1. Introduction
Thyroid neoplasm is a rare disease with an incidence of 586,000 worldwide and 87,000 in Europe [
1]. Differentiated thyroid carcinoma (DTC) represents over 90% of all thyroid neoplasms [
2], of which 10–30% are metastatic [
3,
4].
Treatment of metastatic DTC includes levothyroxine at suppressive dosage, local treatments (such as surgery, external beam therapy, thermoablation, etc.) and radio-iodine (RAI) therapy [
5,
6]. Unfortunately, a range of 60–70% of metastatic DTCs will become RAI refractory (RAI-R) [
7]. The definition of RAI-R tumors is controversial, but most recommendations and publications retain the following criteria [
8]: absence of initial RAI uptake, absence of RAI uptake after treatment with RAI in at least one metastasis, progression of at least one metastasis despite RAI uptake in all metastases and extensive RAI exposure, which includes patients who have received cumulatively 600 mCi (22.2 GBq) or more of RAI without signs of remission.
Mortality rates of patients with DTC from all stages are low (93% overall survival at 5 years) [
9] but rise considerably in the case of metastasis (from 25 to 40% overall survival at 10 years) [
7,
10] and are even higher in the case of RAI-R metastatic DTC (10% overall survival at 10 years) [
7]. Unlike most DTCs, RAI-R metastatic DTCs median survival is low, estimated at 3–5 years [
11].
Therapeutic resources for RAI-R metastatic DTCs are limited and can significantly impair patients’ quality of life. The two multikinase inhibitors available for the treatment of RAI-R DTC in Europe, lenvatinib [
12] and sorafenib [
13] led to 64–85% of grade 3 or more adverse events [
14]. For these reasons, for asymptomatic patients with stable or slowly progressive RAI-R metastatic DTC, a monitoring attitude is recommended, with the aim of therapeutic sparing [
8]. A treatment by multikinase inhibitors should be considered in case of tumor progression and/or threatening metastasis when a focal treatment is not possible [
6].
Therefore, the identification of factors of poor prognosis is essential in order to start early targeted treatment for patients who could benefit from it. Several staging systems to select patients at high risk of cancer death for more aggressive treatment have been developed, such as the EORTC system [
15], MACIS system [
16] or AMES score [
17]. Unfortunately, none of these systems were able to accurately predict cancer-related death risk at an individual level [
18]. The factors of poor prognosis identified to date are male gender [
9], age≥ 55 years old [
19], doubling time of thyroglobulin <1 year [
20], histologic type [
21], the presence of BRAF
V600E mutation [
22], the absence of iodine uptake [
7,
10,
23] and a high tumor burden [
7,
24,
25].
An
18F-FDG PET/CT is recommended for patients with metastatic DTC in order to identify the sites of metastasis and FDG status [
6]. PET-positive lesions are generally of less differentiated histologic type compared with primary thyroid tumors [
26]. Several studies have shown that the intensity of FDG avidity [
23], the number of FDG avid lesions [
24,
27] and the volume of PET-positive lesions [
28] are prognostic factors of poorer survival, while the intensity of
18F-FDG uptake is not predictive of tumor growth in patients with metastatic DTC [
29].
The aim of this study is to determine 18F-FDG PET/CT parameters predictive of survival in patients with RAI-R metastatic DTC.
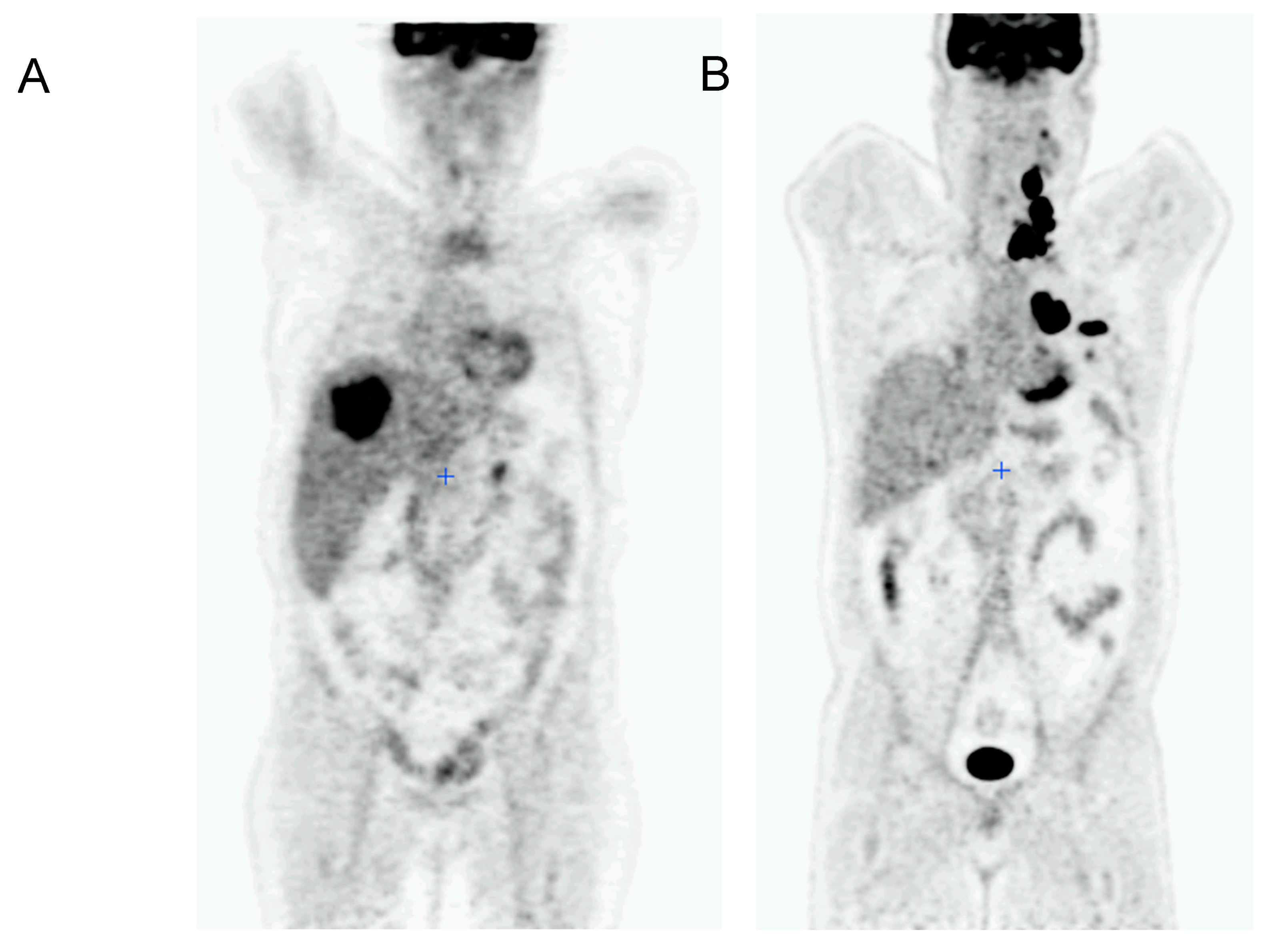
4. Discussion
In this study, we showed that 18FDG PET/CT metrics of metastasis located in the mediastinum and the liver and of the overall tumor burden were prognostic factors of poor overall survival at 1 year and 5 years.
The population of our study was similar to most studies on RAI-R DTC in age and sex distribution, but our patients showed a higher frequency of aggressive pathologic types, at 32%, while the usual rate is 3–24% [
35,
36,
37]. Consistently, the median OS of our population was 22 months, shorter than the expected 3–5 years described in the literature [
38]. On the contrary, in our population, only 20.5% of patients had stage IV AJCC/TNM while this group usually represents 40–50% of patients with RAI-R DTC. The reason for this difference in staging is that we used the eighth edition of the AJCC/TNM classification, implemented on 1 January 2018, which reclassified all metastatic patients aged between 45 and 55 years from stage IV to stage II [
39]. These observations might have introduced a bias in our study since histologic type and AJCC/TNM stage are known prognostic factors of DTC survival. Nevertheless, age, sex, histologic type and stage were not significant prognostic factors of OS in this study. This might be explained by the fact that the inclusion criteria of our study selected patients at a high risk of disease-related death, thus abolishing the pertinence of usual risk factors.
The
18FDG PET/CT metrics we analyzed, MTV and SUVmax, were highly correlated by Spearman’s correlation, with a correlation coefficient close to 1 (minimal ρ = 0.74) regardless of the site of metastasis. We chose to study them nonetheless since both MTV and SUVmax have shown their prognostic value in previous studies [
23,
28].
Metabolic tumor volume is representative of tumor burden, and a high overall tumor burden has long been known to be a factor in poor prognosis. In 2006, a study by Durante et al. of 444 patients with distant metastasis showed that those who had macronodular lung metastasis or multiple bone metastases or both bones and lung metastases had a 7.3 relative risk of death (
p < 0.0001) compared to patients with metastasis on 131 I-TBS but with normal chest and bone x-rays [
7]. In another study in 2011 of 80 patients with metastatic DTC, the two-year survival was 50% for patients with more than 10 lesions with FDG uptake (
p = 0.009) against 70-80% for patients with 1–10 lesions and 100% for patients without lesions with FDG uptake [
24]. Furthermore, in a recent study of 717 patients with metastatic DTC, the presence of 3 or more different distant organ system metastases was the only independent prognostic factor of 10-year OS by multivariate analysis [
25]. Concordantly, Terroir et al. showed that an MTV/patient ≥ 15.2 cm
3 was predictive of poorer 1-year and 2-year OS (
p = 0.005) [
29] and Manohar et al. showed that MTV values above the median were predictive of poorer progression-free survival (
p = 0.007) [
36]. Our results are therefore in accordance with previous studies.
The standardized uptake value is representative of the glycolytic rate of tumors, which is higher in malignant cells. It has been demonstrated that the majority of RAI-R lesions with high FDG avidity are of an aggressive histologic type and correspond to a transformation to a higher grade compared to the primary tumor [
26]. Several studies have shown that the SUV is negatively correlated with OS and have suggested cut-off values ranging from 5 to 13.3 g/mL [
23,
24,
27,
28]. In our study, SUVmax cut-off values were 3.9 for the mediastinum (
p = 0.002), 5.3 for the liver (
p = 0.001) and 18.6 for the total SUVmax (
p = 0.026).
The most common site of metastasis of DTC is the lungs [
3,
7,
10,
24,
40], a finding which was also true in our study with 71% of patients bearing lung metastasis. Respiratory deficiency is the main cause of death in patients with metastatic DTC [
41,
42]. However, lung MTV was not found to be a significant prognostic factor either for 1-year OS or 5-year OS in this study. This could be explained by the frequency of miliary metastases for which the estimation of tumor volume is challenging on
18FDG PET/CT and was observed in 72% of our patients who had lung metastasis. Similarly, a study of 138 patients with metastatic DTC did not find that lung tumor volume was predictive of survival, despite a significant effect on progression-free survival in univariate and multivariate analysis [
43].
Liver MTV was also a significant prognostic factor identified in our study, most probably because metastases in this organ attest to a more advanced stage of illness. Indeed, liver metastases occur in less than 7% of cases of metastatic DTC that are not RAI-R [
7,
13,
35]. On the contrary, in our study, 24% of patients had liver metastases, a rate comparable to those described in the literature for RAI-R DTC that range from 16 to 36% [
25,
44,
45,
46] and liver metastases are rarely sensitive to RAI treatment [
47]. The median volume of liver metastasis in our study was zero, with a range of 0–181.2 cm
3, which means that the results obtained from the analysis of these data can be interpreted as binary instead of continuous. This was evidenced by the binary univariate Cox analysis, which showed a significant association between liver MTV (HR 15.2;
p = 0.015) and overall survival at 1 year. Shah et al. analyzed a cohort of 11 patients bearing liver metastases from DTC and showed that the survival rate was poor but could not be attributed to liver metastases per se because of the extensive metastatic disease at other sites [
48]. Therefore, the presence of liver metastasis itself is a factor of a poor prognosis, regardless of volume.
Patients demonstrating more rapid disease progression over time can be expected to reach a lethal tumor burden more quickly than patients with slowly growing or stable disease [
49]. In our study, this was only true for the progression of lesions in the mediastinum and the liver, as they were the only sites of the progression predictive of poor 1-year and 5-year OS. As discussed above, the progression of pulmonary lesions may have been underestimated because of resolution limitations. Of the 24 patients who had neck lesions, 12 (50%) underwent surgery (
n = 9) or external beam therapy (EBT) (
n = 3) after the reference PET/CT. The absence of correlation between the progression of neck lesions and OS could be explained by the efficacy of surgical reintervention and EBT. The progression of bone metastases might not be predictive of poor OS because they are associated with skeletal-related events responsible for functional-threatening rather than life-threatening complications and usually respond to local treatments such as EBT, radiofrequency or cementoplasty. Therefore, our study reveals the importance of providing more effective treatment for liver and mediastinum lesions that may have fewer therapeutic resources than neck or bone lesions.
In our study, death occurred in 59% of patients. The causes of death were respiratory deficiency (40%), heart failure (10%), kidney failure (5%) or unknown (45%). Thyroid cancer is the main cause of death in patients with metastatic DTC [
41,
50,
51,
52]. Respiratory insufficiency due to large pulmonary metastases replacing lung tissue, massive hemorrhage and airway obstruction due to uncontrolled local tumors, and circulatory failure resulting from compression of the vena cava by extensive mediastinal or sternal metastases have been found to be the most important immediate causes of death [
41,
42,
53]. These findings are consistent with the results of our study, which demonstrated that neck MTV was a prognostic factor of 1-year and of 5-year OS and that mediastinum MTV was a significant factor of poor prognosis by ROC and Kaplan–Meier analysis (
p = 0.002).
One of the strengths of our study is that we have analyzed a rare population, whose incidence is estimated at 4–5 cases per million inhabitants [
5]. Indeed, our enrolment of 34 patients is comparable to other cohorts with similar inclusion criteria [
27,
29,
35,
36,
37].
Our primary endpoint was overall survival at 1 year and 5 years. Overall survival appears to be the most relevant endpoint because it is a precise, objective event not subject to observer interpretation, unlike progression-free survival or disease-specific survival. The median overall survival of patients with iodine-refractory CDT is 3 years [
54] so we chose to study overall survival at 1 year and 5 years to identify short- and medium-term factors of poor prognosis.
One of the main strengths of our study is its originality. Many authors have focused on FDG PET/CT parameters in search of prognostic factors of survival in RAI-R DTC. In contrast, this study is the only one to our knowledge that has investigated these parameters in relation to the organs bearing DTC metastasis. This approach allows a better correlation of FDG PET/CT parameters with the immediate causes of death, thus identifying in patients the lesions at risk of poor prognosis that would require early management.
The main weakness of our study was its retrospective and single-center nature, which included a small number of patients. As stated above, RAI-R DTC is a rare disease, the diagnosis of which is based on a range of investigations (thyroglobulin level, anatomical imaging, post-therapy scintigraphy, FDG PET/CT). For these reasons, the implementation of a prospective study to identify prognostic factors for survival is difficult in this population.
Among the FDG PET/CT parameters, we did not study the SUL peak (peak SUV normalized to the patient’s lean mass). This is the recommended quantitative component according to the PERCIST (PET Response Criteria In Solid Tumors) criteria used for the follow-up of patients with solid cancers. The SUL peak was a prognostic factor of progression-free survival in one study [
27]. It was not possible for us to analyze this parameter because of the heterogeneity of the CT scans to which PET was coupled and from which lean mass was calculated.
This study included patients managed at the Henri Becquerel Cancer Centre between April 2007 and December 2019. During this period, two multikinase inhibitor treatments, sorafenib and lenvatinib, were approved by the European Medicines Agency in 2015. The absence of systemic treatment prior to FDG PET/CT was among our inclusion criteria. However, some patients, particularly those included after 2015, were able to benefit from these new therapies, which have demonstrated efficacy on survival [
12,
13]. This difference in management could have introduced a bias in our study on survival between patients who were treated or not with multikinase inhibitors. However, in our study, kinase inhibitor treatment was not correlated with OS at 1 year and at 5 years in Cox univariate analysis. This result does not refute the benefit of TKI treatment since our study was not designed for this purpose.
It has been shown that the sensitivity of FDG PET/CT may be increased for the number of lesions detected after recombinant human TSH (rhTSH) stimulation compared to FDG-PET/CT performed on suppressive thyroid hormone treatment [
55]. However, the sensitivity for detecting patients with at least one tumor site was not improved by the rhTSH stimulation and the clinical benefit of identifying these additional small lesions remains to be proven.
Finally, the presence of the BRAF
V600E mutation and thyroglobulin doubling time <1 year are poor prognostic factors that we did not include in our analysis. A recent study confirmed that thyroglobulin correlated with overall survival but that MTV was not significantly correlated with thyroglobulin levels [
56]. The retrospective design of our study did not allow for the reliable collection of thyroglobulin levels and BRAFV600E mutation of the included patients because blood samples were often analyzed in external laboratories and surgery was frequently conducted in a care center other than the Henri Becquerel Cancer Centre.
In conclusion, in this study, we demonstrated that in radio-iodine refractory differentiated thyroid cancer, 18FDG PET/CT parameters of the mediastinum, the liver and the overall tumor burden were prognostic factors of poor overall survival at 1 year and 5 years. The identification of these criteria could allow patients to benefit from an early therapeutic intervention in order to improve their overall survival.