Diagnostic Insights from Plethysmographic Alveolar Pressure Assessed during Spontaneous Breathing in COPD Patients
Abstract
1. Introduction
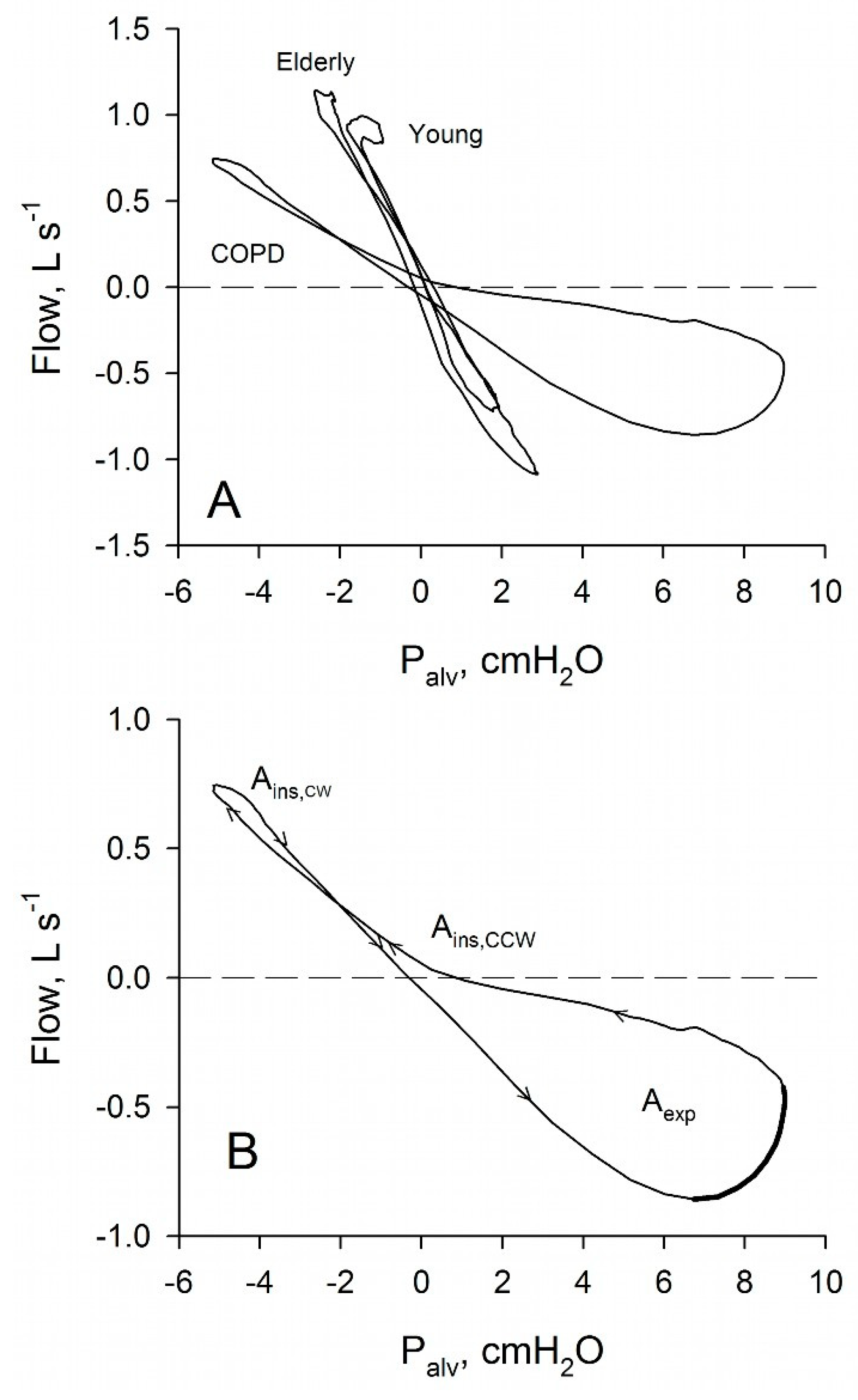
2. Plethysmographic Palv- Loops
2.1. Physiopathological Significance of Plethysmographic Palv- Loops
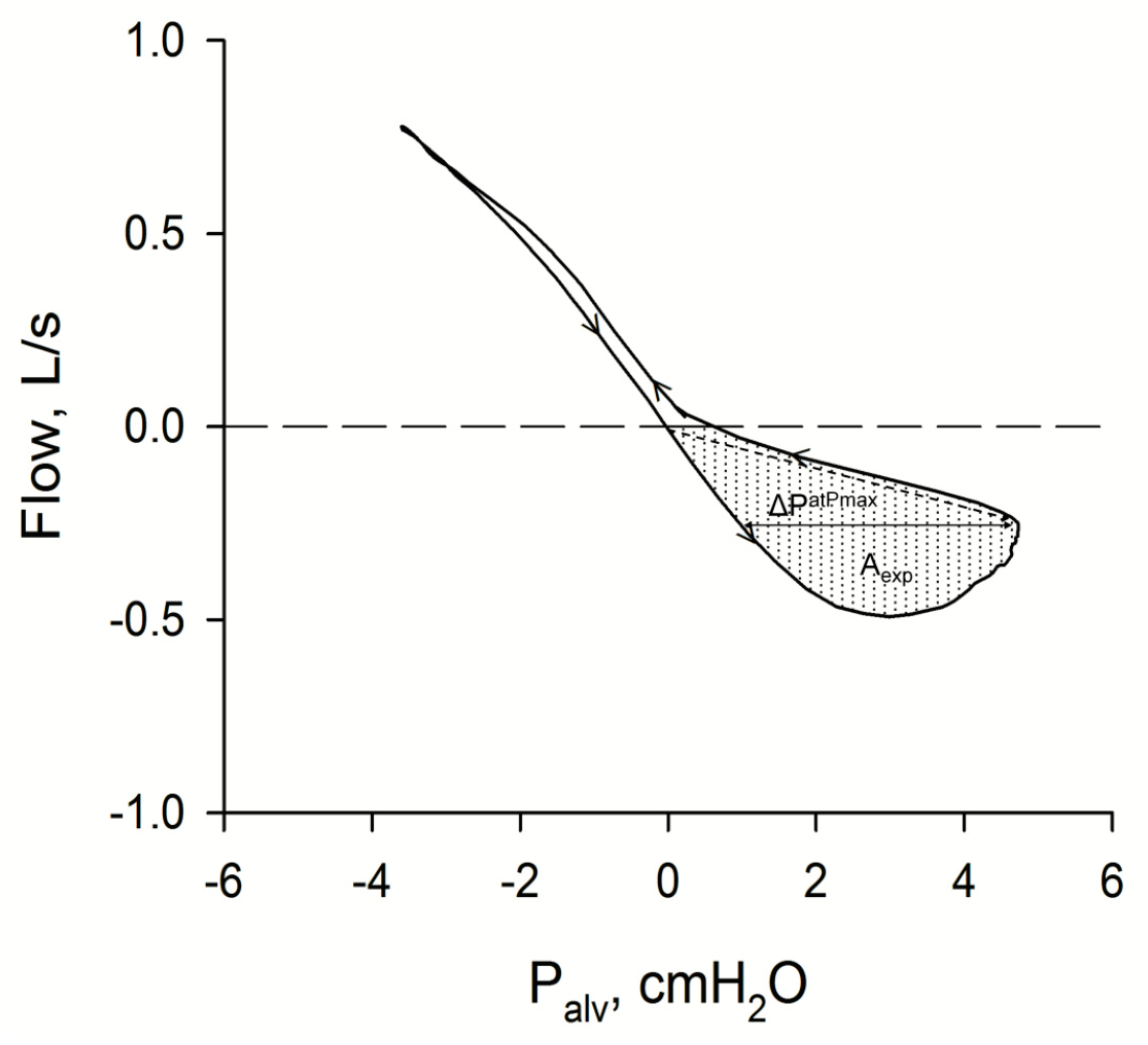
2.2. Predicting Tidal Expiratory Flow Limitation with Palv- Loops
2.3. Other Available Methods to Assess Tidal Expiratory Flow-Limitation
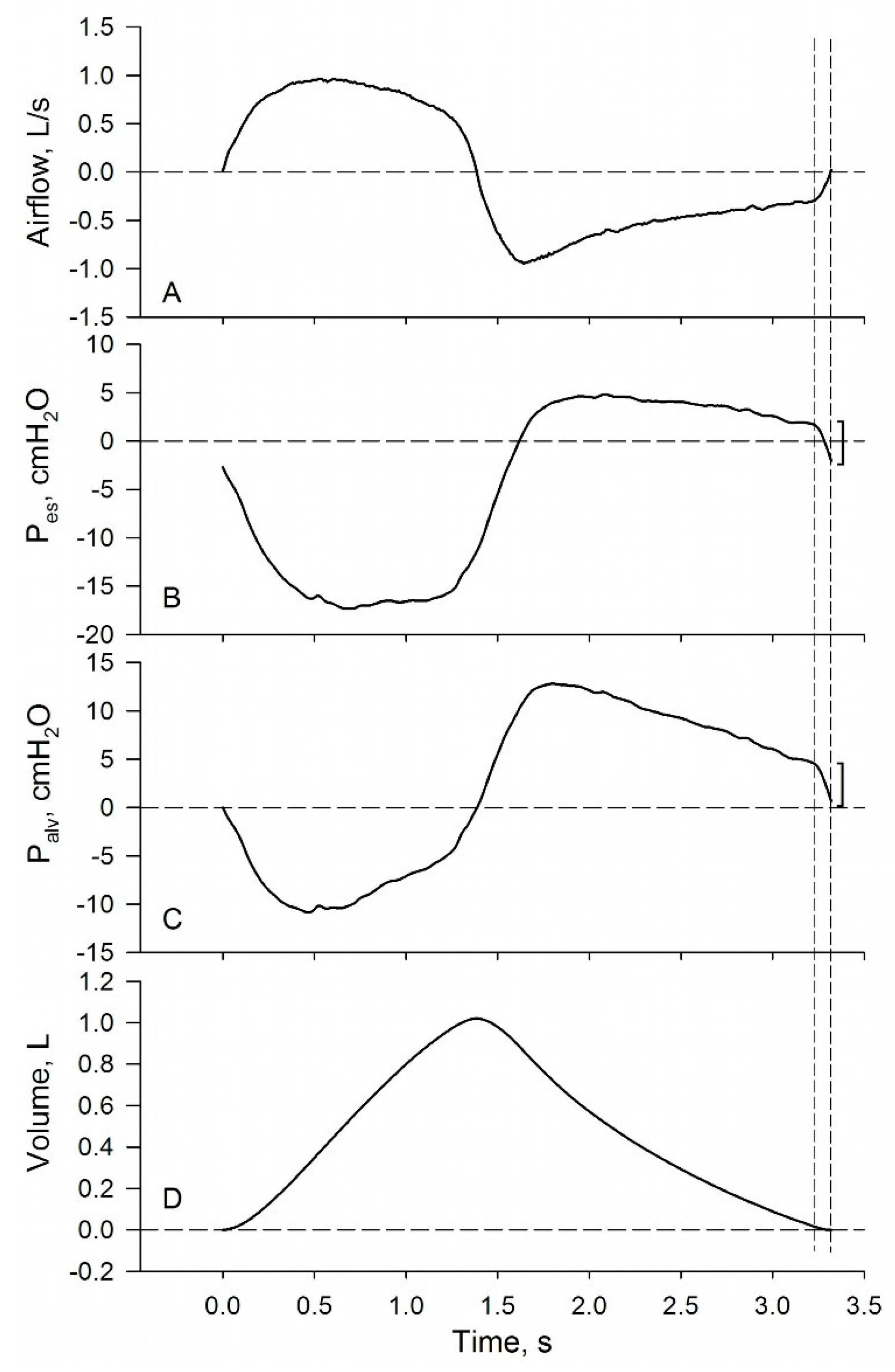
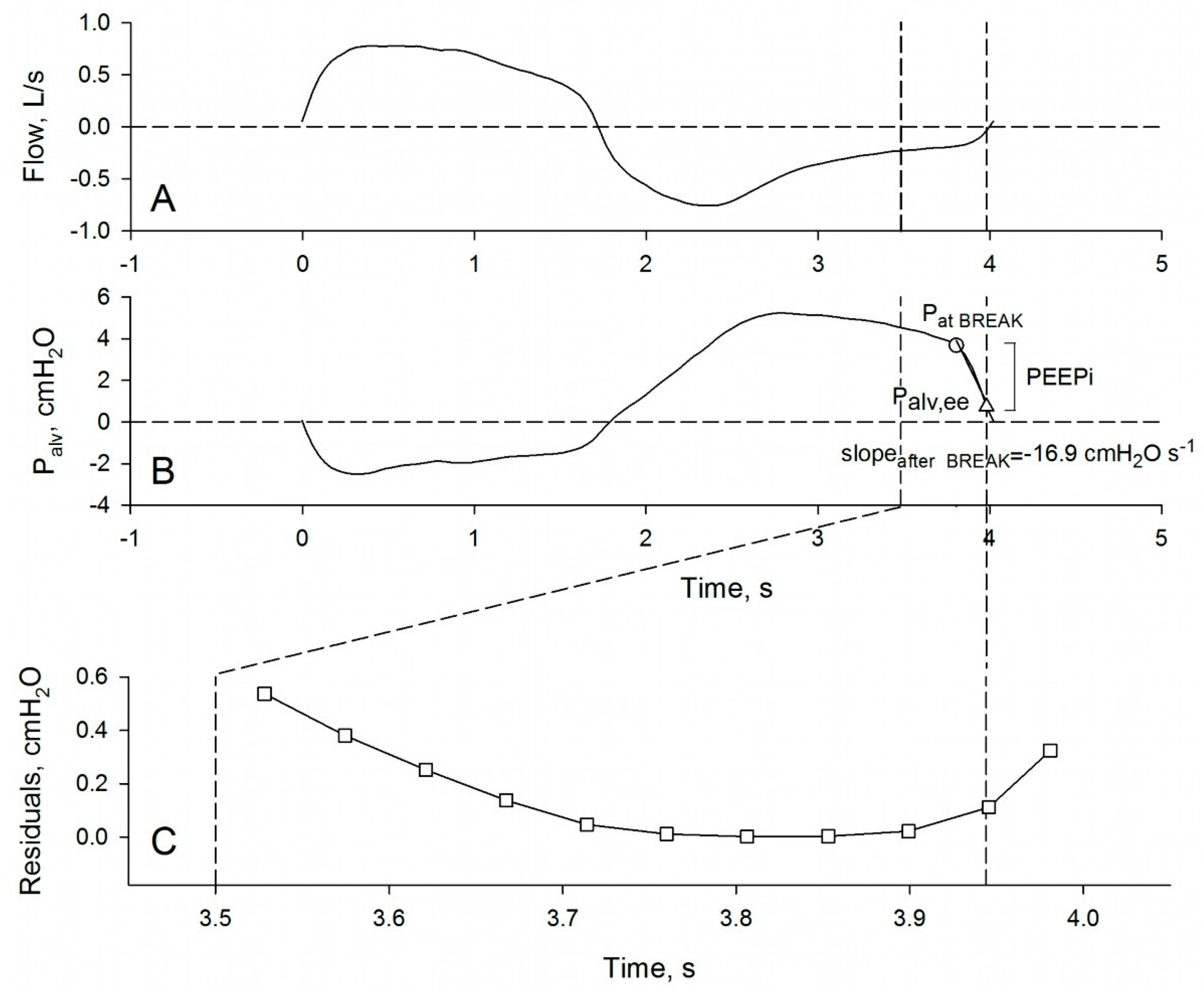
3. Plethysmographic Measurement of Intrinsic PEEP in Spontaneously Breathing Subjects
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Dubois, A.B.; Botelho, S.Y.; Bedell, G.N.; Marshall, R.; Comroe, J.H. A rapid plethysmographic method for measuring thoracic gas volume: A comparison with a nitrogen washout method for measuring functional residual capacity in normal subjects 1. J. Clin. Investig. 1956, 35, 322–326. [Google Scholar] [CrossRef] [PubMed]
- Dubois, A.B.; Botelho, S.Y.; Comroe, J.H. A new method for measuring airway resistance in man using a body plethysmograph: Values in normal subjects and in patients with respiratory disease 1. J. Clin. Investig. 1956, 35, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Briscoe, W.A.; Dubois, A.B. The Relationship Between Airway Resistance, Airway Conductance and Lung Volume in Subjects of Different Age and Body Size. J. Clin. Investig. 1958, 37, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Butler, J.; Caro, C.G.; Alcala, R.; Dubois, A.B. Physiological factors affecting airway resistance in normal subjects and in patients with obstructive respiratory disease. J. Clin. Investig. 1960, 39, 584–591. [Google Scholar] [CrossRef]
- Coates, A.; Peslin, R.; Rodenstein, D.; Stocks, J. Measurement of lung volumes by plethysmography. Eur. Respir. J. 1997, 10, 1415–1427. [Google Scholar] [CrossRef]
- Goldman, M.; Smith, H.; Ulmer, W. Whole-body plethysmography. In Lung Function Testing; European Respiratory Society (ERS): Sheffield, UK, 2005; pp. 15–43. [Google Scholar]
- Criée, C.; Sorichter, S.; Smith, H.; Kardos, P.; Merget, R.; Heise, D.; Berdel, D.; Köhler, D.; Magnussen, H.; Marek, W.; et al. Body plethysmography—Its principles and clinical use. Respir. Med. 2011, 105, 959–971. [Google Scholar] [CrossRef]
- Sackner, M.A.; Feisal, K.A.; Dubois, A.B. Determination of tissue volume and carbon dioxide dissociation slope of the lungs in man. J. Appl. Physiol. 1964, 19, 374–380. [Google Scholar] [CrossRef]
- Jaeger, M.J.; Otis, A.B. Measurement of airway resistance with a volume displacement body plethysmograph. J. Appl. Physiol. 1964, 19, 813–819. [Google Scholar] [CrossRef]
- Jonson, B.; Bouhuys, A. Measurement of alveolar pressure. J. Appl. Physiol. 1967, 22, 1081–1085. [Google Scholar] [CrossRef]
- Matthys, H. Lungenfunktionsdiagnostik Mittels Ganzkörperplethysmographie; Schattauer: Stuttgart, Germany, 1972. [Google Scholar]
- Loring, S.H.; Garcia-Jacques, M.; Malhotra, A. Pulmonary characteristics in COPD and mechanisms of increased work of breathing. J. Appl. Physiol. 2009, 107, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Peslin, R.; Duvivier, C.; Vassiliou, M.; Gallina, C. Thermal artifacts in plethysmographic airway resistance measurements. J. Appl. Physiol. 1995, 79, 1958–1965. [Google Scholar] [CrossRef] [PubMed]
- Peslin, R.; Duvivier, C.; Malvestio, P.; Benis, A.R. Correction of thermal artifacts in plethysmographic airway resistance measurements. J. Appl. Physiol. 1996, 80, 2198–2203. [Google Scholar] [CrossRef] [PubMed]
- Smidt, U.; Muysers, K.; Buchheim, W. Electronic compensation of differences in temperature and water vapour between in- and expired air and other signal handling in body plethysmography. In Progress in Respiration Research, Body Plethys-Mography; van de Woestijne, K., DuBois, A.B., Eds.; Karger: Basel, Switzerland, 1969; pp. 39–49. [Google Scholar]
- Woitowitz, H.; Günthner, W.; Woitowitz, R. Some experiences with electronic simulation of BTPS conditions in body ple-thysmography. In Proceedings of the International Symposium, Progress in Respiration Research, Body Plethysmography, Nijmegen, The Netherlands, 17–18 September 1968; DuBois, A.B., van de Woestijne, K., Eds.; Karger: Basel, Switzerland, 1969; pp. 50–59. [Google Scholar]
- Peslin, R.; Duvivier, C.; Malvestio, P.; Benis, A.; Polu, J. Frequency dependence of specific airway resistance in a commercialized plethysmograph. Eur. Respir. J. 1996, 9, 1747–1750. [Google Scholar] [CrossRef] [PubMed]
- Subbarao, P.; Hülskamp, G.; Stocks, J. Limitations of electronic compensation for measuring plethysmographic airway resistance in infants. Pediatr. Pulmonol. 2005, 40, 45–52. [Google Scholar] [CrossRef]
- Santus, P.; Radovanovic, D.; Henchi, S.; Di Marco, F.; Centanni, S.; D’Angelo, E.; Pecchiari, M. Assessment of acute bronchodilator effects from specific airway resistance changes in stable COPD patients. Respir. Physiol. Neurobiol. 2014, 197, 36–45. [Google Scholar] [CrossRef]
- Topalovic, M.; Derom, E.; Osadnik, C.R.; Troosters, T.; Decramer, M.; Janssens, W.; Belgian Pulmonary Function Study Investigators. Airways resistance and specific conductance for the diagnosis of obstructive airways diseases. Respir. Res. 2015, 16, 88. [Google Scholar] [CrossRef]
- Radovanovic, D.; Pecchiari, M.; Pirracchio, F.; Zilianti, C.; D’Angelo, E.; Santus, P. Plethysmographic Loops: A Window on the Lung Pathophysiology of COPD Patients. Front. Physiol. 2018, 9, 484. [Google Scholar] [CrossRef]
- Jaeger, M.J.; Bouhuys, A. Loop Formation in Pressure vs. Flow Diagrams Obtained by Body Plethysmographic Techniques1. Clin. Exerc. Test. 1970, 4, 116–130. [Google Scholar] [CrossRef]
- Pecchiari, M.; Radovanovic, D.; Santus, P.; D’Angelo, E. Airway occlusion assessed by single breath N2 test and lung P-V curve in healthy subjects and COPD patients. Respir. Physiol. Neurobiol. 2016, 234, 60–68. [Google Scholar] [CrossRef]
- Pecchiari, M.; Santus, P.; Radovanovic, D.; DʼAngelo, E. Acute effects of long-acting bronchodilators on small airways detected in COPD patients by single-breath N2 test and lung P-V curve. J. Appl. Physiol. 2017, 123, 1266–1275. [Google Scholar] [CrossRef]
- Buist, A.S.; Ross, B.B. Quantitative analysis of the alveolar plateau in the diagnosis of early airway obstruction. Am. Rev. Respir. Dis. 1973, 108, 1078–1087. [Google Scholar] [PubMed]
- Bégin, R.; Renzetti, A.D.; Bigler, A.H.; Watanabe, S. Flow and age dependence of airway closure and dynamic compliance. J. Appl. Physiol. 1975, 38, 199–207. [Google Scholar] [CrossRef]
- Pecchiari, M.; Pelucchi, A.; D’Angelo, E.; Foresi, A.; Milic-Emili, J.; D’Angelo, E. Effect of Heliox Breathing on Dynamic Hyperinflation in COPD Patients. Chest 2004, 125, 2075–2082. [Google Scholar] [CrossRef] [PubMed]
- D’Angelo, E.; Santus, P.; Civitillo, M.F.; Centanni, S.; Pecchiari, M. Expiratory flow-limitation and heliox breathing in resting and exercising COPD patients. Respir. Physiol. Neurobiol. 2009, 169, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Eltayara, L.; Ghezzo, H.; Milic-Emili, J. Orthopnea and Tidal Expiratory Flow Limitation in Patients With Stable COPD. Chest 2001, 119, 99–104. [Google Scholar] [CrossRef][Green Version]
- Koulouris, N.G.; Valta, P.; Lavoie, A.; Corbeil, C.; Chassé, M.; Braidy, J.; Milic-Emili, J. A simple method to detect expiratory flow limitation during spontaneous breathing. Eur. Respir. J. 1995, 8, 306–313. [Google Scholar] [CrossRef]
- Pecchiari, M.; Radovanovic, D.; Zilianti, C.; Saderi, L.; Sotgiu, G.; D’Angelo, E.; Santus, P. Tidal expiratory flow limitation induces expiratory looping of the alveolar pressure-flow relation in COPD patients. J. Appl. Physiol. 2020, 129, 75–83. [Google Scholar] [CrossRef]
- Tantucci, C.; Duguet, A.; Similowski, T.; Zelter, M.; Derenne, J.P.; Milic-Emili, J. Effect of salbutamol on dynamic hyperinflation in chronic obstructive pulmonary disease patients. Eur. Respir. J. 1998, 12, 799–804. [Google Scholar] [CrossRef]
- Boni, E.; Bezzi, M.; Carminati, L.; Corda, L.; Grassi, V.; Tantucci, C. Expiratory Flow Limitation Is Associated With Orthopnea and Reversed by Vasodilators and Diuretics in Left Heart Failure. Chest 2005, 128, 1050–1057. [Google Scholar] [CrossRef]
- Topalovic, M.; Exadaktylos, V.; Troosters, T.; Celis, G.; Aerts, J.-M.; Janssens, W. Non-linear parameters of specific resistance loops to characterise obstructive airways diseases. Respir. Res. 2017, 18, 9. [Google Scholar] [CrossRef][Green Version]
- Tantucci, C.; Ellaffi, M.; Duguet, A.; Zelter, M.; Similowski, T.; Derenne, J.-P.; Milic-Emili, J.; Haworth, C.; Freemont, A.; Webb, A.; et al. Dynamic hyperinflation and flow limitation during methacholine-induced bronchoconstriction in asthma. Eur. Respir. J. 1999, 14, 477–478. [Google Scholar] [CrossRef]
- Pedersen, O.F.; Butler, J.P. Expiratory Flow Limitation. In Comprehensive Physiology; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2011; Volume 1, pp. 1861–1882. [Google Scholar]
- Tantucci, C. Expiratory Flow Limitation Definition, Mechanisms, Methods, and Significance. Pulm. Med. 2013, 2013, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Junhasavasdikul, D.; Telias, I.; Grieco, D.L.; Chen, L.; Gutierrez, C.M.; Piraino, T.; Brochard, L. Expiratory Flow Limitation During Mechanical Ventilation. Chest 2018, 154, 948–962. [Google Scholar] [CrossRef]
- Koulouris, N.; Hardavella, G. Physiological techniques for detecting expiratory flow limitation during tidal breathing. Eur. Respir. Rev. 2011, 20, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.A.; Rodarte, J.R.; Butler, J.P. Wave-Speed and Viscous Flow Limitation. In Comprehensive Physiology; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Hyatt, R.E. Forced Expiration. In Comprehensive Physiology; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Koulouris, N.G.; Dimopoulou, I.; Valta, P.; Finkelstein, R.; Cosio, M.G.; Milic-Emili, J. Detection of expiratory flow limitation during exercise in COPD patients. J. Appl. Physiol. 1997, 82, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Díaz, O.; Villafranca, C.; Ghezzo, H.; Borzone, G.; Leiva, A.; Milic-Emili, J.; Lisboa, C. Breathing pattern and gas exchange at peak exercise in COPD patients with and without tidal flow limitation at rest. Eur. Respir. J. 2001, 17, 1120–1127. [Google Scholar] [CrossRef]
- Pecchiari, M.; Anagnostakos, T.; D’Angelo, E.; Roussos, C.; Nanas, S.; Koutsoukou, A. Effect of heliox breathing on flow limitation in chronic heart failure patients. Eur. Respir. J. 2009, 33, 1367–1373. [Google Scholar] [CrossRef]
- Koulouris, N.G.; Kaltsakas, G.; Palamidas, A.F.; Gennimata, S.-A. Methods for Assessing Expiratory Flow Limitation during Tidal Breathing in COPD Patients. Pulm. Med. 2012, 2012, 234145. [Google Scholar] [CrossRef]
- Tantucci, C.; Duguet, A.; Ferretti, A.; Mehiri, S.; Arnulf, I.; Zelter, M.; Similowski, T.; Derenne, J.-P.; Milic-Emili, J. Effect of negative expiratory pressure on respiratory system flow resistance in awake snorers and nonsnorers. J. Appl. Physiol. 1999, 87, 969–976. [Google Scholar] [CrossRef][Green Version]
- Liistro, G.; Veriter, C.; Dury, M.; Aubert, G.; Stanescu, D. Expiratory flow limitation in awake sleep-disordered breathing subjects. Eur. Respir. J. 1999, 14, 185–190. [Google Scholar] [CrossRef][Green Version]
- Verin, E.; Tardif, C.; Portier, F.; Similowski, T.; Pasquis, P.; Muir, J.F. Evidence for expiratory flow limitation of extrathoracic origin in patients with obstructive sleep apnoea. Thorax 2002, 57, 423–428. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ninane, V.; LeDuc, D.; Kafi, S.A.; Nasser, M.; Houa, M.; Sergysels, R. Detection of Expiratory Flow Limitation by Manual Compression of the Abdominal Wall. Am. J. Respir. Crit. Care Med. 2001, 163, 1326–1330. [Google Scholar] [CrossRef] [PubMed]
- Kafi, S.A.; Serste, T.; LeDuc, D.; Sergysels, R.; Ninane, V. Expiratory flow limitation during exercise in COPD: Detection by manual compression of the abdominal wall. Eur. Respir. J. 2002, 19, 919–927. [Google Scholar] [CrossRef] [PubMed]
- E Hyatt, R. The interrelationships of pressure, flow, and volume during various respiratory maneuvers in normal and emphysematous subjects. Am. Rev. Respir. Dis. 1961, 83, 676–683. [Google Scholar]
- Ingram, R.H.; Schilder, D.P. Effect of gas compression on pulmonary pressure, flow, and volume relationship. J. Appl. Physiol. 1966, 21, 1821–1826. [Google Scholar] [CrossRef]
- D’Angelo, E.; Prandi, E.; Milic-Emili, J. Dependence of maximal flow-volume curves on time course of preceding inspiration. J. Appl. Physiol. 1993, 75, 1155–1159. [Google Scholar] [CrossRef]
- Pellegrino, R.; Brusasco, V. Lung hyperinflation and flow limitation in chronic airway obstruction. Eur. Respir. J. 1997, 10, 543–549. [Google Scholar]
- Mead, J.; Whittenberger, J.L. Physical Properties of Human Lungs Measured During Spontaneous Respiration. J. Appl. Physiol. 1953, 5, 779–796. [Google Scholar] [CrossRef]
- Dellacà, R.; Santus, P.; Aliverti, A.; Stevenson, N.; Centanni, S.; Macklem, P.; Pedotti, A.; Calverley, P. Detection of expiratory flow limitation in COPD using the forced oscillation technique. Eur. Respir. J. 2004, 23, 232–240. [Google Scholar] [CrossRef]
- Dellacà, R.L.; Duffy, N.; Pompilio, P.P.; Aliverti, A.; Koulouris, N.G.; Pedotti, A.; Calverley, P.M.A. Expiratory flow limitation detected by forced oscillation and negative expiratory pressure. Eur. Respir. J. 2006, 29, 363–374. [Google Scholar] [CrossRef]
- Laghi, F.; Goyal, A. Auto-PEEP in respiratory failure. Minerva Anestesiol 2011, 78, 201–221. [Google Scholar] [PubMed]
- Dal Vecchio, L.D.; Polese, G.; Poggi, R.; Rossi, A. “Intrinsic” positive end-expiratory pressure in stable patients with chronic obstructive pulmonary disease. Eur. Respir. J. 1990, 3, 74–80. [Google Scholar] [PubMed]
- Haluszka, J.; Chartrand, D.A.; Grassino, A.E.; Milic-Emili, J. Intrinsic PEEP and Arterial P CO2 in Stable Patients with Chronic Obstructive Pulmonary Disease. Am. Rev. Respir. Dis. 1990, 141, 1194–1197. [Google Scholar] [CrossRef]
- Petrof, B.J.; Legare, M.; Goldberg, P.; Milic-Emili, J.; Gottfried, S.B. Continuous Positive Airway Pressure Reduces Work of Breathing and Dyspnea during Weaning from Mechanical Ventilation in Severe Chronic Obstructive Pulmonary Disease. Am. Rev. Respir. Dis. 1990, 141, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Otis, A.B.; McKerrow, C.B.; Bartlett, R.A.; Mead, J.; McIlroy, M.B.; Selverstone, N.J.; Radford, E.P. Mechanical Factors in Distribution of Pulmonary Ventilation. J. Appl. Physiol. 1956, 8, 427–443. [Google Scholar] [CrossRef] [PubMed]
- Gorini, M.; Villella, G.; Ginanni, R.; Augustynen, A.; Tozzi, D.; Corrado, A. Effect of assist negative pressure ventilation by microprocessor based iron lung on breathing effort. Thorax 2002, 57, 258–262. [Google Scholar] [CrossRef]
- Bellani, G.; Coppadoro, A.; Patroniti, N.; Turella, M.; Marocco, S.A.; Grasselli, G.; Mauri, T.; Pesenti, A. Clinical Assessment of Auto-positive End-expiratory Pressure by Diaphragmatic Electrical Activity during Pressure Support and Neurally Adjusted Ventilatory Assist. Anesthesiology 2014, 121, 563–571. [Google Scholar] [CrossRef]
- Appendini, L. About the relevance of dynamic intrinsic PEEP (PEEPi, dyn) measurement. Intensive Care Med. 1999, 25, 252–254. [Google Scholar] [CrossRef]
- Bégin, P.; Grassino, A. Inspiratory Muscle Dysfunction and Chronic Hypercapnia in Chronic Obstructive Pulmonary Disease. Am. Rev. Respir. Dis. 1991, 143, 905–912. [Google Scholar] [CrossRef]
- Peslin, R. Theoretical analysis of airway resistances on an inhomogeneous lung. J. Appl. Physiol. 1968, 24, 761–767. [Google Scholar] [CrossRef]
- Campbell, A.H.; Imberger, H.; Jones, B.M. Increased upper airway resistance in patients with airway narrowing. Br. J. Dis. Chest 1976, 70, 58–65. [Google Scholar] [CrossRef]
- Baz, M.; Haji, G.S.; Menzies-Gow, A.; Tanner, R.J.; Hopkinson, N.S.; Polkey, M.I.; Hull, J.H. Dynamic laryngeal narrowing during exercise: A mechanism for generating intrinsic PEEP in COPD? Thorax 2015, 70, 251–257. [Google Scholar] [CrossRef]
- Higenbottam, T.; Payne, J. Glottis narrowing in lung disease. Am. Rev. Respir. Dis. 1982, 125, 746–750. [Google Scholar] [PubMed]
- Campbell, E.; Friend, J. Action of breathing exercises in pulmonary emphysema. Lancet 1955, 265, 325–329. [Google Scholar] [CrossRef]
- Ninane, V.; Rypens, F.; Yernault, J.-C.; De Troyer, A. Abdominal Muscle Use during Breathing in Patients with Chronic Airflow Obstruction. Am. Rev. Respir. Dis. 1992, 146, 16–21. [Google Scholar] [CrossRef]
- Ninane, V.; Yernault, J.-C.; De Troyer, A. Intrinsic PEEP in Patients with Chronic Obstructive Pulmonary Disease: Role of Expiratory Muscles. Am. Rev. Respir. Dis. 1993, 148, 1037–1042. [Google Scholar] [CrossRef] [PubMed]
- Zakynthinos, S.G.; Vassilakopoulos, T.; Zakynthinos, E.; Roussos, C. Accurate measurement of intrinsic positive end-expiratory pressure: How to detect and correct for expiratory muscle activity. Eur. Respir. J. 1997, 10, 522–529. [Google Scholar]
| Young | Elderly | P(1) | NFLpre | P(2) | FLpre | P(3) | |
|---|---|---|---|---|---|---|---|
| Pat BREAK, cmH2O | 0.46 (0.31) | 0.52 (0.59) | 1.000 | 1.21 (1.18) | 0.003 | 4.50 (2.09) | <0.001 |
| Palv,ee, cmH2O | 0.09 (0.05) | 0.10 (0.11) | 1.000 | 0.23 (0.22) | 0.003 | 0.76 (0.37) | <0.001 |
| Pat BREAK-Palv,ee, cmH2O | 0.40 (0.28) | 0.46 (0.52) | 1.000 | 1.06 (1.10) | 0.003 | 3.82 (1.80) | <0.001 |
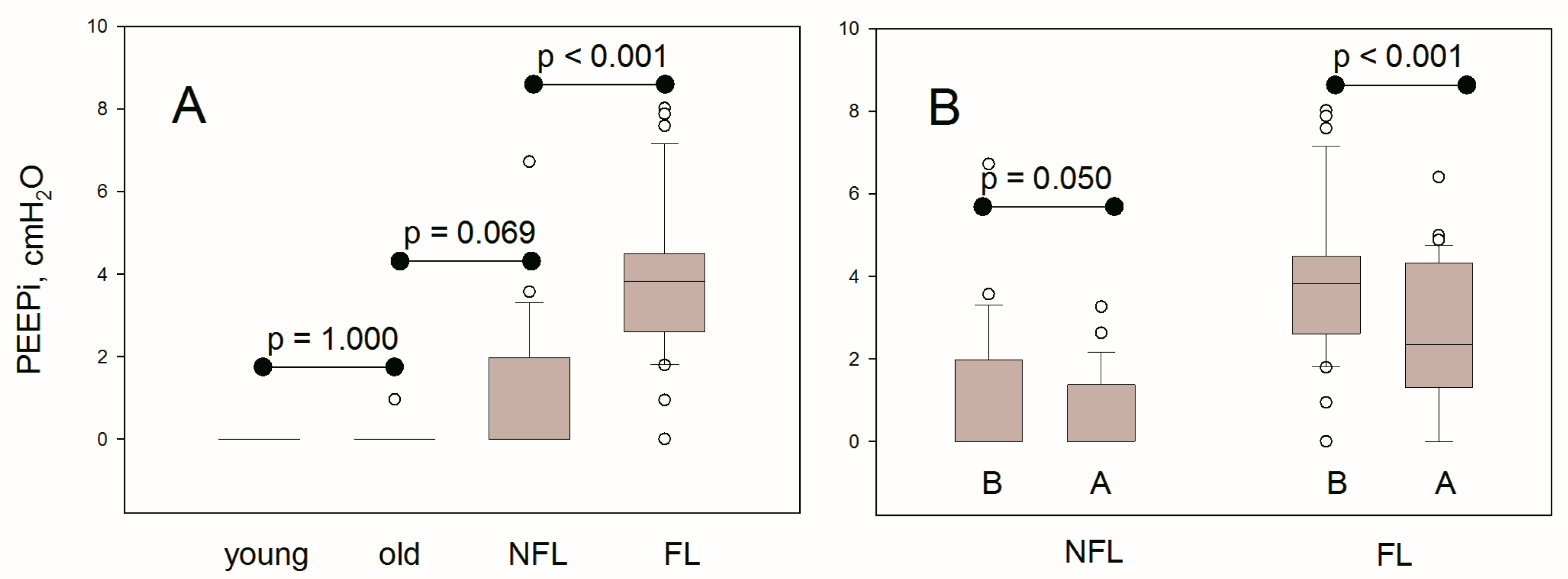
| PEEPi, cmH2O | 0.0 (0.0) | 0.0 (0.0) | 1.000 | 0.0 (1.8) | 0.069 | 3.8 (1.8) | <0.001 |
| Haluszka et al. | Present Investigation | |||
|---|---|---|---|---|
| Esophageal PEEPi | Plethysmographic PEEPi | |||
| R | p | R | p | |
| IC, % p | −0.47 | <0.001 | −0.36 | 0.005 |
| VC, % p | −0.55 | <0.001 | −0.30 | 0.021 |
| FEV1, % p | −0.56 | <0.001 | −0.50 | <0.001 |
| TLC, % p | −0.08 | n.s. | 0.26 | 0.047 |
| RV, % p | 0.45 | <0.001 | 0.36 | 0.004 |
| ITGV, % p | 0.31 | <0.01 | 0.39 | 0.002 |
| Raw, cmH2O s L−1 | 0.69 | <0.001 | 0.53 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zilianti, C.; Santus, P.; Pecchiari, M.; D’Angelo, E.; Radovanovic, D. Diagnostic Insights from Plethysmographic Alveolar Pressure Assessed during Spontaneous Breathing in COPD Patients. Diagnostics 2021, 11, 918. https://doi.org/10.3390/diagnostics11060918
Zilianti C, Santus P, Pecchiari M, D’Angelo E, Radovanovic D. Diagnostic Insights from Plethysmographic Alveolar Pressure Assessed during Spontaneous Breathing in COPD Patients. Diagnostics. 2021; 11(6):918. https://doi.org/10.3390/diagnostics11060918
Chicago/Turabian StyleZilianti, Camilla, Pierachille Santus, Matteo Pecchiari, Edgardo D’Angelo, and Dejan Radovanovic. 2021. "Diagnostic Insights from Plethysmographic Alveolar Pressure Assessed during Spontaneous Breathing in COPD Patients" Diagnostics 11, no. 6: 918. https://doi.org/10.3390/diagnostics11060918
APA StyleZilianti, C., Santus, P., Pecchiari, M., D’Angelo, E., & Radovanovic, D. (2021). Diagnostic Insights from Plethysmographic Alveolar Pressure Assessed during Spontaneous Breathing in COPD Patients. Diagnostics, 11(6), 918. https://doi.org/10.3390/diagnostics11060918






