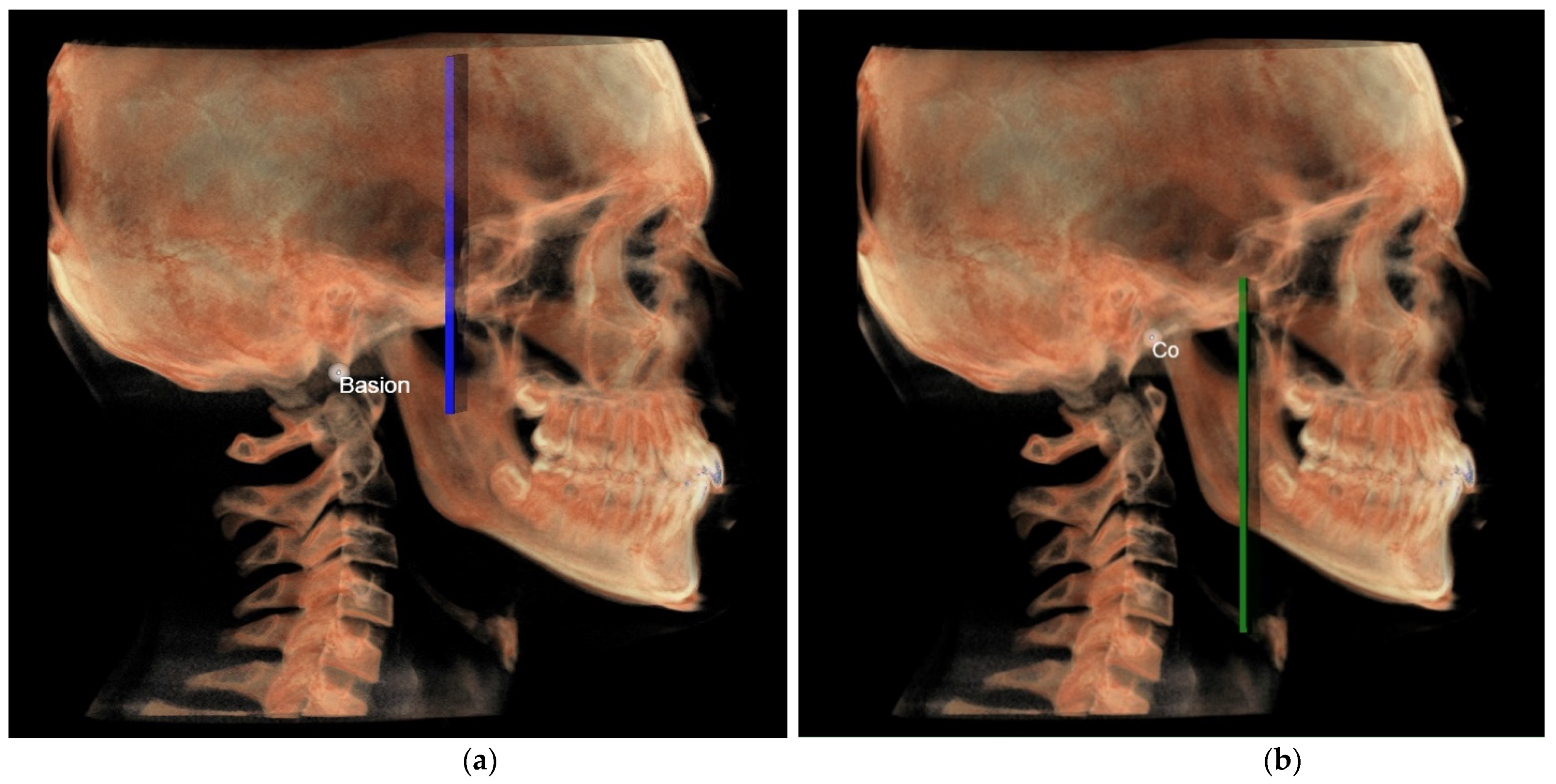
- The middle cranial floor (Figure 10) was determined by the distance from Ba to a plane passing through the two anterior clinoid processes and normal to the axial plane. The anterior clinoid processes were chosen as they represented the most posterior point of the anterior cranial floor and the most anterior point of the middle cranial floor.
- ○
- The mandibular ramus was measured from the right and left condylion to a plane passing through the right and left lingual tuberosity and normal to the axial plane (Figure 10).
2.3. Statistical Analysis
3. Results
Horizontal Counterpart Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Farronato, G.; Garagiola, U.; Dominici, A.; Periti, G.; de Nardi, S.; Carletti, V.; Farronato, D. “Ten-point” 3D cephalometric analysis using low-dosage cone beam computed tomography. Prog. Orthod. 2010, 11, 2–12. [Google Scholar] [CrossRef]
- Holberg, C.; Steinhäuser, S.; Geis, P.; Rudzki-Janson, I. Cone-beam computed tomography in orthodontics: Benefits and limitations. J. Orofac. Orthop. 2005, 66, 434–444. [Google Scholar] [CrossRef]
- Kau, C.H.; Richmond, S.; Palomo, J.M.; Hans, M.G. Three-dimensional cone beam computerized tomography in orthodontics. J. Orthod. 2005, 32, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Swennen, G.R.J.; Schutyse, F. Three-dimensional cephalometry: Spiral multi-slice vs cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Gateno, J.; Xia, J.J.; Teichgraeber, J.F. A New Three-Dimensional Cephalometric Analysis for Orthognathic Surgery. J. Oral Maxillofac. Surg. 2011, 69, 606–622. [Google Scholar] [CrossRef]
- Perrotti, G.; Baccaglione, G.; Clauser, T.; Testarelli, L.; Del Fabbro, M.; Testori, T. Total face approach (TFA) a novel 3D approach to describe the main cephalometric craniomaxillofacial parameters. Methods Protoc. 2021, 4, 15. [Google Scholar] [CrossRef]
- Juerchott, A.; Freudlsperger, C.; Zingler, S.; Saleem, M.A.; Jende, J.M.E.; Lux, C.J.; Bendszus, M.; Heiland, S.; Hilgenfeld, T. In vivo reliability of 3D cephalometric landmark determination on magnetic resonance imaging: A feasibility study. Clin. Oral Investig. 2020, 24, 1339–1349. [Google Scholar] [CrossRef]
- Castillo, J.C.; Gianneschi, G.; Azer, D.; Manosudprasit, A.; Haghi, A.; Bansal, N.; Allareddy, V.; Masoud, M.I. The relationship between 3D dentofacial photogrammetry measurements and traditional cephalometric measurements. Angle Orthod. 2019, 89, 275–283. [Google Scholar] [CrossRef]
- Pittayapat, P.; Limchaichana-Bolstad, N.; Willems, G.; Jacobs, R. Three-dimensional cephalometric analysis in orthodontics: A systematic review. Orthod. Craniofacial Res. 2014, 17, 69–91. [Google Scholar] [CrossRef] [PubMed]
- Smektała, T.; Jędrzejewski, M.; Szyndel, J.; Sporniak-Tutak, K.; Olszewski, R. Experimental and clinical assessment of three-dimensional cephalometry: A systematic review. J. Cranio-Maxillofac. Surg. 2014, 42, 1795–1801. [Google Scholar] [CrossRef] [PubMed]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D cephalometry on reduced FOV CBCT: Skeletal class assessment through AF-BF on Frankfurt Plane–validity and reliability through comparison with 2D measurements. Eur. Radiol. 2020, 30, 6295–6302. [Google Scholar] [CrossRef] [PubMed]
- Kissel, P.; Mah, J.K.; Bumann, A. Modern 3D cephalometry in pediatric orthodontics–downsizing the FOV and development of a new 3D cephalometric analysis within a minimized large FOV for dose reduction. Clin. Oral Investig. 2021, 25, 4651–4670. [Google Scholar] [CrossRef]
- Schwendicke, F.; Chaurasia, A.; Arsiwala, L.; Lee, J.H.; Elhennawy, K.; Jost-Brinkmann, P.G.; Demarco, F.; Krois, J. Deep learning for cephalometric landmark detection: Systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 4299–4309. [Google Scholar] [CrossRef]
- Enlow, D.H.; Hans, M.G. Essential of Facial Growth, 1st ed.; Saunders: Philadelphia, PA, USA, 1996. [Google Scholar]
- Moscagiuri, F.; Caroccia, F.; Lopes, C.; Di Carlo, B.; Di Maria, E.; Festa, F.; D’Attilio, M. Evaluation of Articular Eminence Inclination in Normo-Divergent Subjects with Different Skeletal Classes through CBCT. Int. J. Environ. Res. Public Health 2021, 18, 5992. [Google Scholar] [CrossRef]
- Enlow, D.H.; Kuroda, T.; Lewis, A.B. The morphogenetic basis for craniofacial form and pattern. Angle Orthod. 1971, 41, 161–188. [Google Scholar] [PubMed]
- Drake, R.L.; Vogl, A.W.; Mitchell, A.W.M. Gray’s Anatomy For Student, 3rd ed.; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Dubrul, L.E. Sicher’s Oral Anatomy Italian Edition; Edi.Ermes: Milan, Italy, 1982. [Google Scholar]
- Lucchese, A.; Manuelli, M. Prognosis of third molar eruption: A comparison of three predictive methods. Prog. Orthod. 2003, 4, 4–19. [Google Scholar]
- Park, S.H.; Yu, S.H.; Kim, D.K.; Lee, K.J.; Baik, H.S. A proposal for a new analysis of craniofacial morphology by 3 dimensional computed tomography. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 600.e23–600.e34. [Google Scholar] [CrossRef]
- Dos Santos, R.M.G.; De Martino, J.M.; Neto, F.H.; Passeri, L.A. Cone beam computed tomography-based three-dimensional McNamara cephalometric analysis. J. Craniofacial Surg. 2018, 29, 895–899. [Google Scholar] [CrossRef]
- Bayome, M.; Park, J.H.; Kook, Y.A. New three dimensional cephalometric analyses among adults with a skeletal Class I pattern and normal occlusion. Korean J. Orthod. 2013, 43, 62–73. [Google Scholar] [CrossRef]
- Wang, R.H.; Ho, C.T.; Lin, H.H.; Lo, L.J. Three-dimensional cephalometry for orthognatic planning: Normative data and analyses. J. Formos. Med. Assoc. 2020, 119, 191–203. [Google Scholar] [CrossRef] [PubMed]
- Cheung, L.K.; Chan, Y.M.; Jayaratne, Y.S.N.; Lo, J. Three-dimensional cephalometric norms of Chinese adults in Hong Kong with balanced facial profile. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2011, 112, e56–e73. [Google Scholar] [CrossRef]



| Landmarks | |
|---|---|
| Go | Gonion: Geometric construction point given by the intersection of two lines, one passing from Me to the lower most point of the mandibular corpus, the other passing from Ar to the posterior most point of mandibular ramus |
| Ar | Articulare: Point of intersection between the posterior margin of the ramus and the outer margin of the cranial base |
| Me | Menton: Most inferior point of the mandibular symphysis |
| SE | Sphenoethmoidal junction: Intersection of the averaged image of the right and left shadows of the great wings of the sphenoid with the floor of the anterior cranial fossae |
| PTM | Lowest point in the contour of the pterygomaxillary fissure formed anteriorly by the retromolar tuberosity of the maxilla and posteriorly by the anterior curve of the pterigoid process of the sphenoid bone |
| Poc | Posterior occlusal contact: Most supero-distal contact point of the first molars. |
| Aoc | Anterior occlusal contact: Most mesial contact point of the first premolars or first deciduous molars. |
| A | Most concave point of the anterior maxilla |
| SPr | Superior Prostion: Occlusal limit of bone papillae of the maxillary alveolar bone |
| IPr | Inferior Prostion, occlusal limit of bone papillae of the mandibular alveolar bone |
| B | Most concave point of the mandibular symphysis |
| LT | Lingual tuberosity: Point of intersection between the FOP and the anterior border of mandibular ramus |
| Lines | |
| FOP | Functional occlusal plane, Poc–Aoc |
| PM | Pterygo-mandibular plane, SE-PTM |
| MCF | Middle cranial floor plane, Ar-SE |
| PRa | Posterior ramus alignment: Distance from point Ar to the point where the FOP intersects the posterior margin of the mandibular ramus |
| ARa | Anterior ramus alignment: Line parallel to the PRa from LT to the ref line |
| Ref | Reference plane: Line parallel to the FOP passing through point Ar |
| MR | Mandibular ramus: Ar-Go |
| Point | X (Left to Right) Sagittal View | Y (Superior to Inferior) Axial View | Z (Posterior to Anterior) Coronal View |
|---|---|---|---|
| Basion (Ba) | / | Most anterior point of foramen magnum | / |
| Right condylion (rCo) | Most posterior point of the mandibular condyle, right side | Most posterior point of mandibular condyle, right side | Most posterior point of mandibular condyle, right side |
| Left condylion (lCo) | Most posterior point of mandibular condyle, left side | Most posterior point of mandibular condyle, left side | Most posterior point of mandibular condyle, left side |
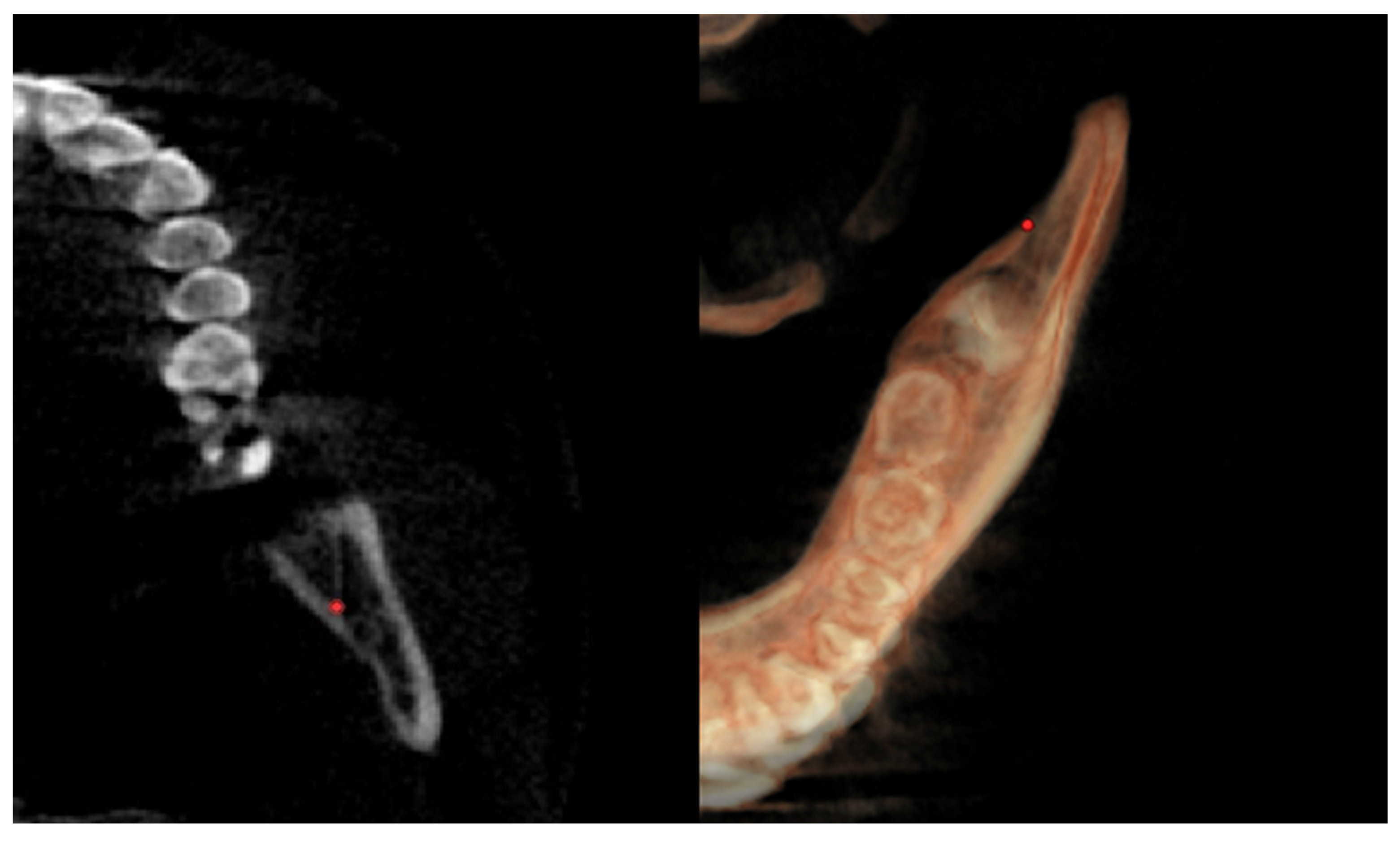
| Right lingual tuberosity (rLT) | / | The most posterior point (apex) of the retromandibular triangle, right side (Figure 5) | / |
| Left lingual tuberosity (lLT) | / | The most posterior point (apex) of the retromandibular triangle, left side (Figure 5) | / |
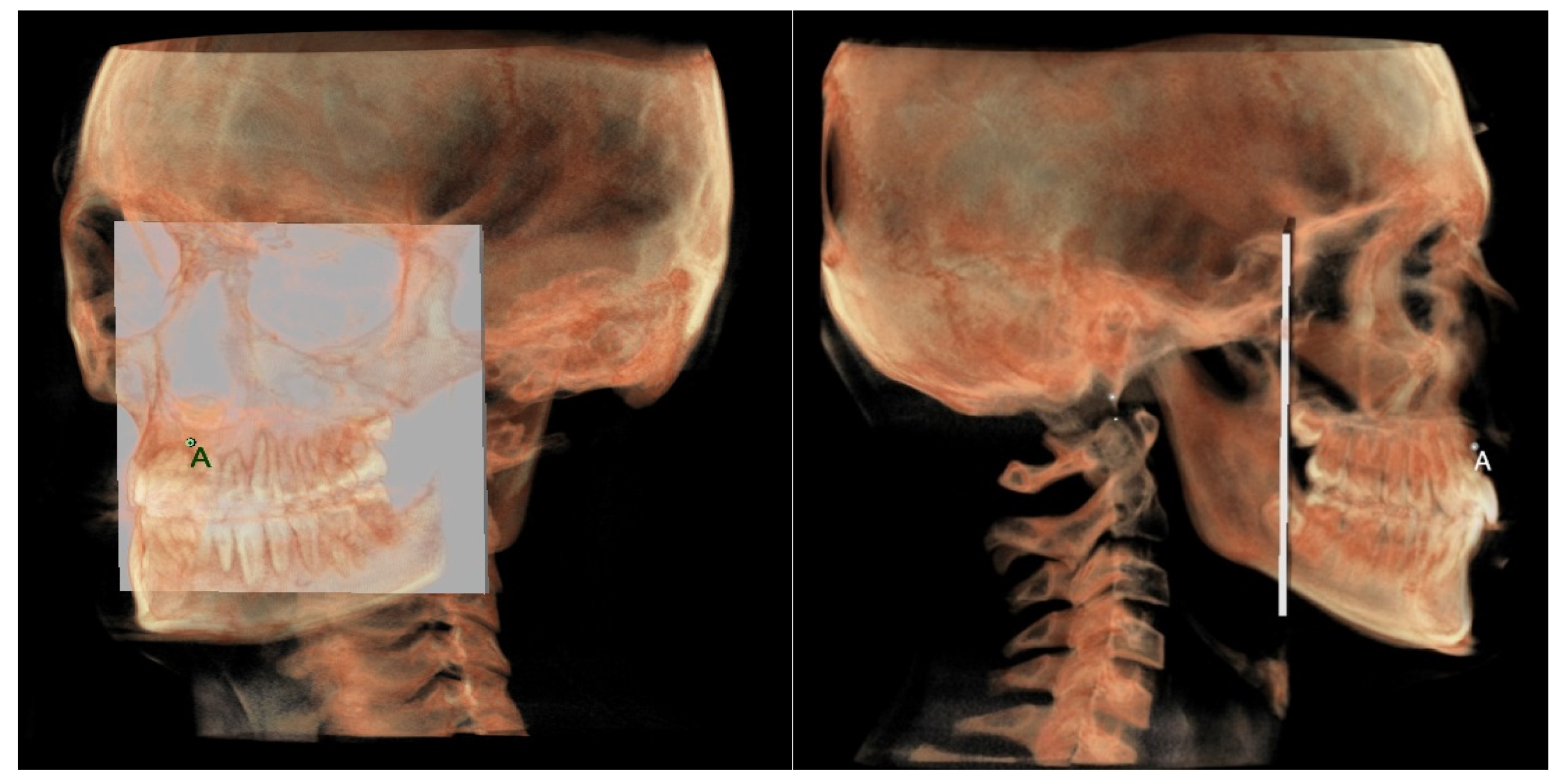
| A | Most concave point on the midline of anterior maxilla | / | / |
| B | Most concave point on the midline of mandibular symphysis | / | / |
| SPr | Most anterior point on the maxillary alveolar process between the central incisor | Most anterior point on the maxillary alveolar process between the central incisor | Most anterior point on the maxillary alveolar process between the central incisor |
| IPr | Most anterior point on the mandibular alveolar process between the central incisor | Most anterior point on the mandibular alveolar process between the central incisor | Most anterior point on the mandibular alveolar process between the central incisor |
| Posterior nasal spine (PNS) | Most posterior point of the hard palate | Most posterior point of the hard palate | Most posterior point of the hard palate |
| Right anterior clinoid process | Most posterior point of the anterior clinoid process, right side | Most posterior point of the anterior clinoid process, right side | Most posterior point of the anterior clinoid process, right side |
| Left anterior clinoid process | Most posterior point of the anterior clinoid process, left side | Most posterior point of the anterior clinoid process, left side | Most posterior point of the anterior clinoid process, left side |
| Index | 2D (Mean ± SD) | 3D (Mean ± SD) | p Value a |
|---|---|---|---|
| Middle cranial floor-mandibular ramus Maxillary-mandibular skeletal arches Maxillary-mandibular dento-alveolar arches | 0.15 ± 0.12 cm | 0.17 ± 0.09 cm | 0.91 |
| −0.52 ± 0.25 cm | −0.54 ± 0.33 cm | 0.89 | |
| −0.29 ± 0.14 cm | −0.47 ± 0.13 cm | 0.18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Attilio, M.; Peluso, A.; Falone, G.; Pipitone, R.; Moscagiuri, F.; Caroccia, F. “3D Counterpart Analysis”: A Novel Method for Enlow’s Counterpart Analysis on CBCT. Diagnostics 2022, 12, 2513. https://doi.org/10.3390/diagnostics12102513
D’Attilio M, Peluso A, Falone G, Pipitone R, Moscagiuri F, Caroccia F. “3D Counterpart Analysis”: A Novel Method for Enlow’s Counterpart Analysis on CBCT. Diagnostics. 2022; 12(10):2513. https://doi.org/10.3390/diagnostics12102513
Chicago/Turabian StyleD’Attilio, Michele, Antonino Peluso, Giulia Falone, Rossana Pipitone, Francesco Moscagiuri, and Francesco Caroccia. 2022. "“3D Counterpart Analysis”: A Novel Method for Enlow’s Counterpart Analysis on CBCT" Diagnostics 12, no. 10: 2513. https://doi.org/10.3390/diagnostics12102513
APA StyleD’Attilio, M., Peluso, A., Falone, G., Pipitone, R., Moscagiuri, F., & Caroccia, F. (2022). “3D Counterpart Analysis”: A Novel Method for Enlow’s Counterpart Analysis on CBCT. Diagnostics, 12(10), 2513. https://doi.org/10.3390/diagnostics12102513









