Positive Predictive Value of Panoramic Radiography for Assessment of the Relationship of Impacted Mandibular Third Molars with the Mandibular Canal Based on Cone-Beam Computed Tomography: A Cross-Sectional Study
Abstract
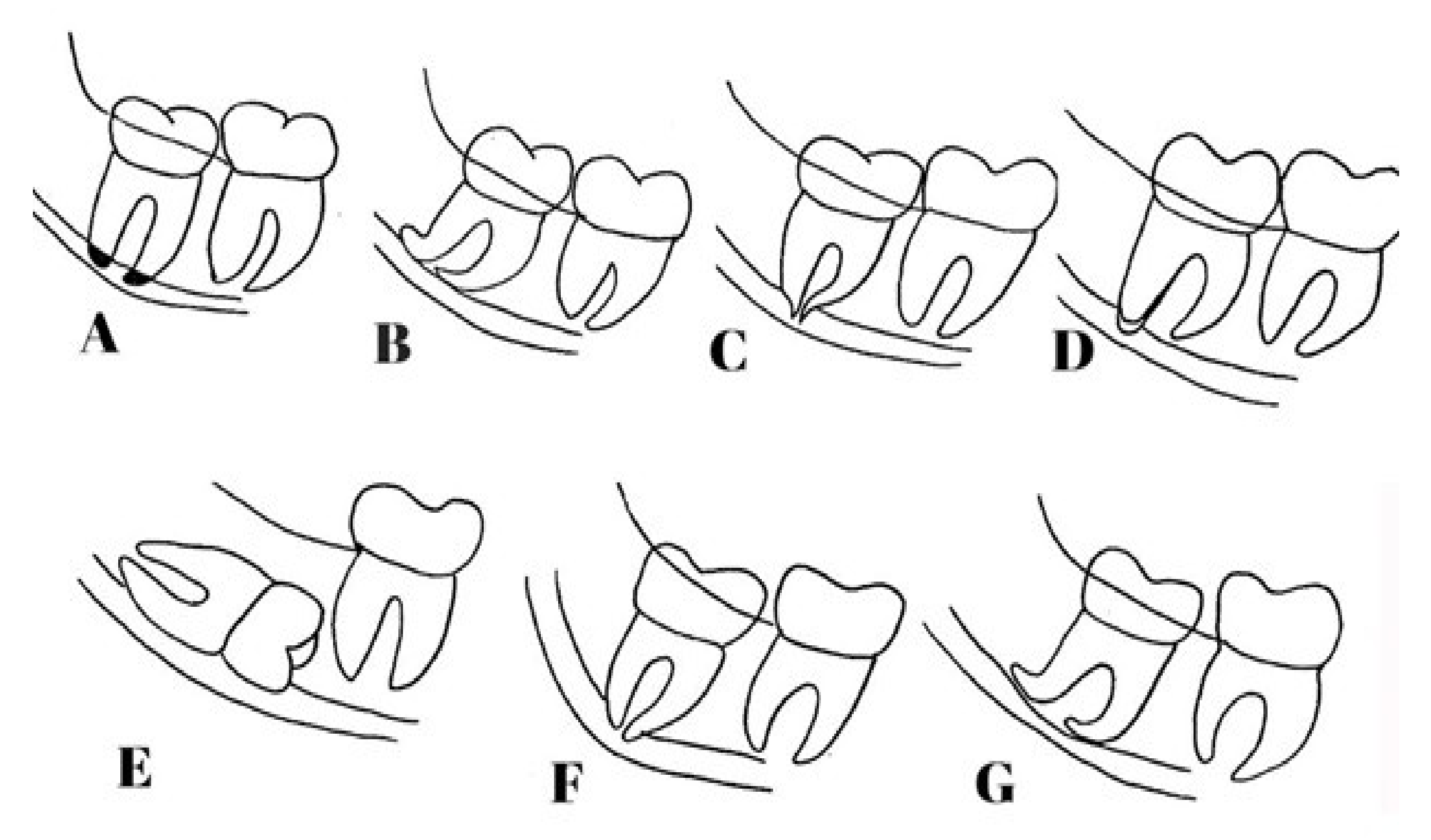
:1. Introduction
2. Methods
2.1. Study Design
2.2. Sample Size
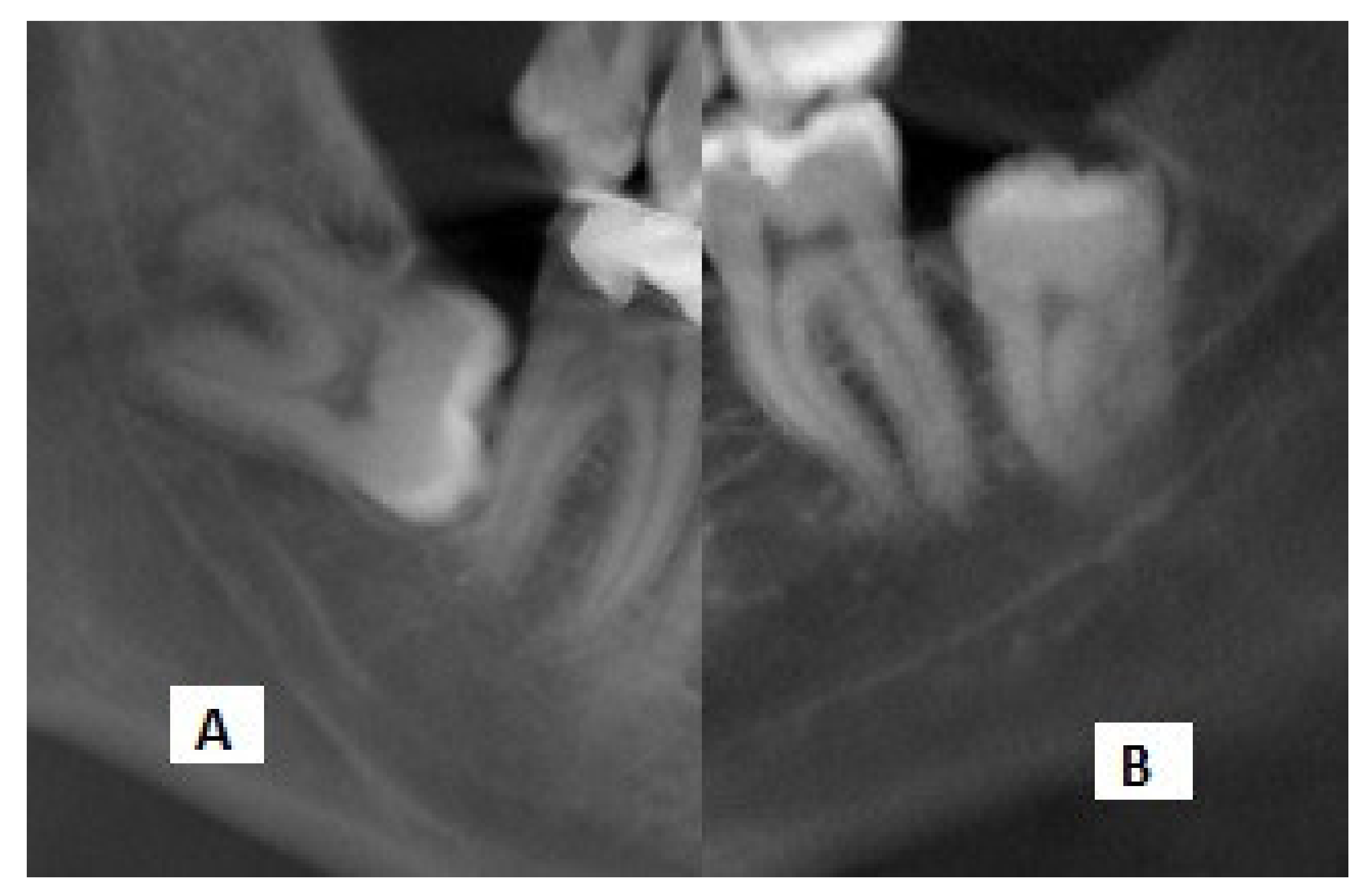
2.3. Evaluation of Images
2.4. Inclusion Criteria
- –
- Samples with IMTMs visible on panoramic radiographs and CBCT scans.
- –
- Radiographs of IMTMs showing root darkening or interference with the white line of the MC as risk factors.
- –
- Absence of developmental and pathological lesions in the mandibular trunk due to possible change in the position of the MC in the area.
- –
- Maturity of the apex of the IMTM root on the panoramic radiograph.
2.5. Exclusion Criteria
2.6. Outcomes
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Maegawa, H.; Sano, K.; Kitagawa, Y.; Ogasawara, T.; Miyauchi, K.; Sekine, J.; Inokuchi, T. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2003, 96, 639–646. [Google Scholar] [CrossRef]
- Miller, C.S.; Nummikoski, P.V.; Barnett, D.A.; Langlais, R.P. Cross-sectional tomography: A diagnostic technique for determining the buccolingual relationship of impacted mandibular third molars and the inferior alveolar neurovascular bundle. Oral Surg. Oral Med. Oral Pathol. 1990, 70, 791–797. [Google Scholar] [CrossRef]
- Haddad, Z.; Khorasani, M.; Bakhshi, M.; Tofangchiha, M.; Shalli, Z. Radiographic Position of Impacted Mandibular Third Molars and Their Association with Pathological Conditions. Int. J. Dent. 2021, 2021, 8841297. [Google Scholar] [CrossRef] [PubMed]
- Benediktsdottir, I.; Hintze, H.; Petersen, J.; Wenzel, A. Accuracy of digital and film panoramic radiographs for assessment of position and morphology of mandibular third molars and prevalence of dental anomalies and pathologies. Dentomaxillofacial Radiol. 2003, 32, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Mallya, S.M.; Lam, E.W.N. White and Pharoah’s Oral Radiology: Principles and Interpretation, 8th ed.; Mosby: Beijing, China, 2019; pp. 151–157. [Google Scholar]
- Holberg, C.; Steinhäuser, S.; Geis, P.; Rudzki-Janson, I. Cone-Beam Computed Tomography in Orthodontics: Benefits and Limitations. J. Orofac. Orthop. Fortschr. Kieferorthopädie 2005, 66, 434–444. [Google Scholar] [CrossRef]
- Cevidanes, L.H.; Bailey, L.J.; Tucker, S.F.; Styner, M.; Mol, A.; Phillips, C.L.; Proffit, W.R.; Turvey, T. Three-dimensional cone-beam computed tomography for assessment of mandibular changes after orthognathic surgery. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Guerrero, M.E.; Jacobs, R.; Loubele, M.; Schutyser, F.; Suetens, P.; Van Steenberghe, D. State-of-the-art on cone beam CT imaging for preoperative planning of implant placement. Clin. Oral Investig. 2006, 10, 1–7. [Google Scholar] [CrossRef]
- Suomalainen, A.; Kiljunen, T.; Käser, Y.; Peltola, J.; Kortesniemi, M. Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillofacial Radiol. 2009, 38, 367–378. [Google Scholar] [CrossRef] [PubMed]
- Miracle, A.; Mukherji, S. Conebeam CT of the Head and Neck, Part 1: Physical Principles. Am. J. Neuroradiol. 2009, 30, 1088–1095. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rood, J.; Shehab, B.N. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br. J. Oral Maxillofac. Surg. 1990, 28, 20–25. [Google Scholar] [CrossRef]
- Tantanapornkul, W.; Mavin, D.; Prapaiphittayakun, J.; Phipatboonyarat, N.; Julphantong, W. Accuracy of Panoramic Radiograph in Assessment of the Relationship Between Mandibular Canal and Impacted Third Molars. Open Dent. J. 2016, 10, 322–329. [Google Scholar] [CrossRef]
- Szalma, J.; Lempel, E.; Jeges, S.; Olasz, L. Darkening of Third Molar Roots: Panoramic Radiographic Associations with Inferior Alveolar Nerve Exposure. J. Oral Maxillofac. Surg. 2011, 69, 1544–1549. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, T.; Ri, S.; Shigeta, T.; Akashi, M.; Imai, Y.; Kakei, Y.; Shibuya, Y.; Komori, T. Risk factors associated with inferior alveolar nerve injury after extraction of the mandibular third molar—A comparative study of preoperative images by panoramic radiography and computed tomography. Int. J. Oral Maxillofac. Surg. 2013, 42, 843–851. [Google Scholar] [CrossRef]
- Wang, D.; Lin, T.; Wang, Y.; Sun, C.; Yang, L.; Jiang, H.; Cheng, J. Radiographic features of anatomic relationship between impacted third molar and inferior alveolar canal on coronal CBCT images: Risk factors for nerve injury after tooth extraction. Arch. Med. Sci. 2018, 14, 532–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clopper, C.J.; Pearson, E.S. The Use of Confidence or Fiducial Limits Illustrated in the Case of the Binomial. Biometrika 1934, 26, 404. [Google Scholar] [CrossRef]
- Nakamori, K.; Tomihara, K.; Noguchi, M. Clinical significance of computed tomography assessment for third molar surgery. World J. Radiol. 2014, 6, 417–423. [Google Scholar] [CrossRef]
- Leung, Y.Y.; Cheung, L.K. Correlation of Radiographic Signs, Inferior Dental Nerve Exposure, and Deficit in Third Molar Surgery. J. Oral Maxillofac. Surg. 2011, 69, 1873–1879. [Google Scholar] [CrossRef]
- Petersen, L.B.; Vaeth, M.; Wenzel, A. Neurosensoric disturbances after surgical removal of the mandibular third molar based on either panoramic imaging or cone beam CT scanning: A randomized controlled trial (RCT). Dentomaxillofacial Radiol. 2016, 45, 20150224. [Google Scholar] [CrossRef]
- Lacerda-Santos, J.T.; Granja, G.L.; Catão, M.H.C.V.; Araújo, F.F.; Freitas, G.B.; Araújo-Filho, J.C.W.P.; Freire, J.C.P.; Dias-Ribeiro, E.; Santos, J.A. Signs of the proximity of third molar roots to the mandibular canal: An observational study in panoramic radiographs. Gen. Dent. 2020, 68, 30–35. [Google Scholar]
- Bell, G. Use of dental panoramic tomographs to predict the relation between mandibular third molar teeth and the inferior alveolar nerve. Br. J. Oral Maxillofac. Surg. 2004, 42, 21–27. [Google Scholar] [CrossRef]
- Elkhateeb, S.M.; Awad, S.S. Accuracy of panoramic radiographic predictor signs in the assessment of proximity of impacted third molars with the mandibular canal. J. Taibah Univ. Med. Sci. 2018, 13, 254–261. [Google Scholar] [CrossRef]
- Tantanapornkul, W.; Okouchi, K.; Fujiwara, Y.; Yamashiro, M.; Maruoka, Y.; Ohbayashi, N.; Kurabayashi, T. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 103, 253–259. [Google Scholar] [CrossRef]
- Yamada, T.; Ishihama, K.; Yasuda, K.; Hasumi-Nakayama, Y.; Ito, K.; Yamaoka, M.; Furusawa, K. Inferior Alveolar Nerve Canal and Branches Detected With Dental Cone Beam Computed Tomography in Lower Third Molar Region. J. Oral Maxillofac. Surg. 2011, 69, 1278–1282. [Google Scholar] [CrossRef] [PubMed]
- Nakamori, K.; Fujiwara, K.; Miyazaki, A.; Tomihara, K.; Tsuji, M.; Nakai, M.; Michifuri, Y.; Suzuki, R.; Komai, K.; Shimanishi, M.; et al. Clinical Assessment of the Relationship Between the Third Molar and the Inferior Alveolar Canal Using Panoramic Images and Computed Tomography. J. Oral Maxillofac. Surg. 2008, 66, 2308–2313. [Google Scholar] [CrossRef]
- Arora, A.; Patil, B.A.; Sodhi, A. Validity of the vertical tube-shift method in determining the relationship between the mandibular third molar roots and the inferior alveolar nerve canal. J. Korean Assoc. Oral Maxillofac. Surg. 2015, 41, 66–73. [Google Scholar] [CrossRef] [Green Version]
- De-Azevedo-Vaz, S.L.; Oenning, A.C.C.; Felizardo, M.G.; Neto, F.H.; De Freitas, D.Q. Accuracy of the vertical tube shift method in identifying the relationship between the third molars and the mandibular canal. Clin. Oral Investig. 2014, 19, 583–588. [Google Scholar] [CrossRef]
- Ghaeminia, H.; Meijer, G.; Soehardi, A.; Borstlap, W.; Mulder, J.; Bergé, S. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int. J. Oral Maxillofac. Surg. 2009, 38, 964–971. [Google Scholar] [CrossRef]
- Albert, D.G.D.M.; Gomes, A.C.A.; Vasconcelos, B.; Silva, E.D.D.O.E.; Holanda, G.Z. Comparison of Orthopantomographs and Conventional Tomography Images for Assessing the Relationship Between Impacted Lower Third Molars and the Mandibular Canal. J. Oral Maxillofac. Surg. 2006, 64, 1030–1037. [Google Scholar] [CrossRef] [PubMed]
- Öhman, A.; Kivijärvi, K.; Blombäck, U.; Flygare, L. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofacial Radiol. 2006, 35, 30–35. [Google Scholar] [CrossRef] [Green Version]
- Monaco, G.; Montevecchi, M.; Bonetti, G.A.; Gatto, M.R.; Checchi, L. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J. Am. Dent. Assoc. 2004, 135, 312–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shujaat, S.; Abouelkheir, H.; Al-Khalifa, K.; Al-Jandan, B.; Marei, H. Pre-operative assessment of relationship between inferior dental nerve canal and mandibular impacted third molar in Saudi population. Saudi Dent. J. 2014, 26, 103–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maloth, K.N.; Kundoor, V.K.R.; Patimeedi, A.; Thakur, M.; Nomula, R.; Sunitha, K. Objectivity and reliability of panoramic radiographic signs and cone-beam computed tomography in the assessment of a superimposed relationship between the impacted mandibular third molars and mandibular nerve: A comparative study. J. Indian Acad. Oral Med. Radiol. 2017, 29, 100. [Google Scholar] [CrossRef]
- Jung, Y.-H.; Nah, K.-S.; Cho, B.-H. Correlation of panoramic radiographs and cone beam computed tomography in the assessment of a superimposed relationship between the mandibular canal and impacted third molars. Imaging Sci. Dent. 2012, 42, 121–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Gender | Presence of Contact Number (%) | Absence of Contact Number (%) | OR (95% CI) | p Value |
|---|---|---|---|---|
| Male | 41 (44.6) | 5 (50) | 0.804 (0.22, 2.97) | 0.74 |
| Female | 51 (55.4) | 5 (50) |
| Radiographic Sign | Presence (%) | Absence (%) | PPV (95% CI) |
|---|---|---|---|
| Root apex darkening | 49 (89.09) | 6 (10.91) | 89.09 (77.75, 95.88) |
| Interference with the white line | 43 (91.48) | 4 (8.52) | 91.48 (79.62, 97.63) |
| Panoramic radiographic signs (total) | 92 (90.19) | 10 (9.81) | 90.19 (82.70, 95.19) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tofangchiha, M.; Koushaei, S.; Mortazavi, M.; Souri, Z.; Alizadeh, A.; Patini, R. Positive Predictive Value of Panoramic Radiography for Assessment of the Relationship of Impacted Mandibular Third Molars with the Mandibular Canal Based on Cone-Beam Computed Tomography: A Cross-Sectional Study. Diagnostics 2021, 11, 1578. https://doi.org/10.3390/diagnostics11091578
Tofangchiha M, Koushaei S, Mortazavi M, Souri Z, Alizadeh A, Patini R. Positive Predictive Value of Panoramic Radiography for Assessment of the Relationship of Impacted Mandibular Third Molars with the Mandibular Canal Based on Cone-Beam Computed Tomography: A Cross-Sectional Study. Diagnostics. 2021; 11(9):1578. https://doi.org/10.3390/diagnostics11091578
Chicago/Turabian StyleTofangchiha, Maryam, Soheil Koushaei, Maryam Mortazavi, Zahra Souri, Ahad Alizadeh, and Romeo Patini. 2021. "Positive Predictive Value of Panoramic Radiography for Assessment of the Relationship of Impacted Mandibular Third Molars with the Mandibular Canal Based on Cone-Beam Computed Tomography: A Cross-Sectional Study" Diagnostics 11, no. 9: 1578. https://doi.org/10.3390/diagnostics11091578
APA StyleTofangchiha, M., Koushaei, S., Mortazavi, M., Souri, Z., Alizadeh, A., & Patini, R. (2021). Positive Predictive Value of Panoramic Radiography for Assessment of the Relationship of Impacted Mandibular Third Molars with the Mandibular Canal Based on Cone-Beam Computed Tomography: A Cross-Sectional Study. Diagnostics, 11(9), 1578. https://doi.org/10.3390/diagnostics11091578







