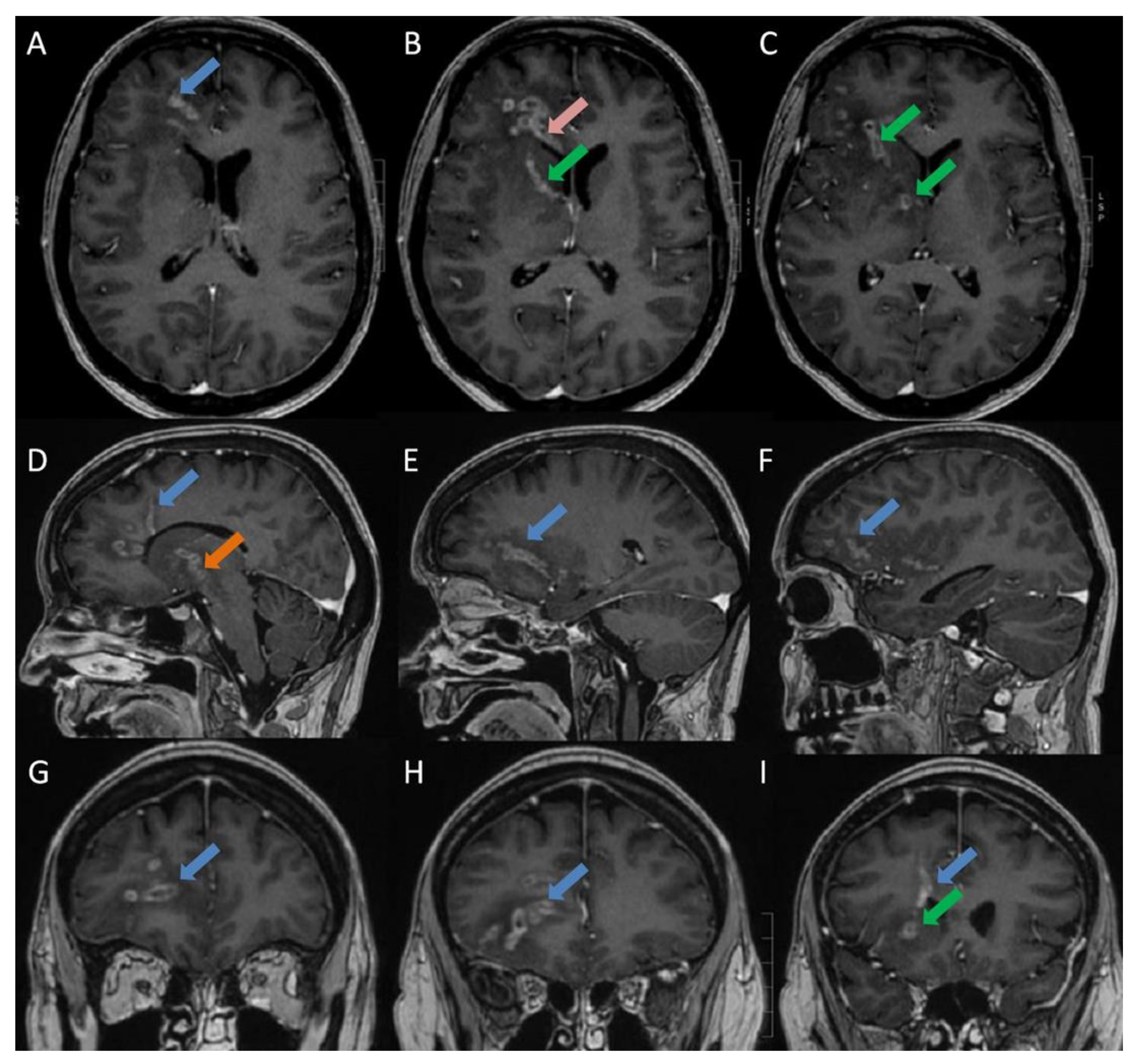
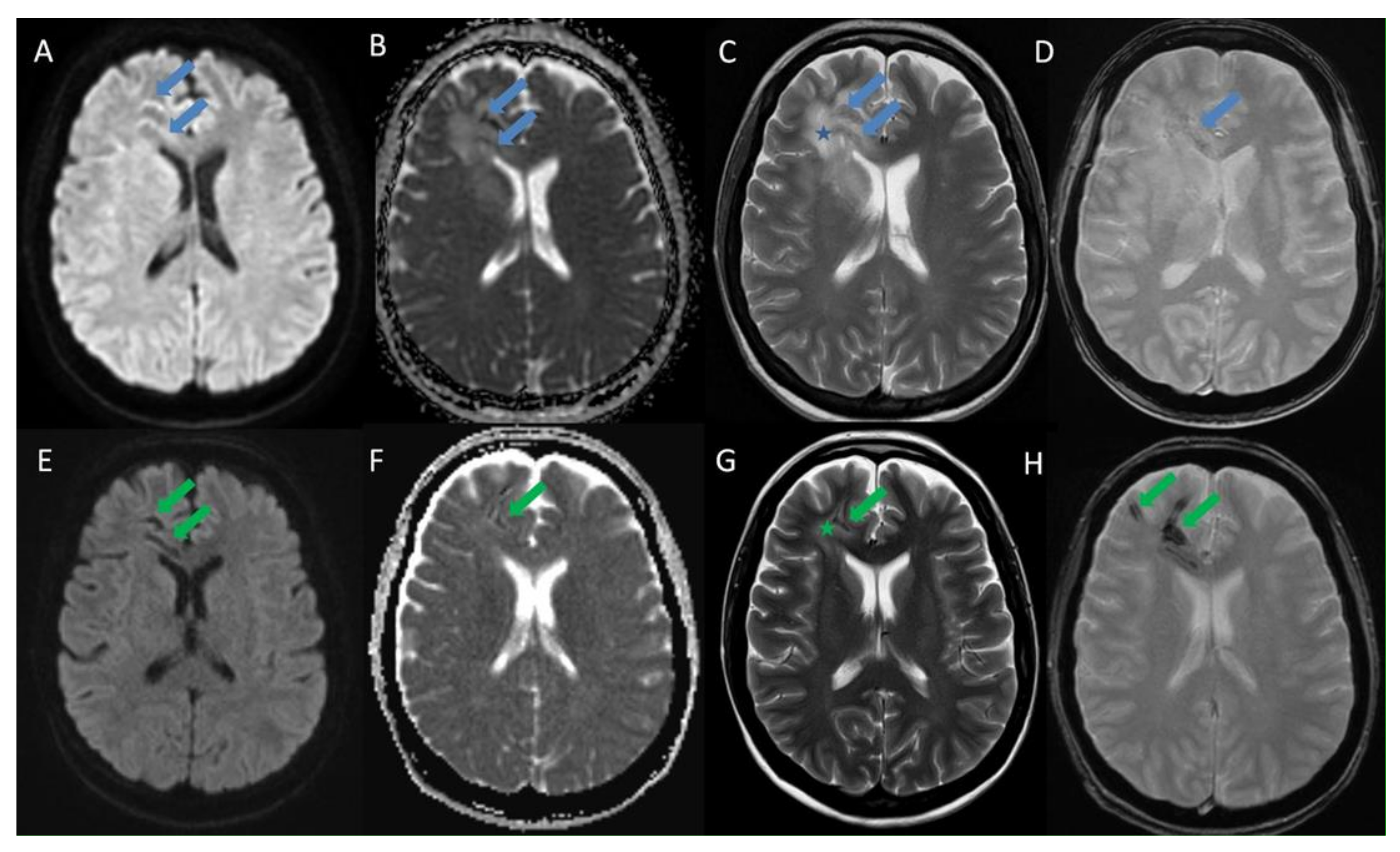
Listeria Monocytogenes Brain Abscesses in a Patient with Disseminated Non-Small Cellular Lung Cancer: MRI Findings
Abstract
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Vázquez-Boland, J.A.; Kuhn, M.; Berche, P.; Chakraborty, T.; Domínguez-Bernal, G.; Goebel, W.; González-Zorn, B.; Wehland, J.; Kreft, J. Listeria Pathogenesis and Molecular Virulence Determinants. Clin. Microbiol. Rev. 2001, 14, 584–640. [Google Scholar] [CrossRef] [PubMed]
- Antal, E.-A.; Løberg, E.M.; Bracht, P.; Melby, K.K.; Maehlen, J. Evidence for Intraaxonal Spread of Listeria monocytogenes from the Periphery to the Central Nervous System. Brain Pathol. 2001, 11, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Dons, L.; Weclewicz, K.; Jin, Y.; Bindseil, E.; Olsen, J.E.; Kristensson, K. Rat dorsal root ganglia neurons as a model for Listeria monocytogenes infections in culture. Med Microbiol. Immunol. 1999, 188, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Charlier, C.; Perrodeau, É.; Leclercq, A.; Cazenave, B.; Pilmis, B.; Henry, B.; Lopes, A.; Maury, M.M.; Moura, A.; Goffinet, F.; et al. Clinical features and prognostic factors of listeriosis: The MONALISA national prospective cohort study. Lancet Infect. Dis. 2017, 17, 510–519. [Google Scholar] [CrossRef]
- Lorber, B. Listeriosis. Clin. Infect. Dis. 1997, 24, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tiri, B.; Priante, G.; Saraca, L.M.; Martella, L.A.; Cappanera, S.; Francisci, D. Listeria monocytogenes Brain Abscess: Controversial Issues for the Treatment—Two Cases and Literature Review. Case Rep. Infect. Dis. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Charlton, K.M. Spontaneous listeric encephalitis in sheep. Electron microscopic studies. Vet. Pathol. 1977, 14, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Oevermann, A.; Di Palma, S.; Doherr, M.G.; Abril, C.; Zurbriggen, A.; Vandevelde, M. Neuropathogenesis of Naturally Occurring Encephalitis Caused byListeria monocytogenesin Ruminants. Brain Pathol. 2010, 20, 378–390. [Google Scholar] [CrossRef] [PubMed]
- Bojanowski, M.W.; Seizeur, R.; Effendi, K.; Bourgouin, P.; Magro, E.; Letourneau-Guillon, L. Spreading of multiple Listeria monocytogenes abscesses via central nervous system fiber tracts: Case report. J. Neurosurg. 2015, 123, 1593–1599. [Google Scholar] [CrossRef] [PubMed]
- Charlier, C.; Poirée, S.; Delavaud, C.; Khoury, G.; Richaud, C.; Leclercq, A.; Hélénon, O.; Lecuit, M. MONALISA study group Imaging of Human Neurolisteriosis: A Prospective Study of 71 Cases. Clin. Infect. Dis. 2018, 67, 1419–1426. [Google Scholar] [CrossRef] [PubMed]
- Van Veen, K.E.B.; Brouwer, M.C.; Van Der Ende, A.; Van De Beek, D. Bacterial Meningitis in Patients using Immunosuppressive Medication: A Population-based Prospective Nationwide Study. J. Neuroimmune Pharmacol. 2017, 12, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Glimåker, M.; Naucler, P.; Sjölin, J. Etiology, clinical presentation, outcome and the effect of initial management in immunocompromised patients with community acquired bacterial meningitis. J. Infect. 2020, 80, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Slezák, O.; Žižka, J.; Kvasnička, T.; Dvořáková, R.; Česák, T.; Ryšková, L.; Ryška, P.; Eliáš, P. Worm-like appearance of Listeria monocytogenes brain abscess: Pesentation of three cases. Neuroradiol. 2020, 62, 1189–1193. [Google Scholar] [CrossRef] [PubMed]
- Peh, W.M.; Hean, G.G.; Clement, Y.H.R. The Tunnel Sign Revisited: A Novel Observation of Cerebral Melioidosis Mimicking Sparganosis. J. Radiol. Case Rep. 2018, 12, 1–11. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simonsen, A.L.; Shekhrajka, N.; Hertz, F.B.; Helweg-Larsen, J.; Bengård Andersen, Å.; Lebech, A.-M. Listeria Monocytogenes Brain Abscesses in a Patient with Disseminated Non-Small Cellular Lung Cancer: MRI Findings. Diagnostics 2021, 11, 1115. https://doi.org/10.3390/diagnostics11061115
Simonsen AL, Shekhrajka N, Hertz FB, Helweg-Larsen J, Bengård Andersen Å, Lebech A-M. Listeria Monocytogenes Brain Abscesses in a Patient with Disseminated Non-Small Cellular Lung Cancer: MRI Findings. Diagnostics. 2021; 11(6):1115. https://doi.org/10.3390/diagnostics11061115
Chicago/Turabian StyleSimonsen, Anders Lykkemark, Nitesh Shekhrajka, Frederik Boëtius Hertz, Jannik Helweg-Larsen, Åse Bengård Andersen, and Anne-Mette Lebech. 2021. "Listeria Monocytogenes Brain Abscesses in a Patient with Disseminated Non-Small Cellular Lung Cancer: MRI Findings" Diagnostics 11, no. 6: 1115. https://doi.org/10.3390/diagnostics11061115
APA StyleSimonsen, A. L., Shekhrajka, N., Hertz, F. B., Helweg-Larsen, J., Bengård Andersen, Å., & Lebech, A.-M. (2021). Listeria Monocytogenes Brain Abscesses in a Patient with Disseminated Non-Small Cellular Lung Cancer: MRI Findings. Diagnostics, 11(6), 1115. https://doi.org/10.3390/diagnostics11061115





