Validity and Test-Retest Reliability of a Novel Push Low-Cost Hand-Held Dynamometer for Knee Strength Assessment during Different Force Ranges
Abstract
:1. Introduction
2. Materials and Methods
2.1. Equipment
2.2. Procedures
2.2.1. Instrumental Validity
2.2.2. Test–Retest Reliability
2.3. Statistical Analysis
3. Results
3.1. Validity Analysis
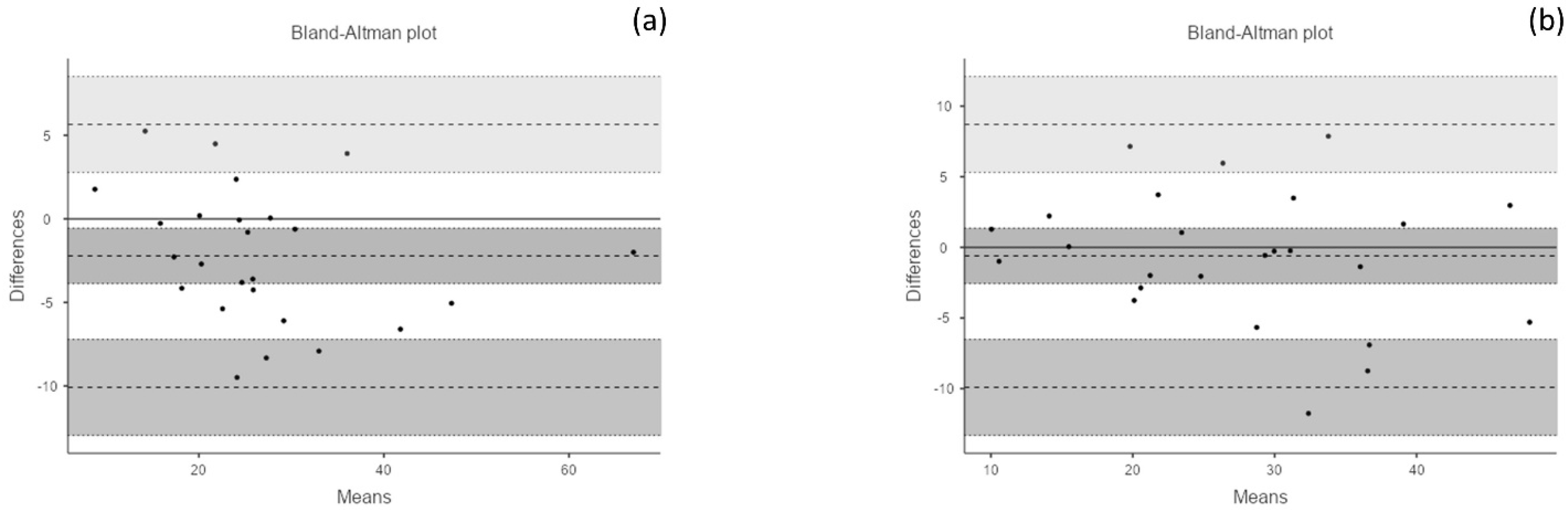
3.2. Reliability Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Manini, T.M.; Clark, B.C. Dynapenia and aging: An update. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2012, 67, 28–40. [Google Scholar] [CrossRef] [Green Version]
- Pijnappels, M.; van der Burg, J.C.E.; Reeves, N.D.; van Dieën, J.H. Identification of elderly fallers by muscle strength measures. Eur. J. Appl. Psychol. 2008, 102, 585–592. [Google Scholar] [CrossRef] [Green Version]
- King, G.W.; Stylianou, A.P.; Kluding, P.; Jernigan, S.D.; Luchies, C.W. Effects of Age and Localized Muscle Fatigue on Ankle Plantar Flexor Torque Development. J. Geriatr. Phys. Ther. 2012, 35, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Lucado, A.; Fraher, L.; Patel, H.; Munck, G. Comparison of portable handheld versus fixed isokinetic dynamometers in measuring strength of the wrist and forearm. Physiother. Theory Pr. 2018, 35, 1–9. [Google Scholar] [CrossRef]
- Malliaropoulos, N.; Mendiguchia, J.; Pehlivanidis, H.; Papadopoulou, S.; Valle, X.; Malliaras, P.; Maffulli, N. Hamstring exercises for track and field athletes: Injury and exercise biomechanics, and possible implications for exercise selection and primary prevention. Br. J. Sports Med. 2012, 46, 846–851. [Google Scholar] [CrossRef]
- Heiderscheit, B.C.; Sherry, M.A.; Silder, A.; Chumanov, E.S.; Thelen, D.G. Hamstring Strain Injuries: Recommendations for Diagnosis, Rehabilitation, and Injury Prevention. J. Orthop. Sports Phys. Ther. 2010, 40, 67–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romero-Franco, N.; Jiménez-Reyes, P.; Montaño-Munuera, J.A. Validity and reliability of a low-cost digital dynamometer for measuring isometric strength of lower limb. J. Sports Sci. 2017, 35, 2179–2184. [Google Scholar] [CrossRef] [PubMed]
- Lum, D.; Haff, G.G.; Barbosa, T.M. The Relationship between Isometric Force-Time Characteristics and Dynamic Performance: A Systematic Review. Sports 2020, 8, 63. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, W.J.; Ratamess, N.A. Fundamentals of Resistance Training: Progression and Exercise Prescription. Med. Sci. Sports Exerc. 2004, 36, 674–688. [Google Scholar] [CrossRef]
- Mcguigan, M.R.; Newton, M.J.; Winchester, J.B.; Nelson, A.G. Relationship Between Isometric and Dynamic Strength in Recreationally Trained Men. J. Strength Cond. Res. 2010, 24, 2570–2573. [Google Scholar] [CrossRef]
- McGuigan, M.; Winchester, J.B. The Relationship Between Isometric and Dynamic Strength in College Football Players. J. Sports Sci. Med. 2008, 7, 101–105. [Google Scholar]
- Diamond, L.E.; Wrigley, T.; Hinman, R.; Hodges, P.; O’Donnell, J.; Takla, A.; Bennell, K. Isometric and isokinetic hip strength and agonist/antagonist ratios in symptomatic femoroacetabular impingement. J. Sci. Med. Sport 2016, 19, 696–701. [Google Scholar] [CrossRef]
- Khayambashi, K.; Ghoddosi, N.; Straub, R.; Powers, C.M. Hip Muscle Strength Predicts Noncontact Anterior Cruciate Ligament Injury in Male and Female Athletes. Am. J. Sports Med. 2016, 44, 355–361. [Google Scholar] [CrossRef]
- Luedke, L.E.; Heiderscheit, B.C.; Williams, D.B.; Rauh, M.J. Association of isometric strength of hip and knee muscles with injury risk in high school cross country runners. Int. J. Sports Phys. Ther. 2015, 10, 868–876. [Google Scholar] [PubMed]
- Gabriner, M.L.; Houston, M.N.; Kirby, J.L.; Hoch, M.C. Contributing factors to Star Excursion Balance Test performance in individuals with chronic ankle instability. Gait Posture 2015, 41, 912–916. [Google Scholar] [CrossRef]
- Peltonen, H.; Walker, S.; Lähitie, A.; Häkkinen, K.; Avela, J. Isometric parameters in the monitoring of maximal strength, power, and hypertrophic resistance-training. Appl. Physiol. Nutr. Metab. 2018, 43, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.L.; Ferreira, I.C.; Ferreira, K.R.; Silveira-Nunes, G.; Barbosa, M.A.; Barbosa, A.C. Validity of an Inexpensive Hanging Scale During Isometric Shoulder Movements. J. Sport Rehabil. 2020, 29, 1218–1221. [Google Scholar] [CrossRef]
- Ferreira, I.C.; Souza, M.A.; Júnior, M.A.; Silveira-Nunes, G.; Barbosa, M.A.; Barbosa, A.C. Validity of a portable hanging scale to assess the isometric muscle strength during knee movement. J. Bodyw. Mov. Ther. 2021, 28, 433–438. [Google Scholar] [CrossRef]
- Romero-Franco, N.; Fernández-Domínguez, J.C.; Montaño-Munuera, J.A.; Romero-Franco, J.; Jiménez-Reyes, P. Validity and reliability of a low-cost dynamometer to assess maximal isometric strength of upper limb. J. Sports Sci. 2019, 37, 1787–1793. [Google Scholar] [CrossRef] [PubMed]
- Toonstra, J.; Mattacola, C.G. Test-retest reliability and validity of isometric knee-flexion and -extension measurement using 3 methods of assessing muscle strength. J. Sport Rehabil. 2013, 22, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Lino, V.T.S.; Rodrigues, N.C.P.; O’Dwyer, G.; Andrade, M.K.D.N.; Mattos, I.E.; Portela, M.C. Handgrip Strength and Factors Associated in Poor Elderly Assisted at a Primary Care Unit in Rio de Janeiro, Brazil. PLoS ONE 2016, 11, e0166373. [Google Scholar] [CrossRef] [Green Version]
- Carty, C.P.; Barrett, R.S.; Cronin, N.J.; Lichtwark, G.A.; Mills, P.M.; Ferrucci, L. Lower Limb Muscle Weakness Predicts Use of a Multiple- Versus Single-Step Strategy to Recover From Forward Loss of Balance in Older Adults. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2012, 67, 1246–1252. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cormack, S.J.; Newton, R.U.; McGuigan, M.R.; Doyle, T.L.A. Reliability of Measures Obtained During Single and Repeated Countermovement Jumps. Int. J. Sports Physiol. Perform. 2008, 3, 131–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Opar, D.A.; Piatkowski, T.; Williams, M.D.; Shield, A.J. A Novel Device Using the Nordic Hamstring Exercise to Assess Eccentric Knee Flexor Strength: A Reliability and Retrospective Injury Study. J. Orthop. Sports Phys. Ther. 2013, 43, 636–640. [Google Scholar] [CrossRef] [Green Version]
- Faulkner, J.A.; Larkin, L.M.; Claflin, D.R.; Brooks, S.V. Age-related changes in the structure and function of skeletal muscles. Clin. Exp. Pharmacol. Physiol. 2007, 34, 1091–1096. [Google Scholar] [CrossRef]


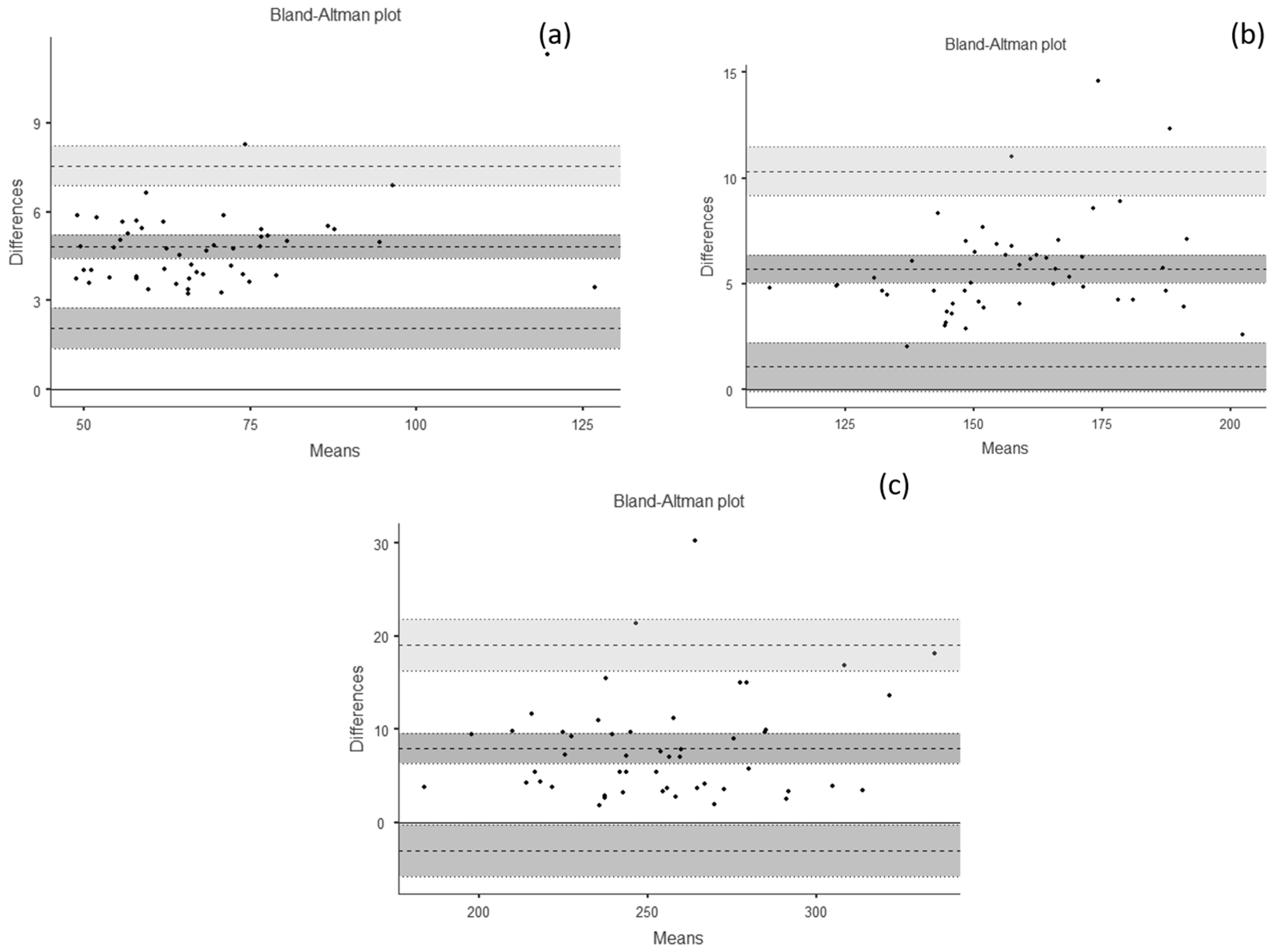
| Outcome | tHHD (in N) | Force Platform (in N) | ICC | Cronbach α | r | r2 | SEM | %SEM | MDC (in N) |
|---|---|---|---|---|---|---|---|---|---|
| Overall | 157.03 ± 79.19 | 163.19 ± 80.67 | 0.999 | 0.999 | 0.999 | 0.998 | 0.14 | 0.09 | 0.38 |
| ~70 N | 65.92 ± 15.97 | 70.73 ± 16.48 | 0.954 | 0.998 | 0.997 | 0.993 | 0.73 | 1.07 | 2.02 |
| ~160 N | 154.36 ± 19.29 | 160.06 ± 19.93 | 0.953 | 0.996 | 0.993 | 0.987 | 0.87 | 0.56 | 2.42 |
| ~250 N | 250.80 ± 31.48 | 258.79 ± 32.56 | 0.955 | 0.992 | 0.985 | 0.970 | 1.20 | 0.47 | 3.32 |
| Outcome | Day 1 (in N) | Day 2 (in N) | ICC | Cronbach α | r | r2 | SEM | %SEM | MDC (in N) |
|---|---|---|---|---|---|---|---|---|---|
| Flexion | 253.03 ± 112.03 | 274.75 ± 122.14 | 0.930 | 0.971 | 0.947 | 0.897 | 0.90 | 3.33 | 2.48 |
| Extension | 266.84 ± 96.39 | 272.76 ± 106.22 | 0.897 | 0.944 | 0.899 | 0.808 | 1.00 | 3.65 | 2.78 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Macedo, M.d.C.; Souza, M.A.; Ferreira, K.R.; Campos, L.O.; Souza, I.S.O.; Barbosa, M.A.; Brito, C.J.; Intelangelo, L.; Barbosa, A.C. Validity and Test-Retest Reliability of a Novel Push Low-Cost Hand-Held Dynamometer for Knee Strength Assessment during Different Force Ranges. Diagnostics 2022, 12, 186. https://doi.org/10.3390/diagnostics12010186
Macedo MdC, Souza MA, Ferreira KR, Campos LO, Souza ISO, Barbosa MA, Brito CJ, Intelangelo L, Barbosa AC. Validity and Test-Retest Reliability of a Novel Push Low-Cost Hand-Held Dynamometer for Knee Strength Assessment during Different Force Ranges. Diagnostics. 2022; 12(1):186. https://doi.org/10.3390/diagnostics12010186
Chicago/Turabian StyleMacedo, Maria de Cássia, Matheus Almeida Souza, Kariny Realino Ferreira, Laura Oliveira Campos, Igor Sérgio Oliveira Souza, Michelle Almeida Barbosa, Ciro José Brito, Leonardo Intelangelo, and Alexandre Carvalho Barbosa. 2022. "Validity and Test-Retest Reliability of a Novel Push Low-Cost Hand-Held Dynamometer for Knee Strength Assessment during Different Force Ranges" Diagnostics 12, no. 1: 186. https://doi.org/10.3390/diagnostics12010186
APA StyleMacedo, M. d. C., Souza, M. A., Ferreira, K. R., Campos, L. O., Souza, I. S. O., Barbosa, M. A., Brito, C. J., Intelangelo, L., & Barbosa, A. C. (2022). Validity and Test-Retest Reliability of a Novel Push Low-Cost Hand-Held Dynamometer for Knee Strength Assessment during Different Force Ranges. Diagnostics, 12(1), 186. https://doi.org/10.3390/diagnostics12010186






