Shear Wave and Strain Elastography in Crohn’s Disease—A Systematic Review
Abstract
:1. Introduction
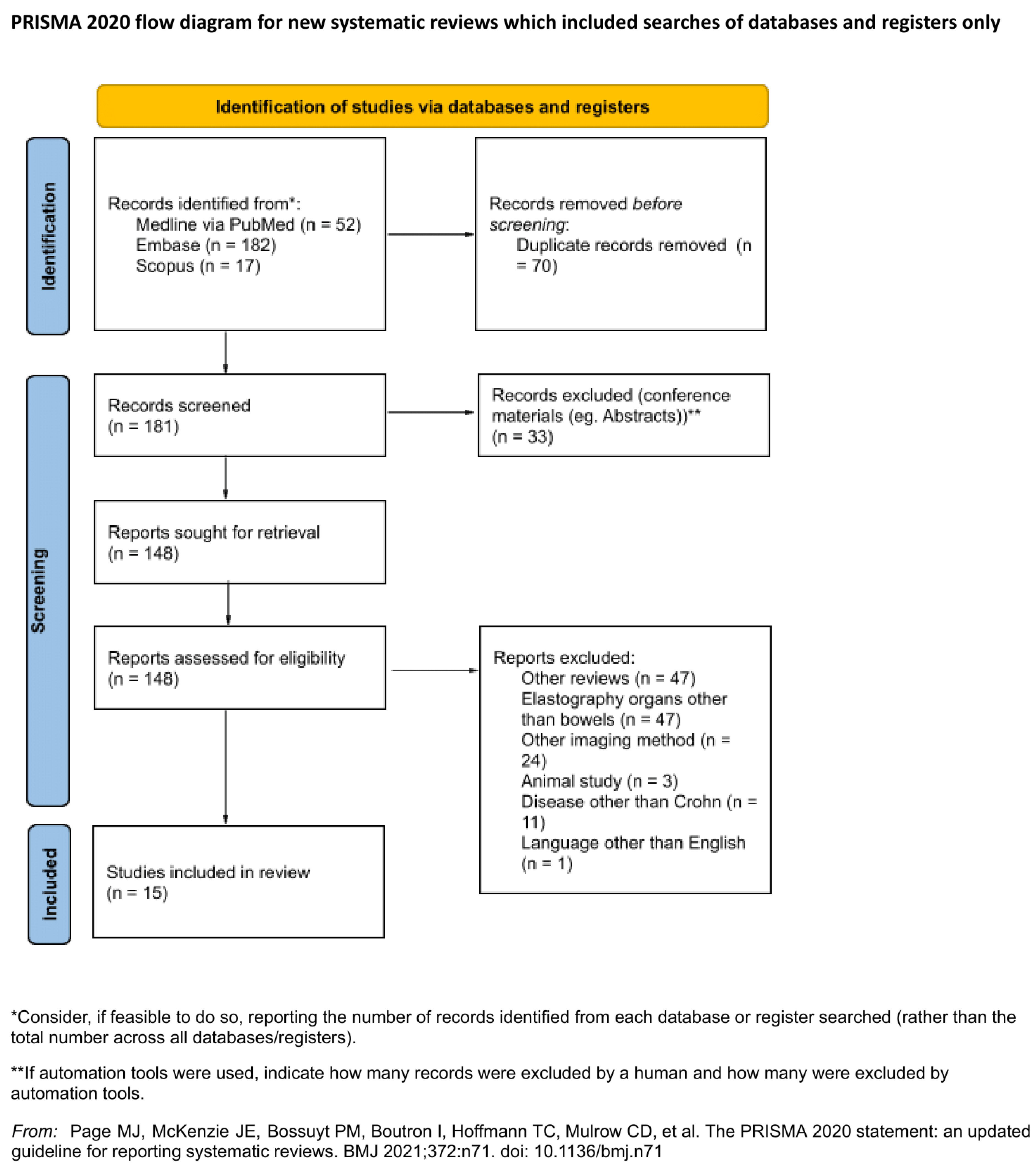
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Data Extraction and Quality Assessment
3. Results
3.1. Conducted Analysis
3.2. Aim of the Studies
3.3. Activity of the Disease, Operations and Additional Circumstances in Which Studies Were Conducted
3.4. Experience and Number of Operators
3.5. Sonoelastography Technique, Region of Interest and Parameters of Sonoelastography
3.6. Results Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baumgart, D.C.; Sandborn, W.J. Crohn’s Disease. Lancet 2012, 380, 1590–1605. [Google Scholar] [CrossRef] [Green Version]
- Ercole, E.; Rigazio, C. Role of Bowel Ultrasound in the Management of Postoperative Crohn’s Disease. World J. Gastrointest. Pathophysiol. 2014, 5, 457–461. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.; Mehandru, S.; Colombel, J.-F.; Peyrin-Biroulet, L. Crohn’s Disease. Lancet 2017, 389, 1741–1755. [Google Scholar] [CrossRef]
- Rieder, F.; Zimmermann, E.M.; Remzi, F.H.; Sandborn, W.J. Crohn’s Disease Complicated by Strictures: A Systematic Review. Gut 2013, 62, 1072–1084. [Google Scholar] [CrossRef] [Green Version]
- Frolkis, A.D.; Dykeman, J.; Negrón, M.E.; Debruyn, J.; Jette, N.; Fiest, K.M.; Frolkis, T.; Barkema, H.W.; Rioux, K.P.; Panaccione, R.; et al. Risk of Surgery for Inflammatory Bowel Diseases Has Decreased over Time: A Systematic Review and Meta-Analysis of Population-Based Studies. Gastroenterology 2013, 145, 996–1006. [Google Scholar] [CrossRef]
- Chan, W.P.W.; Mourad, F.; Leong, R.W. Crohn’s Disease Associated Strictures. J. Gastroenterol. Hepatol. 2018, 33, 998–1008. [Google Scholar] [CrossRef]
- Siegmund, B. Medical Therapy of Fibrostenotic Crohn’s Disease. Visc. Med. 2015, 31, 259–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yaffe, B.H.; Korelitz, B.I. Prognosis for Nonoperative Management of Small-Bowel Obstruction in Crohn’s Disease. J. Clin. Gastroenterol. 1983, 5, 211–215. [Google Scholar] [CrossRef]
- Bouhnik, Y.; Carbonnel, F.; Laharie, D.; Stefanescu, C.; Hébuterne, X.; Abitbol, V.; Nachury, M.; Brixi, H.; Bourreille, A.; Picon, L.; et al. Efficacy of Adalimumab in Patients with Crohn’s Disease and Symptomatic Small Bowel Stricture: A Multicentre, Prospective, Observational Cohort (CREOLE) Study. Gut 2018, 67, 53–60. [Google Scholar] [CrossRef] [Green Version]
- Rieder, F.; Latella, G.; Magro, F.; Yuksel, E.S.; Higgins, P.D.R.; Di Sabatino, A.; de Bruyn, J.R.; Rimola, J.; Brito, J.; Bettenworth, D.; et al. European Crohn’s and Colitis Organisation Topical Review on Prediction, Diagnosis and Management of Fibrostenosing Crohn’s Disease. J. Crohns. Colitis. 2016, 10, 873–885. [Google Scholar] [CrossRef]
- Allocca, M.; Fiorino, G.; Danese, S. Cross-Sectional Imaging Modalities in Crohn’s Disease. Dig. Dis. 2013, 31, 199–201. [Google Scholar] [CrossRef] [PubMed]
- Stidham, R.W.; Cross, R.K. Endoscopy and Cross-Sectional Imaging for Assessing Crohn’s Disease Activity. Tech. Gastrointest. Endosc. 2016, 18, 123–130. [Google Scholar] [CrossRef] [Green Version]
- Chetcuti Zammit, S.; Ellul, P.; Sidhu, R. The Role of Small Bowel Endoscopy for Crohn’s Disease. Curr. Opin. Gastroenterol. 2019, 35, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Bruining, D.H.; Bhatnagar, G.; Rimola, J.; Taylor, S.; Zimmermann, E.M.; Fletcher, J.G. CT and MR Enterography in Crohn’s Disease: Current and Future Applications. Abdom. Imaging 2015, 40, 965–974. [Google Scholar] [CrossRef]
- Puylaert, C.a.J.; Tielbeek, J.a.W.; Bipat, S.; Stoker, J. Grading of Crohn’s Disease Activity Using CT, MRI, US and Scintigraphy: A Meta-Analysis. Eur. Radiol. 2015, 25, 3295–3313. [Google Scholar] [CrossRef] [Green Version]
- Baker, M.E.; Hara, A.K.; Platt, J.F.; Maglinte, D.D.T.; Fletcher, J.G. CT Enterography for Crohn’s Disease: Optimal Technique and Imaging Issues. Abdom. Imaging 2015, 40, 938–952. [Google Scholar] [CrossRef]
- Martínez, M.J.; Ripollés, T.; Paredes, J.M.; Moreno-Osset, E.; Pazos, J.M.; Blanc, E. Intravenous Contrast-Enhanced Ultrasound for Assessing and Grading Postoperative Recurrence of Crohn’s Disease. Dig. Dis. Sci. 2019, 64, 1640–1650. [Google Scholar] [CrossRef]
- Ferraioli, G.; Tinelli, C.; Lissandrin, R.; Zicchetti, M.; Dal Bello, B.; Filice, G.; Filice, C. Point Shear Wave Elastography Method for Assessing Liver Stiffness. World J. Gastroenterol. 2014, 20, 4787–4796. [Google Scholar] [CrossRef] [PubMed]
- Cantisani, V.; Grazhdani, H.; Drakonaki, E.; D’Andrea, V.; Di Segni, M.; Kaleshi, E.; Calliada, F.; Catalano, C.; Redler, A.; Brunese, L.; et al. Strain US Elastography for the Characterization of Thyroid Nodules: Advantages and Limitation. Int. J. Endocrinol. 2015, 2015, 908575. [Google Scholar] [CrossRef] [PubMed]
- Stidham, R.W.; Xu, J.; Johnson, L.A.; Kim, K.; Moons, D.S.; McKenna, B.J.; Rubin, J.M.; Higgins, P.D.R. Ultrasound Elasticity Imaging for Detecting Intestinal Fibrosis and Inflammation in Rats and Humans with Crohn’s Disease. Gastroenterology 2011, 141, 819–826. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, J.M.; Won, J.-K.; Lee, K.-B.; Park, I.A.; Yi, A.; Moon, W.K. Comparison of Shear-Wave and Strain Ultrasound Elastography in the Differentiation of Benign and Malignant Breast Lesions. AJR Am. J. Roentgenol. 2013, 201, W347–W356. [Google Scholar] [CrossRef]
- Dietrich, C.F.; Bamber, J.; Berzigotti, A.; Bota, S.; Cantisani, V.; Castera, L.; Cosgrove, D.; Ferraioli, G.; Friedrich-Rust, M.; Gilja, O.H.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Long Version). Ultraschall Med. 2017, 38, e16–e47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiina, T.; Nightingale, K.R.; Palmeri, M.L.; Hall, T.J.; Bamber, J.C.; Barr, R.G.; Castera, L.; Choi, B.I.; Chou, Y.-H.; Cosgrove, D.; et al. WFUMB Guidelines and Recommendations for Clinical Use of Ultrasound Elastography: Part 1: Basic Principles and Terminology. Ultrasound Med. Biol. 2015, 41, 1126–1147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cosgrove, D.; Piscaglia, F.; Bamber, J.; Bojunga, J.; Correas, J.-M.; Gilja, O.H.; Klauser, A.S.; Sporea, I.; Calliada, F.; Cantisani, V.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography. Part 2: Clinical Applications. Ultraschall Med. 2013, 34, 238–253. [Google Scholar] [CrossRef] [Green Version]
- Săftoiu, A.; Gilja, O.H.; Sidhu, P.S.; Dietrich, C.F.; Cantisani, V.; Amy, D.; Bachmann-Nielsen, M.; Bob, F.; Bojunga, J.; Brock, M.; et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Elastography in Non-Hepatic Applications: Update 2018. Ultraschall Med. 2019, 40, 425–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lichtenstein, G.R.; Loftus, E.V.; Isaacs, K.L.; Regueiro, M.D.; Gerson, L.B.; Sands, B.E. ACG Clinical Guideline: Management of Crohn’s Disease in Adults. Off. J. Am. Coll. Gastroenterol.|ACG 2018, 113, 481–517. [Google Scholar] [CrossRef] [PubMed]
- van Rheenen, P.F.; Aloi, M.; Assa, A.; Bronsky, J.; Escher, J.C.; Fagerberg, U.L.; Gasparetto, M.; Gerasimidis, K.; Griffiths, A.; Henderson, P.; et al. The Medical Management of Paediatric Crohn’s Disease: An ECCO-ESPGHAN Guideline Update. J. Crohns. Colitis. 2020, 161. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater Reliability: The Kappa Statistic. Biochem. Med. (Zagreb.) 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Lu, C.; Gui, X.; Chen, W.; Fung, T.; Novak, K.; Wilson, S.R. Ultrasound Shear Wave Elastography and Contrast Enhancement: Effective Biomarkers in Crohn’s Disease Strictures. Inflamm. Bowel Dis. 2017, 23, 421–430. [Google Scholar] [CrossRef]
- Ding, S.-S.; Fang, Y.; Wan, J.; Zhao, C.-K.; Xiang, L.-H.; Liu, H.; Pu, H.; Xu, G.; Zhang, K.; Xu, X.-R.; et al. Usefulness of Strain Elastography, ARFI Imaging, and Point Shear Wave Elastography for the Assessment of Crohn Disease Strictures. J. Ultrasound Med. 2019, 38, 2861–2870. [Google Scholar] [CrossRef] [PubMed]
- Serra, C.; Rizzello, F.; Pratico’, C.; Felicani, C.; Fiorini, E.; Brugnera, R.; Mazzotta, E.; Giunchi, F.; Fiorentino, M.; D’Errico, A.; et al. Real-Time Elastography for the Detection of Fibrotic and Inflammatory Tissue in Patients with Stricturing Crohn’s Disease. J. Ultrasound 2017, 20, 273–284. [Google Scholar] [CrossRef]
- Quaia, E.; Gennari, A.G.; Cova, M.A.; van Beek, E.J.R. Differentiation of Inflammatory From Fibrotic Ileal Strictures among Patients with Crohn’s Disease Based on Visual Analysis: Feasibility Study Combining Conventional B-Mode Ultrasound, Contrast-Enhanced Ultrasound and Strain Elastography. Ultrasound Med. Biol. 2018, 44, 762–770. [Google Scholar] [CrossRef] [PubMed]
- Lo Re, G.; Picone, D.; Vernuccio, F.; Scopelliti, L.; Di Piazza, A.; Tudisca, C.; Serraino, S.; Privitera, G.; Midiri, F.; Salerno, S.; et al. Comparison of US Strain Elastography and Entero-MRI to Typify the Mesenteric and Bowel Wall Changes during Crohn’s Disease: A Pilot Study. Biomed. Res. Int. 2017, 2017, 4257987. [Google Scholar] [CrossRef] [Green Version]
- Orlando, S.; Fraquelli, M.; Coletta, M.; Branchi, F.; Magarotto, A.; Conti, C.B.; Mazza, S.; Conte, D.; Basilisco, G.; Caprioli, F. Ultrasound Elasticity Imaging Predicts Therapeutic Outcomes of Patients with Crohn’s Disease Treated With Anti-Tumour Necrosis Factor Antibodies. J. Crohn’s Colitis 2018, 12, 63–70. [Google Scholar] [CrossRef]
- Fufezan, O.; Asavoaie, C.; Tamas, A.; Farcau, D.; Serban, D. Bowel Elastography—a Pilot Study for Developing an Elastographic Scoring System to Evaluate Disease Activity in Pediatric Crohn’s Disease. Med. Ultrason. 2015, 17, 422–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fraquelli, M.; Branchi, F.; Cribiù, F.M.; Orlando, S.; Casazza, G.; Magarotto, A.; Massironi, S.; Botti, F.; Contessini-Avesani, E.; Conte, D.; et al. The Role of Ultrasound Elasticity Imaging in Predicting Ileal Fibrosis in Crohn’s Disease Patients. Inflamm. Bowel Dis. 2015, 21, 2605–2612. [Google Scholar] [CrossRef] [Green Version]
- Rustemovic, N.; Cukovic-Cavka, S.; Brinar, M.; Radić, D.; Opacic, M.; Ostojic, R.; Vucelic, B. A Pilot Study of Transrectal Endoscopic Ultrasound Elastography in Inflammatory Bowel Disease. BMC Gastroenterol. 2011, 11, 113. [Google Scholar] [CrossRef] [Green Version]
- Baumgart, D.C.; Müller, H.P.; Grittner, U.; Metzke, D.; Fischer, A.; Guckelberger, O.; Pascher, A.; Sack, I.; Vieth, M.; Rudolph, B. US-Based Real-Time Elastography for the Detection of Fibrotic Gut Tissue in Patients with Stricturing Crohn Disease. Radiology 2015, 275, 889–899. [Google Scholar] [CrossRef]
- Chen, Y.-J.; Mao, R.; Li, X.-H.; Cao, Q.-H.; Chen, Z.-H.; Liu, B.-X.; Chen, S.-L.; Chen, B.-L.; He, Y.; Zeng, Z.-R.; et al. Real-Time Shear Wave Ultrasound Elastography Differentiates Fibrotic from Inflammatory Strictures in Patients with Crohn’s Disease. Inflamm. Bowel Dis. 2018, 24, 2183–2190. [Google Scholar] [CrossRef]
- Havre, R.F.; Leh, S.; Gilja, O.H.; Ødegaard, S.; Waage, J.E.; Baatrup, G.; Nesje, L.B. Strain Assessment in Surgically Resected Inflammatory and Neoplastic Bowel Lesions. Ultraschall Med. 2014, 35, 149–158. [Google Scholar] [CrossRef] [Green Version]
- Sconfienza, L.M.; Cavallaro, F.; Colombi, V.; Pastorelli, L.; Tontini, G.; Pescatori, L.; Esseridou, A.; Savarino, E.; Messina, C.; Casale, R.; et al. In-Vivo Axial-Strain Sonoelastography Helps Distinguish Acutely-Inflamed from Fibrotic Terminal Ileum Strictures in Patients with Crohn’s Disease: Preliminary Results. Ultrasound Med. Biol. 2016, 42, 855–863. [Google Scholar] [CrossRef] [PubMed]
- Goertz, R.S.; Lueke, C.; Wildner, D.; Vitali, F.; Neurath, M.F.; Strobel, D. Acoustic Radiation Force Impulse (ARFI) Elastography of the Bowel Wall as a Possible Marker of Inflammatory Activity in Patients with Crohn’s Disease. Clin. Radiol. 2018, 73, 678.e1–678.e5. [Google Scholar] [CrossRef]
- Thimm, M.A.; Cuffari, C.; Garcia, A.; Sidhu, S.; Hwang, M. Contrast-Enhanced Ultrasound and Shear Wave Elastography Evaluation of Crohn’s Disease Activity in Three Adolescent Patients. Pediatr. Gastroenterol. Hepatol. Nutr. 2019, 22, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Janssen, J.; Schlörer, E.; Greiner, L. EUS Elastography of the Pancreas: Feasibility and Pattern Description of the Normal Pancreas, Chronic Pancreatitis, and Focal Pancreatic Lesions. Gastrointest. Endosc. 2007, 65, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, A.; Grajo, J.R.; Dhyani, M.; Anthony, B.W.; Samir, A.E. Principles of ultrasound elastography. Abdom. Radiol. (NY) 2018, 43, 773–785. [Google Scholar] [CrossRef]
- Aberra, H.; Desalegn, H.; Berhe, N.; Medhin, G.; Stene-Johansen, K.; Gundersen, S.G.; Johannessen, A. Early experiences from one of the first treatment programs for chronic hepatitis B in sub-Saharan Africa. BMC Infect. Dis. 2017, 17, 438. [Google Scholar] [CrossRef]
- Facciorusso, A.; Del Prete, V.; Turco, A.; Buccino, R.V.; Nacchiero, M.C.; Muscatiello, N. Long-term liver stiffness assessment in hepatitis C virus patients undergoing antiviral therapy: Results from a 5-year cohort study. J. Gastroenterol. Hepatol. 2018, 33, 942–949. [Google Scholar] [CrossRef]
- Naidu, J.; Wong, Z.; Palaniappan, S.; Ngiu, C.S.; Yaacob, N.Y.; Hamid, H.A.; Elias, M.H.; Mokhtar, N.M.; Ali, R.A.R. Radiation Exposure in Patients with Inflammatory Bowel Disease: A Fourteen-Year Review at a Tertiary Care Centre in Malaysia. Asian Pac. J. Cancer Prev. 2017, 18, 933–939. [Google Scholar] [CrossRef]
- Bruining, D.H.; Zimmermann, E.M.; Loftus, E.V.; Sandborn, W.J.; Sauer, C.G.; Strong, S.A. Society of Abdominal Radiology Crohn’s Disease-Focused Panel Consensus Recommendations for Evaluation, Interpretation, and Utilization of Computed Tomography and Magnetic Resonance Enterography in Patients with Small Bowel Crohn’s Disease. Radiology 2018, 286, 776–799. [Google Scholar] [CrossRef] [Green Version]
- Reiter, R.; Loch, F.N.; Kamphues, C.; Bayerl, C.; Marticorena Garcia, S.R.; Siegmund, B.; Kühl, A.A.; Hamm, B.; Braun, J.; Sack, I.; et al. Feasibility of Intestinal MR Elastography in Inflammatory Bowel Disease. J. Magn. Reson. Imaging 2021. [Google Scholar] [CrossRef]
- Mazza, S.; Conforti, F.S.; Forzenigo, L.V.; Piazza, N.; Bertè, R.; Costantino, A.; Fraquelli, M.; Coletta, M.; Rimola, J.; Vecchi, M.; et al. Agreement between real-time elastography and delayed enhancement magnetic resonance enterography on quantifying bowel wall fibrosis in Crohn’s disease. Dig. Liver Dis. 2021. [Google Scholar] [CrossRef]
- Coelho, R.; Ribeiro, H.; Maconi, G. Bowel Thickening in Crohn’s Disease: Fibrosis or Inflammation? Diagnostic Ultrasound Imaging Tools. Inflamm. Bowel Dis. 2017, 23, 23–34. [Google Scholar] [CrossRef] [Green Version]
- Dillman, J.R.; Stidham, R.W.; Higgins, P.D.R.; Moons, D.S.; Johnson, L.A.; Rubin, J.M. US Elastography-Derived Shear Wave Velocity Helps Distinguish Acutely Inflamed from Fibrotic Bowel in a Crohn Disease Animal Model. Radiology 2013, 267, 757–766. [Google Scholar] [CrossRef] [Green Version]
- Ishikawa, D.; Ando, T.; Watanabe, O.; Ishiguro, K.; Maeda, O.; Miyake, N.; Nakamura, M.; Miyahara, R.; Ohmiya, N.; Hirooka, Y.; et al. Images of Colonic Real-Time Tissue Sonoelastography Correlate with Those of Colonoscopy and May Predict Response to Therapy in Patients with Ulcerative Colitis. BMC Gastroenterol. 2011, 11, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meng, F.; Zheng, Y.; Zhang, Q.; Mu, X.; Xu, X.; Zhang, H.; Ding, L. Noninvasive Evaluation of Liver Fibrosis Using Real-Time Tissue Elastography and Transient Elastography (FibroScan). J. Ultrasound Med. 2015, 34, 403–410. [Google Scholar] [CrossRef] [PubMed]
- Marin, A.M.; Calapod, O.P.; Moldoveanu, A.C.; Tribus, L.C.; Fierbințeanu-Braticevici, C. Non-invasive Ultrasonographic Score for Assessment of the Severity of Inflammatory Bowel Disease. Ultrasound Med. Biol. 2021, 47, 932–940. [Google Scholar] [CrossRef]
- Skerl, K.; Vinnicombe, S.; Giannotti, E.; Thomson, K.; Evans, A. Influence of Region of Interest Size and Ultrasound Lesion Size on the Performance of 2D Shear Wave Elastography (SWE) in Solid Breast Masses. Clin. Radiol. 2015, 70, 1421–1427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bamber, J.; Cosgrove, D.; Dietrich, C.F.; Fromageau, J.; Bojunga, J.; Calliada, F.; Cantisani, V.; Correas, J.-M.; D’Onofrio, M.; Drakonaki, E.E.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Ultrasound Elastography. Part 1: Basic Principles and Technology. Ultraschall Med. 2013, 34, 169–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moon, J.H.; Hwang, J.-Y.; Park, J.S.; Koh, S.H.; Park, S.-Y. Impact of Region of Interest (ROI) Size on the Diagnostic Performance of Shear Wave Elastography in Differentiating Solid Breast Lesions. Acta Radiol. 2018, 59, 657–663. [Google Scholar] [CrossRef] [Green Version]
- Havre, R.; Gilja, O.H. Elastography and Strain Rate Imaging of the Gastrointestinal Tract. Eur. J. Radiol. 2014, 83, 438–441. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.B.; Gilja, O.H.; Hausken, T.; Gregersen, H.; Matre, K. Strain Measurement during Antral Contractions by Ultrasound Strain Rate Imaging: Influence of Erythromycin. Neurogastroenterol. Motil. 2009, 21, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Giannetti, A.; Biscontri, M.; Matergi, M. Feasibility of Real-Time Strain Elastography in Colonic Diseases. J. Ultrasound 2014, 17, 321–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Authors | Year | Type | Number of Participants | Population | Age (Years), Mean (SD) | Duration of the Disease (Years), Mean (SD) | Aim of the Research | Elastography Technique | Additional Methods | Histopathological Assessment | Device | Operator’s Experience (Years) | Number of Operators |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cathy Lu et al. [24] | 2017 | Prospective | 95 (80 no surgery; 15 surgery) | Adults | Surgery: 41 ± 14.4; no surgery 46.1 ± 13.7 | 12.7 ± 13.9 | To correlate SWE of ileal Crohn’s disease in vivo to CEUS peak enhancement and pathology grades of inflammation, fibrosis and muscular hypertrophy. | SWE | CEUS, US B-Mode | Yes | Acuson S3000 (Siemens Medical Solutions USA, Inc) or Philips Epiq 5 (Philips Healthcare) | 35 (all together) | 4 |
| Ding SS et al. [25] | 2019 | Prospective | 25 (21 inflammatory; 4 fibrotic) | Adults | Inflammatory strictures: 40 ± 14; fibrotic strictures: 35 ± 19 | Inflammatory strictures: 7 ± 6.7; fibrotic strictures: 7.8 ± 5.7 | To evaluate the diagnostic performance of strain elastography, acoustic radiation force impulse (ARFI) imaging and point shear wave elastography (p-SWE) to assess the predominant types of intestinal stenosis in Crohn’s disease. | SE, SWE ARFI, p-SWE | US B-Mode | Yes | S2000 ultrasound scanner (Siemens Medical Solutions, Mountain View, CA) | 10 (ultrasonography), 3 (sonoelastography) | 1 |
| Serra C et al. [26] | 2017 | Prospective | 26 | Adults | 35.5 ± 11.0 | 11.7 ± 7.5 | To measure bowel wall stiffness in stricturing Crohn’s patients using in vivo RTE and to evaluate its role in distinguishing the extent of fibrosis and inflammation assessed by histology. In addition, the relationship between US, colour-Doppler and CEUS, and the histological features of the stenotic bowel wall was assessed. | RT-SE | US B-Mode, CEUS | Yes | iU22 Philips (Philips, Bothell, WA, USA); Philips 5–12 MHz linear transducer | Strong experience | 2 |
| Quaia E et al. [27] | 2018 | Prospective | 20 | Adults | 40.2 ± 10.22 | 6 | To prospectively assess the feasibility of conventional B-mode ultrasound (US) and CEUS combined with real-time SE in the differentiation of inflammatory from fibrotic ileal strictures among patients with CD based on visual analysis. | RT-SE | US B-Mode, CEUS | No | iU22 xMATRIX Ultrasound System (Philips Healthcare, Bothell, WA, USA); broadband 256-element linear-array transducer (L12-5, 5–12 MHz, 50 × 10 mm2) | 10 | 1 |
| Lo Re G et al. [28] | 2017 | Prospective | 35 | Adults | 33.12 | No data | To assess whether SE and DWI could be used to detect mesenteric and bowel wall fibrosis and differentiate it from oedematous/inflammatory changes. | SE | MRE, US B-Mode | No | Samsung RS80A (Samsung Medison Co. Ltd.); linear-array transducer (EUP-L74M, 5–13 MH Samsung) | 15; 5 | 2 |
| Orlando S et al. [29] | 2018 | Prospective | 30 | Adults | 38.8 ± 14.5 | 9.8 ± 7.7 | To investigate whether the severity of intestinal fibrosis, as evaluated by UEI, would predict the therapeutic outcomes of CD patients undergoing treatment with anti-TNF antibodies. The relationship between intestinal fibrosis and anti-TNF-induced transmural healing was also assessed as a secondary outcome. | SE | US B-Mode, Power Doppler | No | Philips iU22 apparatus (Philips Ultrasound; Philips Healthcare, Bothell, WA); multi-frequency convex [C5-2, 5–2 MHz] and a linear array transducer (L12-5, 12–5 MHz) | Strong experience | 1 |
| Fufezan O et al. [30] | 2015 | Prospective | 14 | Paediatric | 12 ± 3.67 | - | The aim of this study is to determine whether SE of the bowel wall, in addition to hydrosonography (HS) of the colon, is a useful tool for assessing and monitoring paediatric patients with CD and to propose an SE scoring system for the assessment of CD activity. | SE | MRE, US B-Mode | Yes | Toshiba Xario V 2.0 ultrasound machine with a linear probe 14–7 MHz | No data | No data |
| Fraqueli M et al. [31] | 2015 | Prospective | 43 (23 surgery; 20 inflammatory) | Adults | Surgery: 40 ± 12; inflammatory 36 ± 13 | Surgery 8 ± 8; inflammatory 8 ± 7 | To assess the correlation between UEI results and bowel wall fibrosis at histology, to verify the feasibility and reproducibility of the technique, and to identify the main determinants of UEI results in patients with ileal CD. The performance of standard bowel US parameters in diagnosing severe ileal fibrosis was assessed as a secondary objective. | SE | US B-Mode | Yes | Philips iU22 apparatus (Philips Ultrasound; Philips Healthcare, Bothell, WA); multifrequency convex (C5-2, 5–2 MHz) and a linear array (L12-5, 12–5 MHz) transducer | No data | 2 |
| Rustemovic N et al. [32] | 2011 | Prospective | 30 | Adults | 30.64 | 5.5 | To assess the role of transrectal ultrasound elastography to distinguish between CD and UC. | Transrectal SE | None | No | Linear echo-endoscope (Pentax FG-38 UX); probes of 7, 5–12 MHz (Hitachi EUB 8500) | No data | 1 |
| Baumgart DC et al. [33] | 2015 | Prospective | 10 | Adults | 49 | 11.6 | The consecutive cohort included consenting adult patients with established Crohn’s disease and symptomatic stenosis that required surgery on the basis of current guidelines and was confirmed by both a gastroenterologist and a surgeon. | RT-SE | US B-Mode, Doppler | Yes | Linear-array transducer (EUP-L74M, 5–13 MHz, 50 × 10 mm2; Hitachi) | 15; 20 | 2 |
| Chen YJ et al. [34] | 2018 | Prospective | 35 | Adults | 34.8 ± 11.3 | 2.7 ± 2.9 | To determine whether shear-wave elastography (SWE), a novel modification of elastography, quantifying tissue stiffness, could differentiate between inflammatory and fibrotic components in strictures of patients with CD. | SWE | US B-Mode | Yes | Aixplorer US system (SuperSonic Imagine S.A., Aix-en-Provence, France); convex broadband probe (SC6-1) and linear array probe (SL 15-4) | 5 | 1 |
| Havre RF et al. [35] | 2014 | Prospective | 27 | Adults | No data | No data | To evaluate whether RTE could distinguish between lesions caused by inflammation and malignant neoplastic lesions using qualitative and semi-quantitative methods for strain assessment. Furthermore, interactions between strain ratio (SR) and changes in the elasticity dynamic range (E-dyn) was assessed. Finally, a correlation analysis of elastography results, a histological semi-quantification of fibrosis, inflammation parameters and tumour description were conducted. | RT-SE | US B-Mode | Yes | Hitachi Hi Vision 900 ultrasound scanner with software version V16–04 STEP 2; L54 M linear probe with frequencies 9–13 MHz (Hitachi Medical Corporation, Tokyo, Japan) | No data | 1 |
| Sconfieza LM et al. [36] | 2015 | Prospective | 16 | Adults | 41 | 10.8 | To ascertain whether RTS could differentiate fibrotic from inflammatory strictures in vivo in patients affected by terminal ileum CD, using MRE as a reference standard. | RTS | US B-Mode, MRE | No | High-resolution linear broadband array transducer (13–6 MHz on MyLab 70 XvG system, Esaote, Genova, Italy) | 10 | 1 |
| Goertz RS et al. [37] | 2018 | Prospective and retrospective group | 98 (77 retrospective group; 21 prospective group) | Adults | Retrospective: 37; prospective: 41 | No data | To evaluate ARFI shear-wave velocities in patients with CD. ARFI measurements of the stomach, the terminal ileum, and the sigmoid were compared and correlated with ultrasonic B-mode findings of bowel wall inflammation and with CD clinical disease activity. | SWE ARFI | US B-Mode | Yes | Acuson S2000 (Siemens Medical Solution, software version VB21A, Erlangen, Germany); the 9 MHz linear transducer | 6 | 1 |
| Thimm MA et al. [38] | 2019 | Series of case studies | 3 | Paediatric | 17.67 | No data | To evaluate disease activity in patients with CD including acute inflammation, chronic inflammation with stricture formation, and a post-surgical fibrotic stricture. Moreover, an interpretation of CEUS kinetic parameters and elastography values in the evaluation of CD activity was performed. | SWE | CEUS, US B-Mode, MRE | No | EPIQ scanner (Philips Healthcare, Bothell, WA, USA); a broadband 162-element curved array transducer (C5-1, 1–5 MHz, and 55.5 mm) | 20 | 1 |
| Authors | Inflammatory Changes | Fibrotic Changes | Stricture/Bowel Wall | Type of Sonoelastography |
|---|---|---|---|---|
| Cathy Lu et al. [24] | +/− | 0 | Stricture | SWE |
| Ding SS et al. [25] | + | + | Stricture | SE, SWE ARFI, p-SWE |
| Serra C et al. [26] | − | − | Stricture | RT-SE |
| Quaia E et al. [27] | + | + | Bowel wall | RT-SE |
| Lo Re G et al. [28] | + | + | Bowel wall | SE |
| Orlando S et al. [29] | + | − | Stricture/bowel wall | SE |
| Fufezan O et al. [30] | + | + | Bowel wall | SE |
| Fraqueli M et al. [31] | + | + | Bowel wall | SE |
| Rustemovic N et al. [32] | + | 0 | Bowel wall | Transrectal SE |
| Baumgart DC et al. [33] | 0 | + | Stricture | RT-SE |
| Chen YJ et al. [34] | − | + | Stricture | SWE |
| Havre RF et al. [35] | − | + | Stricture | RT-SE |
| Sconfieza LM et al. [36] | + | + | Stricture | RTS |
| Goertz RS et al. [37] | +/− | 0 | Bowel wall | SWE ARFI |
| Thimm MA et al. [38] | − | + | Stricture | SWE |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grażyńska, A.; Kufel, J.; Dudek, A.; Cebula, M. Shear Wave and Strain Elastography in Crohn’s Disease—A Systematic Review. Diagnostics 2021, 11, 1609. https://doi.org/10.3390/diagnostics11091609
Grażyńska A, Kufel J, Dudek A, Cebula M. Shear Wave and Strain Elastography in Crohn’s Disease—A Systematic Review. Diagnostics. 2021; 11(9):1609. https://doi.org/10.3390/diagnostics11091609
Chicago/Turabian StyleGrażyńska, Anna, Jakub Kufel, Arkadiusz Dudek, and Maciej Cebula. 2021. "Shear Wave and Strain Elastography in Crohn’s Disease—A Systematic Review" Diagnostics 11, no. 9: 1609. https://doi.org/10.3390/diagnostics11091609
APA StyleGrażyńska, A., Kufel, J., Dudek, A., & Cebula, M. (2021). Shear Wave and Strain Elastography in Crohn’s Disease—A Systematic Review. Diagnostics, 11(9), 1609. https://doi.org/10.3390/diagnostics11091609







