Applications of Advanced Ultrasound Technology in Obstetrics
Abstract
:1. Introduction
2. High-Resolution Ultrasonography
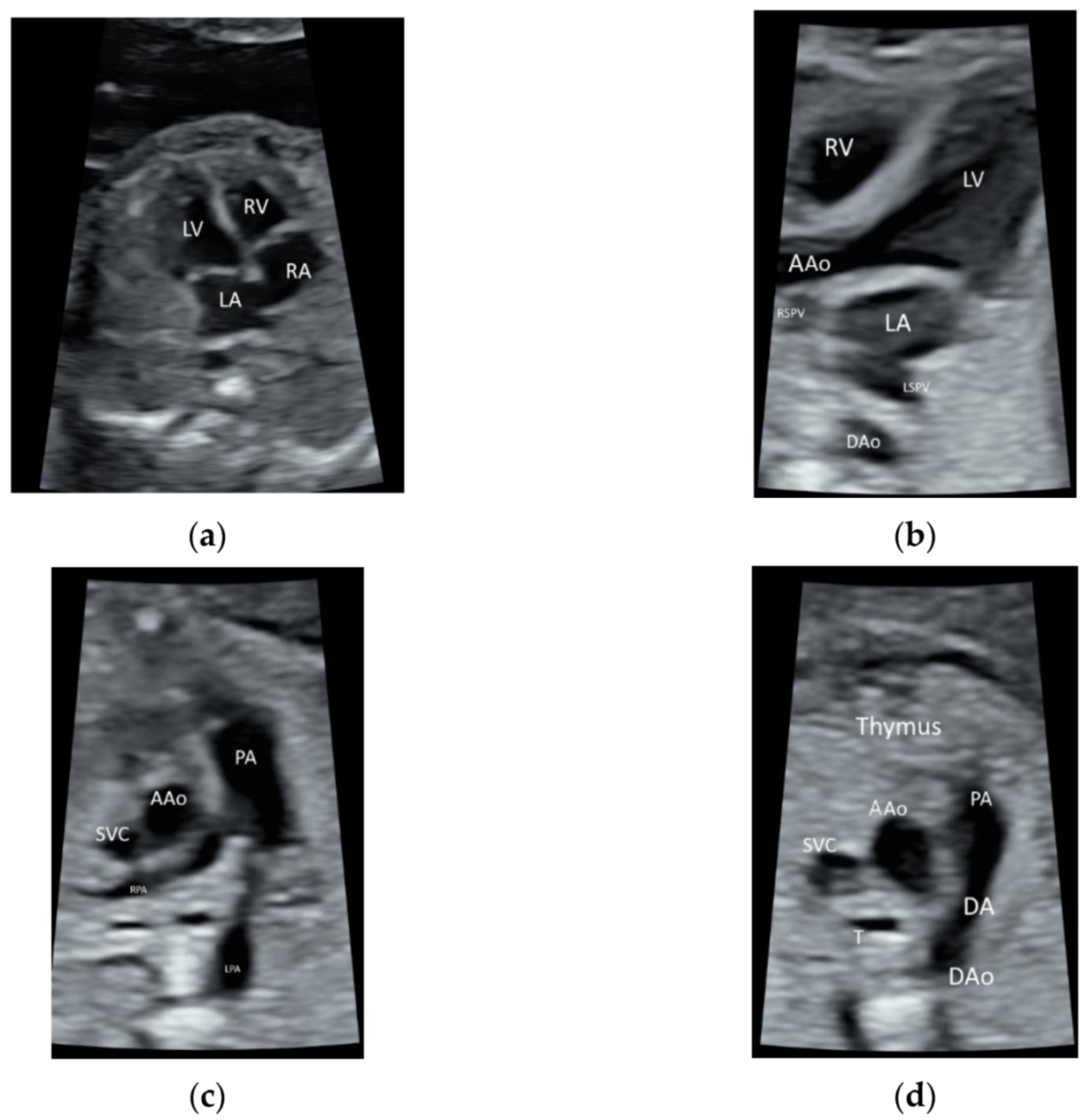
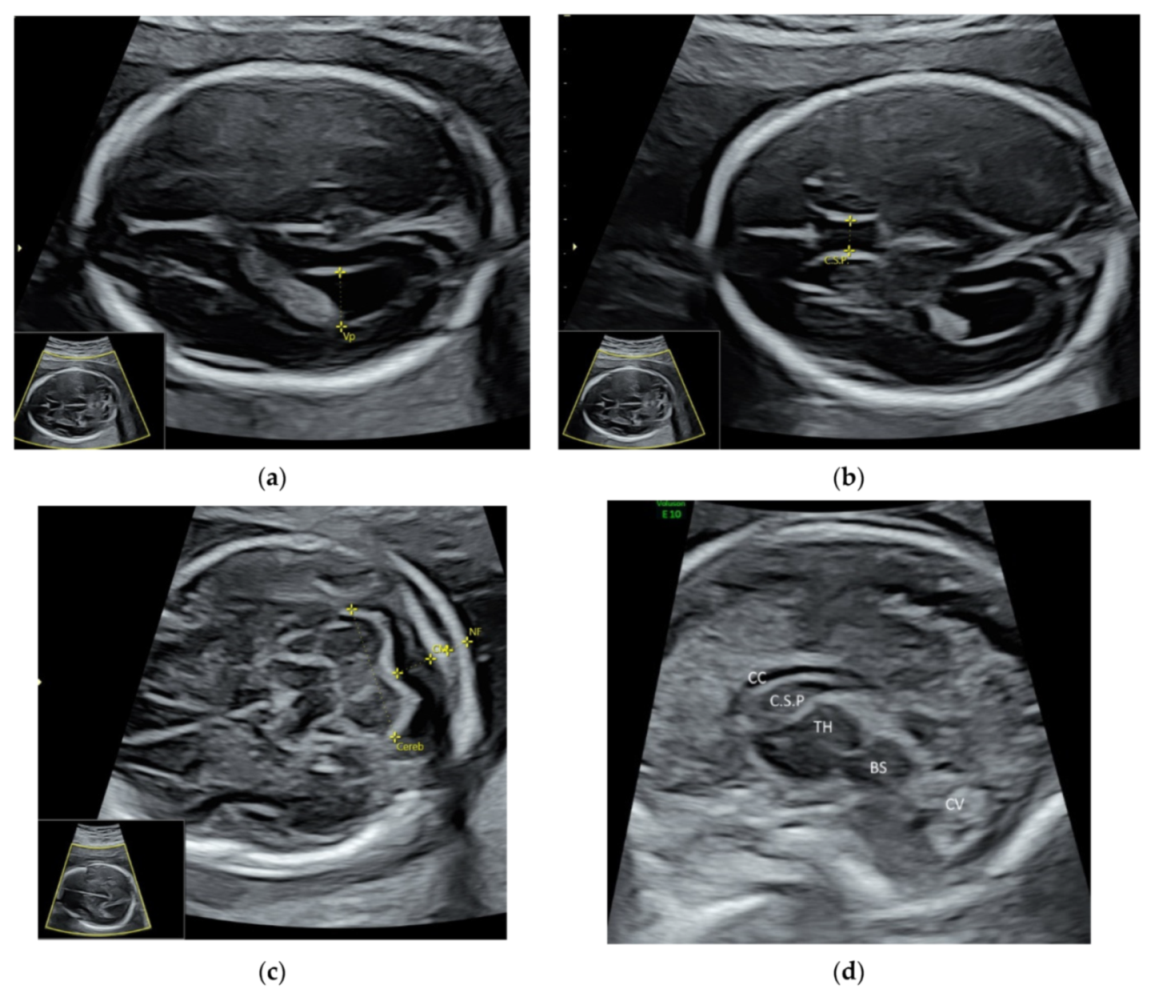
2.1. Fetal Echocardiography and Targeted Neurosonography
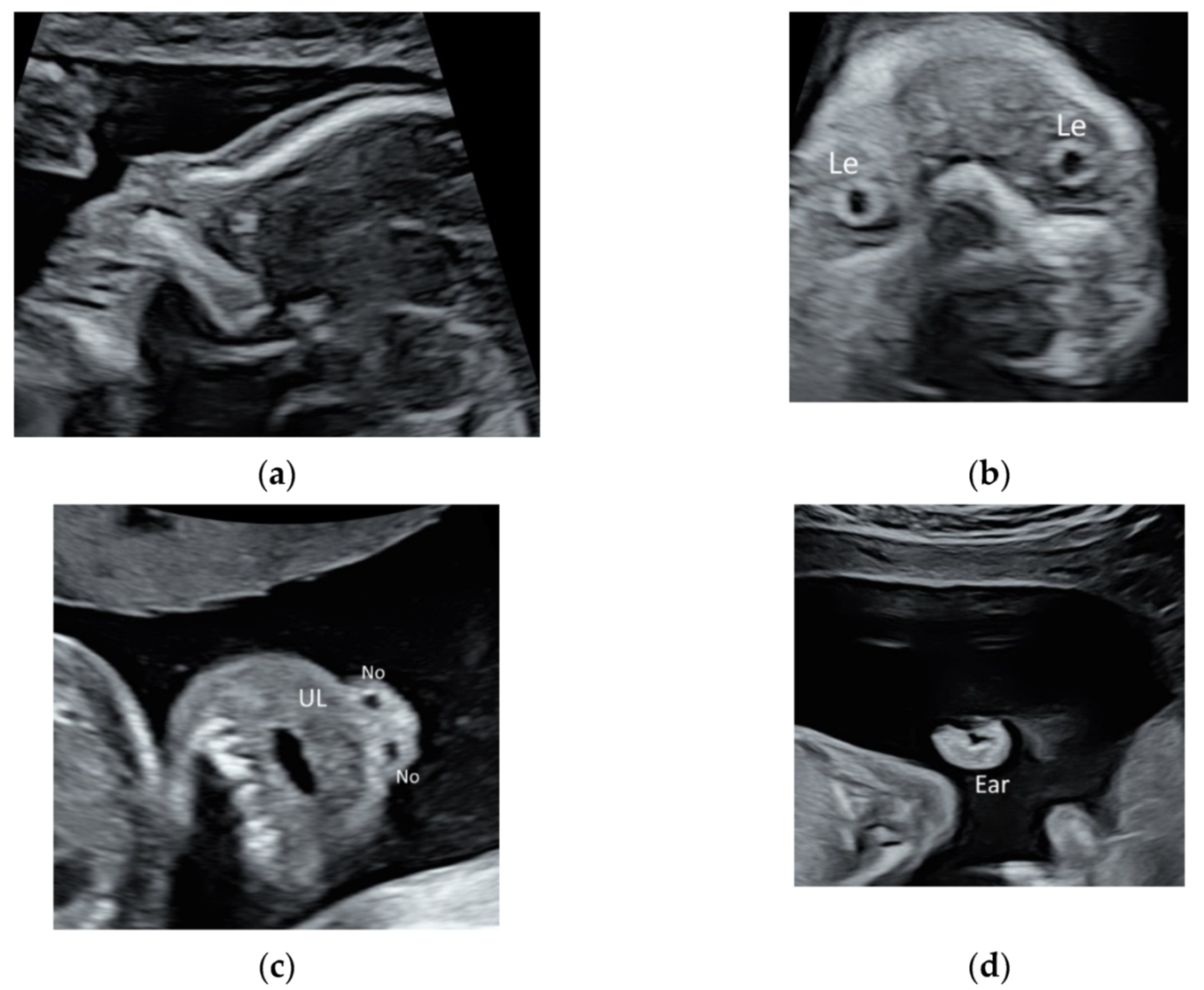
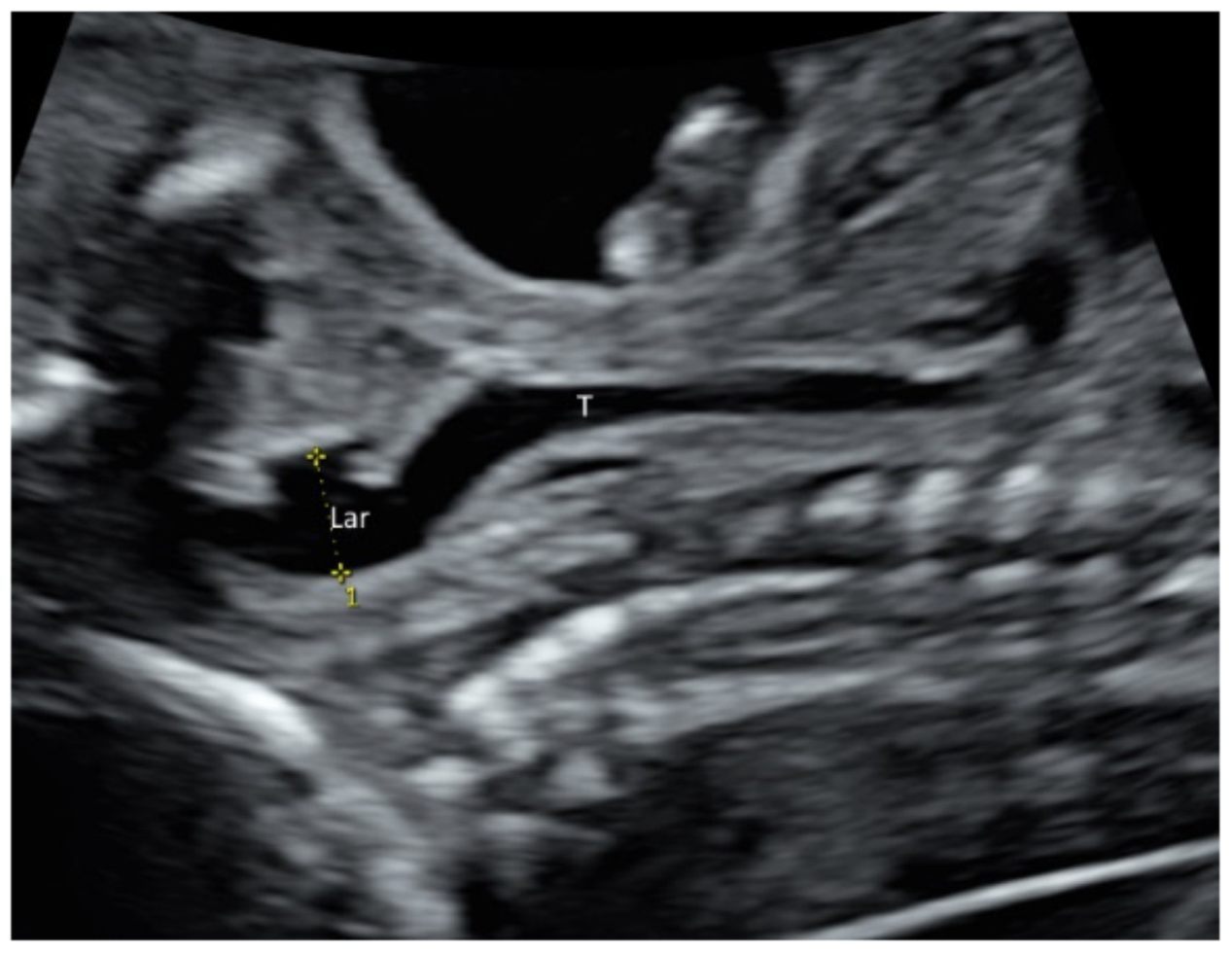
2.2. Face and Neck
2.3. Early Pregnancy Scan
2.4. First Trimester Scan
2.5. Doppler Ultrasound
2.6. Labour Ward Ultrasound
3. Linear Transducer
4. Radiant Flow
5. 3D/4D Ultrasound
- Cleft lip and palate: use gray-scale mode, after a 3D volume acquisition, perform multiplanar/multi-slice analysis and rendering techniques to assess the integrity of palate.
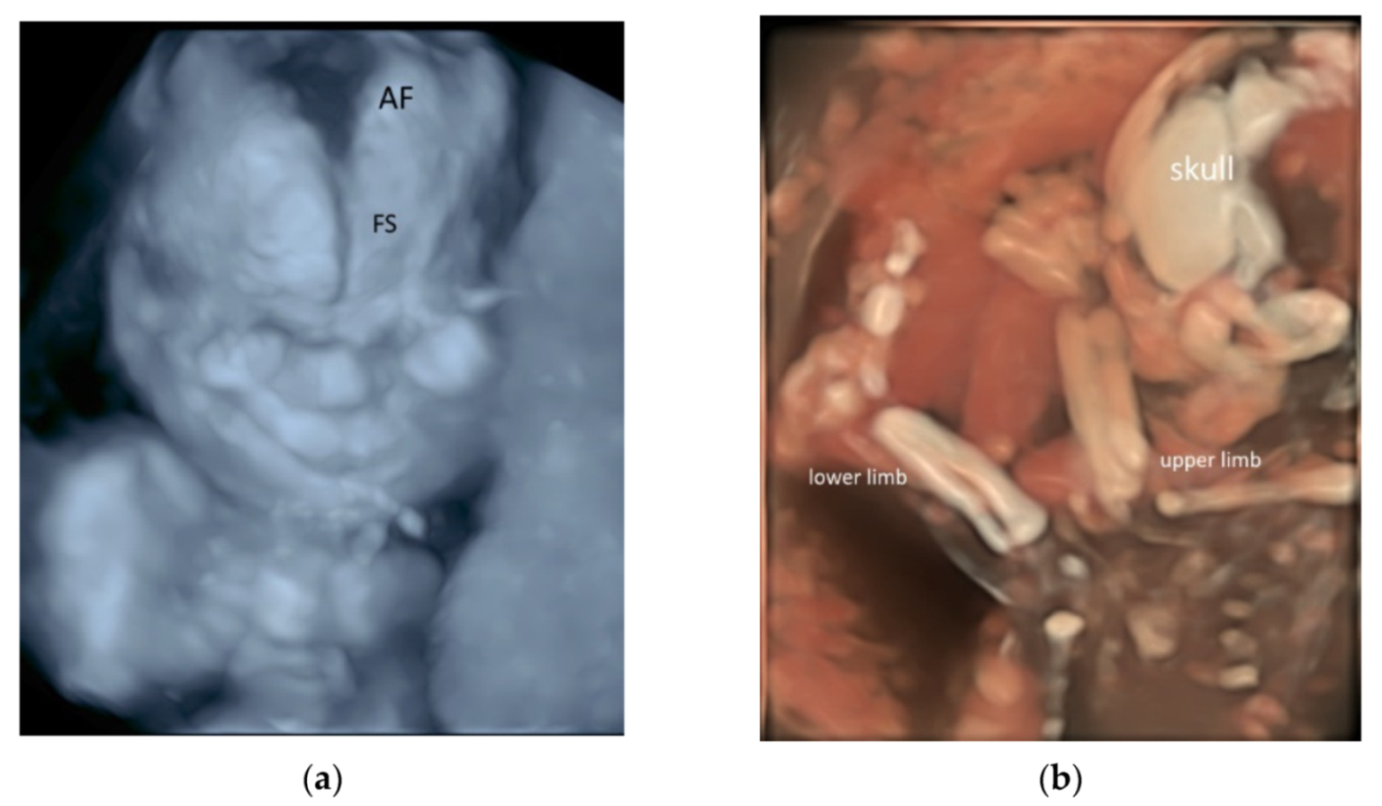
- Short-limbed and short-rib dysplasia: use gray-scale mode, after a 3D volume acquisition with skeletal mode, perform rendering techniques with skeletal mode to examine the long bones and ribs.
- Agenesis of ductus venosus: use high-density power imaging, after a 3D volume acquisition, perform multi-slice analysis to assess the precordial venous system.
- Cardiac outflow tract abnormalities: use color flow, after a STIC volume acquisition, perform multiplanar/multi-slice analysis in a cine-loop of cardiac cycle.
- Atrioventricular valve abnormalities: use matrix probe and gray-scale mode, real- time 4D cine-loop analysis to display the coronal view of atrioventricular valve.
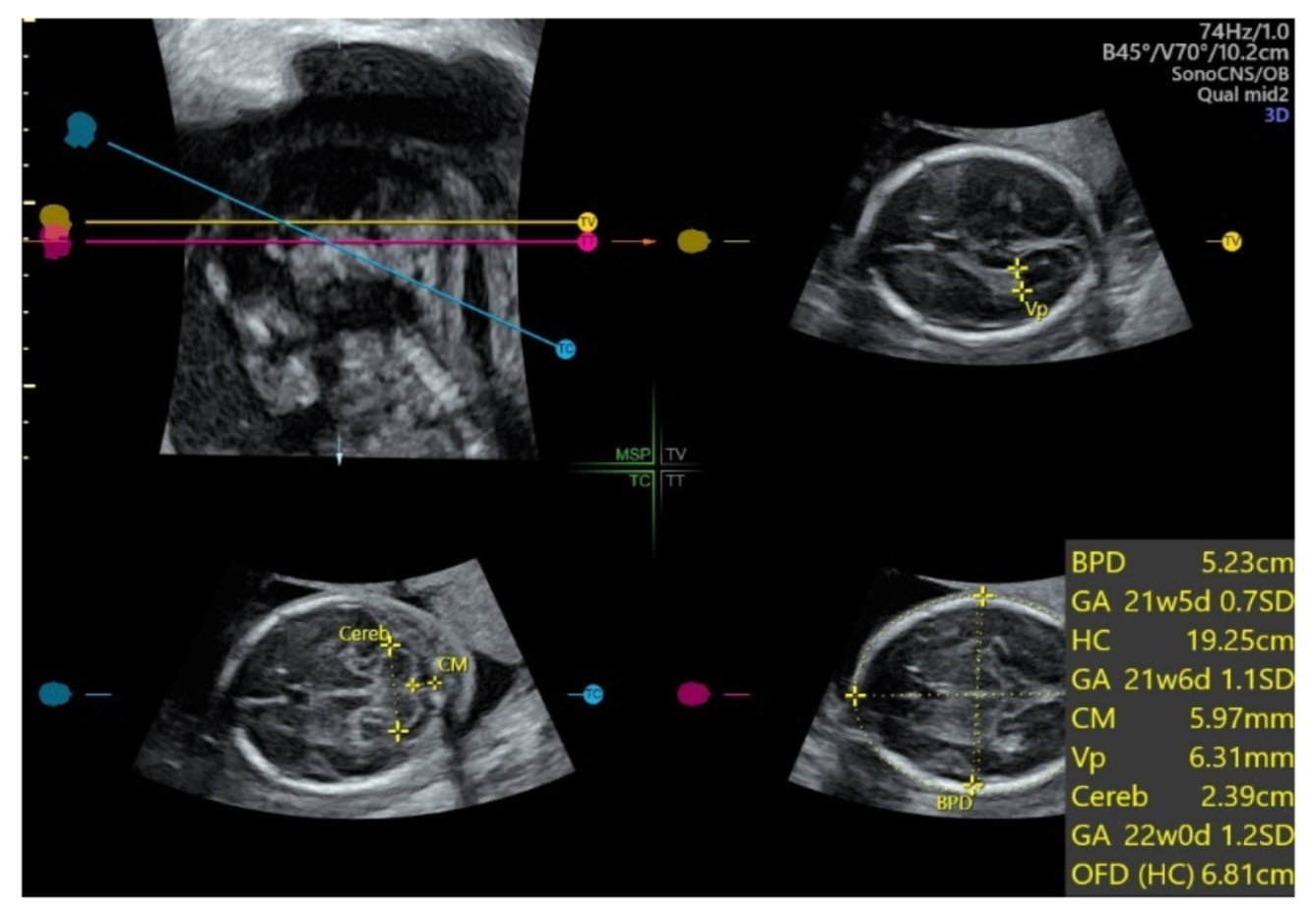
5.1. 3D Neurosonography
5.2. Spatiotemporal Image Correlation
5.3. 3D Ultrasound Examination of Face, Limbs, and Other Structures
5.4. 3D Printing
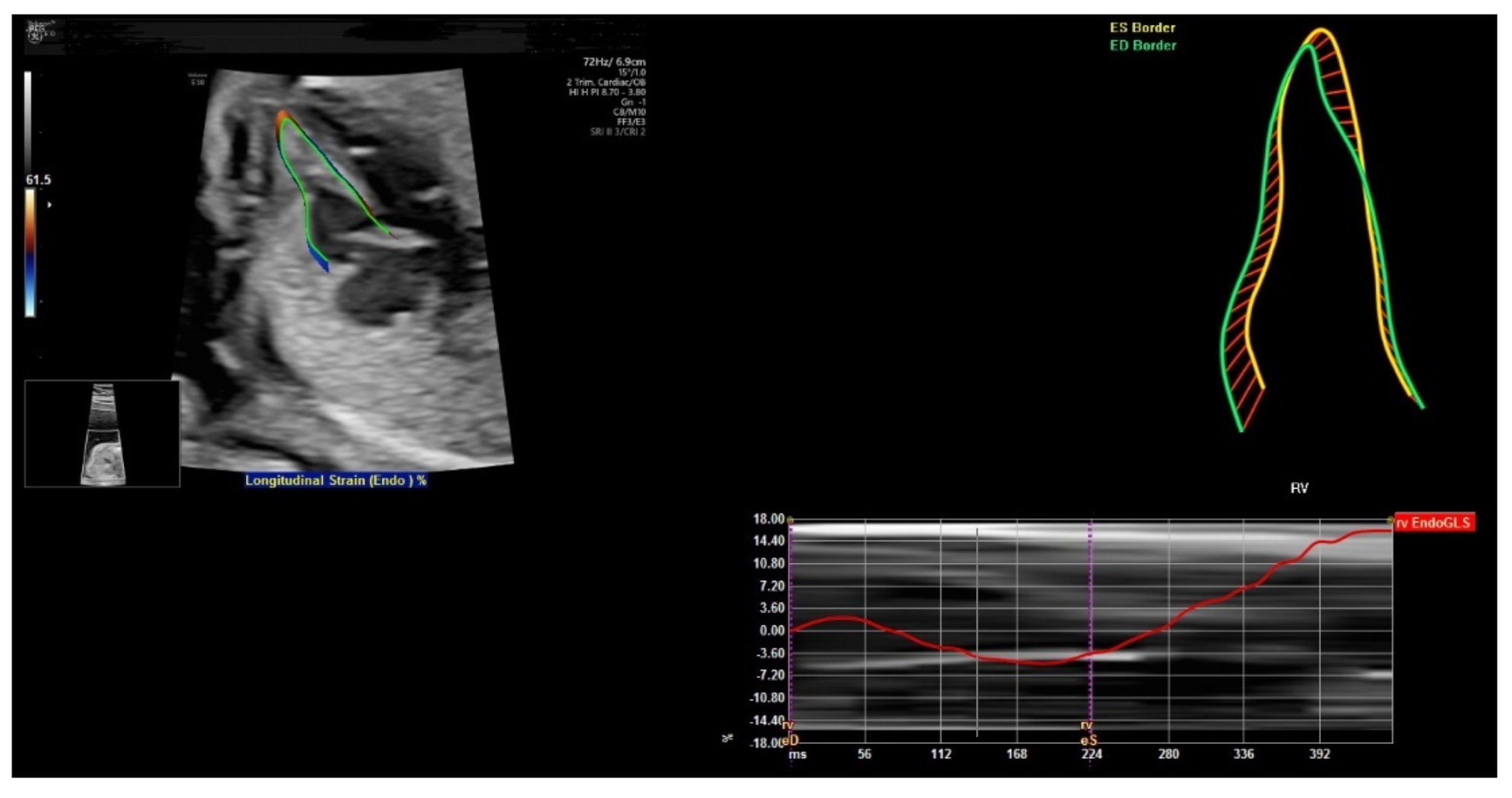
6. FetalHQ
7. Artificial Intelligence
8. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Salomon, L.J.; Alfirevic, Z.; Berghella, V.; Bilardo, C.; Hernandez-Andrade, E.; Johnsen, S.L.; Kalache, K.; Leung, K.Y.; Malinger, G.; Munoz, H.; et al. ISUOG Clinical Standards Committee. Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound Obstet. Gynecol. 2011, 37, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Anonymous. AIUM Practice Parameter for the Performance of Detailed Second- and Third-Trimester Diagnostic Obstetric Ultrasound Examinations. J. Ultrasound Med. 2019, 38, 3093–3100. [Google Scholar] [CrossRef] [PubMed]
- Anonymous. AIUM Practice Parameter for the Performance of Fetal Echocardiography. J. Ultrasound Med. 2020, 39, E5–E16. [Google Scholar]
- Malinger, G.; Paladini, D.; Haratz, K.K.; Monteagudo, A.; Pilu, G.L.; Timor-Tritsch, I.E. ISUOG Practice Guidelines (updated): Sonographic examination of the fetal central nervous system. Part 1: Performance of screening examination and indications for targeted neurosonography. Ultrasound Obstet. Gynecol. 2020, 56, 476–484. [Google Scholar] [CrossRef]
- Paladini, D.; Malinger, G.; Birnbaum, R.; Monteagudo, A.; Pilu, G.; Salomon, L.J.; Timor-Tritsch, I.E. ISUOG Practice Guidelines (updated): Sonographic examination of the fetal central nervous system. Part 2: Performance of targeted neurosonography. Ultrasound Obstet. Gynecol. 2021, 57, 661–671. [Google Scholar] [CrossRef]
- Salomon, L.J.; Alfirevic, Z.; Audibert, F.; Kagan, K.O.; Paladini, D.; Yeo, G.; Raine-Fenning, N.; ISUOG Clinical Standards Committee. ISUOG consensus statement on the impact of non-invasive prenatal testing (NIPT) on prenatal ultrasound practice. Ultrasound Obstet. Gynecol. 2014, 44, 122–123. [Google Scholar] [CrossRef] [Green Version]
- Kenkhuis, M.J.A.; Bakker, M.; Bardi, F.; Fontanella, F.; Bakker, M.K.; Fleurke-Rozema, J.H.; Bilardo, C.M. Effectiveness of a 12-13-week scan for the early diagnosis of fetal congenital anomalies in the cell-free DNA era. Ultrasound Obstet. Gynecol. 2018, 51, 463–469. [Google Scholar] [CrossRef] [Green Version]
- Ficara, A.; Syngelaki, A.; Hammami, A.; Akolekar, R.; Nicolaides, K.H. Value of routine ultrasound examination at 35–37 weeks’ gestation in diagnosis of fetal abnormalities. Ultrasound Obstet. Gynecol. 2020, 55, 75–80. [Google Scholar] [CrossRef]
- Edwards, L.; Hui, L. First and second trimester screening for fetal structural anomalies. Semin. Fetal. Neonatal. Med. 2018, 23, 102–111. [Google Scholar] [CrossRef]
- International Society of Ultrasound in Obstetrics and Gynecology; Carvalho, J.S.; Allan, L.D.; Chaoui, R.; Copel, J.A.; DeVore, G.R.; Hecher, K.; Lee, W.; Munoz, H.; Paladini, D.; et al. ISUOG Practice Guidelines (updated): Sonographic screening examination of the fetal heart. Ultrasound Obstet. Gynecol. 2013, 41, 348–359. [Google Scholar] [CrossRef]
- Platt, L.D. Should the first trimester ultrasound include anatomy survey? Semin. Perinatol. 2013, 37, 310–322. [Google Scholar] [CrossRef] [PubMed]
- Pooh, R.K.; Kurjak, A. 3D/4D sonography moved prenatal diagnosis of fetal anomalies from the second to the first trimester of pregnancy. J. Matern. Fetal. Neonatal. Med. 2012, 25, 433–455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paladini, D.; Vassallo, M.; Tartaglione, A.; Lapadula, C.; Martinelli, P. The role of tissue harmonic imaging in fetal echocardiography. Ultrasound Obstet. Gynecol. 2004, 23, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Biard, J.-M.; Steenhaut, P.; Bernard, P.; Race, V.; Sznajer, Y. Antenatal diagnosis of cardio-facio-cutaneous syndrome: Prenatal characteristics and contribution of fetal facial dysmorphic signs in utero. About a case and review of literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 240, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Mak, A.S.L.; Ma, T.W.L.; Chan, K.Y.K.; Kan, A.S.Y.; Tang, M.H.Y.; Leung, K.Y. Prenatal diagnosis of 5p deletion syndrome: Report of five cases. J. Obstet. Gynaecol. Res. 2019, 45, 923–926. [Google Scholar] [CrossRef]
- Faure, J.M.; Mousty, E.; Bigorre, M.; Wells, C.; Boulot, P.; Captier, G.; Fuchs, F. Prenatal ultrasound diagnosis of cleft palate without cleft lip, the new ultrasound semiology. Prenat. Diagn. 2020, 40, 1447–1458. [Google Scholar] [CrossRef]
- Yu, F.; Leung, K.Y. Prenatal sonographic appearance of laryngeal atresia: A case report. J. Clin. Ultrasound. 2020, 48, 244–246. [Google Scholar] [CrossRef]
- Rogelio, C.M.; Alma, G.V.; Miguel, M.R.; Jonahtan, L.G.; Hugo, L.B.; Eréndira, C.G.; Israel, J.M.; Areli, R.N.; Rosa, V.G.; César, F.H. Prenatal diagnosis of laryngo-tracheo-esophageal anomalies in fetuses with congenital diaphragmatic hernia by ultrasound evaluation of the vocal cords and fetal laryngoesophagoscopy. Prenat. Diagn. 2020, 40, 1540–1546. [Google Scholar]
- Yu, F.N.Y.; Leung, K.Y. Diagnosis and prediction of miscarriage: Can we do better? Hong Kong Med. J. 2020, 26, 90–92. [Google Scholar] [CrossRef]
- Dooley, W.M.; Braud, L.D.; Thanatsis, N.; Memtsa, M.; Jauniaux, E.; Jurkovic, D. Predictive value of presence of amniotic sac without visible embryonic heartbeat in diagnosis of early embryonic demise. Ultrasound Obstet. Gynecol. 2021, 57, 149–154. [Google Scholar] [CrossRef]
- Nadim, B.; Infante, F.; Lu, C.; Sathasivam, C.; Condous, G. Morphological ultrasound types known as ‘blob’ and ‘bagel’ signs should be reclassified from suggesting probable to indicating definite tubal ectopic pregnancy. Ultrasound Obstet. Gynecol. 2018, 51, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Yu, F.N.Y.; Leung, K.Y. Antenatal diagnosis of placenta accreta spectrum (PAS) disorders. Best Pract. Res. Clin. Obstet. Gynaecol. 2021, 72, 13–24. [Google Scholar] [CrossRef] [PubMed]
- D’Antonio, F.; Timor-Tritsch, I.E.; Palacios-Jaraquemada, J.; Monteagudo, A.; Buca, D.; Forlani, F.; Minneci, G.; Foti, F.; Manzoli, L.; Liberati, M.; et al. First-trimester detection of abnormally invasive placenta in high-risk women: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2018, 51, 176–183. [Google Scholar] [CrossRef] [Green Version]
- Salomon, L.J.; Alfirevic, Z.; Bilardo, C.M.; Chalouhi, G.E.; Ghi, T.; Kagan, K.O.; Lau, T.K.; Papageorghiou, A.T.; Raine-Fenning, N.J.; Stirnemann, J.; et al. ISUOG practice guidelines: Performance of first-trimester fetal ultrasound scan. Ultrasound Obstet. Gynecol. 2013, 41, 102–113. [Google Scholar] [PubMed]
- Anonymous. AIUM Practice Parameter for the Performance of Detailed Diagnostic Obstetric Ultrasound Examinations between 12 Weeks 0 Days and 13 Weeks 6 Days. J. Ultrasound Med. 2021, 40, E1–E16. [Google Scholar]
- Minnella, G.P.; Crupano, F.M.; Syngelaki, A.; Zidere, V.; Akolekar, R.; Nicolaides, K.H. Diagnosis of major heart defects by routine first trimester ultrasound examination: Association with increased nuchal translucency, tricuspid regurgitation and abnormal flow in ductus venosus. Ultrasound Obstet. Gynecol. 2020, 55, 637–644. [Google Scholar] [CrossRef]
- Bhide, A.; Acharya, G.; Bilardo, C.M.; Brezinka, C.; Cafici, D.; Hernandez-Andrade, E.; Kalache, K.; Kingdom, J.; Kiserud, T.; Lee, W.; et al. ISUOG practice guidelines: Use of Doppler ultrasonography in obstetrics. Ultrasound Obstet. Gynecol. 2013, 41, 233–239. [Google Scholar] [PubMed]
- Martinez-Portilla, R.J.; Caradeux, J.; Meler, E.; Lip-Sosa, D.L.; Sotiriadis, A.; Figueras, F. Third-trimester uterine artery Doppler for prediction of adverse outcome in late small-for-gestational-age fetuses: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2020, 55, 575–585. [Google Scholar] [CrossRef]
- Sirico, A.; Diemert, A.; Glosemeyer, P.; Hecher, K. Prediction of adverse perinatal outcome by cerebroplacental ratio adjusted for estimated fetal weight. Ultrasound Obstet. Gynecol. 2018, 51, 381–386. [Google Scholar] [CrossRef]
- Khalil, A.; Morales-Roselló, J.; Townsend, R.; Morlando, M.; Papageorghiou, A.; Bhide, A.; Thilaganathan, B. Value of third-trimester cerebroplacental ratio and uterine artery Doppler indices as predictors of stillbirth and perinatal loss. Ultrasound Obstet. Gynecol. 2016, 47, 74–80. [Google Scholar] [CrossRef]
- MacDonald, T.M.; Hui, L.; Robinson, A.J.; Dane, K.M.; Middleton, A.L.; Tong, S.; Walker, S.P. Cerebral-placental-uterine ratio as novel predictor of late fetal growth restriction: Prospective cohort study. Ultrasound Obstet. Gynecol. 2019, 54, 367–375. [Google Scholar] [CrossRef]
- Ghi, T.; Eggebø, T.; Lees, C.; Kalache, K.; Rozenberg, P.; Youssef, A.; Salomon, L.J.; Tutschek, B. ISUOG Practice Guidelines: Intrapartum ultrasound. Ultrasound Obstet. Gynecol. 2018, 52, 128–139. [Google Scholar] [CrossRef] [Green Version]
- Hjartardóttir, H.; Lund, S.H.; Benediktsdóttir, S.; Geirsson, R.T.; Eggebø, T.M. Can ultrasound on admission in active labor predict labor duration and a spontaneous delivery? Am. J. Obstet. Gynecol. MFM. 2021. [Google Scholar] [CrossRef] [PubMed]
- Hjartardóttir, H.; Lund, S.H.; Benediktsdóttir, S.; Geirsson, R.T.; Eggebø, T.M. Fetal descent in nulliparous women assessed by ultrasound: A longitudinal study. Am. J. Obstet. Gynecol. 2021, 224, 378.e1–378.e15. [Google Scholar] [CrossRef] [PubMed]
- Kahrs, B.H.; Usman, S.; Ghi, T.; Youssef, A.; Torkildsen, E.A.; Lindtjørn, E.; Østborg, T.B.; Benediktsdottir, S.; Brooks, L.; Harmsen, L.; et al. Sonographic prediction of outcome of vacuum deliveries: A multicenter, prospective cohort study. Am. J. Obstet. Gynecol. 2017, 217, 69.e1–69.e10. [Google Scholar] [CrossRef] [Green Version]
- Usman, S.; Wilkinson, M.; Barton, H.; Lees, C.C. The feasibility and accuracy of ultrasound assessment in the labor room. J. Matern. Fetal Neonatal. Med. 2019, 32, 3442–3451. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Zhang, Y.; Chen, S.S.; Xiang, X.W.; Wen, J.; Yi, M.; He, B.Y.; Hu, B. Diagnostic accuracy of cervical elastography in predicting preterm delivery: A systematic review and meta-analysis. Meta-Anal. Med. 2019, 98, e16449. [Google Scholar] [CrossRef]
- Lu, J.; Cheng, Y.K.Y.; Ho, S.Y.S.; Sahota, D.S.; Hui, L.L.; Poon, L.C.; Leung, T.Y. The predictive value of cervical shear wave elastography in the outcome of labor induction. Acta Obstet. Gynecol. Scand. 2020, 99, 59–68. [Google Scholar] [CrossRef]
- Mak, A.S.L.; Leung, K.Y. Prenatal ultrasonography of craniofacial abnormalities. Ultrasonography 2019, 38, 13–24. [Google Scholar] [CrossRef] [Green Version]
- Persico, N.; Moratalla, J.; Lombardi, C.M.; Zidere, V.; Allan, L.; Nicolaides, K.H. Fetal echocardiography at 11-13 weeks by transabdominal high-frequency ultrasound. Ultrasound Obstet. Gynecol. 2011, 37, 296–301. [Google Scholar] [CrossRef]
- Votino, C.; Kacem, Y.; Dobrescu, O.; Dessy, H.; Cos, T.; Foulon, W.; Jani, J. Use of a high-frequency linear transducer and MTI filtered color flow mapping in the assessment of fetal heart anatomy at the routine 11 to 13 + 6-week scan: A randomized trial. Ultrasound Obstet. Gynecol. 2012, 39, 145–151. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Y. Fetal Vascular Rings and Pulmonary Slings: Strategies for Two- and Three-Dimensional Echocardiographic Diagnosis. J. Am. Soc. Echocardiogr. 2021, 34, 336–351. [Google Scholar] [CrossRef] [PubMed]
- Yin, H.; Li, Y. Diagnostic value of Omniview technique on the agenesis of corpus callosum. J. Matern. Fetal. Neonatal. Med. 2019, 32, 3806–3811. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, Y.; Wang, M. Prenatal diagnosis of an aberrant ductus venosus draining into the coronary sinus using two- and three-dimensional echocardiography: A case report. BMC Pregnancy Childbirth. 2021, 21, 392. [Google Scholar] [CrossRef]
- Merz, E.; Pashaj, S. Advantages of 3D ultrasound in the assessment of fetal abnormalities. J. Perinat. Med. 2017, 45, 643–650. [Google Scholar] [CrossRef]
- Chaoui, R.; Abuhamad, A.; Martins, J.; Heling, K.S. Recent development in three- and four-dimension fetal echocardiography. Fetal. Diagn Ther. 2020, 47, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Paladini, D.; Volpe, P. Posterior fossa and vermian morphometry in the characterization of fetal cerebellar abnormalities: A prospective three-dimensional ultrasound study. Ultrasound Obstet. Gynecol. 2006, 27, 482–489. [Google Scholar] [CrossRef] [PubMed]
- Pashaj, S.; Merz, E. Detection of Fetal Corpus Callosum Abnormalities by Means of 3D Ultrasound. Ultraschall Med. 2016, 37, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Frisova, V.; Srutova, M.; Hyett, J. 3-D Volume Assessment of the Corpus Callosum and Cerebellar Vermis Using Various Volume Acquisition and Post-Processing Protocols. Fetal. Diagn Ther. 2018, 43, 199–207. [Google Scholar] [CrossRef]
- Wang, L.M.; Leung, K.Y.; Tang, M. Prenatal evaluation of facial clefts by three-dimensional extended imaging. Prenat. Diagn. 2007, 27, 722–729. [Google Scholar] [CrossRef]
- Rotten, D.; Levaillant, J.M.; Martinez, H.; Pointe, H.D.L.; Vicaut, E. The fetal mandible: A 2D and 3D sonographic approach to the diagnosis of retrognathia and micrognathia. Ultrasound Obstet. Gynecol. 2002, 19, 122–130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tutschek, B.; Blaas, H.K.; Abramowicz, J.; Baba, K.; Deng, J.; Lee, W.; Merz, E.; Platt, L.; Pretorius, D.; Timor-Tritsch, I.E.; et al. ISUOG 3D Special Interest Group. Three-dimensional ultrasound imaging of the fetal skull and face. Ultrasound Obstet. Gynecol. 2017, 50, 7–16. [Google Scholar] [CrossRef]
- Schut, P.C.; Cohen-Overbeek, T.E.; Galis, F.; Broek, C.M.A.T.; Steegers, E.A.; Eggink, A.J. Adverse Fetal and Neonatal Outcome and an Abnormal Vertebral Pattern: A Systematic Review. Obstet. Gynecol. Surv. 2016, 71, 741–750. [Google Scholar] [CrossRef] [PubMed]
- Helfer, T.M.; Peixoto, A.B.; Tonni, G.; Júnior, E.A. Craniosynostosis: Prenatal diagnosis by 2D/3D ultrasound, magnetic resonance imaging and computed tomography. Med. Ultrason. 2016, 18, 378–385. [Google Scholar] [CrossRef]
- Dall’Asta, A.; Grisolia, G.; Nanni, M.; Volpe, N.; Schera, G.B.L.; Frusca, T.; Ghi, T. Sonographic demonstration of fetal esophagus using three-dimensional ultrasound imaging. Ultrasound Obstet. Gynecol. 2019, 54, 746–751. [Google Scholar] [CrossRef] [PubMed]
- Calì, G.; Foti, F.; Minneci, G. 3D power Doppler in the evaluation of abnormally invasive placenta. J. Perinat Med. 2017, 45, 701–709. [Google Scholar] [CrossRef] [PubMed]
- Tutschek, B.; Blaas, H.K. A human embryo in the palm of your hand. Ultrasound Obstet. Gynecol. 2017, 50, 539–540. [Google Scholar] [CrossRef] [Green Version]
- Coté, J.J.; Badura-Brack, A.S.; Walters, R.W.; Dubay, N.G.; Bredehoeft, M.R. Randomized Controlled Trial of the Effects of 3D-Printed Models and 3D Ultrasonography on Maternal-Fetal Attachment. J. Obstet. Gynecol. Neonatal. Nurs. 2020, 49, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.L.; Ahn, E.S.; Garcia, J.R.; Miller, G.T.; Satin, A.J.; Baschat, A.A. Ultrasound-based three-dimensional printed medical model for multispecialty team surgical rehearsal prior to fetoscopic myelomeningocele repair. Ultrasound Obstet. Gynecol. 2018, 51, 836–840. [Google Scholar] [CrossRef]
- Chen, S.A.; Ong, C.S.; Hibino, N.; Baschat, A.A.; Garcia, J.R.; Miller, J.L. 3D printing of fetal heart using 3D ultrasound imaging data. Ultrasound Obstet. Gynecol. 2018, 52, 808–809. [Google Scholar] [CrossRef] [Green Version]
- Veronese, P.; Bertelli, F.; Cattapan, C.; Andolfatto, M.; Gervasi, M.T.; Vida, V.L. Three-Dimensional Printing of Fetal Heart With d-Transposition of the Great Arteries From Ultrasound Imaging Data. World J. Pediatr. Congenit. Heart Surg. 2021, 12, 291–292. [Google Scholar] [CrossRef] [PubMed]
- DeVore, G.R.; Klas, B.; Satou, G.; Sklansky, M. 24-segment sphericity index: A new technique to evaluate fetal cardiac diastolic shape. Ultrasound Obstet. Gynecol. 2018, 51, 650–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeVore, G.R.; Satou, G.; Sklansky, M. Abnormal Fetal Findings Associated With a Global Sphericity Index of the 4-Chamber View Below the 5th Centile. J. Ultrasound Med. 2017, 36, 2309–2318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hobbins, J.C.; Gumina, D.L.; Zaretsky, M.V.; Driver, C.; Wilcox, A.; DeVore, G.R. Size and shape of the four-chamber view of the fetal heart in fetuses with an estimated fetal weight less than the tenth centile. Am. J. Obstet. Gynecol. 2019, 221, e1–e495. [Google Scholar] [CrossRef]
- Van Oostrum, N.H.; Chantelle, M.; van der Woude, D.A.; Kemps, H.M.; Oei, S.G.; van Laar, J.O. Fetal strain and strain rate during pregnancy measured with speckle tracking echocardiography: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 250, 178–187. [Google Scholar] [CrossRef]
- Van Oostrum, N.H.; Derks, K.; van der Woude, D.A.; Clur, S.A.; Oei, S.G.; van Laar, J.O. Two-dimensional Speckle tracking echocardiography in Fetal Growth Restriction: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 254, 87–94. [Google Scholar] [CrossRef]
- Kim, H.P.; Lee, S.M.; Kwon, J.Y.; Park, Y.; Kim, K.C.; Seo, J.K. Automatic evaluation of fetal head biometry from ultrasound images using machine learning. Physiol. Meas. 2019, 40, 065009. [Google Scholar] [CrossRef] [Green Version]
- Salim, I.; Cavallaro, A.; Ciofolo-Veit, C.; Rouet, L.; Raynaud, C.; Mory, B.; Billon, A.C.; Harrison, G.; Roundhill, D.; Papageorghiou, A.T. Evaluation of automated tool for two-dimensional fetal biometry. Ultrasound Obstet. Gynecol. 2019, 54, 650–654. [Google Scholar] [CrossRef]
- Society of Diagnostic Medical Sonography. Industry Standards for the Prevention of Work Related Musculoskeletal Disorders in Sonography. J. Diagn. Med. Sonogr. 2017, 33, 371–391. [Google Scholar]
- Pluym, I.D.; Afshar, Y.; Holliman, K.; Kwan, L.; Bolagani, A.; Mok, T.; Silver, B.; Ramirez, E.; Han, C.S.; Platt, L.D. Accuracy of automated three-dimensional ultrasound imaging technique for fetal head biometry. Ultrasound Obstet. Gynecol. 2021, 57, 798–803. [Google Scholar] [CrossRef]
- Yeo, L.; Romero, R. New and advanced features of fetal intelligent navigation echocardiography (FINE) or 5D heart. J. Matern. Fetal Neonatal. Med. 2020, 6, 1–19. [Google Scholar] [CrossRef]
- Drukker, L.; Noble, J.A.; Papageorghiou, A.T. Introduction to artificial intelligence in ultrasound imaging in obstetrics and gynecology. Ultrasound Obstet. Gynecol. 2020, 56, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Abramowicz, J.S. Obstetric ultrasound: Where are we and where are we going? Ultrasonography 2021, 40, 57–74. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Wang, Y.; Yang, X.; Lei, B.; Liu, L.; Li, S.X.; Ni, D.; Wang, T. Deep Learning in Medical Ultrasound Analysis: A Review. Engineering 2019, 5, 261–275. [Google Scholar] [CrossRef]
- Shozu, K.; Komatsu, M.; Sakai, A.; Komatsu, R.; Dozen, A.; Machino, H.; Yasutomi, S.; Arakaki, T.; Asada, K.; Kaneko, S.; et al. Model-Agnostic Method for Thoracic Wall Segmentation in Fetal Ultrasound Videos. Biomolecules 2020, 10, 1691. [Google Scholar] [CrossRef] [PubMed]
- Re, C.; Bertucci, E.; Weissmann-Brenner, A.; Achiron, R.; Mazza, V.; Gindes, L. Fetal thymus volume estimation by virtual organ computer-aided analysis in normal pregnancies. J. Ultrasound Med. 2015, 34, 847–852. [Google Scholar] [CrossRef]
- Qi, H.; Collins, S.; Noble, J.A. Automatic Lacunae Localization in Placental Ultrasound Images via Layer Aggregation. Med. Image Comput. Comput. Assist. Interv. 2018, 11, 921–929. [Google Scholar]







| Mode | Volume Acquisition | 3D/4D Analysis |
|---|---|---|
| Gray scale | 3D: different modes | Multiplanar |
| Color flow | 4D | Multislice |
| Power doppler | STIC 1 | Rendered view: different modes |
| High-density power imaging | Matrix probe | Cine loop |
| B-flow | Semi-automatic analysis | |
| Volume measurement | ||
| Power Doppler measurements |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leung, K.-Y. Applications of Advanced Ultrasound Technology in Obstetrics. Diagnostics 2021, 11, 1217. https://doi.org/10.3390/diagnostics11071217
Leung K-Y. Applications of Advanced Ultrasound Technology in Obstetrics. Diagnostics. 2021; 11(7):1217. https://doi.org/10.3390/diagnostics11071217
Chicago/Turabian StyleLeung, Kwok-Yin. 2021. "Applications of Advanced Ultrasound Technology in Obstetrics" Diagnostics 11, no. 7: 1217. https://doi.org/10.3390/diagnostics11071217
APA StyleLeung, K.-Y. (2021). Applications of Advanced Ultrasound Technology in Obstetrics. Diagnostics, 11(7), 1217. https://doi.org/10.3390/diagnostics11071217





