Multiplex Lateral Flow Immunoassay for the Detection of Expanded-Spectrum Hydrolysis and CTX-M Enzymes
Abstract
:1. Introduction
2. Experimental Section
2.1. Monoclonal Antibodies
2.2. Manufactured Test
2.3. Assay Protocol for Test Validation
2.4. Data Acquisition
2.5. Strains Tested
3. Results
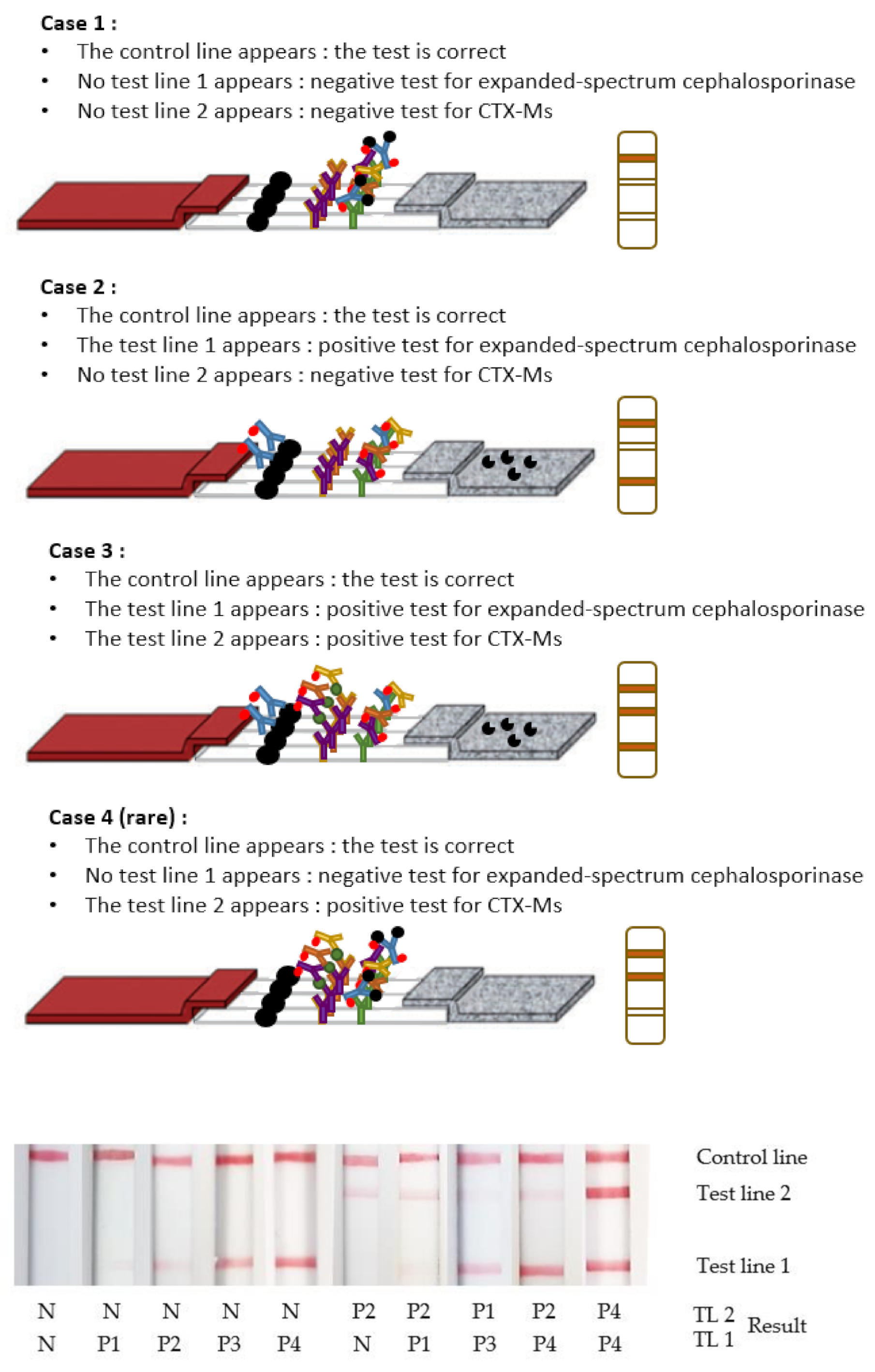
3.1. Test Interpretation
3.2. Test Validation
3.3. Overall Performance
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Neill, J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. Rev. Antimicrob. Resist. 2014, 1–20. [Google Scholar]
- Paterson, D.L. Resistance in Gram-Negative Bacteria: Enterobacteriaceae. Am. J. Infect. Control 2006, 34, S20–S28. [Google Scholar] [CrossRef]
- Bush, K.; Bradford, P.A. β-Lactams and β-Lactamase Inhibitors: An Overview. Cold Spring Harb. Perspect. Med. 2016, 6, a025247. [Google Scholar] [CrossRef]
- Frieden, T. Antibiotic resistance threats in the United States. Cent. Dis. Control Prev. US Dep. Health Hum. Serv. 2013, 23, 11–28. [Google Scholar]
- Bonnet, R. Growing Group of Extended-Spectrum β-Lactamases: The CTX-M Enzymes. Antimicrob. Agents Chemother. 2004, 48, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cantón, R.; González-Alba, J.M.; Galán, J.C. CTX-M Enzymes: Origin and Diffusion. Front. Microbiol. 2012, 3, 110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bevan, E.R.; Jones, A.M.; Hawkey, P.M. Global Epidemiology of CTX-M β-Lactamases: Temporal and Geographical Shifts in Genotype. J. Antimicrob. Chemother. 2017, 72, 2145–2155. [Google Scholar] [CrossRef] [Green Version]
- Cantón, R.; Coque, T.M. The CTX-M Beta-Lactamase Pandemic. Curr. Opin. Microbiol. 2006, 9, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.F.L.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic Resistance—The Need for Global Solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef] [Green Version]
- Hawkey, P.M. Multidrug-Resistant Gram-Negative Bacteria: A Product of Globalization. J. Hosp. Infect. 2015, 89, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Tacconelli, E.; Cataldo, M.A.; Dancer, S.J.; De Angelis, G.; Falcone, M.; Frank, U.; Kahlmeter, G.; Pan, A.; Petrosillo, N.; Rodríguez-Baño, J.; et al. ESCMID Guidelines for the Management of the Infection Control Measures to Reduce Transmission of Multidrug-Resistant Gram-Negative Bacteria in Hospitalized Patients. Clin. Microbiol. Infect. 2014, 20 (Suppl. S1), 1–55. [Google Scholar] [CrossRef] [Green Version]
- Anjum, M.F.; Zankari, E.; Hasman, H. Molecular Methods for Detection of Antimicrobial Resistance. Microbiol. Spectr. 2017, 5, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Drieux, L.; Brossier, F.; Sougakoff, W.; Jarlier, V. Phenotypic Detection of Extended-Spectrum Beta-Lactamase Production in Enterobacteriaceae: Review and Bench Guide. Clin. Microbiol. Infect. 2008, 14 (Suppl. S1), 90–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naas, T.; Oxacelay, C.; Nordmann, P. Identification of CTX-M-Type Extended-Spectrum-Beta-Lactamase Genes Using Real-Time PCR and Pyrosequencing. Antimicrob. Agents Chemother. 2007, 51, 223–230. [Google Scholar] [CrossRef] [Green Version]
- Girlich, D.; Bernabeu, S.; Fortineau, N.; Dortet, L.; Naas, T. Evaluation of the CRE and ESBL ELITe MGB® Kits for the Accurate Detection of Carbapenemase- or CTX-M–Producing Bacteria. Diagn. Microbiol. Infect. Dis. 2018, 92, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Oxacelay, C.; Ergani, A.; Naas, T.; Nordmann, P. Rapid Detection of CTX-M-Producing Enterobacteriaceae in Urine Samples. J. Antimicrob. Chemother. 2009, 64, 986–989. [Google Scholar] [CrossRef] [Green Version]
- Peker, N.; Couto, N.; Sinha, B.; Rossen, J.W. Diagnosis of Bloodstream Infections from Positive Blood Cultures and Directly from Blood Samples: Recent Developments in Molecular Approaches. Clin. Microbiol. Infect. 2018, 24, 944–955. [Google Scholar] [CrossRef] [Green Version]
- Cuzon, G.; Naas, T.; Bogaerts, P.; Glupczynski, Y.; Nordmann, P. Evaluation of a DNA Microarray for the Rapid Detection of Extended-Spectrum β-Lactamases (TEM, SHV and CTX-M), Plasmid-Mediated Cephalosporinases (CMY-2-like, DHA, FOX, ACC-1, ACT/MIR and CMY-1-like/MOX) and Carbapenemases (KPC, OXA-48, VIM, IMP and NDM). J. Antimicrob. Chemother. 2012, 67, 1865–1869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vrioni, G.; Mamali, V.; Zarkotou, O.; Voulgari, E.; Dimitroulia, E.; Themeli-Digalaki, K.; Pournaras, S.; Tsakris, A. Performance of the β LACTATM Test for Rapid Detection of Expanded-Spectrum Cephalosporin-Non-Susceptible Enterobacteriaceae. J. Glob. Antimicrob. Resist. 2017, 10, 285–288. [Google Scholar] [CrossRef]
- Nordmann, P.; Dortet, L.; Poirel, L. Rapid Detection of Extended-Spectrum-β-Lactamase-Producing Enterobacteriaceae. J. Clin. Microbiol. 2012, 50, 3016–3022. [Google Scholar] [CrossRef] [Green Version]
- Sparbier, K.; Schubert, S.; Weller, U.; Boogen, C.; Kostrzewa, M. Matrix-Assisted Laser Desorption Ionization–Time of Flight Mass Spectrometry-Based Functional Assay for Rapid Detection of Resistance against β-Lactam Antibiotics. J. Clin. Microbiol. 2012, 50, 927–937. [Google Scholar] [CrossRef] [Green Version]
- Oviaño, M.; Rodicio, M.R.; Heinisch, J.J.; Rodicio, R.; Bou, G.; Fernández, J. Analysis of the Degradation of Broad-Spectrum Cephalosporins by OXA-48-Producing Enterobacteriaceae Using MALDI-TOF MS. Microorganisms 2019, 7, 614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takeuchi, D.; Akeda, Y.; Sugawara, Y.; Sakamoto, N.; Yamamoto, N.; Shanmugakani, R.K.; Ishihara, T.; Shintani, A.; Tomono, K.; Hamada, S. Establishment of a Dual-Wavelength Spectrophotometric Method for Analysing and Detecting Carbapenemase-Producing Enterobacteriaceae. Sci. Rep. 2018, 8, 15689. [Google Scholar] [CrossRef]
- Bianco, G.; Boattini, M.; Iannaccone, M.; Fossati, L.; Cavallo, R.; Costa, C. Direct β-Lactam Inactivation Method: A New Low-Cost Assay for Rapid Detection of Carbapenemase- or Extended-Spectrum-β-Lactamase-Producing Enterobacterales Directly from Positive Blood Culture Bottles. J. Clin. Microbiol. 2019, 58, e01178-19. [Google Scholar] [CrossRef]
- Shanmugakani, R.K.; Srinivasan, B.; Glesby, M.J.; Westblade, L.F.; Cárdenas, W.B.; Raj, T.; Erickson, D.; Mehta, S. Current State of the Art in Rapid Diagnostics for Antimicrobial Resistance. Lab Chip 2020, 20, 2607–2625. [Google Scholar] [CrossRef]
- Boutal, H.; Vogel, A.; Bernabeu, S.; Devilliers, K.; Creton, E.; Cotellon, G.; Plaisance, M.; Oueslati, S.; Dortet, L.; Jousset, A.; et al. A Multiplex Lateral Flow Immunoassay for the Rapid Identification of NDM-, KPC-, IMP- and VIM-Type and OXA-48-like Carbapenemase-Producing Enterobacteriaceae. J. Antimicrob. Chemother. 2018, 73, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Bernabeu, S.; Ratnam, K.; Boutal, H.; Gonzalez, C.; Vogel, A.; Devilliers, K.; Plaisance, M.; Oueslati, S.; Malhotra-Kumar, S.; Dortet, L.; et al. A Lateral Flow Immunoassay for the Rapid Identification of CTX-M-Producing Enterobacterales from Culture Plates and Positive Blood Cultures. Diagnostics 2020, 10, 764. [Google Scholar] [CrossRef] [PubMed]
- Han, R.; Guo, Y.; Peng, M.; Shi, Q.; Wu, S.; Yang, Y.; Zheng, Y.; Yin, D.; Hu, F. Evaluation of the Immunochromatographic NG-Test Carba 5, RESIST-5 O.O.K.N.V., and IMP K-SeT for Rapid Detection of KPC-, NDM-, IMP-, VIM-Type, and OXA-48-like Carbapenemase Among Enterobacterales. Front. Microbiol. 2021, 11, 3296. [Google Scholar] [CrossRef]
- Moguet, C.; Gonzalez, C.; Sallustrau, A.; Gelhaye, S.; Naas, T.; Simon, S.; Volland, H. Detection of Expanded-Spectrum Cephalosporin Hydrolysis by Lateral Flow Immunoassay. Microb. Biotechnol. 2021, 1–10. [Google Scholar] [CrossRef]
- Thomson, K.S. Extended-Spectrum-β-Lactamase, AmpC, and Carbapenemase Issues. J. Clin. Microbiol. 2010, 48, 1019–1025. [Google Scholar] [CrossRef] [Green Version]
- Naas, T.; Oueslati, S.; Bonnin, R.A.; Dabos, M.L.; Zavala, A.; Dortet, L.; Retailleau, P.; Iorga, B.I. Beta-Lactamase Database (BLDB)—Structure and Function. J. Enzym. Inhib. Med. Chem. 2017, 32, 917–919. [Google Scholar] [CrossRef] [PubMed]
- Lupo, A.; Haenni, M.; Madec, J.-Y. Antimicrobial Resistance in Acinetobacter Spp. and Pseudomonas Spp. Microbiol. Spectr. 2018, 6. [Google Scholar] [CrossRef]
- Jacoby, G.A. AmpC Beta-Lactamases. Clin. Microbiol. Rev. 2009, 22, 161–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naas, T.; Poirel, L.; Nordmann, P. Minor Extended-Spectrum Beta-Lactamases. Clin. Microbiol. Infect. 2008, 14 (Suppl. S1), 42–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nordmann, P.; Gniadkowski, M.; Giske, C.G.; Poirel, L.; Woodford, N.; Miriagou, V. Identification and Screening of Carbapenemase-Producing Enterobacteriaceae. Clin. Microbiol. Infect. 2012, 18, 432–438. [Google Scholar] [CrossRef] [Green Version]
- Oueslati, S.; Retailleau, P.; Marchini, L.; Berthault, C.; Dortet, L.; Bonnin, R.A.; Iorga, B.I.; Naas, T. Role of Arginine 214 in the Substrate Specificity of OXA-48. Antimicrob. Agents Chemother. 2020, 64, e02329-19. [Google Scholar] [CrossRef] [PubMed]
- Docquier, J.-D.; Calderone, V.; De Luca, F.; Benvenuti, M.; Giuliani, F.; Bellucci, L.; Tafi, A.; Nordmann, P.; Botta, M.; Rossolini, G.M.; et al. Crystal Structure of the OXA-48 β-Lactamase Reveals Mechanistic Diversity among Class D Carbapenemases. Chem. Biol. 2009, 16, 540–547. [Google Scholar] [CrossRef]


| Acquired Enzymes | Positive Results (LT1) | Positive Results (LT2) | |
|---|---|---|---|
| Enterobacterales (n = 12) | 0/12 | 1/12 | |
| Escherichia coli (n = 3) | WT (2); CTX-M-93 | 0/3 | 1/3 * |
| Klebsiella pneumonia (n = 1) | WT | 0/1 | 0/1 |
| Citrobacter freundii (n = 1) | WT | 0/1 | 0/1 |
| Enterobacter spp. (n = 3) | IMI-1/2/17 (3) | 0/3 | 0/3 |
| Salmonella spp. (n = 3) | WT (3) | 0/4 | 0/4 |
| Morganella morganii (n = 1) | WT | 0/2 | 0/2 |
| Pseudomonasspp. (n = 4) | WT; Overexpressed efflux pumps (2); OXA-198 | 0/4 | 0/4 |
| Acinetobacter baumannii(n = 1) | OXA-21 | 0/1 | 0/1 |
| Acquired Enzymes | Positive Results (LT1) | Positive Results (LT2) | |
|---|---|---|---|
| Enterobacterales (n = 127) | 127/127 | 83/127 | |
| AmpCs (n = 8) | Overexpressed AmpC (4); DHA-1/2 (2); ACC-1; CMY-136 | 8/8 | 0/8 |
| ESBLs (n = 81) | TEM-3/24 (3); GES-6; SHV-2a/11/12 (3); CTX-M-1/2/3/8/10/14/15/17/18/19/24/27/32/37/55/57/65/71/82/100/101/182 (68); TEM + SHV (2); TEM-52 + CTX-M-15; SHV-2a + CTX-M-15; OXA-48-like (2) | 81/81 | 70/81 |
| Carbapenemases (n = 16) | KPC-2/3 (5); IMP-1/8/14 (3); VIM-2; OXA-48-like (3); NDM-1; TMB-1; GIM-1; FRI-1 | 16/16 | 0/16 |
| AmpCs + ESBLs (n = 1) | Overexpressed AmpC + CTX-M-15 | 1/1 | 1/1 |
| AmpCs + carbapenemases (n = 3) | CMY-13 + VIM-1; CMY-4 + OXA-204; Overexpressed AmpC + SME-1 | 3/3 | 0/3 |
| ESBLs + carbapenemases (n = 16) | SHV-5/12 + IMP-1/8 (3); SHV-5 + VIM-1; SHV-5/11 + OXA-48-like (2); CTX-M-15 + KPC-3; CTX-M-15 + NDM-7/19 (2); TEM-3 + CTX-M-15 + NDM-19; CTX-M-1/9/15 + OXA-48-like (5); SHV-12 + CTX-M-15 + GES-5 | 16/16 | 10/16 |
| AmpCs + ESBLs + carbapenemases (n = 2) | CTX-M-15 + CMY-4 + OXA-48-like; CTX-M-15 + CMY-6 + NDM-4 | 2/2 | 2/2 |
| Pseudomonasspp.(n = 26) | 26/26 | 1/26 | |
| ESBLs (n = 8) | TEM-4; SHV-2a; GES-2/9 (2); PER-1/2 (2); OXA-14; CTX-M-2 | 8/8 | 1/8 |
| Carbapenemases (n = 16) | GES-5; KPC-2; NDM-1; IMP-1/2/13/15/19/26/31/56/63/71 (10); VIM-1/2/4 (3) | 16/16 | 0/16 |
| Broad spectrum penicillinases + AmpCs (n = 2) | Overexpressed AmpC + OXA-13/32 (2) | 2/2 | 0/2 |
| Acinetobacterspp.(n = 18) | 18/18 | 1/18 | |
| AmpCs (n = 1) | Overexpressed AmpC | 1/1 | 0/1 |
| ESBLs (n = 7) | SHV-5 (2); GES-11/12/14 (3); PER-1; CTX-M-15 | 7/7 | 1/7 |
| Carbapenemases (n = 4) | NDM-1/2 (2); IMP-1/4 (2) | 4/4 | 0/4 |
| AmpCs + carbapenemases (n = 6) | Overexpressed AmpC + OXA-23/51/58/97/143/253 (6) | 6/6 | 0/6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moguet, C.; Gonzalez, C.; Naas, T.; Simon, S.; Volland, H. Multiplex Lateral Flow Immunoassay for the Detection of Expanded-Spectrum Hydrolysis and CTX-M Enzymes. Diagnostics 2022, 12, 190. https://doi.org/10.3390/diagnostics12010190
Moguet C, Gonzalez C, Naas T, Simon S, Volland H. Multiplex Lateral Flow Immunoassay for the Detection of Expanded-Spectrum Hydrolysis and CTX-M Enzymes. Diagnostics. 2022; 12(1):190. https://doi.org/10.3390/diagnostics12010190
Chicago/Turabian StyleMoguet, Christian, Camille Gonzalez, Thierry Naas, Stéphanie Simon, and Hervé Volland. 2022. "Multiplex Lateral Flow Immunoassay for the Detection of Expanded-Spectrum Hydrolysis and CTX-M Enzymes" Diagnostics 12, no. 1: 190. https://doi.org/10.3390/diagnostics12010190
APA StyleMoguet, C., Gonzalez, C., Naas, T., Simon, S., & Volland, H. (2022). Multiplex Lateral Flow Immunoassay for the Detection of Expanded-Spectrum Hydrolysis and CTX-M Enzymes. Diagnostics, 12(1), 190. https://doi.org/10.3390/diagnostics12010190







