Weaning Failure in Critically Ill Patients Is Related to the Persistence of Sepsis Inflammation
Abstract
:1. Introduction
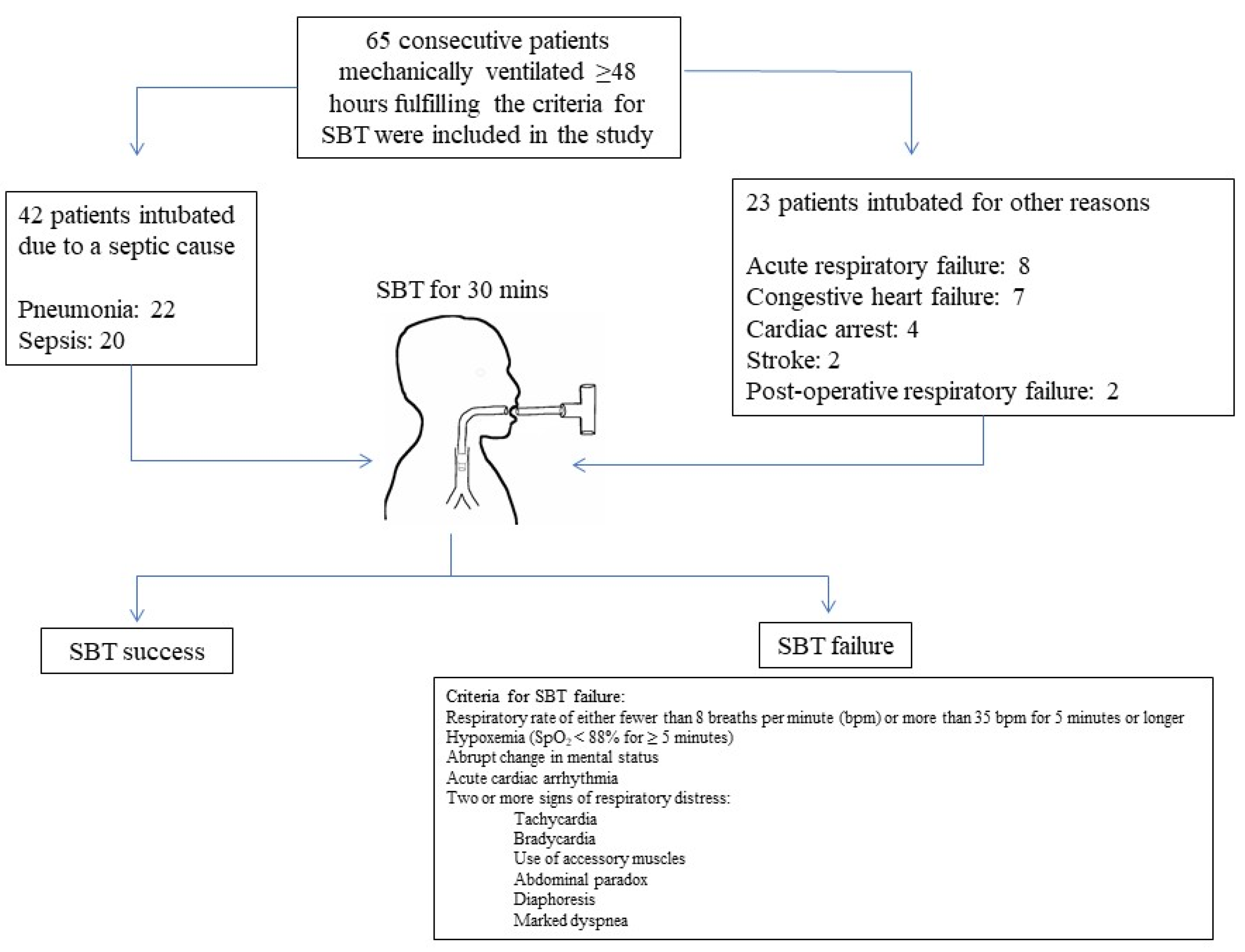
2. Materials and Methods
- ○
- Improvement or resolution of causes leading to acute respiratory failure;
- ○
- Partial Arterial Oxygen tension (PO2) > 60 mmHg with inspired Oxygen fraction (FiO2) < 0.4 and Peep 8 cm H2O;
- ○
- Normal consciousness after discontinuation of sedation (CGS > 9);
- ○
- Without fever (temperature > 38 °C) or hypothermia (temperature < 35 °C);
- ○
- Hgb > 8md/gL;
- ○
- Without hemodynamic instability or need for vasopressors.
- ○
- Intubation and mechanical ventilation for less than 48 h;
- ○
- Age under 18 years old;
- ○
- Tracheostomy (because of need for prolonged weaning);
- ○
- Collaborative patients;
- ○
- Patients with active upper gastrointestinal bleeding;
- ○
- Immunocompromised patients or with human immunodeficiency virus (HIV);
- ○
- Patients receiving a sedative infusion for active seizures or alcohol withdrawal;
- ○
- Patients with evidence of active myocardial ischemia in prior 24 h;
- ○
- Patients with evidence of increased intracranial pressure;
- ○
- Decision to limit life-sustaining treatments.
2.1. Study Protocol
- i.
- Appearance of dyspnea or diaphoresis.
- ii.
- Hypoxemia as defined with saturation of oxygen (SatO2) < 90% when FiO2 0.4 and/or hypercapnia (PaCO2 ˃ 45 mmHg) or respiratory acidosis.
- iii.
- Tachypnea (RR > 35/min) or tachycardia (HR > 140 beats/min) or increases or decreases in HR of more than 20% compared with mechanical ventilation.
- iv.
- Hypertension or hypotension (increase or decrease of blood pressure >20% compared with mechanical ventilation.
- v.
- Impaired consciousness or agitation.
- vi.
- Use of auxiliary respiratory muscles or paradoxical thoraco-abdominal movement.
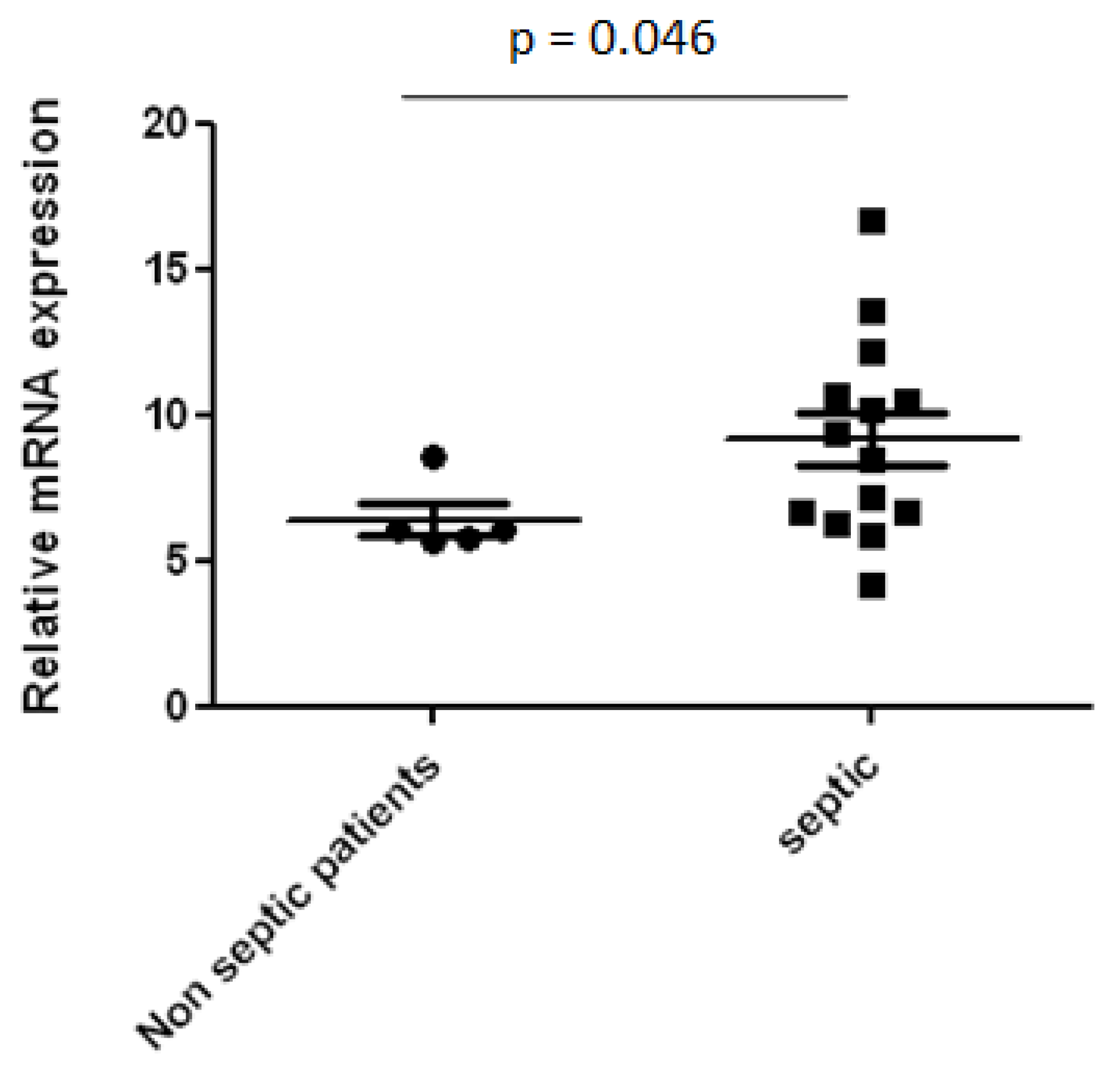
2.2. mRNA Expression of IL-18
2.3. Statistical Analysis
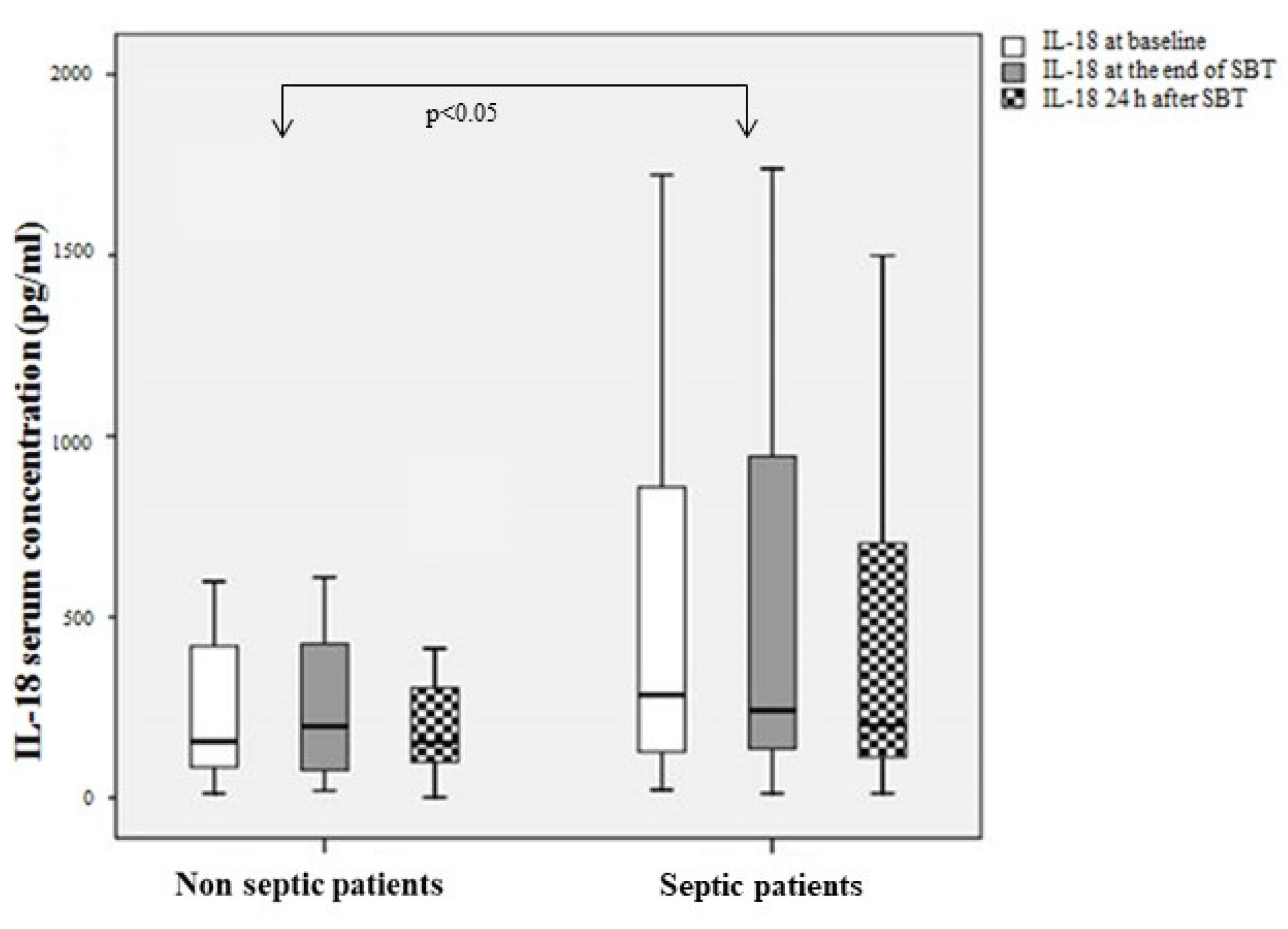
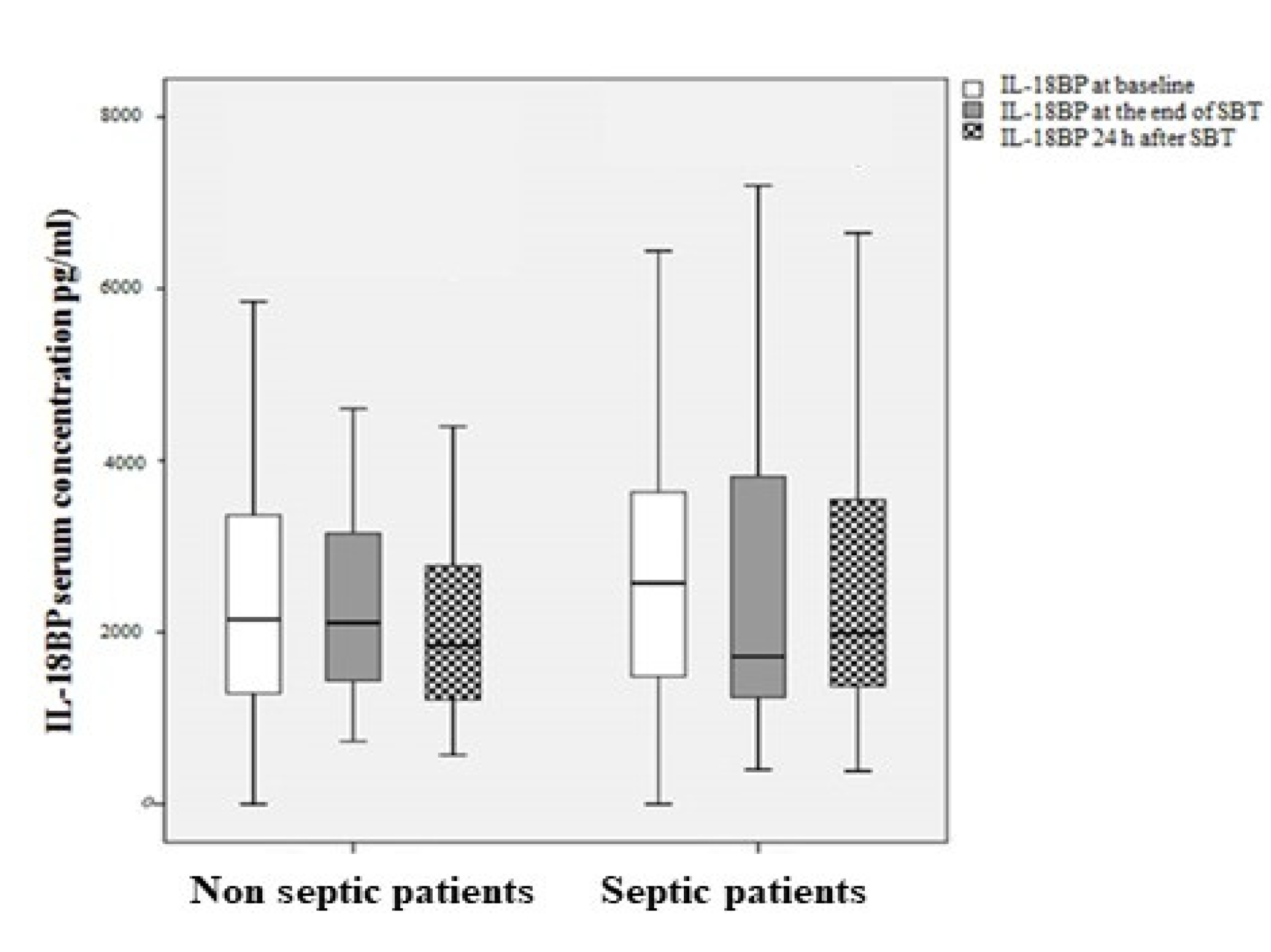
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Angus, D.C.; Linde-Zwirble, W.T.; Lidicker, J.; Clermont, G.; Carcillo, J.; Pinsky, M.R. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit. Care Med. 2001, 29, 1303–1310. [Google Scholar] [CrossRef] [PubMed]
- Amoateng-Adjepong, Y.; Jacob, B.K.; Ahmad, M.; Manthous, C.A. The effect of sepsis on breathing pattern and weaning outcomes in patients recovering from respiratory failure. Chest 1997, 112, 472–477. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.L.; Tobin, M.J. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N. Engl. J. Med. 1991, 324, 1445–1450. [Google Scholar] [CrossRef] [PubMed]
- Epstein, S.K. Evaluation of the rapid shallow breathing index (RVR) in the clinical setting. Am. J. Respir. Crit. Care Med. 1995, 152, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Chatila, W.; Jacob, B.; Guaglionone, D.; Manthous, C.A. The unassisted respiratory rate:tidal volume ratio accurately predicts weaning outcome. Am. J. Med. 1996, 101, 61–67. [Google Scholar] [CrossRef]
- Eastwood, P.; Hillman, D.; Finucane, K.E. Ventilator. Ventilatory responses to inspiratory threshold loading and role of muscle fatigue in task failure. J. Appl. Physiol. 1994, 76, 185–195. [Google Scholar] [CrossRef]
- Thijs, L.G.; Hack, C.E. Time course of cytokine levels in sepsis. Intensiv. Care Med. 1995, 21, S258–S263. [Google Scholar] [CrossRef]
- Claeys, R.; Vinken, S.; Spapen, H.; ver Elst, K.; Huyghens, L.; Gorus, F.K. Plasma procalcitonin and C-reactive protein in acute septic shock: Clinical and biological correlates. Crit Care Med. 2002, 30, 757–762. [Google Scholar] [CrossRef]
- Sellarés, J.; Loureiro, H.; Ferrer, M.; Amaro, R.; Farre, R.; Torres, A. The effect of spontaneous breathing on systemic interleukin-6 during ventilator weaning. Eur. Respir. J. 2012, 39, 654–660. [Google Scholar] [CrossRef]
- Forgiarini, S.G.I.; Rosa, D.; Forgiarini, L.F.; Teixeira, C.; Andrade, C.F.; Forgiarini, L.A.; Felix, E.A.; Friedman, G. Evaluation of systemic inflammation in patients being weaned from mechanical ventilation. Clinics 2018, 73, e256. [Google Scholar] [CrossRef]
- Mikacenic, C.; Price, B.L.; Harju-Baker, S.; O’Mahony, D.S.; Robinson-Cohen, C.; Radella, F.; Hahn, W.O.; Katz, R.; Christiani, D.C.; Himmelfarb, J.; et al. A Two-Biomarker Model Predicts Mortality in the Critically Ill with Sepsis. Am. J. Respir. Crit. Care Med. 2017, 196, 1004–1011. [Google Scholar] [CrossRef]
- Barre, M.; Behnes, M.; Hamed, S.; Pauly, D.; Lepiorz, D.; Lang, S.; Akin, I.; Borggrefe, M.; Bertsch, T.; Hoffmann, U. Revisiting the prognostic value of monocyte chemotactic protein 1 and interleukin-6 in the sepsis-3 era. J. Crit. Care 2018, 43, 21–28. [Google Scholar] [CrossRef]
- Yang, C.-H.; Hsiao, J.-L.; Wu, M.-F.; Lu, M.-H.; Chang, H.-M.; Ko, W.-S.; Chiou, Y.-L. The declined levels of inflammatory cytokines related with weaning rate during period of septic patients using ventilators. Clin. Respir. J. 2018, 12, 772–778. [Google Scholar] [CrossRef]
- Yamada, T.; Ishikawa, M.; Yamashita, H.; Fujiwara, M.; Usami, M.; Ueda, T.; Terashima, M.; Kohama, K.; Nakao, A.; Kotani, J. IL18 production and IL18 promoter polymorphisms correlate with mortality in ICU patients. Vivo 2014, 28, 391–396. [Google Scholar]
- Tabah, A.; Buetti, N.; Barbier, F.; Timsit, J.F. Current opinion in management of septic shock due to Gram-negative bacteria. Curr. Opin. Infect. Dis. 2021, 34, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Gao, Q.; Li, Z.; Mo, X.; Wu, Y.; Zhou, H.; Peng, J. Combined procalcitonin and hemogram parameters contribute to early differential diagnosis of Gram-negative/Gram-positive bloodstream infections. J. Clin. Lab. Anal. 2021, 35, e23927. [Google Scholar] [CrossRef] [PubMed]
- Shakoory, B.; Carcillo, J.A.; Chatham, W.W.; Amdur, R.L.; Zhao, H.; Dinarello, C.A.; Cron, R.Q.; Opal, S.M. Interleukin-1 receptor blockade is associated with reduced mortality in sepsis patients with features of macrophage activation syndrome: Reanalysis of a prior phase III trial. Crit. Care Med. 2016, 44, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Dolinay, T.; Kim, Y.S.; Howrylak, J.; Hunninghake, G.M.; An, C.H.; Fredenburgh, L.; Massaro, A.F.; Rogers, A.; Gazourian, L.; Nakahira, K.; et al. Inflammasome-regulated cytokines are critical mediators of acute lung injury. Am. J. Respir. Crit. Care Med. 2012, 185, 1225–1234. [Google Scholar] [CrossRef] [PubMed]
- Rogers, A.J.; Guan, J.; Trtchounian, A.; Hunninghake, G.M.; Kaimal, R.; Desai, M.; Kozikowski, L.A.; DeSouza, L.; Mogan, S.; Liu, K.D.; et al. Association of Elevated Plasma Interleukin-18 Level With Increased Mortality in a Clinical Trial of Statin Treatment for Acute Respiratory Distress Syndrome. Crit. Care Med. 2019, 47, 1089–1096. [Google Scholar] [CrossRef]
- Mierzchala-Pasierb, M.; Krzystek-Korpacka, M.; Lesnik, P.; Adamik, B.; Placzkowska, S.; Serek, P.; Gamian, A.; Lipinska-Gediga, M. Interleukin-18 serum levels in sepsis: Correlation with disease severity and inflammatory markers. Cytokine 2019, 120, 22–27. [Google Scholar] [CrossRef]
- Elsherbiny, N.M.; Al-Gayyar, M.M.H. The role of IL-18 in type 1 diabetic nephropathy: The problem and future treatment. Cytokine 2016, 81, 15–22. [Google Scholar] [CrossRef]
- Ratsimandresy, R.A.; Indramohan, M.; Dorfleutner, A.; Stehlik, C. The AIM2 inflammasome is a central regulator of intestinal homeostasis through the IL-18/IL-22/STAT3 pathway. Cell. Mol. Immunol. 2017, 14, 127–142. [Google Scholar] [CrossRef]
- Wu, Q.; Xiao, Z.; Pu, Y.; Zhou, J.; Wang, D.; Huang, Z.; Hou, D. TnI and IL-18 levels are associated with prognosis of sepsis. Postgrad. Med J. 2019, 95, 240–244. [Google Scholar] [CrossRef]
- Wu, H.; Craft, M.L.; Wang, P.; Wyburn, K.R.; Chen, G.; Ma, J.; Hambly, B.; Chadban, S.J. IL-18 contributes to renal damage after ischemia-reperfusion. J. Am. Soc. Nephrol. JASN 2008, 19, 2331–2341. [Google Scholar] [CrossRef]
- Kim, S.-H.; Eisenstein, M.; Reznikov, L.; Fantuzzi, G.; Novick, D.; Rubinstein, M.; Dinarello, C.A. Structural requirements of six naturally occurring isoforms of the IL-18 binding protein to inhibit IL-18. Proc. Natl. Acad. Sci. USA 2000, 97, 1190–1195. [Google Scholar] [CrossRef]
- Dinarello, C.A.; Novick, D.; Kim, S.; Kaplanski, G. Interleukin-18 and IL-18 binding protein. Front. Immunol. 2013, 4, 289. [Google Scholar] [CrossRef] [PubMed]
- Novick, D.; Schwartsburd, B.; Pinkus, R.; Suissa, D.; Belzer, I.; Sthoeger, Z.; Keane, W.F.; Chvatchko, Y.; Kim, S.H.; Fantuzzi, G.; et al. A novel IL-18BP ELISA shows elevated serum IL-18BP in sepsis and extensive decrease of free IL-18. Cytokine 2001, 14, 334–342. [Google Scholar] [CrossRef]
- de Oliveira, R.P.; Hetzel, M.P.; dos Anjos Silva, M.; Dallegrave, D.; Friedman, G. Mechanical ventilation with high tidal volume induces inflammation in patients without lung disease. Crit. Care 2010, 14, R39. [Google Scholar] [CrossRef] [PubMed]
- Danielski, L.G.; Della Giustina, A.; Bonfante, S.; Barichello, T.; Petronilho, F. The NLRP3 Inflammasome and Its Role in Sepsis Development. Inflammation 2020, 43, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, H.; Zhou, J.; Zhong, Y.; Ali, M.M.; McGuire, F.; Nagarkatti, P.S.; Nagarkatti, M. Role of cytokines as a double-edged sword in sepsis. Vivo 2013, 27, 669–684. [Google Scholar]
- Godinjak, A.; Iglica, A.; Rama, A.; Tančica, I.; Jusufović, S.; Ajanović, A.; Kukuljac, A. Predictive value of saps II and APACHE II scoring systems for patient outcome in medical intensive care unit. Acta Med. Acad. 2016, 45, 89–95. [Google Scholar] [CrossRef]
- Callahan, L.A.; Supinski, G.S. Sepsis-induced myopathy. Crit. Care Med. 2009, 37 (Suppl. 10), S354–S367. [Google Scholar] [CrossRef]
- Rossignol, B.; Gueret, G.; Pennec, J.-P.; Morel, J.; Rannou, F.; Giroux-Metges, M.-A.; Talarmin, H.; Gioux, M.; Arvieux, C.C. Effects of chronic sepsis on contractile properties of fast twitch muscle in an experimental model of critical illness neuromyopathy in the rat. Crit. Care Med. 2008, 36, 1855–1863. [Google Scholar] [CrossRef]
- Hussain, S.N.; Simkus, G.; Roussos, C. Respiratory muscle fatigue: A cause of ventilatory failure in septic shock. J. Appl. Physiol. 1985, 58, 2033–2040. [Google Scholar] [CrossRef] [PubMed]
- Boczkowski, J.; Dureuil, B.; Branger, C.; Pavlovic, D.; Murciano, D.; Pariente, R.; Aubier, M. Effects of sepsis on diaphragmatic function in rats. Am. Rev. Respir. Dis. 1988, 138, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Supinski, G.S.; Callahan, L.A. Caspase activation contributes to endotoxin-induced diaphragm weakness. J. Appl. Physiol. 2006, 100, 1770–1777. [Google Scholar] [CrossRef] [PubMed]
- Demoule, A.; Divangahi, M.; Yahiaoui, L.; Danialou, G.; Gvozdic, D.; Labbe, K.; Bao, W.; Petrof, B.J. Endotoxin triggers nuclear factor-kappaB-dependent up-regulation of multiple proinflammatory genes in the diaphragm. Am. J. Respir. Crit. Care Med. 2006, 174, 646–653. [Google Scholar] [CrossRef]
- Jubran, A.; Tobin, M.J. Pathophysiologic basis of acute respiratory distress in patients who fail a trial of weaning from mechanical ventilation. Am. J. Respir. Crit. Care Med. 1997, 155, 906–915. [Google Scholar] [CrossRef]
- Georgescu, A.M.; Banescu, C.; Azamfirei, R.; Hutanu, A.; Moldovan, V.; Badea, I.; Voidazan, S.; Dobreanu, M.; Chirtes, I.R.; Azamfirei, L. Evaluation of TNF-alpha genetic polymorphisms as predictors for sepsis susceptibility and progression. BMC Infect. Dis. 2020, 20, 221. [Google Scholar] [CrossRef] [PubMed]
- Roderburg, C.; Benz, F.; Schuller, F.; Pombeiro, I.; Hippe, H.-J.; Frey, N.; Trautwein, C.; Luedde, T.; Koch, A.; Tacke, F.; et al. Serum Levels of TNF Receptor Ligands Are Dysregulated in Sepsis and Predict Mortality in Critically Ill Patients. PLoS ONE 2016, 11, e0153765. [Google Scholar] [CrossRef]
- Shindoh, C.; Hida, W.; Ohkawara, Y.; Yamauchi, K.; Ohno, I.; Takishima, T.; Shirato, K. TNF-alpha mRNA expression in diaphragm muscle after endotoxin administration. Am. J. Respir. Crit. Care Med. 1995, 152 (5 Pt 1), 1690–1696. [Google Scholar] [CrossRef]
- Reid, M.B.; Lännergren, J.; Westerblad, H. Respiratory and limb muscle weakness induced by tumor necrosis factor-alpha: Involvement of muscle myofilaments. Am. J. Respir. Crit. Care Med. 2002, 166, 479–484. [Google Scholar] [CrossRef]
| Total (n = 65) | SBT Success (n = 45) | SBT Failure (n = 20) | p Value | |
|---|---|---|---|---|
| Male sex (%) | 36 (55.4%) | 28 (62.2%) | 8 (40%) | 0.113 |
| Age (yrs) (mean ± SD) | 69.8 ± 13.3 | 69.8 ± 12 | 70 ± 16.2 | 0.962 |
| APACHE II score (mean ± SD) | 22.0 ± 7.5 | 21.6 ± 7.7 | 23.1 ± 6.9 | 0.474 |
| Days in ICU until SBT (mean ± SD) | 8.8 ± 6.3 | 8.8 ± 6.3 | 8.7 ± 5.6 | 0.956 |
| Sepsis (%) | 42 (64.6%) | 25 (55.6%) | 17 (85%) | 0.026 |
| WBC (k/mm3) (mean ± SD) | 13,173 ± 5015 | 12,659 ± 4626 | 11,276 ± 3988 | 0.251 |
| CRP (mg/dL) (mean ± SD) | 10.5 ± 3.6 | 10.8 ± 8.8 | 11.7 ± 4.4 | 0.740 |
| Albumin (g/dL) (mean ± SD) | 2.6 ± 0.3 | 2.9 ± 0.4 | 2.7 ± 0.3 | 0.71 |
| PCT (ng/mL) median (interquartile range) | 0.38 (0.18–0.71) | 0.37 (0.17–0.94) | 0.40 (0.16–0.58) | 0.611 |
| VE MV (lt) | 10.5 ± 1.9 | 10.4 ± 2.2 | 9.8 ± 1.2 | 0.373 |
| VE (lt) | 12.2 ± 4.7 | 12.2 ± 5.4 | 12.1 ± 3.2 | 0.982 |
| f/VT (RSBI) | 98.0 ± 60.8 | 80.0 ± 38.9 | 137.8 ± 80.9 | 0.021 |
| MV (PSV) | SBT | p Value * | ||
|---|---|---|---|---|
| RR | SBT failure | 26 ± 5.7 | 32.4 ± 7.7 | 0.001 |
| SBT success | 23.7 ± 5.6 | 24.5 ± 5.4 | 0.2 | |
| HR | SBT failure | 90.2 ± 15.5 | 95.6 ± 14.1 | 0.053 |
| SBT success | 88.2 ± 17.0 | 91.0 ± 15.9 | <0.001 | |
| MAP | SBT failure | 93.0 ± 14.7 | 96.8 ± 21.2 | 0.494 |
| SBT success | 92.5 ± 15.6 | 88.5 ± 13.8 | 0.207 | |
| PaCO2 | SBT failure | 42.8 ± 6.8 | 49.1 ± 13.6 | 0.003 |
| SBT success | 37.4 ± 6.9 | 37.2 ± 7.4 | 0.844 | |
| Arterial pH | SBT failure | 7.46 ± 0.04 | 7.41± 0.07 | 0.003 |
| SBT success | 7.45 ± 0.05 | 7.45 ± 0.04 | 0.774 | |
| PaO2 | SBT failure | 76.5 ± 12.1 | 83.9 ±34.2 | 0.794 |
| SBT success | 84.1 ± 16.0 | 109.2 ± 33.9 | <0.001 | |
| Lactate (mmol/L) | SBT failure | 1.0 ± 0.3 | 0.9 ± 0.3 | 0.010 |
| SBT success | 1.0 ± 0.4 | 1.0 ± 0.4 | 0.261 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kyriakoudi, A.; Rovina, N.; Koltsida, O.; Kostakou, E.; Konstantelou, E.; Kardara, M.; Kompoti, M.; Palamidas, A.; Kaltsakas, G.; Koutsoukou, A. Weaning Failure in Critically Ill Patients Is Related to the Persistence of Sepsis Inflammation. Diagnostics 2022, 12, 92. https://doi.org/10.3390/diagnostics12010092
Kyriakoudi A, Rovina N, Koltsida O, Kostakou E, Konstantelou E, Kardara M, Kompoti M, Palamidas A, Kaltsakas G, Koutsoukou A. Weaning Failure in Critically Ill Patients Is Related to the Persistence of Sepsis Inflammation. Diagnostics. 2022; 12(1):92. https://doi.org/10.3390/diagnostics12010092
Chicago/Turabian StyleKyriakoudi, Anna, Nikoletta Rovina, Ourania Koltsida, Eirini Kostakou, Elissavet Konstantelou, Matina Kardara, Maria Kompoti, Anastasios Palamidas, Georgios Kaltsakas, and Antonia Koutsoukou. 2022. "Weaning Failure in Critically Ill Patients Is Related to the Persistence of Sepsis Inflammation" Diagnostics 12, no. 1: 92. https://doi.org/10.3390/diagnostics12010092
APA StyleKyriakoudi, A., Rovina, N., Koltsida, O., Kostakou, E., Konstantelou, E., Kardara, M., Kompoti, M., Palamidas, A., Kaltsakas, G., & Koutsoukou, A. (2022). Weaning Failure in Critically Ill Patients Is Related to the Persistence of Sepsis Inflammation. Diagnostics, 12(1), 92. https://doi.org/10.3390/diagnostics12010092






