Artificial Intelligence Model to Detect Real Contact Relationship between Mandibular Third Molars and Inferior Alveolar Nerve Based on Panoramic Radiographs
Abstract
:1. Introduction
2. Materials and Methods
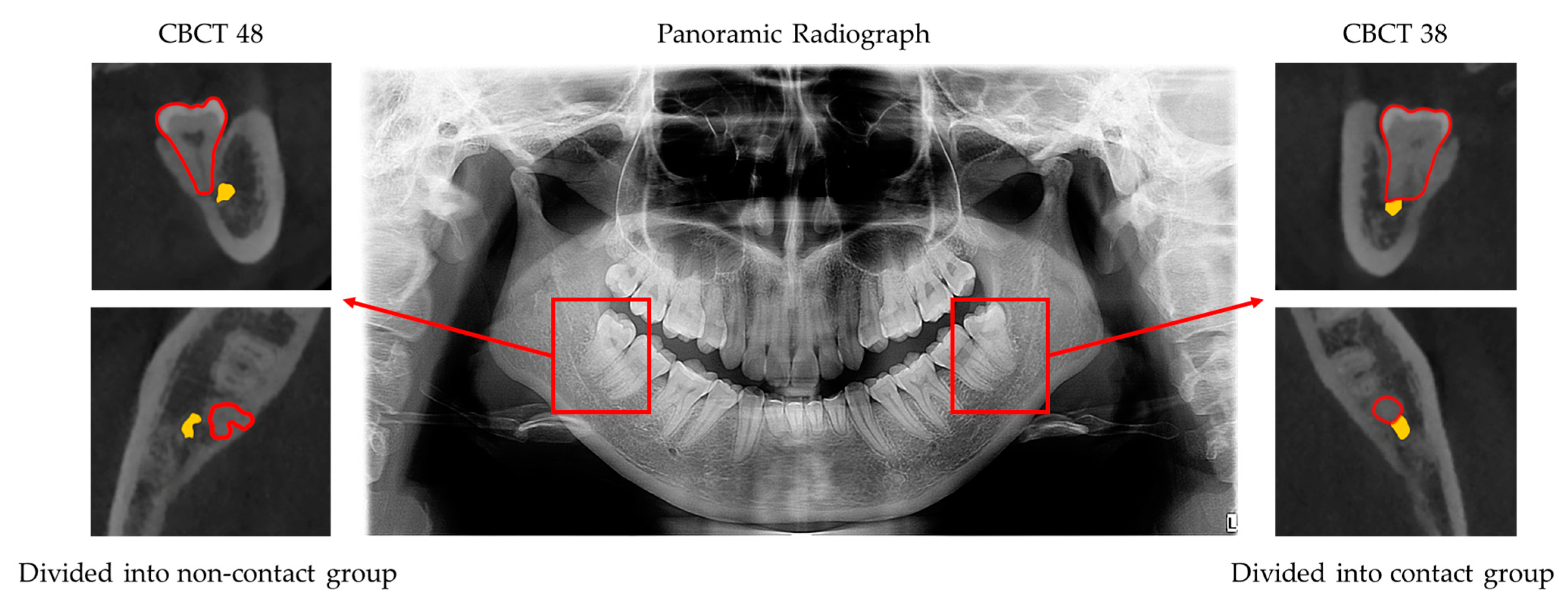
2.1. Image Data Set
2.2. Deep Learning Network Construction and Training
2.3. Diagnostic Performance Analysis
2.4. Statistical Analysis
3. Results
3.1. Deep Learning Network Accuracy
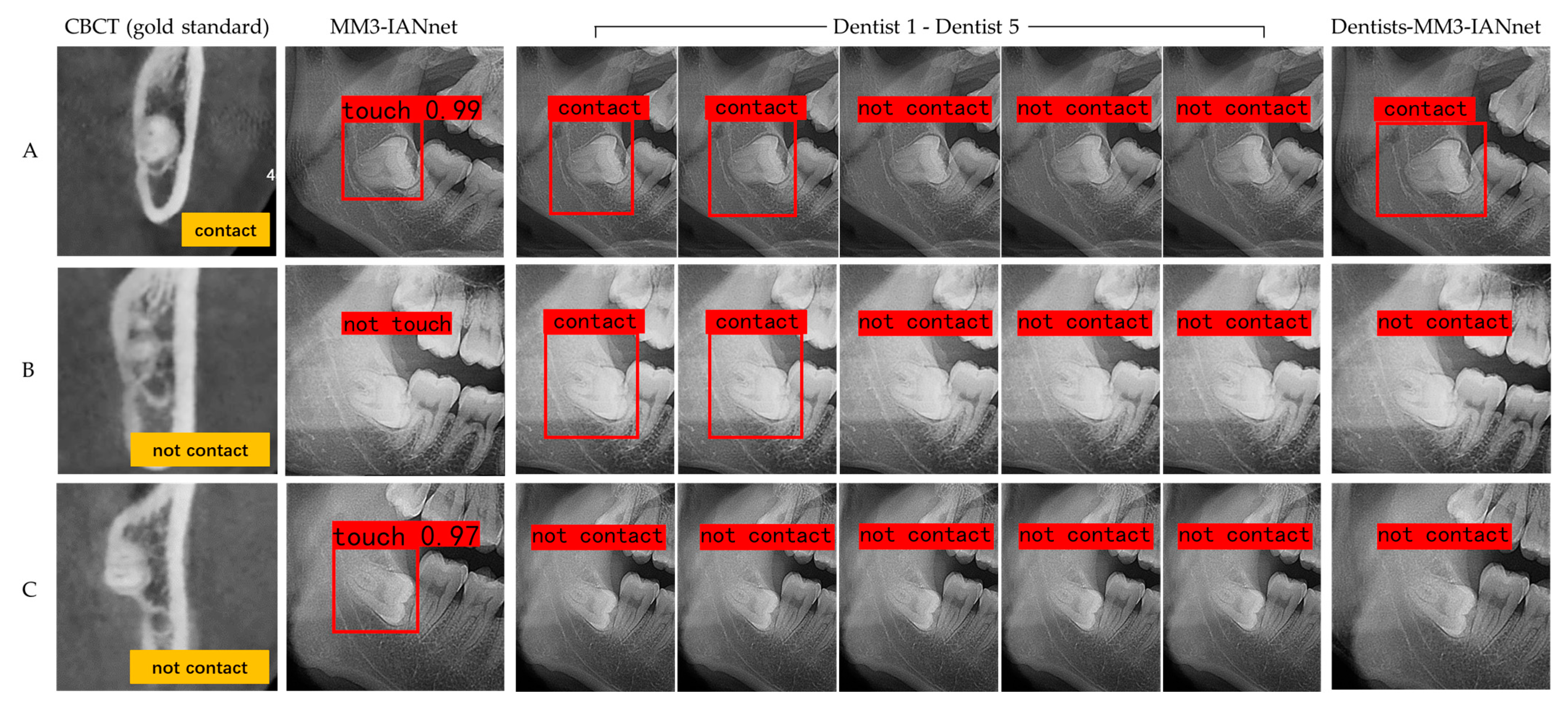
3.2. Diagnostic Performance Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alvira-González, J.; Figueiredo, R.; Valmaseda-Castellón, E.; Quesada-Gómez, C.; Gay-Escoda, C. Predictive factors of difficulty in lower third molar extraction: A prospective cohort study. Med. Oral Patol. Oral Y Cir. Bucal 2017, 22, e108–e114. [Google Scholar] [CrossRef] [Green Version]
- Luo, Q.; Diao, W.; Luo, L.; Zhang, Y. Comparisons of the Computed Tomographic Scan and Panoramic Radiography Before Mandibular Third Molar Extraction Surgery. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2018, 24, 3340–3347. [Google Scholar] [CrossRef]
- Kim, J.W.; Cha, I.H.; Kim, S.J.; Kim, M.R. Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2012, 70, 2508–2514. [Google Scholar] [CrossRef]
- Gu, L.; Zhu, C.; Chen, K.; Liu, X.; Tang, Z. Anatomic study of the position of the mandibular canal and corresponding mandibular third molar on cone-beam computed tomography images. Surg. Radiol. Anat. SRA 2018, 40, 609–614. [Google Scholar] [CrossRef] [Green Version]
- Liu, W.; Yin, W.; Zhang, R.; Li, J.; Zheng, Y. Diagnostic value of panoramic radiography in predicting inferior alveolar nerve injury after mandibular third molar extraction: A meta-analysis. Aust. Dent. J. 2015, 60, 233–239. [Google Scholar] [CrossRef]
- Gomes, A.C.; Vasconcelos, B.C.; Silva, E.D.; Caldas Ade, F., Jr.; Pita Neto, I.C. Sensitivity and specificity of pantomography to predict inferior alveolar nerve damage during extraction of impacted lower third molars. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2008, 66, 256–259. [Google Scholar] [CrossRef]
- Kubota, S.; Imai, T.; Nakazawa, M.; Uzawa, N. Risk stratification against inferior alveolar nerve injury after lower third molar extraction by scoring on cone-beam computed tomography image. Odontology 2020, 108, 124–132. [Google Scholar] [CrossRef]
- Sánchez-Torres, A.; Soler-Capdevila, J.; Ustrell-Barral, M.; Gay-Escoda, C. Patient, radiological, and operative factors associated with surgical difficulty in the extraction of third molars: A systematic review. Int. J. Oral Maxillofac. Surg. 2020, 49, 655–665. [Google Scholar] [CrossRef]
- Barreiro-Torres, J.; Diniz-Freitas, M.; Lago-Méndez, L.; Gude-Sampedro, F.; Gándara-Rey, J.M.; García-García, A. Evaluation of the surgical difficulty in lower third molar extraction. Med. Oral Patol. Oral Y Cir. Bucal 2010, 15, e869–e874. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.; Ra, J.B. Dynamic focal plane estimation for dental panoramic radiography. Med. Phys. 2019, 46, 4907–4917. [Google Scholar] [CrossRef]
- Nardi, C.; Calistri, L.; Grazzini, G.; Desideri, I.; Lorini, C.; Occhipinti, M.; Mungai, F.; Colagrande, S. Is Panoramic Radiography an Accurate Imaging Technique for the Detection of Endodontically Treated Asymptomatic Apical Periodontitis? J. Endod. 2018, 44, 1500–1508. [Google Scholar] [CrossRef]
- Sedaghatfar, M.; August, M.A.; Dodson, T.B. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2005, 63, 3–7. [Google Scholar] [CrossRef]
- Komerik, N.; Muglali, M.; Tas, B.; Selcuk, U. Difficulty of impacted mandibular third molar tooth removal: Predictive ability of senior surgeons and residents. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2014, 72, 1062.e1–1062.e6. [Google Scholar] [CrossRef]
- Selvi, F.; Dodson, T.B.; Nattestad, A.; Robertson, K.; Tolstunov, L. Factors that are associated with injury to the inferior alveolar nerve in high-risk patients after removal of third molars. Br. J. Oral Maxillofac. Surg. 2013, 51, 868–873. [Google Scholar] [CrossRef]
- Matzen, L.H.; Berkhout, E. Cone beam CT imaging of the mandibular third molar: A position paper prepared by the European Academy of DentoMaxilloFacial Radiology (EADMFR). Dento Maxillo Facial Radiol. 2019, 48, 20190039. [Google Scholar] [CrossRef] [PubMed]
- Ghaeminia, H.; Gerlach, N.L.; Hoppenreijs, T.J.; Kicken, M.; Dings, J.P.; Borstlap, W.A.; de Haan, T.; Bergé, S.J.; Meijer, G.J.; Maal, T.J. Clinical relevance of cone beam computed tomography in mandibular third molar removal: A multicentre, randomised, controlled trial. J. Cranio-Maxillo-Facial Surg. Off. Publ. Eur. Assoc. Cranio-Maxillo-Facial Surg. 2015, 43, 2158–2167. [Google Scholar] [CrossRef] [PubMed]
- Estrela, C.; Bueno, M.R.; Leles, C.R.; Azevedo, B.; Azevedo, J.R. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J. Endod. 2008, 34, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Miclotte, A.; Van Hevele, J.; Roels, A.; Elaut, J.; Willems, G.; Politis, C.; Jacobs, R. Position of lower wisdom teeth and their relation to the alveolar nerve in orthodontic patients treated with and without extraction of premolars: A longitudinal study. Clin. Oral Investig. 2014, 18, 1731–1739. [Google Scholar] [CrossRef] [PubMed]
- Su, N.; van Wijk, A.; Berkhout, E.; Sanderink, G.; De Lange, J.; Wang, H.; van der Heijden, G. Predictive Value of Panoramic Radiography for Injury of Inferior Alveolar Nerve After Mandibular Third Molar Surgery. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2017, 75, 663–679. [Google Scholar] [CrossRef]
- Tolstunov, L. The quest for causes of inferior alveolar nerve injury after extraction of mandibular third molars. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2014, 72, 1644–1646. [Google Scholar] [CrossRef]
- Ma, J.; Zhang, Y.; Gu, S.; Zhang, Y.; Zhu, C.; Wang, Q.; Liu, X.; An, X.; Ge, C.; Cao, S.-C.; et al. AbdomenCT-1K: Is Abdominal Organ Segmentation A Solved Problem? IEEE Trans. Pattern Anal. Mach. Intell. 2021. Epub ahead of print. [Google Scholar] [CrossRef]
- Krois, J.; Ekert, T.; Meinhold, L.; Golla, T.; Kharbot, B.; Wittemeier, A.; Dörfer, C.; Schwendicke, F. Deep Learning for the Radiographic Detection of Periodontal Bone Loss. Sci. Rep. 2019, 9, 8495. [Google Scholar] [CrossRef]
- Banar, N.; Bertels, J.; Laurent, F.; Boedi, R.M.; De Tobel, J.; Thevissen, P.; Vandermeulen, D. Towards fully automated third molar development staging in panoramic radiographs. Int. J. Leg. Med. 2020, 134, 1831–1841. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, D.H.; Jeong, S.N.; Choi, S.H. Detection and diagnosis of dental caries using a deep learning-based convolutional neural network algorithm. J. Dent. 2018, 77, 106–111. [Google Scholar] [CrossRef]
- Vinayahalingam, S.; Xi, T.; Bergé, S.; Maal, T.; de Jong, G. Automated detection of third molars and mandibular nerve by deep learning. Sci. Rep. 2019, 9, 9007. [Google Scholar] [CrossRef]
- Tack, A.; Preim, B.; Zachow, S. Fully automated Assessment of Knee Alignment from Full-Leg X-Rays employing “a YOLOv4 And Resnet Landmark regression Algorithm” (YARLA): Data from the Osteoarthritis Initiative. Comput. Methods Programs Biomed. 2021, 205, 106080. [Google Scholar] [CrossRef]
- Kumar, N.S.; Goel, A.K.; Jayanthi, S. A Scrupulous Approach to Perform Classification and Detection of Fetal Brain using Darknet YOLO v4. In Proceedings of the 2021 International Conference on Advance Computing and Innovative Technologies in Engineering (ICACITE), New Delhi, India, 4–5 March 2021; pp. 578–581. [Google Scholar]
- Bochkovskiy, A.; Wang, C.-Y.; Liao, H.J.A. YOLOv4: Optimal Speed and Accuracy of Object Detection. arXiv 2020, arXiv:2004.10934. [Google Scholar]
- Abdurahman, F.; Fante, K.A.; Aliy, M. Malaria parasite detection in thick blood smear microscopic images using modified YOLOV3 and YOLOV4 models. BMC Bioinform. 2021, 22, 112. [Google Scholar] [CrossRef] [PubMed]
- Ghaeminia, H.; Meijer, G.J.; Soehardi, A.; Borstlap, W.A.; Mulder, J.; Bergé, S.J. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int. J. Oral Maxillofac. Surg. 2009, 38, 964–971. [Google Scholar] [CrossRef] [PubMed]

| Categories | Non-Contact Group | Contact Group |
|---|---|---|
| MM3 Number | 530 | 328 |
| Actual Performance | |||
|---|---|---|---|
| 1 | 0 | ||
| Predicted Performance | 1 | True Positive (TP) | False Positive (FP) |
| 0 | False Negative (FN) | True Negative (TN) | |
| Parameter | MM3-IANnet |
|---|---|
| Average precision | 85.05% |
| Precision | 87.18% |
| Recall | 82.93% |
| F1-score | 84.99% |
| Parameter | Dentist 1 | Dentist 2 | Dentist 3 | Dentist 4 | Dentist 5 | Mean ± SD |
|---|---|---|---|---|---|---|
| Average precision | 66.82% | 71.33% | 87.75% | 73.53% | 82.82% | 76.45% ± 8.60% |
| Precision | 95.45% | 90.91% | 97.22% | 82.35% | 83.33% | 89.85% ± 6.81% |
| Recall | 70.00% | 76.92% | 89.74% | 84.00% | 94.34% | 83.00% ± 9.76% |
| F1-score | 80.77% | 83.33% | 93.33% | 83.17% | 88.50% | 85.82% ± 5.06% |
| Parameter | MM3-IANnet | Dentists (Mean) | Dentists-MM3-IANnet |
|---|---|---|---|
| Average precision | 83.02% | 76.45% | 88.06% |
| Precision | 88.71% | 89.85% | 93.88% |
| Recall | 91.67% | 83.00% | 92.00% |
| F1-score | 90.16% | 85.82% | 92.93% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, T.; Chen, D.; Wu, F.; Zhu, F.; Zhu, H. Artificial Intelligence Model to Detect Real Contact Relationship between Mandibular Third Molars and Inferior Alveolar Nerve Based on Panoramic Radiographs. Diagnostics 2021, 11, 1664. https://doi.org/10.3390/diagnostics11091664
Zhu T, Chen D, Wu F, Zhu F, Zhu H. Artificial Intelligence Model to Detect Real Contact Relationship between Mandibular Third Molars and Inferior Alveolar Nerve Based on Panoramic Radiographs. Diagnostics. 2021; 11(9):1664. https://doi.org/10.3390/diagnostics11091664
Chicago/Turabian StyleZhu, Tianer, Daqian Chen, Fuli Wu, Fudong Zhu, and Haihua Zhu. 2021. "Artificial Intelligence Model to Detect Real Contact Relationship between Mandibular Third Molars and Inferior Alveolar Nerve Based on Panoramic Radiographs" Diagnostics 11, no. 9: 1664. https://doi.org/10.3390/diagnostics11091664
APA StyleZhu, T., Chen, D., Wu, F., Zhu, F., & Zhu, H. (2021). Artificial Intelligence Model to Detect Real Contact Relationship between Mandibular Third Molars and Inferior Alveolar Nerve Based on Panoramic Radiographs. Diagnostics, 11(9), 1664. https://doi.org/10.3390/diagnostics11091664






