Applied Machine Learning in Spiral Breast-CT: Can We Train a Deep Convolutional Neural Network for Automatic, Standardized and Observer Independent Classification of Breast Density?
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. BCT Examinations
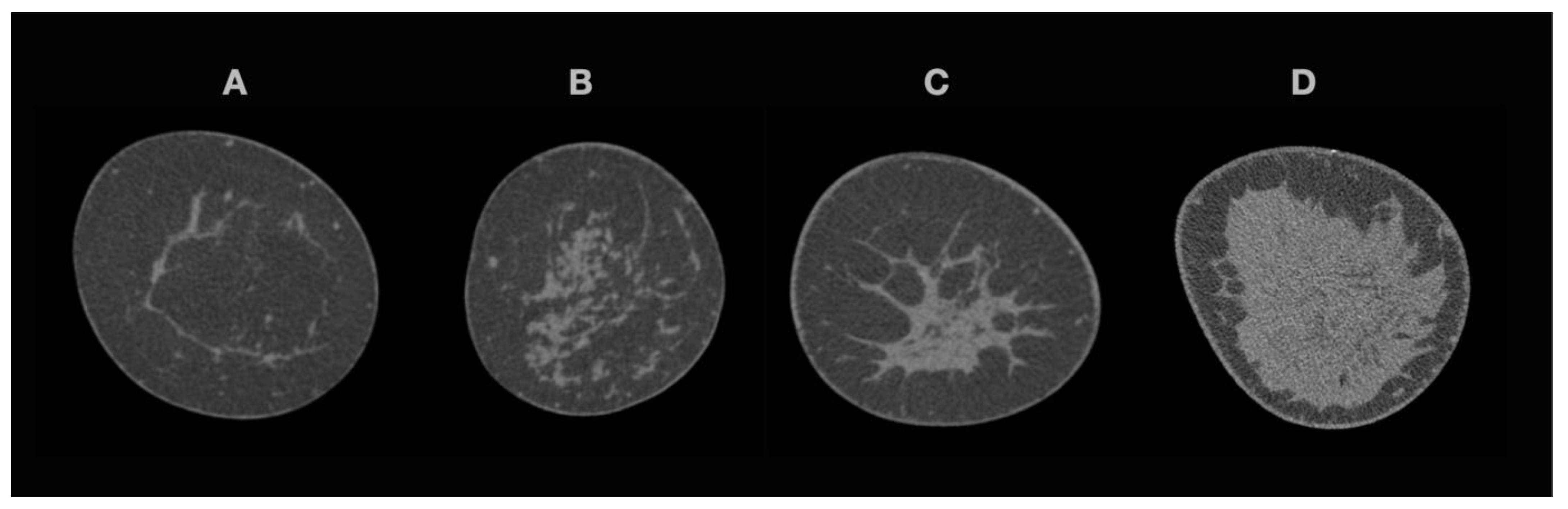
2.3. Breast Density
2.4. Data Preparation
2.5. dCNN Architecture and Training
2.6. Human Readout “Real-World” Subsets
2.7. Statistical Analyses
3. Results
3.1. Patient Selection and Image Processing
3.1.1. Patient Cohort
3.1.2. Accuracies in Training, Validation and “Real-World” Test Datasets
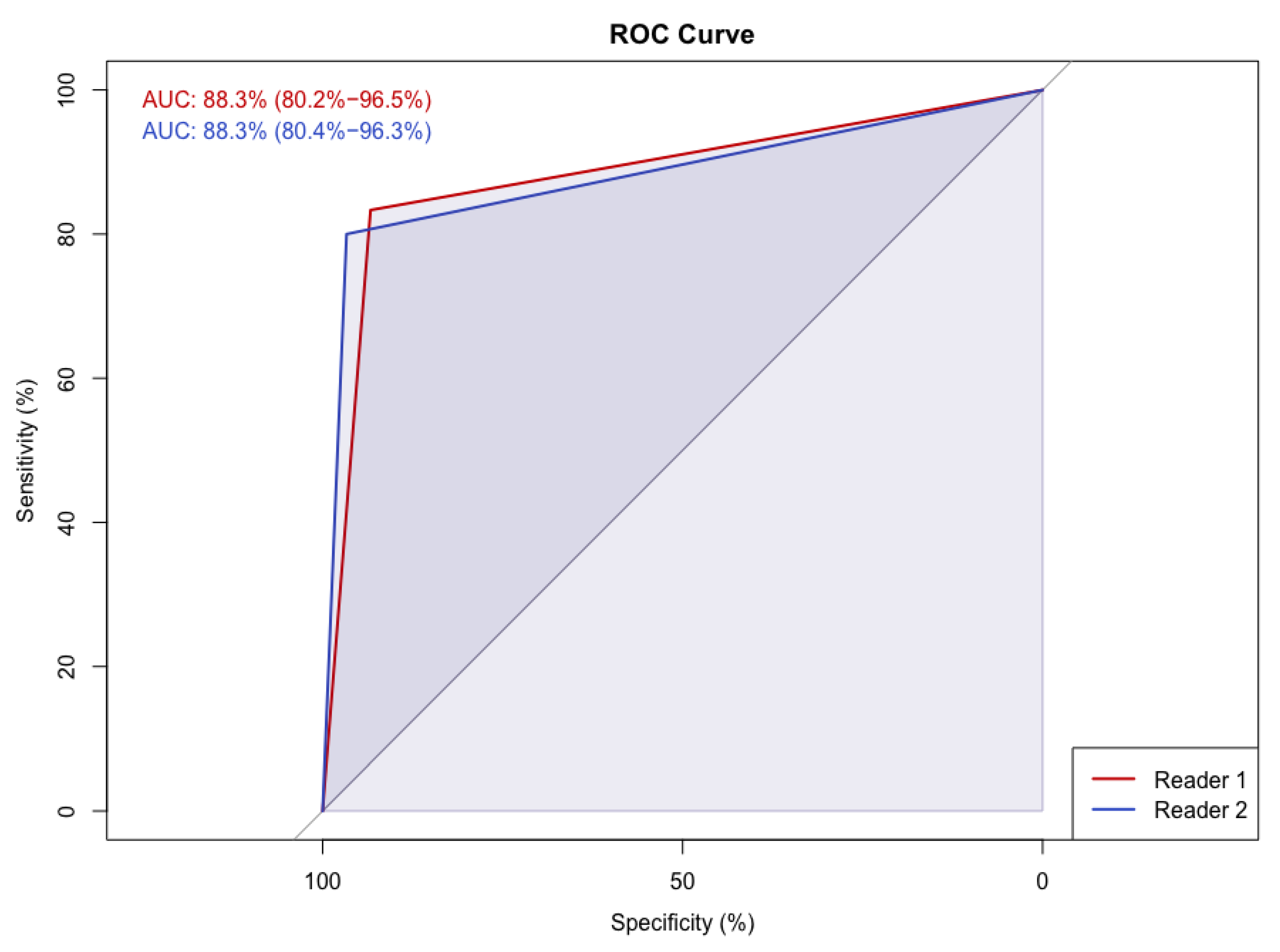
3.1.3. Human Readout
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moreno-Aspitia, A.; Advani, P. Current strategies for the prevention of breast cancer. Breast Cancer Targets Ther. 2014, 6, 59–71. [Google Scholar] [CrossRef][Green Version]
- Plevritis, S.K.; Munoz, D.; Kurian, A.W.; Stout, N.K.; Alagoz, O.; Near, A.M.; Lee, S.J.; Broek, J.J.V.D.; Huang, X.; Schechter, C.B.; et al. Association of Screening and Treatment with Breast Cancer Mortality by Molecular Subtype in US Women, 2000–2012. JAMA J. Am. Med Assoc. 2018, 319, 154–164. [Google Scholar] [CrossRef] [PubMed]
- Boyd, N.F.; Martin, L.J.; Sun, L.; Guo, H.; Chiarelli, A.; Hislop, G.; Yaffe, M.; Minkin, S. Body Size, Mammographic Density, and Breast Cancer Risk. Cancer Epidemiol. Biomark. Prev. 2006, 15, 2086–2092. [Google Scholar] [CrossRef] [PubMed]
- Kamangar, F.; Dores, G.M.; Anderson, W.F. Patterns of Cancer Incidence, Mortality, and Prevalence Across Five Continents: Defining Priorities to Reduce Cancer Disparities in Different Geographic Regions of the World. J. Clin. Oncol. 2006, 24, 2137–2150. [Google Scholar] [CrossRef]
- Lam, P.B.; Vacek, P.M.; Geller, B.M.; Muss, H.B. The association of increased weight, body mass index, and tissue density with the risk of breast carcinoma in Vermont. Cancer 2000, 89, 369–375. [Google Scholar] [CrossRef]
- Burton, A.; Maskarinec, G.; Perez-Gomez, B.; Vachon, C.; Miao, H.; Lajous, M.; López-Ridaura, R.; Rice, M.; Pereira, A.; Garmendia, M.L.; et al. Mammographic density and ageing: A collaborative pooled analysis of cross-sectional data from 22 countries worldwide. PLoS Med. 2017, 14, e1002335. [Google Scholar] [CrossRef] [PubMed]
- Spak, D.; Plaxco, J.; Santiago, L.; Dryden, M.; Dogan, B. BI-RADS ® fifth edition: A summary of changes. Diagn. Interv. Imaging 2017, 98, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Hollingsworth, A.B. Redefining the sensitivity of screening mammography: A review. Am. J. Surg. 2019, 218, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Kolb, T.M.; Lichy, J.; Newhouse, J.H. Comparison of the Performance of Screening Mammography, Physical Examination, and Breast US and Evaluation of Factors that Influence Them: An Analysis of 27,825 Patient Evaluations. Radiology 2002, 225, 165–175. [Google Scholar] [CrossRef]
- Wöckel, A.; Festl, J.; Stüber, T.; Brust, K.; Krockenberger, M.; Heuschmann, P.U.; Jírů-Hillmann, S.; Albert, U.-S.; Budach, W.; Follmann, M.; et al. Interdisciplinary Screening, Diagnosis, Therapy and Follow-up of Breast Cancer. Guideline of the DGGG and the DKG (S3-Level, AWMF Registry Number 032/045OL, December 2017)—Part 2 with Recommendations for the Therapy of Primary, Recurrent and Advanced Breast Cancer. Geburtshilfe Frauenheilkd. 2018, 78, 1056–1088. [Google Scholar] [CrossRef]
- Berger, N.; Marcon, M.; Frauenfelder, T.; Boss, A. Dedicated Spiral Breast Computed Tomography with a Single Photon-Counting Detector. Investig. Radiol. 2020, 55, 68–72. [Google Scholar] [CrossRef]
- Berger, N.; Marcon, M.; Saltybaeva, N.; Kalender, W.A.; Alkadhi, H.; Frauenfelder, T.; Boss, A. Dedicated Breast Computed Tomography with a Photon-Counting Detector: Initial Results of Clinical In Vivo Imaging. Investig. Radiol. 2019, 54, 409–418. [Google Scholar] [CrossRef]
- Wienbeck, S.; Fischer, U.; Luftner-Nagel, S.; Lotz, J.; Uhlig, J. Contrast-enhanced cone-beam breast-CT (CBBCT): Clinical performance compared to mammography and MRI. Eur. Radiol. 2018, 28, 3731–3741. [Google Scholar] [CrossRef]
- Li, H.; Yin, L.; He, N.; Han, P.; Zhu, Y.; Ma, Y.; Liu, A.; Lu, H.; Gao, Z.; Liu, P.; et al. Comparison of comfort between cone beam breast computed tomography and digital mammography. Eur. J. Radiol. 2019, 120, 108674. [Google Scholar] [CrossRef]
- Shim, S.; Saltybaeva, N.; Berger, N.; Marcon, M.; Alkadhi, H.; Boss, A. Lesion Detectability and Radiation Dose in Spiral Breast CT With Photon-Counting Detector Technology. Investig. Radiol. 2020, 55, 515–523. [Google Scholar] [CrossRef]
- Wienbeck, S.; Uhlig, J.; Luftner-Nagel, S.; Zapf, A.; Surov, A.; von Fintel, E.; Stahnke, V.; Lotz, J.; Fischer, U. The role of cone-beam breast-CT for breast cancer detection relative to breast density. Eur. Radiol. 2017, 27, 5185–5195. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Cao, Y.; Liu, A.; Yin, L.; Han, P.; Li, H.; Zhang, X.; Ye, Z. A Reliability Comparison of Cone-Beam Breast Computed Tomography and Mammography: Breast Density Assessment Referring to the Fifth Edition of the BI-RADS Atlas. Acad. Radiol. 2019, 26, 752–759. [Google Scholar] [CrossRef]
- Wieler, J.; Berger, N.; Frauenfelder, T.; Marcon, M.; Boss, A. Breast density in dedicated breast computed tomography. Medicine 2021, 100, e25844. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.; Marcon, M.; Ghafoor, S.; Wurnig, M.C.; Frauenfelder, T.; Boss, A. Deep Learning in Mammography. Investig. Radiol. 2017, 52, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Ciritsis, A.; Rossi, C.; De Martini, I.; Eberhard, M.; Marcon, M.; Becker, A.S.; Berger, N.; Boss, A. Determination of mammographic breast density using a deep convolutional neural network. Br. J. Radiol. 2018, 92, 20180691. [Google Scholar] [CrossRef] [PubMed]
- Ciritsis, A.; Rossi, C.; Eberhard, M.; Marcon, M.; Becker, A.; Boss, A. Automatic classification of ultrasound breast lesions using a deep convolutional neural network mimicking human decision-making. Eur. Radiol. 2019, 29, 5458–5468. [Google Scholar] [CrossRef]
- Saffari, N.; Rashwan, H.; Abdel-Nasser, M.; Singh, V.K.; Arenas, M.; Mangina, E.; Herrera, B.; Puig, D. Fully Automated Breast Density Segmentation and Classification Using Deep Learning. Diagnostics 2020, 10, 988. [Google Scholar] [CrossRef] [PubMed]
- Kundel, H.L.; Polansky, M. Measurement of Observer Agreement. Radiology 2003, 228, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Cohen, J. Weighted kappa: Nominal scale agreement provision for scaled disagreement or partial credit. Psychol. Bull. 1968, 70, 213–220. [Google Scholar] [CrossRef]
- Delong, E.R.; Delong, D.M.; Clarke-Pearson, D.L. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Rutter, D.R.; Calnan, M.; Vaile, M.S.; Field, S.; Wade, K.A. Discomfort and pain during mammography: Description, prediction, and prevention. BMJ 1992, 305, 443–445. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Whelehan, P.; Evans, A.; Wells, M.; MacGillivray, S. The effect of mammography pain on repeat participation in breast cancer screening: A systematic review. Breast 2013, 22, 389–394. [Google Scholar] [CrossRef]
- Stomper, P.C.; D’Souza, D.J.; DiNitto, P.A.; Arredondo, M.A. Analysis of parenchymal density on mammograms in 1353 women 25–79 years old. Am. J. Roentgenol. 1996, 167, 1261–1265. [Google Scholar] [CrossRef] [PubMed]
- Ekpo, E.U.; Ujong, U.P.; Mello-Thoms, C.; McEntee, M.F. Assessment of Interradiologist Agreement Regarding Mammographic Breast Density Classification Using the Fifth Edition of the BI-RADS Atlas. Am. J. Roentgenol. 2016, 206, 1119–1123. [Google Scholar] [CrossRef]
- Winkel, R.R.; Von Euler-Chelpin, M.; Nielsen, M.; Diao, P.; Nielsen, M.B.; Uldall, W.Y.; Vejborg, I. Inter-observer agreement according to three methods of evaluating mammographic density and parenchymal pattern in a case control study: Impact on relative risk of breast cancer. BMC Cancer 2015, 15, 274. [Google Scholar] [CrossRef] [PubMed]
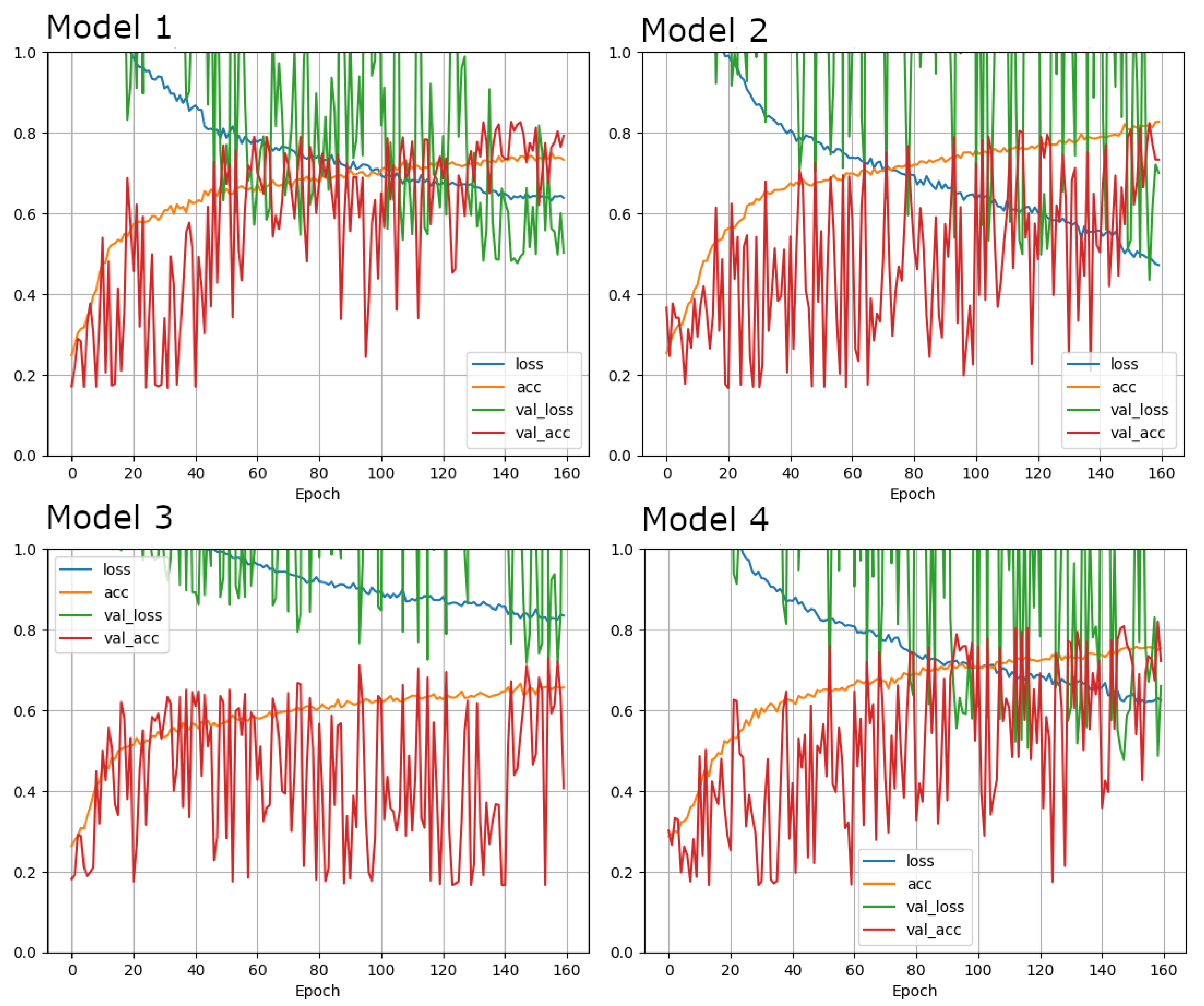

| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| Architecture | brayZNet | brayZNet | brayZNet | brayZNet |
| Learning rate | 1 × 10−5 | 1 × 10−5 | 1 × 10−5 | 1 × 10−5 |
| Loss function | Cross entropy | Cross entropy | Cross entropy | Cross entropy |
| Optimizer | Adam | Adam | SGD | Adam |
| Augmentation | {‘zooming’: 0.1, ‘rotation’: 45.0, ‘horizontal_shift’: 0.1, ‘vertical_shift’: 0.1, ‘brightness’: 0.0} | {‘zooming’: 0.1, ‘rotation’: 45.0, ‘horizontal_shift’: 0.1, ‘vertical_shift’: 0.1, ‘brightness’: 0.0} | {‘zooming’: 0.1, ‘rotation’: 45.0, ‘horizontal_shift’: 0.1, ‘vertical_shift’: 0.1, ‘brightness’: 0.0} | {‘zooming’: 0.1, ‘rotation’: 45.0, ‘horizontal_shift’: 0.1, ‘vertical_shift’: 0.1, ‘brightness’: 0.0} |
| Epochs | 160 | 160 | 160 | 160 |
| Batch size | 8 | 8 | 8 | 8 |
| Dropout | 0.5 | 0.5 | 0.5 | 0.5 |
| Input Shape | [512, 512, 1] | [256, 256, 1] | [512, 512, 1] | [512, 512, 1] |
| Cropping | None | None | None | [0.12826739057573872, 0.8474049572056288, 0.200998651126856, 0.8363919170216573] |
| Dense layers | 2 | 2 | 2 | 2 |
| Units in layer | 128 | 128 | 128 | 128 |
| Regularization | l1 = 1 × 10−6, l2 = 1 × 10−6 | l1 = 1 × 10−6, l2 = 1 × 10−6 | l1 = 1 × 10−6, l2 = 1 × 10−6 | l1 = 1 × 10−6, l2 = 1 × 10−6 |
| Test accuracy | 0.8041666746139526 | 0.8583333492279053 | 0.7354166507720947 | 0.8020833134651184 |
| Density Level | Ultrasound (US) | Reason for US Examination | |||
|---|---|---|---|---|---|
| Yes | No | Density | Other | ||
| A | 58 | 14 | 44 | 0 | 14 |
| B | 118 | 64 | 54 | 28 | 36 |
| C | 83 | 80 | 3 | 57 | 23 |
| D | 58 | 56 | 2 | 43 | 13 |
| Total n | 317 | 214 | 103 | 128 | 86 |
| Predicted Density Level | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | ||||||||||||||
| A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | ||
| Density level (ground truth) | A | 91 | 15 | 0 | 0 | 90 | 15 | 1 | 0 | 93 | 13 | 0 | 0 | 63 | 43 | 0 | 0 |
| B | 19 | 131 | 23 | 0 | 12 | 142 | 19 | 0 | 31 | 129 | 10 | 3 | 4 | 154 | 15 | 0 | |
| C | 0 | 25 | 101 | 2 | 0 | 11 | 112 | 5 | 1 | 38 | 88 | 1 | 0 | 20 | 106 | 2 | |
| D | 0 | 0 | 10 | 63 | 0 | 1 | 4 | 68 | 0 | 1 | 29 | 43 | 0 | 0 | 11 | 62 | |
| dCNN | Reader 1 | Reader 2 | ||
|---|---|---|---|---|
| A | 14 | 15 | 16 | Low density |
| B | 16 | 18 | 19 | |
| C | 15 | 17 | 10 | High density |
| D | 15 | 10 | 15 |
| Ground-Truth | dCNN | Reader 1 | Reader 2 | |
|---|---|---|---|---|
| Ground-Truth | 0.84 | 0.87 | 0.82 | |
| dCNN | 0.71 | 0.73 | ||
| Reader 1 | 0.73 | |||
| Reader 2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landsmann, A.; Wieler, J.; Hejduk, P.; Ciritsis, A.; Borkowski, K.; Rossi, C.; Boss, A. Applied Machine Learning in Spiral Breast-CT: Can We Train a Deep Convolutional Neural Network for Automatic, Standardized and Observer Independent Classification of Breast Density? Diagnostics 2022, 12, 181. https://doi.org/10.3390/diagnostics12010181
Landsmann A, Wieler J, Hejduk P, Ciritsis A, Borkowski K, Rossi C, Boss A. Applied Machine Learning in Spiral Breast-CT: Can We Train a Deep Convolutional Neural Network for Automatic, Standardized and Observer Independent Classification of Breast Density? Diagnostics. 2022; 12(1):181. https://doi.org/10.3390/diagnostics12010181
Chicago/Turabian StyleLandsmann, Anna, Jann Wieler, Patryk Hejduk, Alexander Ciritsis, Karol Borkowski, Cristina Rossi, and Andreas Boss. 2022. "Applied Machine Learning in Spiral Breast-CT: Can We Train a Deep Convolutional Neural Network for Automatic, Standardized and Observer Independent Classification of Breast Density?" Diagnostics 12, no. 1: 181. https://doi.org/10.3390/diagnostics12010181
APA StyleLandsmann, A., Wieler, J., Hejduk, P., Ciritsis, A., Borkowski, K., Rossi, C., & Boss, A. (2022). Applied Machine Learning in Spiral Breast-CT: Can We Train a Deep Convolutional Neural Network for Automatic, Standardized and Observer Independent Classification of Breast Density? Diagnostics, 12(1), 181. https://doi.org/10.3390/diagnostics12010181






