Computer-Aided Detection False Positives in Colonoscopy
Abstract
1. Introduction
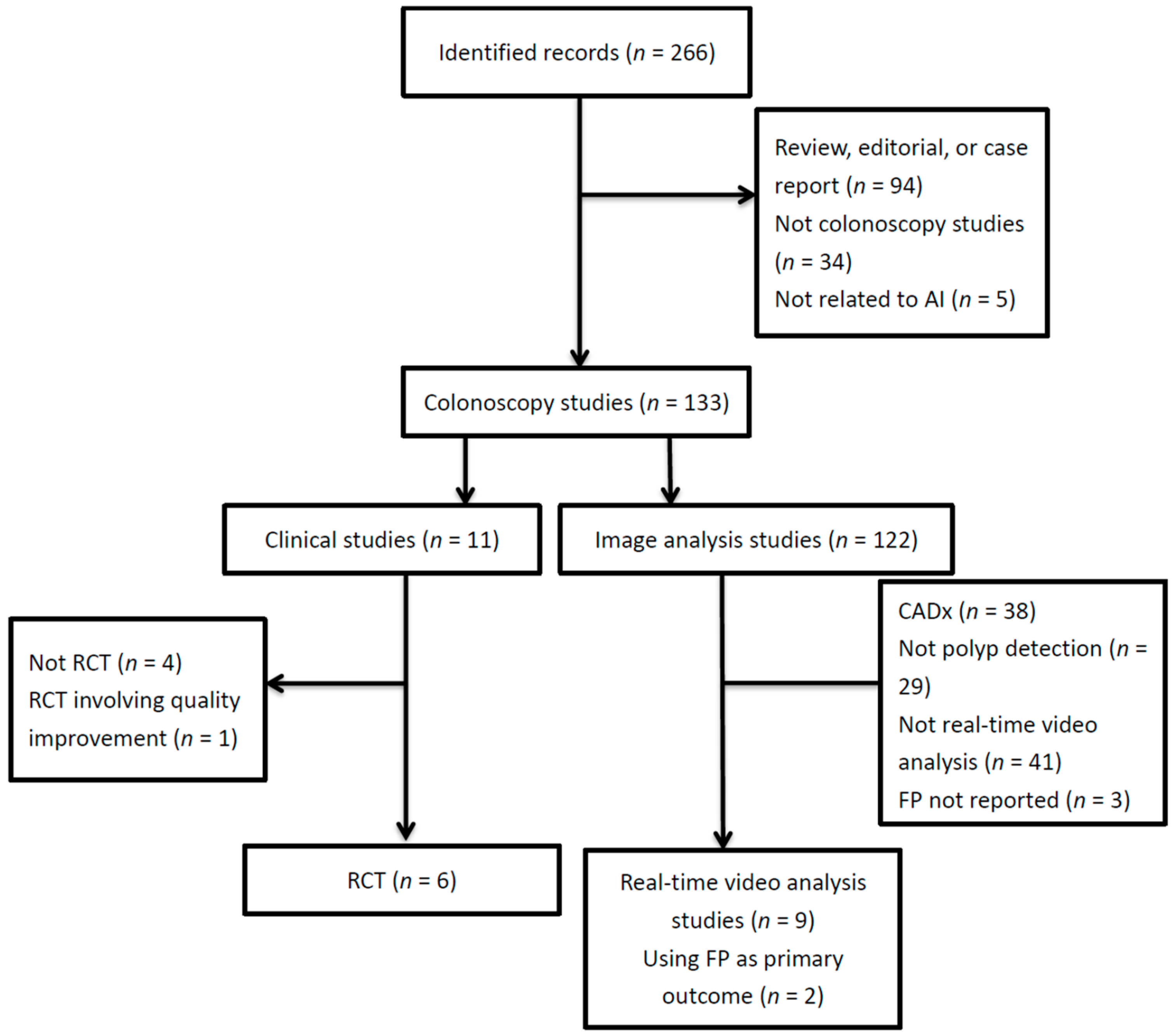
2. Method
3. Definition of False Positives
4. Studies That Report False Positives
4.1. Using CADe Based on Deep Learning for Real-Time Polyp Detection in Colonoscopy Videos
4.2. RCTs Comparing Real-Time CADe with Control
4.3. Video Analysis Studies Using FPs as the Primary Uutcome
5. The Causes of False Positives
6. Adverse Effects of FPs
6.1. Increased Withdrawal Time
6.2. Unnecessary Polypectomies of Non-Neoplastic Lesions
6.3. Increased User Fatigue, Distractions, and Decreased Enthusiasm
7. How to Address the Occurrence of FPs
8. Water Exchange and Its Potential Beneficial Effect on Reducing FPs
9. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Le Clercq, C.M.; Bouwens, M.W.; Rondagh, E.J.; Bakker, C.M.; Keulen, E.T.; de Ridder, R.J.; Winkens, B.; Masclee, A.A.; Sanduleanu, S. Postcolonoscopy colorectal cancers are preventable: A population-based study. Gut 2014, 63, 957–963. [Google Scholar] [CrossRef]
- Rex, D.K.; Schoenfeld, P.S.; Cohen, J.; Pike, I.M.; Adler, D.G.; Fennerty, M.B.; Lieb, J.G., 2nd; Park, W.G.; Rizk, M.K.; Sawhney, M.S.; et al. Quality indicators for colonoscopy. Gastrointest. Endosc. 2015, 81, 31–53. [Google Scholar] [CrossRef]
- Vinsard, D.G.; Mori, Y.; Misawa, M.; Kudo, S.E.; Rastogi, A.; Bagci, U.; Rex, D.K.; Wallace, M.B. Quality assurance of computer-aided detection and diagnosis in colonoscopy. Gastrointest. Endosc. 2019, 90, 55–63. [Google Scholar] [CrossRef]
- Liu, W.N.; Zhang, Y.Y.; Bian, X.Q.; Wang, L.J.; Yang, Q.; Zhang, X.D.; Huang, J. Study on detection rate of polyps and adenomas in artificial-intelligence-aided colonoscopy. Saudi J. Gastroenterol. 2020, 26, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Repici, A.; Badalamenti, M.; Maselli, R.; Correale, L.; Radaelli, F.; Rondonotti, E.; Ferrara, E.; Spadaccini, M.; Alkandari, A.; Fugazza, A.; et al. Efficacy of Real-Time Computer-Aided Detection of Colorectal Neoplasia in a Randomized Trial. Gastroenterology 2020, 159, 512–520.e7. [Google Scholar] [CrossRef] [PubMed]
- Su, J.R.; Li, Z.; Shao, X.J.; Ji, C.R.; Ji, R.; Zhou, R.C.; Li, G.C.; Liu, G.Q.; He, Y.S.; Zuo, X.L.; et al. Impact of a real-time automatic quality control system on colorectal polyp and adenoma detection: A prospective randomized controlled study (with videos). Gastrointest. Endosc. 2020, 91, 415–424.e4. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Berzin, T.M.; Glissen Brown, J.R.; Bharadwaj, S.; Becq, A.; Xiao, X.; Liu, P.; Li, L.; Song, Y.; Zhang, D.; et al. Real-time automatic detection system increases colonoscopic polyp and adenoma detection rates: A prospective randomised controlled study. Gut 2019, 68, 1813–1819. [Google Scholar] [CrossRef]
- Wang, P.; Liu, X.; Berzin, T.M.; Glissen Brown, J.R.; Liu, P.; Zhou, C.; Lei, L.; Li, L.; Guo, Z.; Lei, S.; et al. Effect of a deep-learning computer-aided detection system on adenoma detection during colonoscopy (CADe-DB trial): A double-blind randomised study. Lancet Gastroenterol. Hepatol. 2020, 5, 343–351. [Google Scholar] [CrossRef]
- Hassan, C.; Spadaccini, M.; Iannone, A.; Maselli, R.; Jovani, M.; Chandrasekar, V.T.; Antonelli, G.; Yu, H.; Areia, M.; Dinis-Ribeiro, M.; et al. Performance of artificial intelligence in colonoscopy for adenoma and polyp detection: A systematic review and meta-analysis. Gastrointest. Endosc. 2021, 93, 77–85.e6. [Google Scholar] [CrossRef]
- Ahmad, O.F.; Mori, Y.; Misawa, M.; Kudo, S.E.; Anderson, J.T.; Bernal, J.; Berzin, T.M.; Bisschops, R.; Byrne, M.F.; Chen, P.J.; et al. Establishing key research questions for the implementation of artificial intelligence in colonoscopy: A modified Delphi method. Endoscopy 2020. [Google Scholar] [CrossRef]
- Tang, C.P.; Shao, P.P.; Hsieh, Y.H.; Leung, F.W. A review of water exchange and artificial intelligence in improving adenoma detection. Tzu. Chi. Med. J. 2021, 33, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Hassan, C.; Badalamenti, M.; Maselli, R.; Correale, L.; Iannone, A.; Radaelli, F.; Rondonotti, E.; Ferrara, E.; Spadaccini, M.; Alkandari, A.; et al. Computer-aided detection-assisted colonoscopy: Classification and relevance of false positives. Gastrointest. Endosc. 2020, 92, 900–904.e4. [Google Scholar] [CrossRef]
- Holzwanger, E.A.; Bilal, M.; Glissen Brown, J.R.; Singh, S.; Becq, A.; Ernest-Suarez, K.; Berzin, T.M. Benchmarking definitions of false-positive alerts during computer-aided polyp detection in colonoscopy. Endoscopy 2020. [Google Scholar] [CrossRef]
- Liu, P.; Wang, P.; Glissen Brown, J.R.; Berzin, T.M.; Zhou, G.; Liu, W.; Xiao, X.; Chen, Z.; Zhang, Z.; Zhou, C.; et al. The single-monitor trial: An embedded CADe system increased adenoma detection during colonoscopy: A prospective randomized study. Therap. Adv. Gastroenterol. 2020, 13. [Google Scholar] [CrossRef] [PubMed]
- Becq, A.; Chandnani, M.; Bharadwaj, S.; Baran, B.; Ernest-Suarez, K.; Gabr, M.; Glissen-Brown, J.; Sawhney, M.; Pleskow, D.K.; Berzin, T.M. Effectiveness of a Deep-learning Polyp Detection System in Prospectively Collected Colonoscopy Videos With Variable Bowel Preparation Quality. J. Clin. Gastroenterol. 2020, 54, 554–557. [Google Scholar] [CrossRef]
- Guo, Z.; Nemoto, D.; Zhu, X.; Li, Q.; Aizawa, M.; Utano, K.; Isohata, N.; Endo, S.; Kawarai Lefor, A.; Togashi, K. Polyp detection algorithm can detect small polyps: Ex vivo reading test compared with endoscopists. Dig. Endosc. 2021, 33, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Misawa, M.; Kudo, S.E.; Mori, Y.; Cho, T.; Kataoka, S.; Yamauchi, A.; Ogawa, Y.; Maeda, Y.; Takeda, K.; Ichimasa, K.; et al. Artificial Intelligence-Assisted Polyp Detection for Colonoscopy: Initial Experience. Gastroenterology 2018, 154, 2027–2029.e3. [Google Scholar] [CrossRef]
- Urban, G.; Tripathi, P.; Alkayali, T.; Mittal, M.; Jalali, F.; Karnes, W.; Baldi, P. Deep Learning Localizes and Identifies Polyps in Real Time With 96% Accuracy in Screening Colonoscopy. Gastroenterology 2018, 155, 1069–1078.e8. [Google Scholar] [CrossRef]
- Misawa, M.; Kudo, S.E.; Mori, Y.; Hotta, K.; Ohtsuka, K.; Matsuda, T.; Saito, S.; Kudo, T.; Baba, T.; Ishida, F.; et al. Development of a computer-aided detection system for colonoscopy and a publicly accessible large colonoscopy video database (with video). Gastrointest. Endosc. 2021, 93, 960–967.e3. [Google Scholar] [CrossRef]
- Hassan, C.; Wallace, M.B.; Sharma, P.; Maselli, R.; Craviotto, V.; Spadaccini, M.; Repici, A. New artificial intelligence system: First validation study versus experienced endoscopists for colorectal polyp detection. Gut 2020, 69, 799–800. [Google Scholar] [CrossRef]
- Lee, J.Y.; Jeong, J.; Song, E.M.; Ha, C.; Lee, H.J.; Koo, J.E.; Yang, D.H.; Kim, N.; Byeon, J.S. Real-time detection of colon polyps during colonoscopy using deep learning: Systematic validation with four independent datasets. Sci. Rep. 2020, 10, 8379. [Google Scholar] [CrossRef]
- Podlasek, J.; Heesch, M.; Podlasek, R.; Kilisinski, W.; Filip, R. Real-time deep learning-based colorectal polyp localization on clinical video footage achievable with a wide array of hardware configurations. Endosc. Int. Open 2021, 9, E741–E748. [Google Scholar] [CrossRef]
- Fernandez-Esparrach, G.; Bernal, J.; Lopez-Ceron, M.; Cordova, H.; Sanchez-Montes, C.; Rodriguez de Miguel, C.; Sanchez, F.J. Exploring the clinical potential of an automatic colonic polyp detection method based on the creation of energy maps. Endoscopy 2016, 48, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Younghak, S.; Balasingham, I. Comparison of hand-craft feature based SVM and CNN based deep learning framework for automatic polyp classification. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2017, 2017, 8037556. [Google Scholar] [CrossRef]
- Wang, P.; Xiao, X.; Glissen Brown, J.R.; Berzin, T.M.; Tu, M.; Xiong, F.; Hu, X.; Liu, P.; Song, Y.; Zhang, D.; et al. Development and validation of a deep-learning algorithm for the detection of polyps during colonoscopy. Nat. Biomed. Eng. 2018, 2, 741–748. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Peralta, L.F.; Bote-Curiel, L.; Picon, A.; Sanchez-Margallo, F.M.; Pagador, J.B. Deep learning to find colorectal polyps in colonoscopy: A systematic literature review. Artif. Intell. Med. 2020, 108, 101923. [Google Scholar] [CrossRef]
- Abu Dayyeh, B.K.; Thosani, N.; Konda, V.; Wallace, M.B.; Rex, D.K.; Chauhan, S.S.; Hwang, J.H.; Komanduri, S.; Manfredi, M.; Maple, J.T.; et al. ASGE Technology Committee systematic review and meta-analysis assessing the ASGE PIVI thresholds for adopting real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest. Endosc. 2015, 81, 502.e1–502.e16. [Google Scholar] [CrossRef]
- Mori, Y.; Kudo, S.E.; Misawa, M.; Mori, K. Simultaneous detection and characterization of diminutive polyps with the use of artificial intelligence during colonoscopy. VideoGIE 2019, 4, 7–10. [Google Scholar] [CrossRef]
- Ozawa, T.; Ishihara, S.; Fujishiro, M.; Kumagai, Y.; Shichijo, S.; Tada, T. Automated endoscopic detection and classification of colorectal polyps using convolutional neural networks. Therap. Adv. Gastroenterol. 2020, 13. [Google Scholar] [CrossRef]
- Lavine, R.A.; Sibert, J.L.; Gokturk, M.; Dickens, B. Eye-tracking measures and human performance in a vigilance task. Aviat. Space Environ. Med. 2002, 73, 367–372. [Google Scholar]
- Warm, J.S.; Parasuraman, R.; Matthews, G. Vigilance requires hard mental work and is stressful. Hum. Factors 2008, 50, 433–441. [Google Scholar] [CrossRef]
- Chen, Y.; Fu, R.; Xu, Q.; Yuan, W. Mobile Phone Use in a Car-Following Situation: Impact on Time Headway and Effectiveness of Driver’s Rear-End Risk Compensation Behavior via a Driving Simulator Study. Int. J. Environ. Res. Public Health 2020, 17, 1328. [Google Scholar] [CrossRef] [PubMed]
- Wadhwa, V.; Alagappan, M.; Gonzalez, A.; Gupta, K.; Brown, J.R.G.; Cohen, J.; Sawhney, M.; Pleskow, D.; Berzin, T.M. Physician sentiment toward artificial intelligence (AI) in colonoscopic practice: A survey of US gastroenterologists. Endosc. Int. Open 2020, 8, E1379–E1384. [Google Scholar] [CrossRef] [PubMed]
- Chaptini, L.A.; Janec, E.M.; Seltzer, G.; Peikin, S.; Elfant, A.B. Sublingual hyoscyamine spray as premedication for colonoscopy: A randomized double-blinded placebo-controlled trial. Am. J. Surg. 2008, 196, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Kutyla, M.; O’Connor, S.; Gurusamy, S.R.; Gururatsakul, M.; Gould, K.; Whaley, A.; Kendall, B.J.; Hourigan, L.; Holtmann, G.J. Influence of Simethicone Added to the Rinse Water during Colonoscopies on Polyp Detection Rates: Results of an Unintended Cohort Study. Digestion 2018, 98, 217–221. [Google Scholar] [CrossRef]
- Zhang, S.; Zheng, D.; Wang, J.; Wu, J.; Lei, P.; Luo, Q.; Wang, L.; Zhang, B.; Wang, H.; Cui, Y.; et al. Simethicone improves bowel cleansing with low-volume polyethylene glycol: A multicenter randomized trial. Endoscopy 2018, 50, 412–422. [Google Scholar] [CrossRef]
- Hwang, J.H.; Jamidar, P.; Kyanam Kabir Baig, K.R.; Leung, F.W.; Lightdale, J.R.; Maranki, J.L.; Okolo, P.I., 3rd; Swanstrom, L.L.; Chak, A. GIE Editorial Board top 10 topics: Advances in GI endoscopy in 2019. Gastrointest. Endosc. 2020, 92, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Cadoni, S.; Falt, P.; Rondonotti, E.; Radaelli, F.; Fojtik, P.; Gallittu, P.; Liggi, M.; Amato, A.; Paggi, S.; Smajstrla, V.; et al. Water exchange for screening colonoscopy increases adenoma detection rate: A multicenter, double-blinded, randomized controlled trial. Endoscopy 2017, 49, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, Y.H.; Tseng, C.W.; Hu, C.T.; Koo, M.; Leung, F.W. Prospective multicenter randomized controlled trial comparing adenoma detection rate in colonoscopy using water exchange, water immersion, and air insufflation. Gastrointest. Endosc. 2017, 86, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Jia, H.; Pan, Y.; Guo, X.; Zhao, L.; Wang, X.; Zhang, L.; Dong, T.; Luo, H.; Ge, Z.; Liu, J.; et al. Water Exchange Method Significantly Improves Adenoma Detection Rate: A Multicenter, Randomized Controlled Trial. Am. J. Gastroenterol. 2017, 112, 568–576. [Google Scholar] [CrossRef]
- Fuccio, L.; Frazzoni, L.; Hassan, C.; La Marca, M.; Paci, V.; Smania, V.; De Bortoli, N.; Bazzoli, F.; Repici, A.; Rex, D.; et al. Water exchange colonoscopy increases adenoma detection rate: A systematic review with network meta-analysis of randomized controlled studies. Gastrointest. Endosc. 2018, 88, 589–597.e11. [Google Scholar] [CrossRef] [PubMed]
- Cadoni, S.; Ishaq, S.; Hassan, C.; Falt, P.; Fuccio, L.; Siau, K.; Leung, J.W.; Anderson, J.; Binmoeller, K.F.; Radaelli, F.; et al. Water-assisted colonoscopy: An international modified Delphi review on definitions and practice recommendations. Gastrointest. Endosc. 2020, 93, 1411–1420.e18. [Google Scholar] [CrossRef]
- Hsieh, Y.H.; Koo, M.; Tseng, C.W.; Yang, H.W.; Leung, F.W. Reduction of multitasking distractions underlies the higher adenoma detection rate of water exchange compared to air insufflation—Blinded analysis of withdrawal phase videos. United Eur. Gastroenterol. J. 2019, 7, 230–238. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.L.; Kuo, Y.L.; Hsieh, Y.H.; Tang, J.H.; Leung, F.W. Comparison of Right Colon Adenoma Miss Rates Between Water Exchange and Carbon Dioxide Insufflation: A Prospective Randomized Controlled Trial. J. Clin. Gastroenterol. 2020. ahead of print. [Google Scholar] [CrossRef] [PubMed]
| Study | Per-Frame FPR | Per-polyp FPR | FPR per Colonoscopy | Causes of FP |
|---|---|---|---|---|
| Becq et al. [15] | NA | 60% | NA | NA |
| Guo et al. [16] | When confidence ≥ 10%, 7.8% When confidence ≥ 30%, 2.8% | NA | NA | NA |
| Misawa et al. [17] | 37% | 60% | NA | NA |
| Urban et al. [18] | 7% | NA | NA | NA |
| Misawa et al. [19] | 6.3% | NA | NA | NA |
| Hassan et al. [20] * | 0.9% | NA | NA | NA |
| Lee et al. [21] | 8.3% | NA | 19 | NA |
| Podlasek et al. [22] | 3% | NA | NA | NA |
| Wang et al. [7] | NA | NA | 0.075 | Feces and bubbles 66% Crumpled wall 18% Others 26% |
| Wang et al. [8] | NA | NA | 0.1 | NA |
| Su et al. [6] | NA | NA | 0.201 | NA |
| Liu et al. [4] | NA | NA | 0.071 | Feces and bubbles 64% Crumpled wall 19% Others 17% |
| Liu et al. [14] | NA | NA | 0.074 | Wrinkled mucosa 41% Feces 13.8% Bubbles: 10.3% Others: 34.5% |
| Holzwanger et al. [13] | NA | NA | 26.3 | Folds 91.8% Bubbles 5.6% Stool or others 2.5% |
| Hassan et al. [12] | NA | NA | 27.3 | Bowel wall 88% Bowel contents 12% (stools 5.8%, mucus 2.8%, bubble 2.3%, etc.) |
| Variability | 41 folds | 1 fold | 338 folds | From bowel wall to feces and bubbles |
| Study | Primary Outcome | Videos Reviewed (n) | Polyps Detected | Sensitivity | Specificity |
|---|---|---|---|---|---|
| Misawa et al. [17] | Accuracy of CADe | 155 positive videos and 391 negative videos. Most of the polyps were flat. | NA | Per-frame: 90% | Per-frame: 63.3% |
| Urban et al. [18] | Polyp detection by CADe | 9 randomly selected colonoscopy videos | Performing endoscopist: 28 Three expert reviewers without CADe: 36 One expert reviewer with CADe: 45 | Per-polyp: 94% | Per-frame: 93% |
| Becq et al. [15] | Polyp detection by CADe | 50 colonoscopies from consecutive patients with various bowel preparations. | Performing endoscopist: 55 CADe: 401 possible polyps (100 definite polyps, 63 possible polyps, and 238 false positives | Per-polyp: 98.8% | NA |
| Guo et al. [16] | Accuracy of CADe | 50 videos with small polyps and 50 videos without polyps. | NA | When confidence level ≥10%, per-frame: 66.9% When confidence level ≥30%, per-frame: 56.8% | When confidence level ≥10%, per-frame: 92% When confidence level ≥30%, per-frame: 98% |
| Wang et al. [25] | Accuracy of CADe | 138 videos with polyps and 54 videos without polyps | NA | Per-frame: 91.6% | Per-frame: 95.4% |
| Misawa et al. [19] | Accuracy of CADe in a large, publicly accessible database. | 100 videos | NA | Per-frame: 90.5% Per-polyp: 98.0% | Per frame: 93.7% |
| Hassan et al. [20] | Accuracy of CADe | 138 polyp-positive short videos | NA | Per-frame: 99.7% | NA |
| Lee et al. [21] | Accuracy of CADe | 15 unaltered videos | Performing endoscopist: 38 CADe: 45 | Per-frame: 89.3% | NA |
| Podlasek et al. [22] | Accuracy of CADe | 42 colonoscopy videos | Reviewer: 84 CADe: 79 | Per-polyp: 94.1% | NA |
| Study | Location of Study | Control vs. CADe (n) | Overall ADR | Non-Neoplastic Polyps Detected, n (%) | CADe Used During Insertion | Number of Screens Used | Withdrawal Time, Mean, Minutes | Withdrawal Time, Exclude Biopsy, Mean, Minutes |
|---|---|---|---|---|---|---|---|---|
| Wang et al. [7] | China | 536 vs. 522 | 20.3% vs. 29.1% * | 94 (34.9) vs. 217 (43.6) * (hyperplastic plus inflammatory) | No | 2 | 6.39 vs. 6.89 * | 6.07 vs. 6.18 |
| Wang et al. [8] | China | 478 vs. 484 | 28% vs. 34% * | 113 (37) vs. 200 (40) * (hyperplastic plus inflammatory) | No | 1 | 6.99 vs. 7.46 * | 6.37 vs. 6.48 |
| Repici et al. [5] | Italy | 344 vs. 341 | 40.4% vs. 54.8% * | 57 (16.6) vs. 68 (19.9) (Normal, hyperplastic, inflammatory and others) | Yes | 1 | NA | 7.0 vs. 7.3 |
| Su et al. [6] | China | 308 vs. 315 | 16.5% vs. 28.9% * | NA | No | 2 | 5.68 vs. 7.03 * | 6.74 vs. 6.82 * |
| Liu et al. [4] | China | 518 vs. 508 | 23.9% vs. 39.1% * | 92 (37.1) vs. 203 (41.8) * (proliferative and inflammatory) | No | 2 | NA | 6.32 vs. 6.37 |
| Liu et al. [14] | China | 397 vs. 393 | 20.9% vs. 29.0% * | 87 (42.7) vs. 222 (52.7) * (hyperplastic and inflammatory) | No | 1 | 6.94 vs. 7.29 * | 6.62 vs. 6.71 |
| Relevant Data | Holzwanger et al. [13] | Hassan et al. [12] |
|---|---|---|
| Manufacturer of CADe model | Shanghai Wision AI Co., Ltd. | GI-GENIUS, Medtronic, Version 1.0.2. June 2019 |
| Primary outcome | FPs per colonoscopy | To generate a structured classification of FPs and to estimate their frequency and clinical relevance |
| Videos reviewed (n) | 62 colonoscopy videos collected prospectively with consecutive patients undergoing routine colonoscopy | A post hoc analysis of 40 withdrawal phase videos of the CADe arm from an RCT |
| Study | Sample Size, Air Insufflation vs. WE (n) | Primary Outcome: ADR (95%CI) | Overall BBPS Scores or | Right Colon BBPS Score |
|---|---|---|---|---|
| Jia et al. [40] | 1650 vs. 1653 | 13.4% vs. 18.3%; RR 1.45 (1.20–1.75) * | 7.0 ± 2.3 vs. 7.3 ± 1.6 # (Mean ± SD) | 2.3 ± 0.7 vs. 2.2 ± 1.5 # |
| Hsieh et al. [39] | 217 vs. 217 | 37.5% (31.6–44.4%) vs. 49.8% (43–56.4%) * | 6.2 ± 1.1 vs. 7.1 ± 1.3 # (Mean ± SD) | NA |
| Cadoni et al. [38] | 408 vs. 408 | 43.4% (35.6–45.3 %) vs. 49.3% (44.3 –54.2 %) * | 8.0 (6.0–9.0) vs. 9.0 (7.0–9.0) # [Median (IQR)] | 2.0 (2.0–3.0) vs. 3.0 (2.0–3.0) # |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, Y.-H.; Tang, C.-P.; Tseng, C.-W.; Lin, T.-L.; Leung, F.W. Computer-Aided Detection False Positives in Colonoscopy. Diagnostics 2021, 11, 1113. https://doi.org/10.3390/diagnostics11061113
Hsieh Y-H, Tang C-P, Tseng C-W, Lin T-L, Leung FW. Computer-Aided Detection False Positives in Colonoscopy. Diagnostics. 2021; 11(6):1113. https://doi.org/10.3390/diagnostics11061113
Chicago/Turabian StyleHsieh, Yu-Hsi, Chia-Pei Tang, Chih-Wei Tseng, Tu-Liang Lin, and Felix W. Leung. 2021. "Computer-Aided Detection False Positives in Colonoscopy" Diagnostics 11, no. 6: 1113. https://doi.org/10.3390/diagnostics11061113
APA StyleHsieh, Y.-H., Tang, C.-P., Tseng, C.-W., Lin, T.-L., & Leung, F. W. (2021). Computer-Aided Detection False Positives in Colonoscopy. Diagnostics, 11(6), 1113. https://doi.org/10.3390/diagnostics11061113






